Figure 4. Mediators of inflammation in large vessel vasculitis.
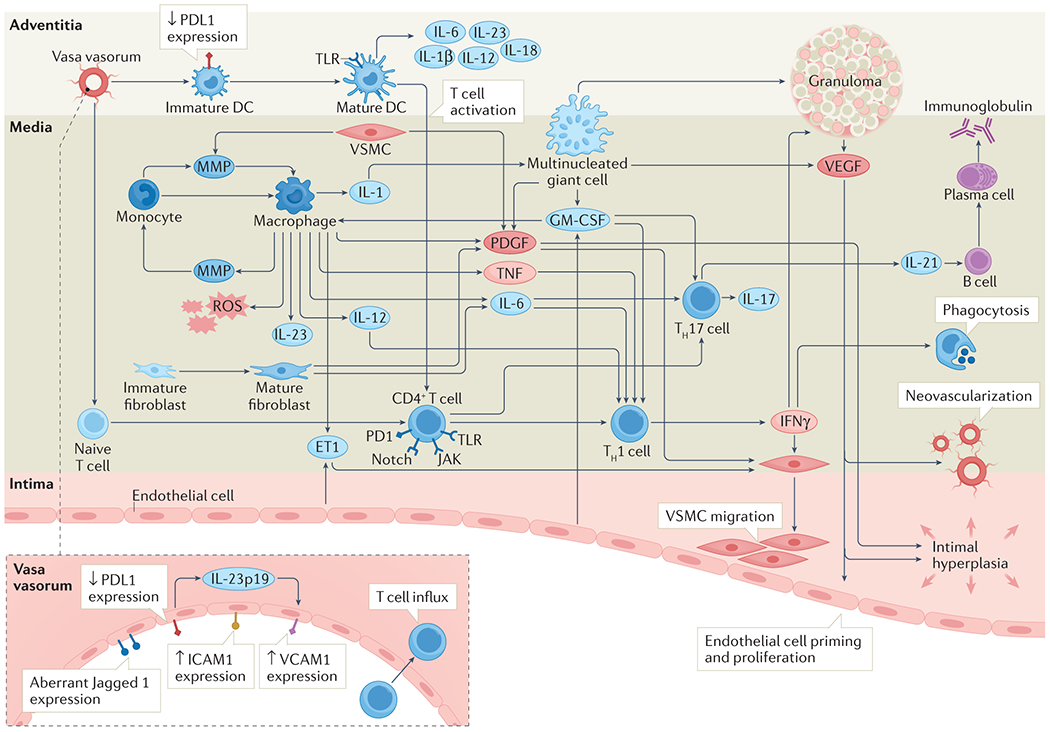
Once immune tolerance has been overcome, a cascade of pro-inflammatory mediators leads to progressive tissue damage. Stimulated dendritic cells act as instigators by recruiting and retaining pro-inflammatory cells including monocytes and T cells. Monocytes differentiate into macrophages which amplify inflammation through release of an assortment of effector molecules. Recruited T cells differentiate into Th1 cells and Th17 cells, further driving the inflammatory cascade through release of cytokines including IFN-γ (Th1) and IL-17/IL-21 (Th17). Vascular inflammation is propagated by neo-vascularisation within the vessel wall which sustains the inflammatory milieu and allows further influx of inflammatory cells. Ultimately, persistent inflammation and attempted remodelling lead to vessel wall damage including intimal hyperplasia and fibrosis, with clinical manifestations including arterial stenosis, occlusion and aneurysm formation.
DC, dendritic cell; EC, endothelial cell; ET-1, endothelin-1; GM-CSF, granulocyte macrophage colony stimulating factor; ICAM-1, intercellular adhesion molecule 1; 1IFN-γ, interferon-gamma; IL-, interleukin; JAK, Janus kinase; MMP, matrix metalloproteinase; PDGF, platelet derived growth factor; PD-1, programmed death-1; PD-L1, programmed death ligand-1; ROS, reactive oxygen species; TLR, toll-like receptor; TNF-α, tumour necrosis factor alpha; VCAM-1, vascular cell adhesion molecule 1; VSMC, vascular smooth muscle cell.
