Figure 5. Investigation and diagnosis of large vessel vasculitis.
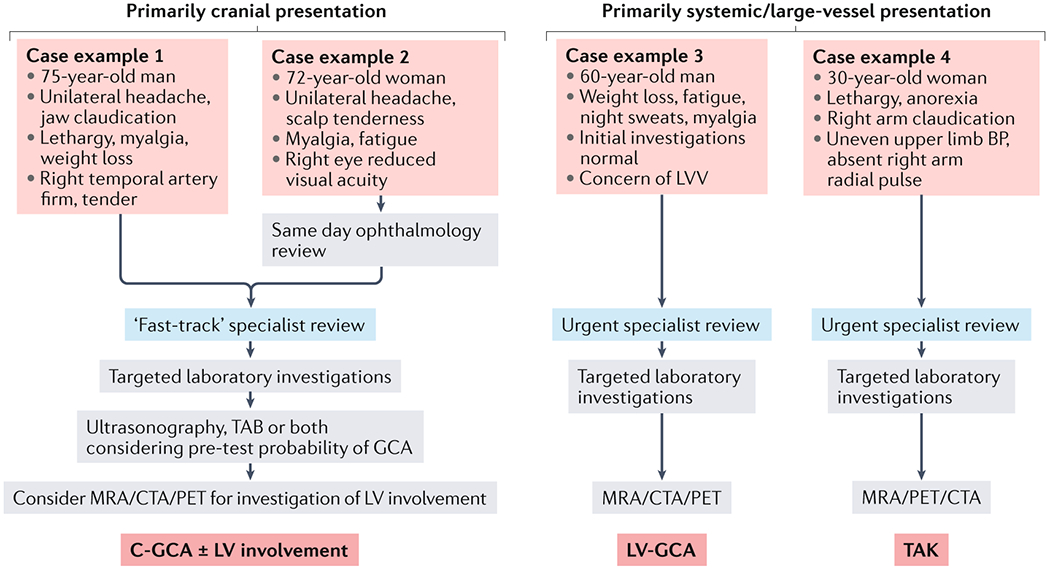
Schematic outlining a simplified approach to the investigation and diagnosis of different large vessel vasculitis (LVV) clinical syndromes. Typical features of cranial giant cell arteritis (C-GCA) (case examples 1 and 2) include headache and jaw and scalp pain, together with constitutional symptoms. Visual disturbance (case example 2) should prompt rapid ophthalmological review. The diagnostic approach to a patient with a primarily cranial presentation of LVV should consider the pre-test probability of C-GCA, which will inform whether ultrasonography or temporal arterial biopsy (TAB) is the most appropriate initial investigation116. Co-existing involvement of the aorta and associated great vessels should be considered in all patients with C-GCA. Case examples 3 and 4 depict more non-specific disease presentations typical of large vessel giant cell arteritis (LV-GCA) (case examples 3) and TAK (case examples 4). In these cases, imaging with either MRA, CTA and/or PET is required. BP, blood pressure; CTA, computed tomography angiogram; MRA, magnetic resonance angiogram; PET, positron emission tomography; TAK, Takayasu arteritis.
