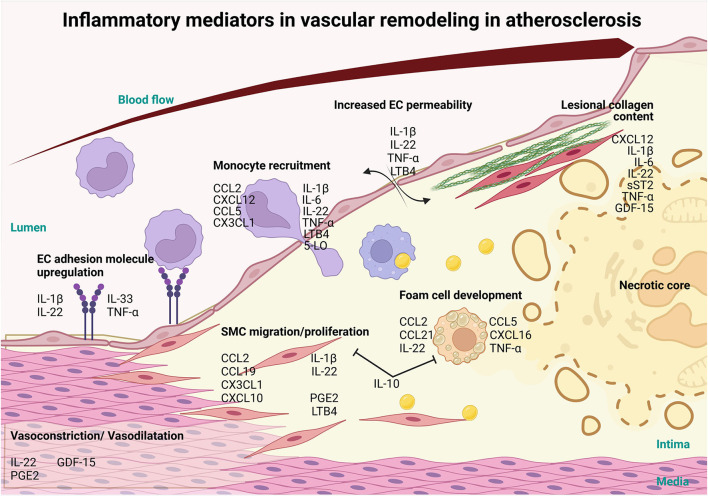
Figure 1.
Involvement of inflammatory mediators in vascular remodeling in atherosclerosis. Inflammatory mediators, such as interlukin-1β (IL-1β), IL-22, IL-33 and tumor necrosis factor-α (TNFα) cytokines can influence the progression of atherosclerosis and CVD via the activation of the endothelium resulting in the upregulation of adhesion molecules. Furthermore, these mediators increase vascular permeability, through IL-1β, IL-22, TNFα and LTB4 and along with the adhesion molecule upregulation allows for the infiltration of monocytes and other immune cells recruited via chemokine ligand 2 (CCL2), C-X-C Motif Chemokine Ligand 12 (CXCL12), CCL5, CX3CL1, IL-1β, IL-6, IL-22, TNF-α Leukotriene B4 (LTB4), 5-LO. Mediators like CCL2, CCL19, CXCL10, CX3CL1, IL-1β, IL-22, Prostaglandin E2 (PGE2) and LTB4 also induce the migration and proliferation of VSMCs into the intima and affect the production of collagen, which, in turn, modulates plaque stability. Foam cell formation is initiated by CCL2, CCL5, CCL21, CXCL16, IL-22 and TNFα and exhausted foam cells undergoing apoptosis and necrosis to establish the necrotic core of the lesion. On the other hand, IL-10, a potent anti-inflammatory cytokine, prevents the formation of foam cells and SMC migration and proliferation. As the lesion grows, blood vessel lumen is narrowing eventually causing vessel occlusion which may lead to major adverse cardiovascular complications. Inflammatory mediators CXCL12, IL-1β, IL-6, IL-22, soluble suppression of tumorigenesis-2 (sST2), TNFα and Growth/Differentiation Factor-15 (GDF-15) also play a role in the stability of the lesion by controlling collagen in the fibrous cap. In addition, mediators like LL-22, GDF-15 and PGE2 regulate vasoconstriction and vasodilation of the arteries thereby controlling blood pressure and ensuring proper vascular function (this figure was made with Biorender.com).