FIGURE 4.
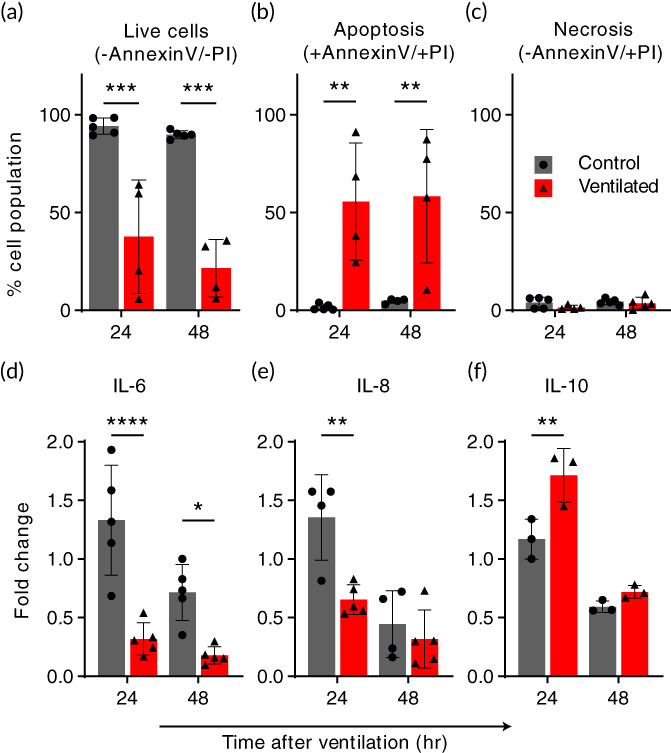
Ventilation exposure modulates apoptotic pathways and epithelial inflammatory cytokine secretions. Cells and culture medium were collected from models 24 and 48 h following ventilation exposure and compared with baseline levels. Air ventilation was performed for 4 h, or the ventilator machine kept off for the same duration as a control. Following the exposure, culture medium was filled back into the models. (a‐c) An increase in apoptotic cells indicates a biotraumatic response. Cells were collected from models and analyzed using flow cytometry (FACS) following Annexin‐V and Propidium Iodide (PI) staining. The % total population of (a) live cells decreased by 60% at 24 h and 75% at 48 h in the ventilated group relative to the control, which is largely unaffected at either time point. Most of this increase in nonviable cells is found in (b) the apoptotic, ventilated group while (c) negligible necrotic cells were counted for either exposure group. The increase in apoptosis was consistent in models analyzed both 24 and 48 h following the exposure experiment. (d‐f) Changes in the secretion of inflammatory cytokines following ventilation suggest a signaling pathway. Cytokines IL‐6 (d), IL‐8 (e), and IL‐10 (f) were measured in culture medium collected from the models after 24 and 48 h periods before and following simulated ventilation, respectively. Measurements from repeated experiments are plotted as normalized fold change to highlight signaling changes resulting from the test exposure. In (d) and (e), we measured a significant reduction in pro‐inflammatory IL‐6 (75% at both 24 and 48 h) and IL‐8 (50% at 24 h) relative to the control, while conversely in (f), we find that IL‐10, an anti‐inflammatory cytokine, is elevated >30% at the 24‐h time point compared with the control. All values are normalized relative to their baseline, that is, divided by pre‐exposure secretory levels. Cytokines were measured using ELISA. All graphs show mean (SD) values. *p < 0.05; ** p < 0.01; *** p < 0.001; ****p < 0.0001
