Abstract
The impacts of the Coronavirus Disease 2019 (COVID‐19) pandemic on sleep health have been studied extensively. However, little is known about sleep problems within the family system during the pandemic. This study aimed to examine the influence of the COVID‐19 pandemic on insomnia in both adults and children, and to explore whether parental COVID‐19 related worries, lifestyles, and insomnia were associated with child insomnia. A total of 1355 parent–child dyads (39.2% fathers, mean age 38.37 years, SD = 5.34; 52.7% boys, mean age 12.47 years, SD = 1.67) were recruited from Jiangxi province in China from 4 to 18 February 2020. Data on insomnia, COVID‐19 related worries, physical activity, and screen time were collected using online questionnaires. Path analysis showed that COVID‐19 related worries and screen time were positively associated with insomnia in both parents and children; while children's physical activity was negatively related to children's insomnia. Parents' insomnia, COVID‐19 related worries, physical activity, and screen time were positively associated with children's insomnia, COVID‐19 related worries, physical activity, and screen time, respectively. Bootstrap tests showed that parents' worries were positively associated with children's insomnia via parents' insomnia and children's worries; parents' physical activity was negatively associated with children's insomnia via children's physical activity, parents' screen time was positively associated with children's insomnia via parents' insomnia and children's screen time. Both parental and child sleep are affected by the pandemic. Parental insomnia, stress reaction, and lifestyles contribute to child insomnia. Child sleep health may be maintained or improved by family bonds, home exercise, and sleep schedules.
Keywords: family study, insomnia, parent–child, physical activity, screen time, worries
1. INTRODUCTION
The Coronavirus Disease 2019 (COVID‐19) outbreak has a widespread and profound impact on daily routine, psychological distress, and physical health (Cao et al., 2020; Fisher et al., 2020; Pierce et al., 2020; Sanudo et al., 2020). Sleep, as a public health issue, is also impacted by the pandemic. Cross‐sectional studies have revealed a high prevalence of insomnia among Chinese adults and adolescents (23.2%–29.9%) during the COVID‐19 pandemic (Yu et al., 2020; Zhou et al., 2020). A longitudinal study also reported that insomnia increased from 26.2% in pre‐COVID‐19 to 33.7% during early‐COVID‐19 periods (Li et al., 2020), although some studies reported opposite findings (e.g. longer night‐time sleep duration, better sleep quality, and less daytime sleepiness) (Gao & Scullin, 2020; Ong et al., 2021). Previous studies have demonstrated that COVID‐19 related stress, sociodemographic characteristics, environmental background, and biological factors were associated with sleep problems during the COVID‐19 pandemic (Ong et al., 2021; Yu et al., 2020; Zhou et al., 2020). However, little is known about sleep problems within the family system during the pandemic.
To cope with COVID‐19, restrictions and lockdown strategies were carried out. Schools were closed and non‐essential public places were prohibited. People spent more time at home and contacted their families more often. Thus, parents and children may share similar sleep changes during this special period. The links between parents' sleep and children's sleep may be bidirectional. A cross‐sectional study by Uccella et al. (2021) found that parents' discomfort related to quarantine (COVID‐19 stress, sleep problems) was strongly associated with behavioural changes in their children (age under 18 years). Considering parents' roles in child development, parental factors might have greater effects on children's sleep. More studies are needed to examine whether parental factors, such as parental psychological distress, lifestyles, or insomnia, are associated with children's insomnia during the pandemic.
During the outbreak of COVID‐19, parents and children stayed at home and faced various stressors together. Although children may experience increased stress and anxiety during the COVID‐19 pandemic, parents too may experience poorer mental health given employment/financial circumstances, health concerns, and uncertainty (Fisher et al., 2020; Pierce et al., 2020). COVID‐19 related stress (being worried about COVID‐19, self‐quarantine, and community infection) may be associated with increased parent anxiety, depression, and insomnia symptoms (Cao et al., 2020; Lu et al., 2020; Meyer et al., 2020). It is possible that children may become aware of their parents' worry about COVID‐19 from direct discussion with their parents or by observing their behaviour. To date, no longitudinal studies have investigated the association between parents and children's COVID‐19 related worries. However, one cross‐sectional study also found positive associations between parents' and children's COVID‐19 related fear (Suffren et al., 2021). These studies suggest that COVID‐19 related worries could transfer from parents to children, and it is possible that these worries could affect sleep quality.
Home confinement also greatly changed people's lifestyles, especially for physical activity and screen time (Lopez‐Bueno et al., 2020; Sanudo et al., 2020; Zheng et al., 2020). Because social isolation and physical distance restrictions were enacted, the usual exercise places were no longer accessible. Reduced physical activity levels and increased screen time have been reported (Meyer et al., 2020; Sanudo et al., 2020; Zheng et al., 2020). Insufficient physical activity is a key risk factor for physical health, mental well‐being, cognition, and sleep (Biddle et al., 2019). With more time at home, people spend less time exercising, while spending more time watching TV, playing on computers, and using cell phones (Sanudo et al., 2020; Zheng et al., 2020). Limited physical activity and increased screen time during the COVID‐19 pandemic negatively affected mental health and sleep quality (Lu et al., 2020; Meyer et al., 2020; Sanudo et al., 2020). Thus, it is essential to take physical activity and screen time into consideration with insomnia when it comes to the impact of the COVID‐19 pandemic on sleep (Becker & Gregory, 2020).
Parental participation plays an important role in children's physical activity and screen time (Rhodes et al., 2020). One longitudinal study that collected three waves of data from 2007 to 2013 reported that parents' physical activity increased children's physical activity (Garriguet et al., 2017). Another longitudinal study that examined TV behaviours in parents and their girls at age 9 and 11 years, found that parents' TV‐related behaviours increased girls' TV time (Davison et al., 2005). Furthermore, parental involvement may promote children's sleep through household practices and good sleep hygiene (Godsell & White, 2019; Mindell & Williamson, 2018). Also, a positive family environment, with less chaos and disorganisation could benefit children's sleep (Billows et al., 2009; Koopman‐Verhoeff et al., 2019). Thus, those who have good family relationships and spend time with their parents may have good physical health, regular sufficient sleep, and good sleep quality. These findings suggested the positive role of parental lifestyles and sleep on child sleep. However, in the context of the COVID‐19 pandemic, rare studies assess parents' sleep and children's sleep together, and physical activity levels and screen time simultaneously.
In this study, we aimed to examine: (1) How COVID‐19 related worries and lifestyles influenced parents' and children's insomnia? (2) How parents' COVID‐19 related worries, physical activity, screen time, and insomnia were associated with children's COVID‐19 related worries, physical activity, screen time, and insomnia, respectively? (3) Whether parental COVID‐19 related worries, lifestyles, and insomnia were associated with children's insomnia? The first hypothesis was that parents and children with fewer COVID‐19 related worries, more positive and regular lifestyles would show fewer insomnia symptoms during the COVID‐19 pandemic. The second hypothesis was that parents who were more physically active, reporting less screen time, having fewer COVID‐19 related worries and insomnia would have children who were also more physically active, reporting less screen time, having fewer COVID‐19 related worries and insomnia. The third hypothesis was that children's insomnia might be associated with parents' insomnia, via COVID‐19 related worries, physical activity, and screen time.
METHODS
Participants and procedure
The cross‐sectional data were collected online from 4 to 18 February 2020 after the outbreak of COVID‐19 in China. Students above fourth grade and at least one of their parents from two schools in Jiangxi Province located in east China volunteered to participate in this project. The COVID‐19 problems were relatively severe in Jiangxi Province. On 24 January 2020, Jiangxi province initiated a Level 1 public health response, ordered to close entertainment places, and implemented enclosed management (http://www.jiangxi.gov.cn/art/2020/1/25/art_16141_3322712.html). Work resumption and the spring semester of primary and high school were delayed until at least 29 February (http://www.jiangxi.gov.cn/art/2020/2/10/art_4969_1498534.html) and 11 May 2020 (http://sfj.nc.gov.cn/ncsfj/xwdt/202005/9b91db5c8fbd4cb7ba6654480387f23f.shtml), respectively. On 4 February 2020, the Health Commission of Jiangxi Province announced 548 confirmed cases in Jiangxi Province (http://www.jiangxi.gov.cn/art/2020/2/5/art_16140_1503738.html). By midnight on 18 February, 571 confirmed cases were reported (http://www.jiangxi.gov.cn/art/2020/2/19/art_16140_1507646.html). An online platform was chosen to comply with social restrictions and confinement regulations during pandemic events. Online questionnaires were distributed to students and parents, respectively, to collect data of demographics, physical activity, screen time, COVID‐19 related worries, self‐quarantine, community infection, and insomnia symptoms through the Wenjuanxing platform (https://www.wjx.cn/). A total of 1876 children participated in this survey. After removing incomplete questionnaires and unmatched parent–child samples, 1355 parent–child dyads were included in the study. The final sample consisted of 1355 parents (39.2% male; mean age 38.37 years, SD = 5.34, ranging from 27 to 69) and 1355 children (52.7% male; mean age 12.47 years, SD = 1.67, ranging from 9 to 17).
Approval for this study was obtained from the local Bureau of Education and the Ethics Committee of the School of Psychology, Jiangxi Normal University. All participants signed informed consent to participate in the study online. Due to logistics challenges caused by the outbreak of the COVID‐19 pandemic (e.g., participants' fear of infection), an online survey is a convenient and efficient method to assess participants' psychological distress and to obtain informed consent. Numerous studies have used a similar procedure to investigate the psychological impact of quarantine (Brooks et al., 2020).
Measures
Demographics
Demographic variables contained gender (male, female), age, location (urban, rural) and the highest level of education (primary school, junior middle school, high school, and college degree or above). Variables of location and education levels were only included in the parent's version questionnaire.
Physical activity
One item was used to measure parent and child physical activity level: “How many days per week did you exercise in the past two weeks?” Five different choices are given, each with a value of 1 to 5 (1 = null, 2 = <1 day per week, 3 = 1–2 days per week, 4 = 3–4 days per week, 5 = 5–7 days per week).
Screen time
Three items were used to assess parent and child screen time: (1) How many hours per day do you spend on TV? (2) How many hours per day do you spend on the computer? (3) How many hours per day do you spend on your cell phone? All questions were responded on a 4‐point Likert scale (1 = <1 hour per day, 2 = 1–2 hours per day, 3 = 3–5 hours per day, 4 = ≥6 hours per day). The hours of screen viewing (TV, computer, and cell phone) were added up to obtain an overall screen time.
COVID‐19 related stress
Self‐quarantine
Parents were asked to indicate their current status (self‐quarantine): Are you confirmed or suspected as having COVID‐19? This item was rated from 1 to 5 (1 = confirmed, 2 = suspected, 3 = isolated in hospital, 4 = home isolation, 5 = normal people). Because category 1–4 had few responses, we recoded this item from 0 (no) to 1 (yes).
Community infection
Parents were also asked to indicate their current community infection status: Was anyone confirmed or suspected as having COVID‐19 in your community or village? This item was rated from 1 to 3 (1 = confirmed, 2 = nobody, 3 = do not know).
COVID‐19 related worries
Both parents' and children's COVID‐19 related worries were measured using the following questions: (1) Are you worried about yourself being infected with COVID‐19? (2) Are you worried about your family members being infected with COVID‐19? (3) Are you worried about residents of your community or village being infected with COVID‐19? They were rated from 1 to 3 (1 = not worried, 2 = worried, 3 = very worried).The Cronbach's α of COVID‐19 related worries for parents and children were 0.86 and 0.90, respectively.
Insomnia
To keep consistent with the assessment for children, the Youth Self‐Rating Insomnia Scale (YSIS) was used to measure parents' and children's insomnia within the past 2 weeks (Liu et al., 2019). The YSIS consists of eight items that were based on ICSD‐3 and DSM‐5 diagnostic criteria. The eight items specifically are asking about sleep quality, sleep satisfaction, and sleep problems (difficulty initiating sleep, difficulty maintaining sleep, early morning awakening, sleep insufficiency, unrefreshing sleep, daytime functioning impairment). Each item is rated from 1 to 5. The total score ranges from 8 to 40. The cutoffs were as follows: normal (8–21), mild insomnia (22–25), moderate insomnia (26–29), and severe insomnia (30–48) (Liu et al., 2019). The YSIS has been used in Chinese community adults (Geng et al., 2021) and college students (Wang et al., 2021), demonstrating good reliability and validity. Besides, Cronbach's α was 0.88 with the current parent sample, and 0.89 with the children's sample, indicating good reliability.
Statistical analyses
Descriptive statistics were used to analyse sample characteristics, COVID‐19 related worries, self‐quarantine, community infection, the proportion of physical activity level, and the proportion of screen time. Pearson correlations between insomnia and all variables were examined. To examine our study hypotheses, path analysis was used to examine the relationships of physical activity, screen time, COVID‐19 related worries, self‐quarantine, and community infection among parents and children. Demographics were modelled as covariates; indirect effects were calculated with bootstrapping. Regarding COVID‐19 related worries, 36 participants did not report their worries because they indicated that their family members or community had been infected with COVID‐19. Two methods have been used to deal with these participants. First, they were grouped into the “very worried” category given the higher stress they might meet. Second, they were regarded as missing data. The results of the two methods are similar. The findings of the first method are presented in the results section, and the main findings of the second method are supplied, see Figure S1.
The fit of model without an interaction term was evaluated by chi‐square (χ2), the comparative fit index (CFI), the Tucker‐Lewis index (TLI), and the root mean square error of approximation (RMSEA). Values of CFI and TLI above 0.09, and RMSEA values below 0.08 are an acceptable model fit (Hu & Bentler, 1999). Multiple group contrasts were conducted to examine differences in the effects of parents' lifestyles and well‐being on their children between different demographics, including parents' sex, children's sex, children's age, and parent–child relationships (father‐boy, father‐girl, mother‐boy, and mother‐girl). Changes of χ2 were used to test significance. Statistical analyses were conducted with SPSS 26.0 and Mplus 7.0. The significant level was set at p < 0.05, two tails.
RESULTS
Descriptive statistics of demographics, COVID‐19 related worries, physical activity, and screen time
The demographics, COVID‐19 related worries, self‐quarantine, and community infection are presented in Table 1. A majority of parents resided in the rural area (62.7%) and had junior middle school education (65.5%). About 6.6% of parents reported that they were in self‐quarantine, and 8.9% reported that residents in their community or village were infected. High percentages of parents (71.5%) and children (62.5%) worried about themselves being infected with COVID‐19. While the worries about family members being infected were more common, with 81.0% and 71.9% for parents and children, respectively. A much higher proportion of 1199 (88.5%) parents and 1042 (76.9%) children reported their worries about residents in their community or village being infected with COVID‐19. Additionally, parents reported mild, moderate, and severe insomnia at a rate of 5.2%, 1.2%, and 1.4%, respectively, while children reported mild, moderate, and severe insomnia at a rate of 7.8%, 2.7%, and 1.6%, respectively.
TABLE 1.
Demographics and COVID‐19 related stress variables
| Variable | Parents, n (%) | Children, n (%) |
|---|---|---|
| Age, years (mean ± SD) | 38.37 ± 5.34 | 12.47 ± 1.67 |
| Sex | ||
| Male | 531 (39.2) | 714 (52.7) |
| Female | 824 (60.8) | 641 (47.3) |
| Location | ||
| Urban | 505 (37.3) | — |
| Rural | 850 (62.7) | — |
| Education | ||
| Primary school | 242 (17.9) | — |
| Junior middle school | 888 (65.5) | — |
| High school | 186 (13.7) | — |
| College degree or above | 39 (2.9) | — |
| Self‐quarantine | ||
| Yes | 89 (6.6) | — |
| No | 1266 (93.4) | — |
| Community infection | ||
| Yes | 121 (8.9) | — |
| No | 901 (66.5) | — |
| Do not know | 333 (24.6) | — |
| Are you worried about being infected with COVID‐19? | ||
| Not worried | 386 (28.5) | 508 (37.5) |
| Worried | 734 (54.2) | 662 (48.9) |
| Very worried | 235 (17.3) | 185 (13.7) |
| Are you worried about your family members being infected with COVID‐19? | ||
| Not worried | 258 (19.0) | 381 (28.1) |
| Worried | 734 (54.2) | 696 (51.4) |
| Very worried | 363 (26.8) | 278 (20.5) |
| Are you worried about residents of your community or village being infected with COVID‐19? | ||
| Not worried | 156 (11.5) | 313 (23.1) |
| Worried | 869 (64.1) | 809 (59.7) |
| Very worried | 330 (24.4) | 233 (17.2) |
The proportions of physical activity and screen time among parents and children are presented in Table 2. More parents spent less than 1 day a week exercising than children (52.4% parents versus 43.1% children). The proportions of screen time among parents and children were quite similar. Most parents and children spent 1–2 h per day watching TV (39.2% parents, 41.4% children), and less than 1 h per day on the computer (75.9% parents, 66.2% children). The proportions using cell phones for 1–2 h per day among parents and children were 28.3% and 34.9%, respectively, and for 3–5 h per day among parents and children were 30.6% and 28.8%, respectively.
TABLE 2.
Proportions (n, weighted %) of physical activity and screen time among parents and children
| Variable | Parents, n (%) | Children, n (%) |
|---|---|---|
| Physical activity | ||
| 0 day/week | 387 (28.6) | 266 (19.6) |
| <1 day/week | 322 (23.8) | 318 (23.5) |
| 1–2 day/week | 356 (26.3) | 420 (31.0) |
| 3–4 day/week | 194 (14.3) | 225 (16.6) |
| 5–7 day/week | 96 (7.1) | 126 (9.3) |
| TV | ||
| <1 h/day | 351 (25.9) | 379 (28.0) |
| 1–2 h/day | 531 (39.2) | 561 (41.4) |
| 3–5 h/day | 326 (24.1) | 313 (23.1) |
| ≥6 h/day | 147 (10.8) | 102 (7.5) |
| Computer | ||
| <1 h/day | 1029 (75.9) | 897 (66.2) |
| 1–2 h/day | 190 (14.0) | 292 (21.5) |
| 3–5 h/day | 86 (6.3) | 117 (8.6) |
| ≥6 h/day | 50 (3.7) | 49 (3.6) |
| Cell phone | ||
| <1 h/day | 238 (17.6) | 352 (26.0) |
| 1–2 h/day | 384 (28.3) | 473 (34.9) |
| 3–5 h/day | 414 (30.6) | 390 (28.8) |
| ≥6 h/day | 319 (23.5) | 140 (10.3) |
The Pearson correlation matrix of study variables
Table 3 presents means, standard deviations, and the Pearson correlation matrix of study variables. For parents, there were no significant correlations of insomnia with age, sex, location, education, and physical activity, while community infection, self‐quarantine, screen time, COVID‐19 related worries were significantly positively correlated with insomnia. For children, children's insomnia was negatively correlated with physical activity, while positively correlated with parents' self‐quarantine, children's screen time, and COVID‐19 related worries. Parents' insomnia, COVID‐19 related worries, screen time, and physical activity were associated with children's insomnia, COVID‐19 related worries, screen time, and physical activity, respectively.
TABLE 3.
Pearson correlations between all variables
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 Age (parents) | 1.00 | |||||||||||||||
| 2 Sex (parents) | −0.29*** | 1.00 | ||||||||||||||
| 3 Location (parents) | 0.03 | −0.07* | 1.00 | |||||||||||||
| 4 Education (parents) | −0.06* | −0.12*** | −0.12*** | 1.00 | ||||||||||||
| 5 Physical activity (parents) | 0.06* | −0.02 | −0.04 | 0.05 | 1.00 | |||||||||||
| 6 Screen time (parents) | −0.05 | −0.05 | −0.10*** | 0.08** | 0.09*** | 1.00 | ||||||||||
| 7 COVID‐19 related worries (parents) | 0.01 | −0.07** | −0.01 | 0.04 | −0.04 | 0.00 | 1.00 | |||||||||
| 8 Insomnia (parents) | 0.03 | −0.02 | −0.01 | 0.02 | 0.00 | 0.15*** | 0.10*** | 1.00 | ||||||||
| 9 Community infection (parents) | 0.02 | 0.01 | −0.03 | −0.00 | 0.01 | −0.03 | 0.12*** | 0.14*** | 1.00 | |||||||
| 10 Self‐quarantine (parents) | −0.05 | −0.01 | −0.01 | −0.02 | 0.02 | 0.02 | 0.06* | 0.09*** | 0.04 | 1.00 | ||||||
| 11 Age (children) | 0.27*** | −0.06* | 0.02 | −0.17*** | 0.02 | 0.01 | 0.01 | 0.08** | 0.02 | −0.01 | 1.00 | |||||
| 12 Sex (children) | −0.03 | 0.05 | 0.02 | −0.03 | −0.07* | −0.02 | −0.03 | 0.06* | 0.03 | −0.01 | −0.01 | 1.00 | ||||
| 13 Physical activity (children) | 0.00 | −0.02 | −0.05 | 0.07** | 0.34*** | 0.07* | −0.00 | −0.04 | −0.02 | −0.01 | −0.04 | −0.07** | 1.00 | |||
| 14 Screen time (children) | −0.04 | −0.02 | −0.02 | −0.00 | 0.06* | 0.30*** | −0.01 | 0.07* | −0.00 | 0.02 | 0.08** | −0.06* | 0.08** | 1.00 | ||
| 15 COVID‐19 related worries (children) | 0.05 | −0.06* | 0.00 | −0.02 | −0.01 | −0.01 | 0.41*** | 0.06* | 0.05 | 0.02 | −0.03 | 0.02 | −0.01 | 0.02 | 1.00 | |
| 16 Insomnia (children) | 0.06* | 0.01 | 0.02 | −0.07** | −0.03 | 0.01 | 0.07* | 0.34*** | 0.07* | 0.09*** | 0.13*** | 0.08** | −0.08** | 0.12*** | 0.15*** | 1.00 |
| M | 38.37 | — | — | — | 0.21 | 6.18 | 6.11 | 13.00 | 0.09 | 0.07 | 12.47 | — | 0.26 | 5.83 | 5.64 | 16.10 |
| SD | 5.34 | — | — | — | 0.41 | 1.89 | 1.72 | 5.24 | 0.29 | 0.25 | 1.67 | — | 0.44 | 1.85 | 1.83 | 4.65 |
p < 0.05.
p < 0.01.
p < 0.001.
Path analysis
The best fitting model and its standardised path coefficients are shown in Figure 1. The model obtained acceptable fit: χ2 = 72.685, df = 39, CFI = 0.963, TLI = 0.946, RMSEA (95% CI) = 0.025 (0.016–0.034).
FIGURE 1.
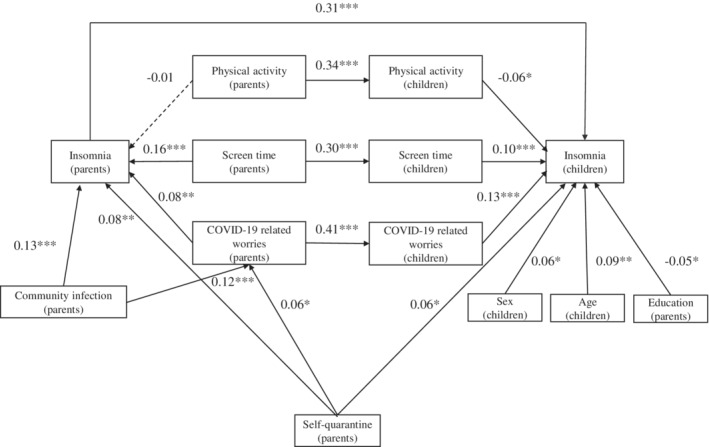
Path diagram of hypothetical model. The rectangle represents an observed variable. *p < 0.05, **p < 0.01, ***p < 0.001
All path coefficients are summarised as follows. The three COVID‐19 related variables, community infection (β = 0.13, p < 0.001), self‐quarantine (β = 0.08, p < 0.01), and COVID‐19 related worries (β = 0.08, p < 0.01) significantly and positively associated with parents' insomnia. However, for lifestyle variables, only screen time was positively associated with parents' insomnia (β = 0.16, p < 0.001). Physical activity was not statistically related to parents' insomnia (β = −0.01, p = 0.663). For the child sample: parents' quarantine (β = 0.06, p < 0.05), children's sex (β = 0.06, p < 0.05), age (β = 0.09, p < 0.01), and education (β = −0.05, p < 0.05) significantly associated with children's insomnia. In addition, children's insomnia was negatively associated with children's physical activity (β = −0.06, p < 0.05), and positively associated with screen time (β = 0.10, p < 0.001) and COVID‐19 related worries (β = 0.13, p < 0.001). Parents' insomnia (β = 0.31, p < 0.001), physical activity (β = 0.34, p < 0.001), screen time (β = 0.30, p < 0.001), and COVID‐19 related worries (β = 0.41, p < 0.001) were separately and positively associated with children's insomnia, physical activity, screen time, and COVID‐19 related worries. The results of indirect effects are presented in Table 4. Bootstrap analyses indicated that parents' insomnia, children's lifestyles, and COVID‐19 related worries completely mediated the relationship of parental lifestyles and COVID‐19 related worries with children's insomnia (specific effect β = −0.020, 95% CI = −0.036 to −0.003 for physical activity; total effects β = 0.077, 95% CI = 0.051–0.103 for screen time; total effects β = 0.080, 95% CI = 0.053–0.106 for COVID‐19 related worries).
TABLE 4.
Bootstrap analysis of indirect effects
| Path | Effect | Bootstrap S.E. | p | Bootstrap (95% CI) | |
|---|---|---|---|---|---|
| Lower 2.5% | Upper 2.5% | ||||
| Total indirect effects from physical activity (parents) to insomnia (children) | −0.024 | 0.013 | 0.064 | −0.048 | 0.002 |
| Physical activity (parents) → insomnia (parents) → insomnia (children) | −0.004 | 0.009 | 0.665 | −0.021 | 0.015 |
| Physical activity (parents) → physical activity (children) → insomnia (children) | −0.020 | 0.009 | 0.021 | −0.036 | −0.003 |
| Total indirect effects from screen time (parents) to insomnia (children) | 0.077 | 0.013 | 0.000 | 0.051 | 0.103 |
| Screen time (parents) → insomnia (parents) → insomnia (children) | 0.048 | 0.011 | 0.000 | 0.029 | 0.070 |
| Screen time (parents) → screen time (children) → insomnia (children) | 0.028 | 0.008 | 0.001 | 0.012 | 0.045 |
| Total indirect effects from COVID‐related worries (parents) to insomnia (children) | 0.080 | 0.013 | 0.000 | 0.053 | 0.106 |
| COVID‐related worries (parents) → insomnia (parents) → insomnia (children) | 0.025 | 0.009 | 0.006 | 0.008 | 0.043 |
| COVID‐related worries (parents) → COVID‐19 related worries (children) → insomnia (children) | 0.055 | 0.010 | 0.000 | 0.036 | 0.076 |
| Total indirect effects from community infection to insomnia (children) | 0.049 | 0.011 | 0.000 | 0.028 | 0.072 |
| Community infection → insomnia (parents) → insomnia (children) | 0.040 | 0.010 | 0.000 | 0.021 | 0.062 |
| Community infection → COVID‐related worries (parents) → insomnia (parents) → insomnia (children) | 0.003 | 0.001 | 0.022 | 0.001 | 0.006 |
| Community infection → COVID‐related worries (parents) → COVID‐19 related worries (children) → insomnia (children) | 0.006 | 0.002 | 0.001 | 0.003 | 0.010 |
| Total indirect effects from self‐quarantine (parents) to insomnia (children) | 0.030 | 0.009 | 0.001 | 0.013 | 0.048 |
| Self‐quarantine (parents) → insomnia (parents) → insomnia (children) | 0.025 | 0.009 | 0.005 | 0.009 | 0.043 |
| Self‐quarantine (parents) → COVID‐related worries (parents) → insomnia (parents) → insomnia (children) | 0.001 | 0.001 | 0.104 | 0.000 | 0.003 |
| Self‐quarantine (parents) → COVID‐related worries (parents) → COVID‐19 related worries (children) → insomnia (children) | 0.003 | 0.002 | 0.044 | 0.000 | 0.007 |
Parental lifestyles and COVID‐19 related worries were not directly associated with children's insomnia. The significant effect of parents' physical activity on children's insomnia was mediated by children's physical activity (specific effect β = −0.020, 95% CI = −0.036 to −0.003). Both parents' screen time (specific effect β = 0.048, 95% CI = 0.029–0.070) and COVID‐19 related worries (specific effect β = 0.025, 95% CI = 0.008–0.043) could be indirectly associated with increased children's insomnia via parents' insomnia; the effects of parents' screen time and COVID‐19 related worries on children's insomnia were also partly mediated by children's screen time (specific effect β = 0.028, 95% CI = 0.012–0.045) and COVID‐19 related worries (specific effect β = 0.055, 95% CI = 0.036–0.076), respectively. In addition, parents' reported community infection was not directly associated with children's insomnia, except for parents' self‐quarantine. The indirect effects of community infection (specific effect β = 0.040, 95% CI = 0.021–0.062) and self‐quarantine (specific effect β = 0.025, 95% CI = 0.009–0.043) on children's insomnia were also mostly mediated by parents' insomnia.
The results of multiple group contrasts showed that relationships from parents' physical activity, screen time, worries, and insomnia to their children were not different between parents' sex, children's sex, and parent–child relationship [Δχ2(1) from 0.02 to 2.29, Δχ2(3) from 0.19 to 2.29; all p > 0.05]. However, the relationships from parents' screen time and COVID‐19 related worries to their children's screen time [Δχ2 (1) = 4.032, p = 0.044] and COVID‐19 related worries [Δχ2 (1) = 3.928, p = 0.047] were different between young (9–12 years) and older children (13–17 years). Young children were more likely to be affected by their parents in screen time and COVID‐19 related worries.
DISCUSSION
Previous studies have examined insomnia symptoms in different samples during the COVID‐19 pandemic (Lu et al., 2020; Yu et al., 2020; Zhou et al., 2020), but currently, family studies are limited. This is the first study using the same questionnaires to assess insomnia, COVID‐19 related worries, self‐quarantine, community infection, physical activity, and screen time of parents and children during the COVID‐19 outbreak. Our findings showed that self‐quarantine, COVID‐19 related worries, screen time were associated with insomnia in both parents and children; while community infection was specifically related to parents' insomnia, and physical activity was related to children's insomnia. Parents' insomnia, COVID‐19 related worries, physical activity, screen time separately and positively associated with children's insomnia, COVID‐19 related worries, physical activity and screen time. Parental COVID‐19 related worries and lifestyles could be associated with children's insomnia via complex mediation of COVID‐19 related stress, lifestyles, and insomnia.
The prevalence of insomnia in the current study is lower than that reported by using the Insomnia Severity Index (Li et al., 2020) and also lower than that reported by the YSIS scale in a community sample before the pandemic (Geng et al., 2021). However, the figure aligns with the findings of a study conducted among college students, which showed a similar proportion (6.1%) of clinical insomnia through for the YSIS scale (Wang et al., 2021). This may be attributed to the special data collection period and the resilience of individuals. The data were collected after the Chinese New Year and winter vacation. On the one hand, during Chinese New Year, each family reunites together and enjoys happiness through shared activities (e.g., exercise, games, and meals). People feel closer to their family members and enhance family bonds that could promote feelings of safety and healthy sleep. On the other hand, parents and children escape from busy work/school schedules, having more time to relax and sleep. Recent studies have also found improved sleep (Blume et al., 2020; Wright et al., 2020). These findings indicated that the general public may remain resilient and flexible in school/work schedules and preserve/enhance sleep health (Becker & Gregory, 2020; Gao & Scullin, 2020). Finally, another possible reason may be that the participants were mostly from rural areas. Families could be more protected by the fact of being able to stay in the open air, and through the confinement due to the lower possibility of being infected.
Consistent with previous studies (Suffren et al., 2021), our findings showed that parents' COVID‐19 related worries were significantly related to children's COVID‐19 related worries. One study has indicated that COVID‐19 related worries was one of important risk factors for insomnia (Lu et al., 2020). Extending this study, we found associations of parental COVID‐19 related worries and insomnia with children's insomnia. Parents' COVID‐19 related worries could be indirectly associated with increased children's insomnia via parents' insomnia and children's COVID‐19 related worries. One study has revealed that parents' reported COVID‐19 fear was more affected by contextual concerns (e.g., financial resources and health services) than their children (Suffren et al., 2021). Thus, parents may convey their concerns about the epidemic to children through communication/behaviours, which would affect children's cognition of the pandemic, and lead to poor sleep.
Similar to previous studies, we found that parents and children's insomnia were positively associated with screen time (Lopez‐Bueno et al., 2020; Suffren et al., 2021; Zheng et al., 2020), while children's physical activity was specifically related to children's insomnia. Contrary to the expectation that physical activity would be significantly associated with insomnia (Lu et al., 2020), we did not find support in our parent sample. One reason for such insignificance might be that parents spent less time exercising, and more time watching TV, playing on the computer or using cell phones; thus, the effect of physical activity on sleep was decreased. This also accords with a previous study (Qin et al., 2020), which showed that people stay at home, spend less time exercising, and more time sitting, and expose themselves to more artificial light or digital screens with excessive use of TV, cell phone, and computer. In general, increased screen time and less physical activity may have adverse effects on sleep quality (Sanudo et al., 2020).
This current study confirmed that children's physical activity and screen time were positively associated with parents' physical activity and screen time (Garriguet et al., 2017). Importantly, findings showed that parents' lifestyles and insomnia could be indirectly associated with children's insomnia: (1) parents' physical activity was indirectly associated with children's insomnia via children's physical activity; (2) parents' screen time was indirectly associated with children's insomnia via parents' insomnia and children's screen time. These results could be explained in different ways. Sleep behaviour is associated with strong familial aggregation, as well as some genetic transmission (Dauvilliers et al., 2005; Partinen et al., 1983). Family studies also confirmed the effects of genetic factors on insomnia (Watson et al., 2006). Moreover, one study pointed out that adolescents' insomnia was significantly associated with parental insomnia symptoms in China (Liu et al., 2016). Nevertheless, it also suggested that adolescents' sleep may largely be affected by biological and environmental factors (Liu et al., 2016). During the COVID‐19 crisis, environmental factors could be parental involvement (e.g., parenting, parents' modelling role and parent–child relationship) (Garriguet et al., 2017; Rhodes et al., 2020). Typically, children spend most of their time with their parents during the COVID‐19 pandemic. Children may imitate their parents' behaviours, such as parents' exercise habits, and digital habits. It should also be noted that links of COVID‐19 related worries, lifestyles, and sleep between parents and children may be bidirectional (Sleddens et al., 2017). To date, only one cross‐sectional family study reported that parents with children under 6 years were more likely to be affected by the COVID‐19 pandemic (Uccella et al., 2021). Thus, longitudinal analysis is needed to examine possible bidirectional associations.
These findings have potential implications for parental involvement and sleep during the pandemic. Solutions to promote good sleep are to keep a regular and healthy sleep schedule, exercise regularly, use fewer electronic devices before sleep, and pay less attention to the COVID‐19 pandemic that would rouse anxiety. Owing to the independent impact of COVID‐19 related worries, physical activity, screen time, and the indirect impact of parental involvement, it is expected that increasing physical activity, limiting screen time, and COVID‐19 related worries concurrently with parental involvement would be a better protective factor to improve child sleep than only focusing on physical activity or others. Moreover, these results can be used to guide physical and psychological measures to prevent insomnia of parents and children.
This current study has its strengths and limitations. Although a large sample of parent–child dyads assessed by the same questionnaire is a strength, several limitations should be noted. First, this study is cross‐sectional, so the causal effect cannot be determined. Second, the findings of this study were derived from participants that were mostly from rural areas. Furthermore, children under 9 years and their parents were not recruited, as children were required to finish the self‐report questionnaire. However, several studies indicate that parents who have young children reported more behavioural and emotional problems than those with older ones during the COVID‐19 outbreak (Jiao et al., 2020; Uccella et al., 2021). Third, this study was conducted in February 2020, just after the COVID‐19 outbreak. The long‐term effect of the pandemic on parents and children needs further study. Fourth, this study only contains one indicator of sleep‐insomnia symptoms. Longitudinal studies with possible more objective measures and sleep pattern indexes among parents and children of all ages are required in the future.
CONCLUSION
Both parents and children's sleep are affected by the pandemic. Parental COVID‐19 related worries and unhealthy lifestyles appear to be risk factors for children's sleep. These findings provide initial evidence of a positive parental role in children's sleep quality in the Chinese sample during the pandemic. To prevent and treat insomnia, it is worthwhile to emphasise the joint effect of healthy lifestyle promotion and parental involvement in child development. Additional studies with a longitudinal design and objective measures are needed to determine how genetic and parental behaviour factors interact in this topic.
CONFLICT OF INTEREST
None.
AUTHOR CONTRIBUTIONS
Nalan Zhan collected and analysed the data and drafted the manuscript; Yeqing Zhang collected the data and revised the manuscript; Dongjie Xie revised the manuscript; Fulei Geng designed the study, supervised the collection and analyses of data, and revised the manuscript.
Supporting information
Figure S1 Path analysis results for participants with missing data in COVID‐19 related worries
ACKNOWLEDGMENTS
The present study was funded by National Natural Science Foundation of China (grant numbers: 31700987). The funder had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Zhan, N. , Zhang, Y. , Xie, D. , & Geng, F. (2022). The associations of parental COVID‐19 related worries, lifestyles, and insomnia with child insomnia during the COVID‐19 outbreak. Journal of Sleep Research, e13590. 10.1111/jsr.13590
Funding information National Natural Science Foundation of China, Grant/Award Number: 31700987
DATA AVAILABILITY STATEMENT
The dataset and Mplus code are available on request from the corresponding author, Fulei Geng.
REFERENCES
- Becker, S. P. , & Gregory, A. M. (2020). Editorial perspective: Perils and promise for child and adolescent sleep and associated psychopathology during the COVID‐19 pandemic. Journal of Child Psychology and Psychiatry, 61(7), 757–759. 10.1111/jcpp.13278 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Biddle, S. J. H. , Ciaccioni, S. , Thomas, G. , & Vergeer, I. (2019). Physical activity and mental health in children and adolescents: An updated review of reviews and an analysis of causality. Psychology of Sport and Exercise, 42, 146–155. 10.1016/j.psychsport.2018.08.011 [DOI] [Google Scholar]
- Billows, M. , Gradisar, M. , Dohnt, H. , Johnston, A. , McCappin, S. , & Hudson, J. (2009). Family disorganization, sleep hygiene, and adolescent sleep disturbance. Journal of Clinical Child and Adolescent Psychology, 38(5), 745–752. 10.1080/15374410903103635 [DOI] [PubMed] [Google Scholar]
- Blume, C. , Schmidt, M. H. , & Cajochen, C. (2020). Effects of the COVID‐19 lockdown on human sleep and rest‐activity rhythms. Current Biology, 30(14), R795–R797. 10.1016/j.cub.2020.06.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brooks, S. K. , Webster, R. K. , Smith, L. E. , Woodland, L. , Wessely, S. , Greenberg, N. , & Rubin, G. J. (2020). The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. Lancet, 395(10227), 912–920. 10.1016/S0140-6736(20)30460-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cao, W. , Fang, Z. , Hou, G. , Han, M. , Xu, X. , Dong, J. , & Zheng, J. (2020). The psychological impact of the COVID‐19 epidemic on college students in China. Psychiatry Research, 287, 112934. 10.1016/j.psychres.2020.112934 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dauvilliers, Y. , Maret, S. , & Tafti, M. (2005). Genetics of normal and pathological sleep in humans. Sleep Medicine Reviews, 9(2), 91–100. 10.1016/j.smrv.2004.06.001 [DOI] [PubMed] [Google Scholar]
- Davison, K. K. , Francis, L. A. , & Birch, L. L. (2005). Links between parents' and girls' television viewing behaviors: A longitudinal examination. The Journal of Pediatrics, 147(4), 436–442. 10.1016/j.jpeds.2005.05.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisher, J. R. , Tran, T. D. , Hammarberg, K. , Sastry, J. , Nguyen, H. , Rowe, H. , Popplestone, S. , Stocker, R. , Stubber, C. , & Kirkman, M. (2020). Mental health of people in Australia in the first month of COVID‐19 restrictions: A national survey. The Medical Journal of Australia, 213(10), 458–464. 10.5694/mja2.50831 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gao, C. , & Scullin, M. K. (2020). Sleep health early in the coronavirus disease 2019 (COVID‐19) outbreak in the United States: Integrating longitudinal, cross‐sectional, and retrospective recall data. Sleep Medicine, 73, 1–10. 10.1016/j.sleep.2020.06.032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garriguet, D. , Colley, R. , & Bushnik, T. (2017). Parent‐child association in physical activity and sedentary behaviour. Health Reports, 28(6), 3–11. https://www.ncbi.nlm.nih.gov/pubmed/28636068 [PubMed] [Google Scholar]
- Geng, F. , Zou, J. , Liang, Y. , Zhan, N. , Li, S. , & Wang, J. (2021). Associations of positive and adverse childhood experiences and adulthood insomnia in a community sample of Chinese adults. Sleep Medicine, 80, 46–51. 10.1016/j.sleep.2021.01.022 [DOI] [PubMed] [Google Scholar]
- Godsell, S. , & White, J. (2019). Adolescent perceptions of sleep and influences on sleep behaviour: A qualitative study. Journal of Adolescence, 73, 18–25. 10.1016/j.adolescence.2019.03.010 [DOI] [PubMed] [Google Scholar]
- Hu, Li. T. , & Bentler P. M. (1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling: A Multidisciplinary Journal, 6(1), 1–55. 10.1080/10705519909540118 [DOI] [Google Scholar]
- Jiao, W. Y. , Wang, L. N. , Liu, J. , Fang, S. F. , Jiao, F. Y. , Pettoello‐Mantovani, M. , & Somekh, E. (2020). Behavioral and emotional disorders in children during the COVID‐19 epidemic. The Journal of Pediatrics, 221, 264, e261–266. 10.1016/j.jpeds.2020.03.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koopman‐Verhoeff, M. E. , Serdarevic, F. , Kocevska, D. , Bodrij, F. F. , Mileva‐Seitz, V. R. , Reiss, I. , Hillegers, M. H. J. , Tiemeier, H. , Cecil, C. A. M. , Verhulst, F. C. , & Luijk, M. (2019). Preschool family irregularity and the development of sleep problems in childhood: A longitudinal study. Journal of Child Psychology and Psychiatry, 60(8), 857–865. 10.1111/jcpp.13060 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li, Y. , Qin, Q. , Sun, Q. , Sanford, L. D. , Vgontzas, A. N. , & Tang, X. (2020). Insomnia and psychological reactions during the COVID‐19 outbreak in China. Journal of Clinical Sleep Medicine, 16(8), 1417–1418. 10.5664/jcsm.8524 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu, J. , Liu, X. , Ji, X. , Wang, Y. , Zhou, G. , & Chen, X. (2016). Sleep disordered breathing symptoms and daytime sleepiness are associated with emotional problems and poor school performance in children. Psychiatry Research, 242, 218–225. 10.1016/j.psychres.2016.05.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu, X. , Yang, Y. , Liu, Z.‐Z. , Luo, Y. , Fan, F. , & Jia, C.‐X. (2019). Psychometric properties of youth self‐rating insomnia scale (YSIS) in Chinese adolescents. Sleep and Biological Rhythms, 17(3), 339–348. 10.1007/s41105-019-00222-3 [DOI] [Google Scholar]
- Lopez‐Bueno, R. , Lopez‐Sanchez, G. F. , Casajus, J. A. , Calatayud, J. , Gil‐Salmeron, A. , Grabovac, I. , Tully, M. A. , & Smith, L. (2020). Health‐related behaviors among school‐aged children and adolescents during the Spanish Covid‐19 confinement. Frontiers in Pediatrics, 8, 573. 10.3389/fped.2020.00573 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu, C. , Chi, X. , Liang, K. , Chen, S. T. , Huang, L. , Guo, T. , Jiao, C. , Yu, Q. , Veronese, N. , Soares, F. C. , Grabovac, I. , Yeung, A. , & Zou, L. (2020). Moving more and sitting less as healthy lifestyle behaviors are protective factors for insomnia, depression, and anxiety among adolescents during the COVID‐19 pandemic. Psychology Research and Behavior Management, 13, 1223–1233. 10.2147/PRBM.S284103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer, J. , McDowell, C. , Lansing, J. , Brower, C. , Smith, L. , Tully, M. , & Herring, M. (2020). Changes in physical activity and sedentary behavior in response to COVID‐19 and their associations with mental health in 3052 US adults. International Journal of Environmental Research and Public Health, 17(18), 6469. 10.3390/ijerph17186469 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mindell, J. A. , & Williamson, A. A. (2018). Benefits of a bedtime routine in young children: Sleep, development, and beyond. Sleep Medicine Reviews, 40, 93–108. 10.1016/j.smrv.2017.10.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ong, J. L. , Lau, T. , Massar, S. A. A. , Chong, Z. T. , Ng, B. K. L. , Koek, D. , Zhao, W. , Yeo, B. T. T. , Cheong, K. , & Chee, M. W. L. (2021). COVID‐19‐related mobility reduction: Heterogenous effects on sleep and physical activity rhythms. Sleep, 44(2), zsaa179. 10.1093/sleep/zsaa179 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Partinen, M. , Kaprio, J. , Koskenvuo, M. , Putkonen, P. , & Langinvainio, H. (1983). Genetic and environmental determination of human sleep. Sleep, 6(3), 179–185. 10.1093/sleep/6.3.179 [DOI] [PubMed] [Google Scholar]
- Pierce, M. , Hope, H. , Ford, T. , Hatch, S. , Hotopf, M. , John, A. , Kontopantelis, E. , Webb, R. , Wessely, S. , McManus, S. , & Abel, K. M. (2020). Mental health before and during the COVID‐19 pandemic: A longitudinal probability sample survey of the UK population. The Lancet Psychiatry, 7(10), 883–892. 10.1016/s2215-0366(20)30308-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qin, F. , Song, Y. , Nassis, G. P. , Zhao, L. , Dong, Y. , Zhao, C. , Feng, Y. , & Zhao, J. (2020). Physical activity, screen time, and emotional well‐being during the 2019 novel coronavirus outbreak in China. International Journal of Environmental Research and Public Health, 17(14), 5170. 10.3390/ijerph17145170 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rhodes, R. E. , Guerrero, M. D. , Vanderloo, L. M. , Barbeau, K. , Birken, C. S. , Chaput, J. P. , Faulkner, G. , Janssen, I. , Madigan, S. , Masse, L. C. , McHugh, T. L. , Perdew, M. , Stone, K. , Shelley, J. , Spinks, N. , Tamminen, K. A. , Tomasone, J. R. , Ward, H. , Welsh, F. , & Tremblay, M. S. (2020). Development of a consensus statement on the role of the family in the physical activity, sedentary, and sleep behaviours of children and youth. International Journal of Behavioral Nutrition and Physical Activity, 17(1), 74. 10.1186/s12966-020-00973-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanudo, B. , Fennell, C. , & Sanchez‐Oliver, A. J. (2020). Objectively‐assessed physical activity, sedentary behavior, smartphone use, and sleep patterns pre‐ and during‐COVID‐19 quarantine in young adults from Spain. Sustainability, 12(15), 5890. 10.3390/su12155890 [DOI] [Google Scholar]
- Sleddens, E. F. C. , Gubbels, J. S. , Kremers, S. P. J. , van der Plas, E. , & Thijs, C. (2017). Bidirectional associations between activity‐related parenting practices, and child physical activity, sedentary screen‐based behavior and body mass index: A longitudinal analysis. International Journal of Behavioral Nutrition and Physical Activity, 14(1), 89. 10.1186/s12966-017-0544-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suffren, S. , Dubois‐Comtois, K. , Lemelin, J. P. , St‐Laurent, D. , & Milot, T. (2021). Relations between child and parent fears and changes in family functioning related to COVID‐19. International Journal of Environmental Research and Public Health, 18(4), 12. 10.3390/ijerph18041786 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uccella, S. , De Grandis, E. , De Carli, F. , D'Apruzzo, M. , Siri, L. , Preiti, D. , Di Profio, S. , Rebora, S. , Cimellaro, P. , Biolcati Rinaldi, A. , Venturino, C. , Petralia, P. , Ramenghi, L. A. , & Nobili, L. (2021). Impact of the COVID‐19 outbreak on the behavior of families in Italy: A focus on children and adolescents. Frontiers in Public Health, 9, 608358. 10.3389/fpubh.2021.608358 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang, D. , Chen, H. , Zhai, S. , Zhu, Z. , Huang, S. , Zhou, X. , Pan, Y. , Meng, D. , Yang, Z. , Zhao, J. , Fan, F. , & Liu, X. (2021). Is returning to school during the COVID‐19 pandemic stressful? A study on immediate mental health status of Chinese college students. Journal of Affective Disorders, 287, 261–267. 10.1016/j.jad.2021.03.035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watson, N. F. , Goldberg, J. , Arguelles, L. , & Buchwald, D. (2006). Genetic and environmental influences on insomnia, daytime sleepiness, and obesity in twins. Sleep, 29(5), 645–649. 10.1093/sleep/29.5.645 [DOI] [PubMed] [Google Scholar]
- Wright, K. P., Jr. , Linton, S. K. , Withrow, D. , Casiraghi, L. , Lanza, S. M. , Iglesia, H. , Vetter, C. , & Depner, C. M. (2020). Sleep in university students prior to and during COVID‐19 stay‐at‐home orders. Current Biology, 30(14), R797–R798. 10.1016/j.cub.2020.06.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu, B. Y. , Yeung, W. F. , Lam, J. C. , Yuen, S. C. , Lam, S. C. , Chung, V. C. , Chung, K. F. , Lee, P. H. , Ho, F. Y. , & Ho, J. Y. (2020). Prevalence of sleep disturbances during COVID‐19 outbreak in an urban Chinese population: A cross‐sectional study. Sleep Medicine, 74, 18–24. 10.1016/j.sleep.2020.07.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zheng, C. , Huang, W. Y. , Sheridan, S. , Sit, C. H. , Chen, X. K. , & Wong, S. H. (2020). COVID‐19 pandemic brings a sedentary lifestyle in young adults: A cross‐sectional and longitudinal study. International Journal of Environmental Research and Public Health, 17(17), 6035. 10.3390/ijerph17176035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou, S. J. , Wang, L. L. , Yang, R. , Yang, X. J. , Zhang, L. G. , Guo, Z. C. , Chen, J. C. , Wang, J. Q. , & Chen, J. X. (2020). Sleep problems among Chinese adolescents and young adults during the coronavirus‐2019 pandemic. Sleep Medicine, 74, 39–47. 10.1016/j.sleep.2020.06.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Figure S1 Path analysis results for participants with missing data in COVID‐19 related worries
Data Availability Statement
The dataset and Mplus code are available on request from the corresponding author, Fulei Geng.


