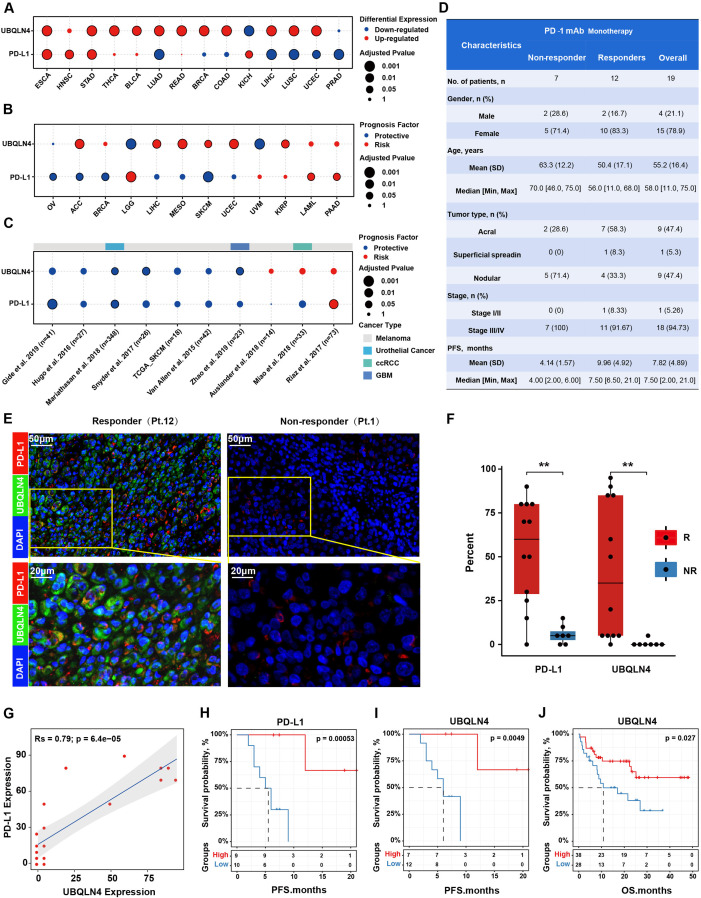
Figure 6.
UBQLN4/PD-L1 expression levels were correlated with the efficacy of PD-1 mAb therapy in melanoma patients. (A) Differential expression of UBQLN4 and PD-L1 across 16 cancer types compared with paired normal samples (fold change >1.5; adjusted p<0.05). Cancer types with UBQLN4 or PD-L1 significantly differentially expressed were shown. (B) Survival analysis demonstrated the effect of UBQLN4 and PD-L1 on patient overall survival in traditional therapy strategies. (C) Survival analysis demonstrated the effect of UBQLN4 and PD-L1 on patient overall survival in anti-PD-1 immunotherapy. (D) Clinical characteristics of anti-PD-1 monotherapy cohorts. Patients were stratified into response groups based on RECIST (Response Evaluation Criteria in Solid Tumors) 1.1 criteria, patients with a complete response (CR), partial response (PR), or stable disease (SD) with progression-free survival (PFS) longer than 6 months were classified as responders, while patients with SD with PFS shorter than 6 months and PD were categorized as non-responders. TNM stage based on the eighth Edition Melanoma Stage Classification. (E) Representative fluorescent images of UBQLN4 and PD-L1 in two patients with a different response. (F) Significantly differential expression of UBQLN4 and PD-L1 between non-responder and responder. Significance was determined by the Wilcoxon rank-sum test, **p<0.01. (G) Scatterplot showed a significant correlation between UBQLN4 and PD-L1 expression. (H, I) Kaplan-Meier estimates for PFS of patients derived from Xiangya hospital patients (n=19) were stratified into two groups based on the median expression level of PD-L1 (H) and UBQLN4 (I), respectively. Significance was determined by the log-rank test. (J) Kaplan-Meier estimates for overall survival of patients derived from Harel et al,39 (n=66).