Abstract
Endothelium, the gatekeeper of our blood vessels, is highly heterogeneous and a crucial physical barrier with the ability to produce vasoactive and protective mediators under physiological conditions. It regulates vascular tone, haemostasis, vascular inflammation, remodelling, and angiogenesis. Several cardio-, reno-, and cerebrovascular diseases begin with the dysfunction of endothelial cells, and more recently, COVID-19 was also associated with endothelial disease highlighting the need to monitor its function towards prevention and reduction of vascular dysfunction. Endothelial cells are an important therapeutic target in predictive, preventive, and personalised (3P) medicine with upmost importance in vascular diseases. The development of novel non-invasive techniques to access endothelial dysfunction for use in combination with existing clinical imaging modalities provides a feasible opportunity to reduce the burden of vascular disease.
This review summarises recent advances in the principles of endothelial function measurements. This article presents an overview of invasive and non-invasive techniques to determine vascular function and their major advantages and disadvantages. In addition, the article describes mechanisms underlying the regulation of vascular function and dysfunction and potential new biomarkers of endothelial damage. Recognising these biomarkers is fundamental towards a shift from reactive to 3P medicine in the vascular field. Identifying vascular dysfunction earlier with non-invasive or minimally invasive techniques adds value to predictive diagnostics and targeted prevention (primary, secondary, tertiary care). In addition, vascular dysfunction is a potential target for treatments tailored to the person.
Keywords: Vascular function and endothelium, Predictive preventive personalised medicine, Invasive and non-invasive techniques, Biomarkers, Individualised patient profile, Improved individual outcomes
Introduction
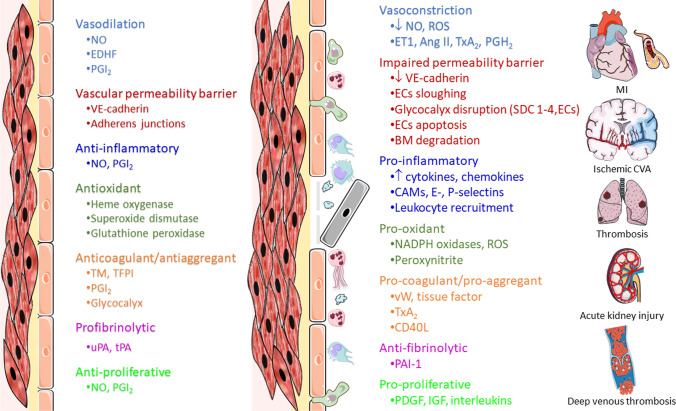
Predictive, preventive, and personalised (3P) medicine is increasingly important to reduce cardiovascular events and increase life expectation worldwide [1]. The endothelium comprises a monolayer of endothelial cells (ECs) facing the lumen of blood and lymphatic vessels. It has an extension of more than 1000m2 covering the vasculome. ECs display a marked phenotypic heterogeneity, with specific receptors, a transcriptome and different functions tailored to each region of the organism [2, 3]. Despite this diversity, key features typical of many ECs can be summarised in Fig. 1.
Fig. 1.

Various endothelial cells functional properties. VSMCs, vascular smooth muscle cells
Traditional and emergent risk factors for cardiovascular disease foster the damage of ECs monolayer conducting to endothelial cell activation and dysfunction (Fig. 2).
Fig. 2.
At left, some physiologic endothelial functions are summarised. In the middle, the main changes that occur when endothelium is activated and becomes dysfunctional leading to several cardiovascular diseases are illustrated. Ang II, angiotensin II; BM, basement membrane; CAMs, cellular adhesion molecules; CD40L, CD40 ligand; CVA, cerebrovascular accident; ECs, endothelial cells; EDHF, endothelial-derived hyperpolarizing factor; ET1, endothelin 1; IGF, insulin-like growth factor; MI, myocardial infarction; NADPH, nicotinamide adenine dinucleotide phosphate; NO, nitric oxide; PAI-1, plasminogen activator inhibitor 1; PDGF, platelet-derived growth factor; PGH2, prostaglandin H2; PGI2, prostacyclin; ROS, reactive oxygen species; SDC 1–4, syndecans 1–4; TFPI, tissue factor pathway inhibitor; TM, thrombomodulin; tPA, tissue plasminogen activator; TxA2, thromboxane A2; uPA, urokinase plasminogen activator; VE-cadherin, vascular endothelial cadherin; vW, von Willebrand factor
Pathophysiology of endothelium
Endothelial dysfunction has a major role in the initial phases and in the progression of several diseases as cardiovascular disease, some types of cancer and infection diseases as COVID-19 [4]. The aetiology is diverse and ranges from genetic, environmental, and metabolic factors [5].
Due to several risk factors, ECs became activated and reduce the production or availability of vasodilators in particular nitric oxide (NO) and increase the number of vasoconstrictors such as endothelin 1, angiotensin II, thromboxane A2 (TxA2), and prostaglandin (PGH2) in the vasculature [6]. The vascular permeability barrier becomes impaired with glycocalyx disruption [syndecans (SDC 1–4), endocan], the decrement in vascular endothelial-cadherin, ECs sloughing and apoptosis and basement membrane degradation [7–9]. The pro-oxidant (increased expression of nicotinamide adenine dinucleotide phosphate (NADPH) oxidase and reactive oxygen species (ROS)), pro-coagulant (von Willebrand factor, tissue factor, TxA2), and pro-inflammatory milieu enriched with cytokines, chemokines, cell adhesion molecules (CAMs, E- and P-selectins), and the leukocyte recruitment to the subintima region constitute the early stages of atherosclerosis and promote vascular dysfunction. A pro-proliferative state with increased levels of platelet-derived growth factor, insulin-like growth factor-1, interleukins (Fig. 2) can foster the increment of media layer leading to hypertension [6, 10].
In larger arteries, the major vasodilator in the vascular wall is NO while in smaller vessels, depending on the local, it is more heterogeneous (endothelial-derived hyperpolarizing factors or prostacyclin (PGI2) [10]).
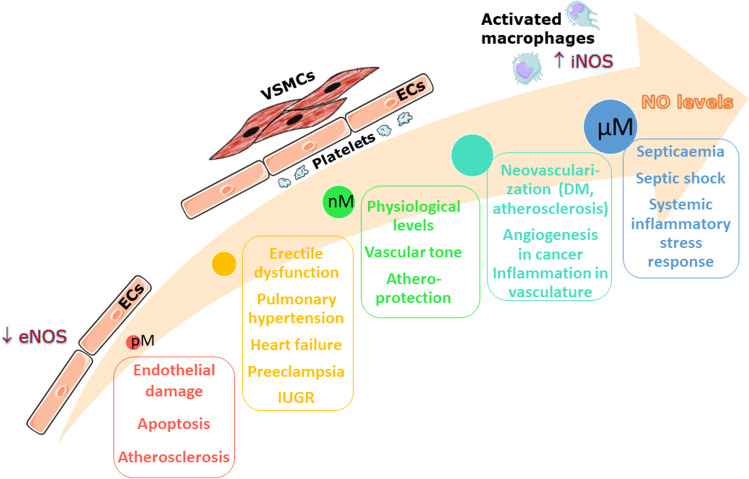
Under physiological conditions, NO is atheroprotective, a potent vasodilator, inhibits proliferation of vascular smooth muscle cells (VSMCs), platelet aggregation and reduces inflammation. In the vascular wall NO production in ECs, platelets, VSMCs, and activated macrophages is dependent on the activities of endothelial nitric oxide synthase (eNOS) and inducible NOS (iNOS). A reduction in NO bioavailability due to oxidative stress or/and eNOS uncoupling leads to atherosclerosis and other vascular abnormalities [6] (Fig. 3). Higher levels of NO, due to increased expression of iNOS in activated macrophages, are associated with inflammatory vascular responses and very high levels are related with infections, systemic inflammatory stress response, septicaemia, and lead to septic shock [11] (Fig. 3).
Fig. 3.
Physiological and pathological functions of nitric oxide. Nitric oxide (NO) plays a significant role in maintaining the optimum physiological function within the cardiovascular system. The levels of NO vary depending on the tissue and intracellular conditions, ranging from subpicomolar to micromolar concentrations. In endothelial cells (ECs), vascular smooth muscle cells and activated macrophages, endothelial nitric oxide synthase (eNOS), and inducible nitric oxide synthase (iNOS) enzyme activities contribute to maintain the fine balance of NO. At physiological levels, NO regulates the local vascular tone and is atheroprotective. A shift to both lower and higher concentrations of NO contribute to pathological conditions within the cardiovascular system. DM, diabetes mellitus; ECs, endothelial cells; eNOS, endothelial nitric oxide synthase; iNOS, inducible nitric oxide synthase; IUGR, intrauterine growth restriction; NO, nitric oxide; VSMCs, vascular smooth muscle cells
Vascular barrier impairment is common in various infectious or inflammatory diseases [12, 13]. In animal models, several compounds have been shown the ability to enhance endothelial barrier properties such as activated protein C, angiopoietins, anti-vascular endothelial growth factor, corticosteroids, histamine receptor blockades, protein kinase C inhibitors, RhoA inhibitors, sphingosine 1-phosphate, and vasopressin type 1a agonists [9, 14–17] although not all demonstrate clinical efficacy [18]. Novel therapeutic approaches and clinical trials are needed to unravel the key pathways to barrier structure and function in vascular diseases.
Importantly, the damaged endothelium can be repaired, mobilizing endothelial progenitor cells from bone marrow [19]. Endothelial dysfunction is reversible, and its early identification could help to prevent irreversible vascular disease and improve individual outcomes.
Assessment of endothelial function
Endothelial function determination is difficult due to its diversity and heterogeneity. Several techniques have been used to measure endothelial function based on the quantification of decreased endothelial-dependent vasodilation compared with endothelial-independent vasodilation (Fig. 4), in an invasive or non-invasive fashion. The most suitable technique should be non-invasive, safe, repeatable, reproducible, inexpensive, and standardised [5].
Fig. 4.
Scheme summarizing the basis to endothelial function evaluation (left panel) and the used of acetylcholine as a stimulus for endothelial cells (ECs, right panel) with subsequent nitric oxide (NO) production and relaxation in vascular smooth muscle cells. ECs, endothelial cells; M1, M3, muscarinic receptors; NO, nitric oxide; VSMCs, vascular smooth muscle cells
Invasive methods
Vascular function can be measured using invasive techniques involving the intra-arterial infusion of vasoactive substances that lead to increase NO release, promoting the dilation of the VSMCs (Fig. 4).
Quantitative coronary angiography with intracoronary infusion of vasoactive agents
One of the most accurate and reliable method to evaluate endothelium in coronary arteries is through the quantitative coronary angiography (QCA) with intracoronary infusion of vasoactive agents [20]. QCA remains the gold standard and most direct method for the functional evaluation of coronary arteries [21]. Measurement of vascular diameter changes in response to intracoronary infusion of vasoactive compounds is performed in addition with the evaluation of coronary blood flow, vascular resistance, and coronary flow reserve (typically after infusion of adenosine or stimulus such as pacing or exercise). More recently, several authors have developed three-dimensional (3D) QCA to overcome some of the limitations of two-dimensional (2D) QCA enabling a more accurate measurement of real vessel size due to the fusion of two angiographic views [22–24].
The advantage of this method is the evaluation of the coronary artery vascular bed through dose response curves to agonists and antagonists of ECs and the study of the basal endothelial function with infusion of eNOS antagonists. The major drawbacks are the invasive nature of the methodology, the costs, the risks associated with the catheterization of arteries (myocardial infraction, stroke, infection) impeding its use on a wide scale as a screening method of large asymptomatic populations [25].
Intravascular ultrasound
Intravascular ultrasound (IVUS) is a Doppler technique that in association with acetylcholine (ACh) or other vasoactive infusions can be used to evaluate coronary blood flow velocity using a Doppler-guided wire to obtain vessel measurements. IVUS provides a full assessment of lumen morphology and lesion severity when compared to visual estimation on 2D-QCA [26]. In contrast, 3D-QCA may be analogous to IVUS in recognizing functionally important coronary stenosis, as evaluated by fractional flow reserve [5, 23].
IVUS is excellent for the characterization of an atherosclerotic plaque (evaluates plaque burden and composition). The drawbacks of the method are associated with its invasive nature and limited availability, the need to use an iodinated contrast agent for catheter positioning, and does not evaluate the adventitia [27].
Venous occlusion plethysmography with intrabrachial infusion of vasoactive agents
Venous occlusion plethysmography (VOP) is a methodology used for more than a century to evaluate blood flow [28]. This method is suitable to study the endothelial function, the vasodilator response to different stimuli in both healthy and pathologic situations, and the regulation of blood flow by autonomic nervous system [29, 30].
The underlying principle of VOP is that during occlusion of venous return, the rate of forearm distension can be used to determine the rate of arterial blood flow. A cuff surrounding the arm (Fig. 5) is inflated applying a pressure lower than the diastolic pressure (i.e. 40 mmHg) for a short period of time (5–10 s), occluding venous return but unaffecting arterial inflow. The rate of forearm distension distally can be assessed measuring forearm circumference by a strain gauge. A lower cuff is placed around the wrist and inflated to suprasystolic pressure (i.e. 200 mmHg) just before the measurement to ensure that the circulation to the hand does not interfere with the results [31].
Fig. 5.
Several techniques to evaluate endothelial function. ED, endothelial dysfunction; FMD, flow-mediated dilation; NO, nitric oxide; PAT, peripheral arterial tonometry
This stimulus can be mechanical, promoting reactive hyperaemia, or chemical and invasive, through the administration of intra-arterial infusion of vasoactive substances. Endothelium-independent vasodilation is determined through the infusion of precursors of NO, such as sodium nitroprusside. This method measures blood flow, not arterial diameter, depends on conditions at baseline and lacks standardization between laboratories. Despite these limitations, VOP using intra-arterial infusion of vasoactive compounds is regarded the gold standard for the evaluation of vascular function [32].
An advantage of this method is that the brachial artery is more accessible and easier to cannulate. Despite the need for arterial cannulation, it provides useful and reproducible surrogate measures in a less invasive manner than 3D-QCA enabling dose response curves to agonists and antagonists of ECs and the study of the basal endothelial function with infusion of antagonists of eNOS. The major drawbacks are the invasive nature of the methodology, the risks associated with the catheterization of the artery, the possibility of damage or injection of median nerve, and the variability due to several individual subject characteristics making it unsuitable for large clinical trials and requiring repetitive measurements.
Functional studies ex vivo
Functional assessment of endothelial function has been available for several decades in organ bath systems and myographic recordings enabling the detection of the endothelium-dependent and endothelium-independent relaxation of arterial rings, in response to known agonists such as ACh and sodium nitroprusside, respectively [33]. Endothelial-derived vasodilators include NO and PGI2 are produced in response to several agonists of ECs enabling the functional evaluation of endothelium [34].
Isolated organ bath is an ex vivo method that evaluates vascular reactivity of biological preparations creating dose–response curves to agonists and antagonists to study the physiological and pharmacological responses of ECs, VSMCs, and others. Tissues and organs typically studied include rings of arteries, veins, intestine (duodenum, jejunum, and ileum), or strips of atrium, ventricle, or papillary muscle, among others. The evaluation of these samples in the appropriate physiological environment (nutrient solution, controlled temperature, aeration) enables its characterization through cumulative doses of vasoactive agents or electrical stimulation (the organ is fixed between two platinum electrodes connected to an electrical stimulator), which result in the contraction or relaxation of the muscle under evaluation. From the experimental results, dose–response curves are generated, and endothelial dependent and independent evaluation is performed [33–36].
Advantages of this technique include the evaluation of multiple preparations in simultaneous, an accurate control of the experimentation conditions as well as a precise quantification of the responses. In addition, it enables isolating components of endothelial function pharmacologically (for instance, using inhibitors of the eNOS enzyme). A major drawback of this method is that its use is generally limited to animal experiments, due to ethical considerations that restrain the availability and quantity of human samples and the variability of responses in patients. In human studies, sampling is often opportunistic or from subcutaneous fat [37, 38]. Another disadvantage is the inability to evaluate vessels with smaller diameters (< 60 mm). Being the most widely used method for the study of endothelial function in animal models, it has the limitation of not distinguishing the biological events that occur in the lumen and outside the blood vessel, not studying the impact of perivascular tissues usually removed in these studies [39].
Non-invasive methods
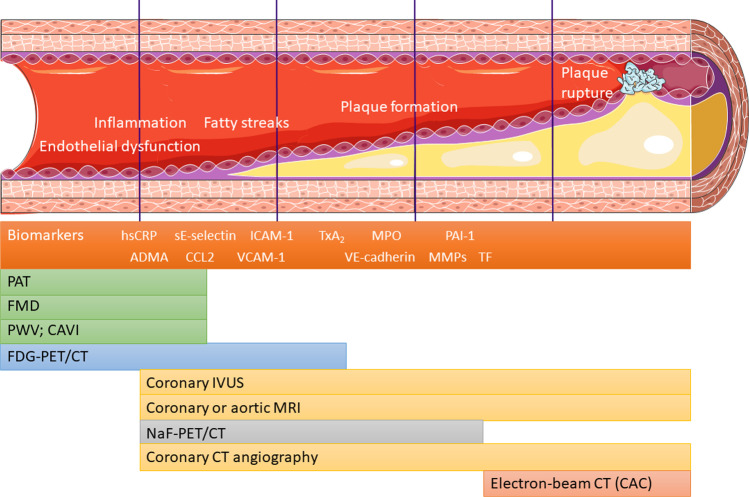
The development and utilization of non-invasive methods is always preferred to evaluate vascular function [40]. Most imaging techniques are non-invasive and provide the structural evaluation of blood vessels given no indication about their function. In the last decade, major technologic advances enabled the detection of early atherosclerosis with these techniques as carotid intima-media thickness (cIMT), computed tomography (CT) angiography, IVUS, and 18-fluorodeoxyglucose positron emission tomography (FDG-PET). The latter associated with CT imaging can detect and localize the increased metabolic uptake of radiolabelled glucose. FDG-PET signal is increased in early atherosclerotic process and when endothelial inflammation occurs (Fig. 6) [27, 41].
Fig. 6.
The progression of atherosclerosis accompanied by different imaging modalities capable of monitoring the events. In this figure, it is represented the beginning of the atherosclerotic process starting with endothelial dysfunction, followed by an increment in the expression of cellular adhesion molecules that response to hypertension or dyslipidaemia with monocyte recruitment. The monocytes can incorporate lipids and become foam cells. In addition, smooth muscle cells migrate from the media into the intima, producing elastin and collagen that forms the fibrous cap. Plaque growth can downgrade blood flow to distal regions, leading to peripheral arterial disease or stable angina. Otherwise, erosion of the fibrous cap can uncover its prothrombotic content, causing clot formation and infarction, either in the brain or the myocardium. Imaging modalities for the various stages should be chosen in accordance with the physiological modifications anticipated to a given stage of the process. ADMA, asymmetric dimethylarginine; CAC, coronary artery calcium; CAVI, cardio-ankle vascular index; CCL2, CC-chemokine ligand 2; CT, computed tomography; FDG-PET, 18-fluorodeoxyglucose positron emission tomography; FMD, flow-mediated dilatation; hsCRP, high sensitive C-reactive protein; ICAM-1, intercellular adhesion molecule 1; IVUS, intravascular ultrasound; MMPs, metalloproteinases; MPO, myeloperoxidase; MRI, magnetic resonance imaging; NaF-PET, sodium fluoride positron emission tomography; PAI-1, plasminogen activator inhibitor 1; PAT, peripheral arterial tonometry, detects changes in small arteries; PWV, pulse wave velocity, monitors arterial stiffness and integrity of tunica media; sE-selectin, soluble E-selectin; TF, tissue factor; TxA2, thromboxane A2; VE-cadherin, vascular endothelial cadherin; VCAM-1, soluble vascular cellular adhesion molecule 1
Assessment of carotid intima-media thickness
Ultrasound image of the common carotid artery obtained with an echocardiograph using a 12L linear probe is the most validated imaging biomarker for prediction of atherosclerotic risk and follows specific international guidelines [42–44]. For this examination, participants are placed in the supine position, with the neck slightly hyperextended and rotated away from the transducer. In the two-dimensional images obtained from the neck vessels, the distal common carotid artery should be capture along its longitudinal path to the carotid bifurcation. The cIMT is typically measured on the posterior wall, at a distance of at least 5 mm from the bifurcation. The arterial segment under analysis must have the lumen/intima and media/adventitia interfaces clearly visible, along a length of at least 1 cm. The evaluation is carried out in telediastole, coinciding with the R wave of the electrocardiogram tracing. A semi-automatic image processing method performed at least 50 to 60 measurements of the cIMT on the selected segment, then presenting a final value that corresponded to the average of the measurements performed [45, 46].
A large meta-analysis with 37,197 patients showed that for every 0.1 mm increase in cIMT adjusted risk of future myocardial infraction or stroke enhances by approximately 10% and 13%, respectively [47]. Studies in paediatric age confirm the existence of a pro-atherosclerotic environment correlated with the increase in carotid intima-media thickness [46, 48].
The main advantages are the relative simplicity, accuracy, and reproducibility. Indeed, cIMT provides a non-invasive reliable tool for evaluating vessel wall structural modification at the macrovascular level. One disadvantage is that is operator dependent, and it does not measure adventitial thickness, an important contributor for atherosclerotic development [49].
Flow-mediated dilation
Flow-mediated dilation (FMD) is a non-invasive method that enables the determination of endothelial dysfunction in the brachial artery in response to reactive hyperaemia [40]. A pneumatic cuff placed at the upper arm or wrist occludes (200–250 mmHg) arterial flow for 5 min, followed by rapid cuff deflation that induces reactive hyperaemia leading to shear stress and subsequent release of vasodilators as NO and PGI2 [29, 50]. Classically, an ultrasonography system equipped with a high-resolution linear artery transducer (7.5–12 MHz) is used for the measurement of brachial artery diameter (monitoring baseline measurements, at rest, and during reactive hyperaemia). In response to a transient physiologic stimulus (increase in blood flow), vasodilators are released and arteries, including brachial artery dilate and increase in diameter (Figs. 5 and 7). The FMD is the percent increment of the diameter value of the artery with respect to the baseline. FMD is calculated as FMD = (peak diameter—baseline diameter)/baseline diameter. Intraarterial infusion of eNOS inhibitors (i.e. Ng-mono-methyl-L-arginine) clearly showed that this process is dependent on the release of NO from the endothelium. Endothelium-independent vasodilation is assessed through sublingual administration of sodium nitroprusside or nitroglycerin [51].
Fig. 7.
Flow-mediated dilation procedures. NO, nitric oxide
Impaired FMD is an important tool to detect endothelial dysfunction and has the potential to predict and identify risk factors for cardiovascular events, even in asymptomatic patients [52]. In addition, FMD enables stratification of individuals for upcoming cardiometabolic events, and impaired FMD has long-term prognostic value in cardiovascular patients [53, 54].
FMD is a gold-standard method, extensively validated that strongly correlates with coronary artery function. Moreover, there are several disadvantages associated with FMD. First, the lack of standardization and variations in the placement of cuffs in the wrists/arms and in vessel diameters make it difficult to compare the results between laboratories. In addition, alterations in blood vessel structures and impaired dilation can act as limiting factors. The lack of resolution compared with the relative size of the artery, the inter-measurement variability, the poor reproducibility, and the operator dependence are the main disadvantages of this methodology. It is imperative that well-trained and experienced operators perform the technique in addition with several precautions to obtain more accurate results. Indeed, strict recommendations must be considered to reduce the variability associated with this methodology (Table 1) [55].
Table 1.
There are several conditions that need to be performed to obtain a significant decrease in variability in studies with flow-mediated dilation
| - Evaluations should be performed with the subject fasting for at least 6 h |
|---|
| - Tests with repeated evaluations must be done on the same day |
| - Vasoactive medication (when possible) must be avoided (4 half-lives before the measurements) and the results evaluated accordingly |
| - Anti-inflammatory medication such as NSAIDs must be withdrawn 1 and 3 days before |
| - Abstinence of physical activity at least 12 h before the test |
| - Caffeine and other stimulatory drugs must be avoided 12 h before the examination |
| - No smoking or exposition to cigarette smoke at least 12 h before the test |
| - Vitamin supplementation must be withdrawn at least 72 h before the examination |
| - Women in fertile phase must be evaluated in the follicular phase of the menstrual cycle |
| - The measurements must be performed in a calm environment, with a room temperature between 20 and 25 °C |
NSAIDs Non-steroid anti-inflammatory drugs
More recently, a novel approach, based in an oscillometric method, was used to quantify flow-mediated dilation–enclosed zone FMD (ezFMD) [56]. Blood pressure can be measured by an oscillometric method using and automatic instrument and in simultaneous oscillation amplitude can also be quantified. There is a proportional relation between oscillation amplitude and volumetric change with pulse pressure in brachial artery. The change in peak oscillation amplitude after a 5-min occlusion of the artery reflects a volume change instigated by reactive hyperaemia. Classic FMD is based in changes in vascular diameter determined by ultrasonography, whereas ezFMD is based in changes in vessel volume indirectly determined by oscillation amplitude. ezFMD = (peak amplitude–baseline amplitude)/baseline amplitude. ezFMD is an operator independent method, automatically performed after the placement of a blood pressure cuff around the upper arm [56, 57].
Arterial stiffness
Pulse wave velocity
Arterial stiffness is an independent biomarker of cardiovascular disease. It is associated with modification in functional (regulation of vascular tone due to contraction/relaxation of VSMCs) and structural (elastin, collagen fibres, extracellular matrix components) properties of the arteries. Several methods have been used to measure arterial stiffness, non-invasively: (1) vascular imaging techniques, such as ultrasound and magnetic resonance imaging (MRI) allowing the measurement of arterial compliance with sonographic stiffness indices (i.e., augmentation index) and (2) recording of the pulse wave by tonometry or ultrasound Doppler. After left ventricular contraction, a pressure wave is generated travelling along the arterial tree. The velocity of this wave is called pulse wave velocity (PWV) and reflects the rigidity of the arteries. PWV is calculated by dividing the travelled distance by expended time [58, 59]. The lower the PWV, the more elastic and healthier the vessel is. However, when the vessel has a high level of rigidity, there is an increase in the propagation of pulse waves in the aorta artery and great vessels, in addition to causing an early return of pulse waves reflected from the periphery [60]. The pulse wave is normally reflected at any point of discontinuity in the arterial tree, causing a retrograde wave in the ascending aorta. This early return, even at the end of systole, promotes an overload in cardiac work [61].
Age, hypertension, diabetes, increased homocysteine levels, and diastolic dysfunction are associated with arterial stiffness [62, 63]. Impaired homocysteine metabolism, recently recognised as a target in 3P medicine [64], may lead to an increment in homocysteine levels, fostering vascular dysfunction.
Carotid-femoral PWV (cfPWV) is the gold standard, non-invasive assessment for arterial stiffness [65–67]. The evaluation is done with the individual in supine position, and two transducers are positioned, one in the right common carotid artery and the other in the right femoral artery. PWV is calculated by dividing the distance between the transducers and the difference in time between the onset of the carotid pulse wave and the onset of the femoral pulse wave [66, 68]. The method is reproducible but the accuracy of recording the pulse waveform is not reliable in patients with atrial fibrillation or peripheral artery disease [69].
The major drawback of PWV is that is strongly influenced by blood pressure and, to a lesser extent, by heart rate.
Cardio-ankle vascular index
Cardio-ankle vascular index (CAVI) reflects the general stiffness of elastic and muscular arteries from the beginning of the aorta to the ankle. It delivers operator-independent information regarding changes in structural and functional arteriosclerotic processes. CAVI is less influenced by short-term blood pressure changes compared with PWV and a mathematical correction can further improve this limitation [70].
Peripheral arterial tonometry
Reactive hyperaemia peripheral artery tonometry (RH-PAT) is a non-invasive technique that combines flow-mediated dilation with disposable pneumatic finger-tip probes to measure arterial pulse wave amplitude and obtain the reactive hyperaemia index that reflects microvascular endothelial function [71, 72] (Fig. 5).
Shortly, the individuals are placed in a supine and comfortable position with the hands at the level of the heart. Disposable modified pneumatic probes on the index fingers record pulse wave amplitudes. After baseline measurement, arterial flow to the arm is occluded for 5 min using a blood pressure cuff inflated to 40 mmHg above systolic pressure. At the end, the cuff is rapidly deflated, and a transient increment in blood flow occurs. The ratio between the post- and pre-occlusion pulse wave amplitude values is used to calculate the RH-PAT index. The value is normalised using the data from the opposite finger to correct for modifications in systemic vascular tone [72].
RH-PAT and FMD evaluate distinct aspects of vascular function (Table 2, Fig. 7), and most studies do not show a correlation between these methodologies and defend a more complementary association [73–75]. Several studies describe that RH-PAT correlates with coronary microvascular function, predicts cardiovascular events, and is associated with classic cardiometabolic risk factors [76–79]. Noteworthy, digital microvessel dilatation during hyperaemia is only partially dependent on NO bioavailability [80], functioning as a biomarker of peripheral microvascular capacity. More recently, PAT was described to be a predictor of stroke incidence. RH-PAT index may suggest early subclinical cerebrovascular remodelling and damage, atherosclerosis, or autonomic nervous system abnormalities [81].
Table 2.
Comparison between several non-invasive vascular tests: FMD, RH-PAT, and PWV
| Vascular test | FMD | RH-PAT | cfPWV | baPWV |
|---|---|---|---|---|
| Vascular layer evaluated | Endothelium | Media | ||
| Vascular bed | Brachial artery | Finger arterioles | Aorta | Aorto-muscular |
| Parameter | Endothelial function | Arterial stiffness | ||
baPWV, brachial-ankle pulse wave velocity; cfPWV, carotid-femoral pulse wave velocity; FMD, flow-mediated dilation; RH-PAT, reactive hyperaemia peripheral arterial tonometry
RH-PAT is a non-invasive, safe, and rapid, operator independent technique that can reflect basal endothelial function. The main disadvantages are the sensitivity to the autonomic tone, the prognosis value, the low reproducibility, the lack of correlation with FMD, and the influence of structural vascular aspects (Table 3) [82, 83].
Table 3.
Advantages and disadvantages of different endothelial dysfunction assessment techniques
| Method | Advantages | Disadvantages |
|---|---|---|
| Quantitative coronary angiography |
• Directly quantifies endothelial function in the vascular bed of interest • Allows to establish the relationship between agonists and antagonists • Allows to examine basal endothelial function after administration of NOS antagonists |
• Invasive • Expensive • Risks related to coronary artery catheterization: stroke, MI, infection |
| Venous occlusion plethysmography |
• More accessible • High reproducibility, validity • Allows to establish the relationship between agonists and antagonists • Allows to examine basal endothelial function after administration of NOS antagonists |
• Semi-Invasive • Indirect measure of blood flow • Time consuming • Limited applications in exercise • Risks: median nerve injury, infections, vascular injury |
| Doppler ultrasound |
• Non-invasive • Possible to measure blood flow velocity Continuous wave Doppler • Simpler hardware implementation • Ability to measure high blood flow velocity • Wide depth range Pulse wave Doppler • Measurement range definition |
• Precise positioning over a large blood vessel at an appropriate angle • Expensive • Contact gel Continuous wave Doppler • Measurement range ambiguity Pulse wave Doppler • For use by qualified personnel only • “Aliasing” artefacts at high blood flow velocities • Measurement depth limitations |
| Arterial tonometry |
• Non-invasive • Safe and rapid • Less operator dependent than FMD • Accurately records the arterial blood pressure waveform • Can reflect basal endothelial function |
• Influenced by structural vascular aspects and less by the endothelium • Sensitivity to the autonomic tone • Temperature dependent • Requires clipping of long fingernails • Movement artefacts |
| Flow-mediated dilation |
• Non-invasive • Safe, rapid • Well correlated with coronary endothelial function • Blood flow is a physiological stimulus of vasodilation, like agonists • Gold-standard method |
• Low resolution influenced by the vessel size • Inter-measurement variability • Operator dependence • Poor reproducibility • Lack of strict protocols |
| Intravascular ultrasound | • Excellent for evaluation of plaque burden and composition |
• Invasive • Limited availability • Iodinated contrast agent required (for catheter positioning) |
FMD, Flow-mediated dilation; MI, myocardial infarction; NOS, nitric oxide synthase
Microvascular endothelial function assessment
The endothelial function in microvascular blood vessels can also be evaluated noninvasively by different methodologies with direct and indirect approaches (Table 4) [84].
Table 4.
Advantages and disadvantages of different microvascular endothelial function assessment techniques
| Method | Advantages | Disadvantages |
|---|---|---|
| Arterial glycocalyx |
• Tracer dilution method: direct measure • OPS + SDF: simple, non-invasive, bedside performance |
• Tracer dilution method: invasive and time-consuming • OPS + SDF: indirect measures |
| Near-infrared spectroscopy |
• Non-invasive, portable • Tissue oxygen consumption measurement • Recordings during exercise |
• Affected by adipose tissue thickness • Myoglobin may interfere |
| Laser Doppler flowmetry |
• Simple, non-invasive • Continuous blood flow measurement during exercise • Coupling with reactivity tests |
• Expensive equipment • Requires experienced operator for high accuracy and low variability over time • Susceptible to changes in autonomic nervous system and vasomotor tone • Temperature dependent |
| Laser speckle contrast analysis |
• Simple, non-invasive • Real-time recording of blood flow changes |
• Expensive equipment • Requires experienced operator for high accuracy and low variability over time • Movement artefacts • No recordings in absolute flow units |
OPS, orthogonal polarization spectral; SDF, sidestream darkfield
Direct methods enable the observation of the vessels (e.g. shallow capillaries, arterioles, and venules in skin, sublingual mucosa, bulbar conjunctiva, and in the retina) using microscopy in combination with photo/video recording. More recently, optical coherence tomography imaging has been introduced into the microvascular research to visualize microvessels in the skin or capillaries in the retina [85–89]. Obtaining and analysing large datasets of microvascular measurements is challenging and time consuming [90]. For some measurements, (semi-)automated applications have been developed to analyse images improving reproducibility, saving time and being user independent. Computer-assisted analyses of microvascular datasets including machine learning, and deep learning [91, 92] are proving its value in epidemiological research and clinical trials, an example already established is the retinal dynamic vessel analyzer [93–95].
Indirect methods enable the specific characterization of function in small blood vessels. In animal models, in vivo, intravital microscopy is the most frequent and reliable approach. This technique monitors vascular dynamic events such as vascular permeability and tonus, blood flow [96], or the arterial glycocalyx [97–99]. Evaluation of dynamic functions include for instance blood flow/perfusion measurements using laser-Doppler flowmetry (LDF; skin) or plethysmography (skin and muscle), blood oxygenation and hemodynamic measurements using near-infrared spectroscopy (brain, muscle, skin) [100, 101], transcutaneous oxygen pressure determinations (tcpO2; skin), and tissue microvascular blood flow and blood volume measurements using contrast-enhanced ultrasonography (adipose tissue, muscle, kidney, liver, heart) [102]. The last method is invasive since it involves the infusion of a contrast agent. The other techniques use non-invasive assessment of microvasculature. In addition, RH-PAT (discussed above) also reflects microvascular endothelial function [103].
Other methodologies that indirectly monitor microvascular function include measuring microalbuminuria [33, 104]; determining biomarkers of acute kidney damage [105]; measuring skin mottling over the anterior surface of the knee [101]; measuring protein concentrations in alveolar fluid lavage; and haemostasis-related biomarkers (von Willebrand factor, factor VIII, partial thromboplastin time, international normalised ratio, and platelet count) [106].
Different stimuli may be used to evaluate dynamically the microvasculature. For instance, flicker light exposure promotes reactive hyperaemia in the retinal microvessels. This response implicates neurovascular coupling and is partially mediated by endothelial NO production [107]. In skin, reactive hyperaemia can be induced during local skin heating or after ischaemia promoted by arterial occlusion and evaluated with laser Doppler–based techniques (see the “Laser Doppler flowmetry” section). These responses are dependent on endothelial vasorelaxant factors (e.g., NO, endothelial derived hyperpolarizing factor, prostaglandins) [108]. Systemic or local infusion of vasoactive substances, or via iontophoresis, can stimulate ECs (e.g. acetylcholine,) or VSMCs (e.g. sodium nitroprusside). The following outcomes (vasodilation/constriction and augmented/reduced perfusion) can be observed with different methodologies. Some devices can even combine several techniques like LDF and tcpO2 [109] or charge-coupled device and laser speckle contrast imaging [108].
Noteworthy, it is vital to recall that the phenotype of the endothelium is heterogeneous along the vascular tree [3]. The endothelium exhibits different responses to stimuli producing different vasoactive substances depending on the location (i.e., venules or arterioles of different size). Therefore, the results obtained in microvascular function are difficult to compare since they measure different vessel types within the microcirculation or evaluate distinct areas. Obtaining and combining information from different areas may be important and complementary, for instance, improving the diagnosis of a disease [110].
Moreover, the control of microvascular function varies considerably among different tissues, depending on their function, and nourishing requirements. The retinal microcirculation does not possess sympathetic innervation, and the brain and kidney microvasculature typically display low impedance in contrast to that of skin or muscle [111]. All these details need to be considered when determining and analysing microvascular function.
Arterial glycocalyx
One of the diagnostic methods to evaluate endothelial function is grounded on the measurement of the glycocalyx integrity and thickness by intravital microscopy or by orthogonal polarization spectral (OPS) imaging [112].
Intravital microscopy using sidestream darkfield (SDF) imaging is a non-invasive method utilised to analyse the sublingual microcirculation. The technique monitors red blood cells within the microvasculature when light emitted by a diode probe is reflected by haemoglobin and monitored by a SDF camera [113]. Total vessel density, perfused vessel density, proportion of perfused vessels, and microvascular flow index are predicted, and more recently using validated automatic software platforms, the operator-dependent limitations are minimised [114]. SDF imaging detection of red blood cells is used as a marker of microvascular perfusion, and measurement of the distance between the endothelium and red blood cells in circulation represents the thickness or dimension of the glycocalyx that correlates with levels of classical cardiovascular risk biomarkers such as blood glucose, low-density lipoprotein (LDL), high-density lipoprotein, and body mass index.
Multiple studies have shown, in critically ill patients, sublingual microvascular glycocalyx impairment [115–118]. The exactness of in vivo glycocalyx determination has been analysed further with an in vitro approach using atomic force microscopy [118, 119]. Consensus European Society of Intensive Care Medicine guidelines released recommendations for acquisition and interpretation of microcirculatory images obtained with hand-held vital microscopes for assessment of the microcirculation in critically ill patients [97].
Arterial glycocalyx can be evaluated using direct measurement with dilution tracers, but they are invasive and time-consuming methods. OPS and SDF are simple, non-invasive, bedside performance, indirect methods to measure arterial glycocalyx [120].
Laser Doppler flowmetry
Laser Doppler flowmetry is an excellent non-invasive technique to evaluate skin microvasculature function after a stimulus [121, 122]. It is based on diffusion and refraction of a laser beam light through moving blood cells related with the concentration and velocity of measured [108]. LDF determines modifications in the skin microcirculation in real time after stimuli, such as post-occlusion reactive hyperaemia, the infusion of vasoactive substances or the iontophoresis of small, charged molecules. For instance, intradermal administration of ACh by iontophoresis induces endothelium-dependent dilatation that, in association with LDF, enables quantification of the regional blood flow [123]. Microvascular reactivity obtained with LDF proved to be an impartial predictor of atherosclerotic disease in diabetic conditions [124].
LDF is a relatively simple, non-invasive method that monitors continuous blood flow measurement during exercise and can be coupled with reactivity tests. It has good accuracy for quantifying rapid modifications in cutaneous blood flow. Tough, the characteristic heterogeneity of this tissue, due to differences in its anatomy, promotes spatial variability that contributes to a relatively low reproducibility [122, 125]. The use of integrated probes helps to reduce spatial variability enabling to increase the reproducibility [108]. Another advantage of this technique, when coupled with intradermal infusion, is the safety, given the small amount of drug infused. The main limitations involve an equipment very expensive requirement of an experienced operator for high accuracy and low variability over time. In addition, it is an indirect method unable to determine the local blood flow, but it provides an index of skin perfusion [120].
Laser speckle contrast analysis
Laser speckle contrast analysis is a novel, fast, non-invasive technique that enables continuous measurement of skin blood flow. The main principle relies on the backscattered light from a tissue lit with laser light creates a random interference pattern on the detector (i.e. ‘speckle pattern’). This method can be combined with reactivity tests such as local thermal hyperaemia, and post-occlusive reactive hyperaemia enhancing reproducibility when compared with the LDF [126]. The method has been performed to evaluate distinct vascular beds [127, 128] in patients with type 1 diabetes mellitus [129], chronic kidney disease [130], and coronary artery disease [131]. Laser speckle contrast analysis is a simple, non-invasive real-time recording of blood flow changes. The equipment is expensive and requires experienced operators for high accuracy and low variability over time. It is sensitive to movement artefacts, and no records in absolute flow units can be obtained [132].
Index of microvascular resistance in coronary arteries
The index of microvascular resistance (IMR), the product of hyperaemic distal coronary pressure and hyperaemic transit time, is currently thought the standard of microvascular (dys)function. IMR has been shown to be specific for microvascular function [133] and has been correlated to outcome. However, it is an invasive method that depends on the injection technique of the operator (adenosine-induced hyperaemia is obligatory for both coronary flow reserve or coronary flow velocity reserve and IMR).
Recently, Konst and co-workers [134] performed an invasive investigational protocol with acetylcholine testing (for endothelium-dependent epicardial microvascular spasm), adenosine testing (for endothelium independent dysfunction), and measurement of absolute coronary blood flow and microvascular resistance as an innovative method for quantitative assessment of microvascular disease in patients with suspects of ischaemia with nonobstructive coronary arteries [135] and used fractional flow reserve testing to evaluate functionally epicardial disease. Absolute flow and resistance measurement, in the study by Konst et al. [134], does not require pharmacological stimuli since the saline infusion itself induces a maximum hyperaemia very rapidly. In contrast to coronary flow reserve or coronary flow velocity reserve and IMR, it is completely operator independent [135, 136]. Thus, evaluations of absolute flow and resistance are predictable to be of complementary importance to IMR.
Near-infrared spectroscopy
Near-infrared spectroscopy (NIRS) is a novel, non-invasive method that determines local tissue oxygenation providing crucial information about tissue oxygen consumption and blood flow [120]. A portable device produces near-infrared light irradiating the examined tissue and detecting and measuring changes in absorbance of oxygen carrier compounds (i.e. haemoglobin and myoglobin) based on their oxygenation state [137]. The ‘modified Beer-Lamberts law’ is the basis for this methodology [137] that allows the evaluation of microvascular reactivity and skeletal muscle oxygenation at rest and during exercise, via non-stop recording of functional alterations in oxygenated haemoglobin dissociation [138]. Moreover, using post-occlusion reactive hyperaemia, NIRS provides information on microvascular function and muscle’s oxidative capacity and oxygenation, both at rest and during exercise [138].
The main advantages of NIRS are that is a portable, non-invasive technique and measures the tissue oxygen consumption, at rest and during exercise. The major drawbacks are that the measurements are affected by adipose tissue thickness and myoglobin content [137].
Biomarkers
The application of serum biomarkers to monitor endothelial function has countless advantages given the relative simplicity of the procedures. Indeed, venous blood samples are commonly used in clinical laboratories and could be an accessible way to measure systemic biomarkers of vascular disease. The use of these biological markers (Fig. 8, Table 5) to assess the prognosis and/or diagnosis of vascular disorders is continuously growing due to its clinical relevance [106, 139, 140]. Identifying biomarkers is fundamental towards the shift from reactive to 3P medicine in the vascular field helping to obtain an individualised patient profile and improve individual outcomes.
Fig. 8.

Systemic endothelial dysfunction biomarkers. ADMA, asymmetric dimethylarginine; ED, endothelial dysfunction; EMP, Endothelial microparticles; EPCs, Endothelial progenitor cells; sICAM-1, soluble intercellular adhesion molecule 1; sVCAM-1, soluble vascular cellular adhesion molecule 1
Table 5.
Summary of the most frequent circulating biomarkers to monitor endothelial dysfunction in human studies
| Method | Characteristics | Advantages | Disadvantages |
|---|---|---|---|
| Serum markers | Blood drawn | ||
| NOS inhibitors | |||
| ADMA, SDMA | Competitive inhibitor of NOS | Some prospective clinical data | Not widely available |
| Inflammatory biomarkers | |||
| ET1 | Proinflammatory peptide | Some prospective clinical data | Not widely available |
|
hsCRP, IL-6, IL-8, IL-1β, TNF-α, CCL2, TWEAK, PTX3, CD40L |
Inflammatory biomarkers | Widely available; many data in CVD and ED | May be high in inflammation/infection |
| Cell adhesion molecules | |||
| sICAM-1, sVCAM-1, sE-selectin, sP-selectin | Adhesion molecules | Some prospective clinical data |
Not widely available Expensive |
| Coagulation pathway molecules | |||
| vWF, tPA, PAI-1, TM, fibrinogen, ADAMTS13 | Thromboembolic markers | vWF is widely available | Not a lot of data on ED |
| Glycocalyx damage | |||
| Endocan, syndecan 1; | Endothelial glycocalyx | Not widely available | |
| Oxidative stress | |||
| MPO | Activated neutrophils and macrophages increment MPO and increase ROS | Biomarker of oxidative stress | Not widely available |
| oxLDL | |||
| Cellular markers | |||
| cEPCs | Circulating endothelial progenitor cells promoting vasculogenesis | Good correlation with CAD and ED | Expensive, not widely available |
| CEC, EMP | Good correlation with CAD and ED | Not widely available | |
ADMA, asymmetric dimethylarginine; CAD, coronary artery disease; CCL2, CC-chemokine ligand 2; CEC, circulating endothelial cells; cEPCs, endothelial progenitor cells; CVD, cardiovascular disease; ED, endothelial dysfunction; EMP, endothelial microparticles; ET1, endothelin 1; hsCRP, high sensitive C-reactive protein; IL-1β, interleukin 1β, IL-6, interleukin-6, IL-8, interleukin-8, MPO, myeloperoxidase; NOS, nitric oxide synthase; oxLDL, oxidized low-density lipoprotein; PAI-1, plasminogen activator inhibitor 1; PTX3, pentraxin 3; SDMA, symmetric dimethylarginine; sE-selectin, soluble E-selectin; sICAM-1, soluble intercellular adhesion molecule; sP-selectin, soluble P-selectin; sVCAM-1, soluble vascular cellular adhesion molecule; TM, thrombomodulin; TNF-α, tumour necrosis factor α; TWEAK, TNF-like weak inducer of apoptosis; tPA, tissue plasminogen activator; vWF, von Willebrand factor
Serum biomarkers
Endothelial activation is triggered by several inflammatory stimuli such as toxins, inflammatory markers such as C-reactive protein, CD40 ligand (CD40L), interleukins (such as IL-1β, IL-18), CC-chemokine ligand 2 (CCL2), pentraxin-3, and sortilin (Table 5) [141–143]. In addition, inflammation is a vital feature in the development and progression of atherosclerosis and its complications. The inflammatory cascade is present in endothelial dysfunction and throughout the process of atherosclerosis [144].
Cell adhesion molecules
Endothelial cells are major players regulating the permeability and transport of molecules between the blood and the interstitial space and controlling the signalling pathways associated with innate immunity. Due to inflammation, ECs are activated, and the expression of adhesion molecules is incremented. Cell adhesion molecules are considered early markers of endothelial activation and systemic inflammation [141].
Soluble CAMs (i.e. intercellular adhesion molecule-1 (ICAM-1), E-selectins, and vascular cell adhesion molecule-1 (VCAM-1)) regulate the transmigration of leukocytes. ICAM-1 and VCAM-1 belong to the immunoglobulin superfamily and are ligands for β integrins on leukocytes and mononuclear cells, respectively [145, 146]. ICAM-1 is highly expressed in ECs and subendothelial macrophages [147] while VCAM-1 is predominant to ECs and is not present in healthy endothelium [147]. ICAM-1 participates in the adhesion and transmigration of leukocytes in the vascular endothelial wall and leads to endothelial cell activation and inflammation, early steps in the initiation and progression of atherosclerosis [148]. VCAM-1 expression probably results from endothelial activation, as it enhances local recruitment of monocytes and its interaction with ECs during the early phases of the atherosclerotic process [149].
E-selectin, belongs to the C-type lectin family, is one of the most specific markers of endothelial activation [5, 150]. Its expression is limited to the ECs and induced by inflammatory cytokines. E-selectin recruits leukocytes mediating its rolling to the site of inflammation [150].
Elevated levels of soluble adhesion molecules, as VCAM-1, P-selectin, and ICAM-1 have also been reported in COVID-19 patients [151, 152].
C-reactive protein
C-reactive protein (CRP) is a pentraxin with a crucial role in the innate human immune response [153]. CRP, traditionally consider a biomarker of inflammation, has pro-atherogenic properties, increasing the expression of adhesion molecules, reducing NO bioavailability, promoting vasoconstriction and endothelial dysfunction [144, 154]. CRP promotes endothelial activation through the expression of ICAM-1, VCAM-1, E-selectins, and CCL2 and activates macrophages that express cytokines and tissue factors [154]. CRP leads to a reduction in vasoactive factors derived from the endothelium, mainly NO, affecting vascular homeostasis. This process may promote apoptosis in ECs and reduce compensatory mechanisms important for angiogenesis [155].
Concomitantly, CRP increases the production of endothelin 1, a potent endothelium-dependent vasoconstrictor, and IL-6, a key pro-inflammatory cytokine [156]. CRP is considered a predictor of atherosclerosis and vascular dysfunction. This protein is able to modify the endothelial cell phenotype and contributing to lesion formation, plaque rupture, and coronary thrombosis. CRP is an inflammatory biomarker and a mediator of vascular disease [141].
CD40 ligand
The CD40L, belongs to the TNF superfamily, is a type II transmembrane soluble protein that comprises a pathophysiological pathway linked to inflammation and atherogenesis [157]. CD40L is primarily produced in platelets being fundamental in haemostasis and in the inflammatory response in the vascular wall [158]. Activated platelets express CD40L on their surface stimulating the secretion of chemokines and expression of adhesion molecules in ECs leading to the recruitment and mobilization of leukocytes to the lesion location [159].
CD40L can rapidly detach from the platelet membrane, appearing systemically. CD40L has proinflammatory, pro-oxidant and prothrombotic activity, increasing platelet activation and aggregation, and platelet-leukocyte and leukocyte-endothelial coupling both in the soluble form and in the platelet [160]. Indeed, CD40L leads to chronic inflammation, contributing to endothelial dysfunction and atherogenesis [157].
CC-chemokine ligand 2
The increased expression of CCL2 attracts monocytes from the vessel lumen into the subendothelial space and in association with adhesion molecules facilitates monocytes binding to the ECs and transmigration to the intima layer. The monocyte recruitment and migration are mediated by CCL2 [161, 162]. Inside the intima, monocytes differentiate into macrophages and start to express receptors such as macrophage scavenger receptor (SR-A), lecitin-like oxidized LDL receptor 1 (LOX-1), and CD36 that internalize modified LDL beginning the atherosclerotic process [162].
Endothelial damage triggers the increased expression of CCL2. The measurement of systemic levels of CCL2 is considered a biomarker of endothelial dysfunction [162].
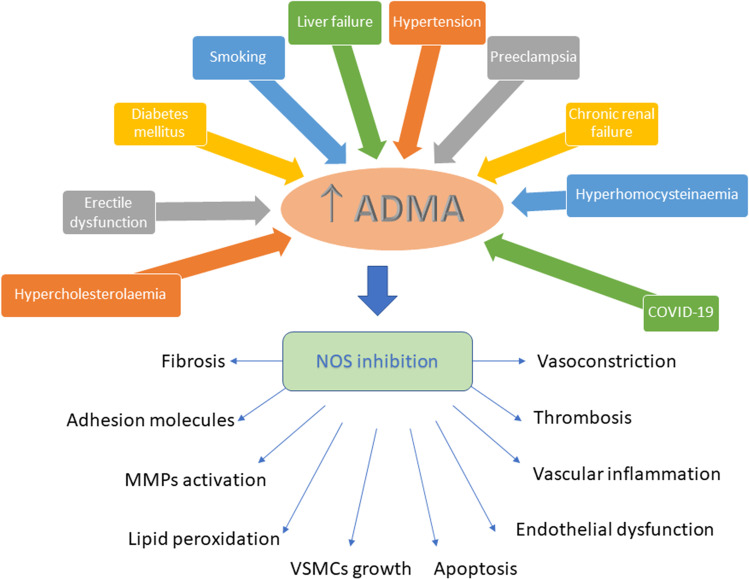
Asymmetric dimethylarginine
Asymmetric dimethylarginine (ADMA) is an endogenous inhibitor of NO synthase [163] and a biomarker of NO impairment and atherosclerosis [164, 165]. ADMA levels independently correlate with endothelial function measurements [166, 167]. Elevated plasma levels of ADMA are related with hyperlipidaemia, hypertension, coronary artery disease, unstable angina, end-stage renal disease, myocardial infarction, stroke, and diabetes (Fig. 9) [168–174]. Type 2 diabetes has been associated with elevated ADMA levels. ADMA and NO are crucial determinants of insulin resistance [175]. Metformin reduced serum levels of ADMA by 30% in type 2 diabetic patients [176]. Similarly, rosiglitazone reduced ADMA levels in insulin-resistant non-diabetic hypertensive individuals [177]. Increased levels have been reported in COVID-19 patients [178].
Fig. 9.
Major risk factors incrementing ADMA levels with subsequent nitric oxide synthase inhibition and concomitant consequences. ADMA, asymmetric dimethylarginine; MMPs, metalloproteinases; NOS, nitric oxide synthase; VSMCs, vascular smooth muscle cells
Endocan
Endocan, a soluble chondroitin/dermatan sulphate proteoglycan, is expressed and secreted mostly by the activated endothelium. Several pro-inflammatory cytokines and pro-angiogenic factors upregulate its synthesis and secretion [179]. Elevated levels of endocan have been associated with various cardiometabolic disorders, such as hypertension [180–182], chronic kidney disease [183], coronary artery disease [184–186], fatty liver disease [187], type 2 diabetes [188–190], and atherosclerosis [190–192]. In hypertension, endocan levels are positively correlated with cIMT, high-sensitivity CRP levels [180, 193], and arterial stiffness [194]. It has recently been implicated in the early phases of atherosclerosis in patients with type 2 diabetes [190].
Endocan is involved in atherosclerosis through endothelial dysfunction by promoting inflammation, cell adhesion, and oxidative stress [195]. Endocan enhances under proinflammatory conditions (i.e. increment in IL-1β, TNF-α, and other pro-inflammatory factors) leading to further augmentation of VCAM-1 and ICAM-1, with subsequent adhesion of leukocytes to the endothelium and recruitment and migration of inflammatory cells. In macrophages, in vitro, endocan treatment stimulated NO and ROS production and increased iNOS and CRP expression [196].
Endocan is an important predictor of progression and prognosis of cardiovascular events [195, 197].
Myeloperoxidase and reactive oxygen species
Myeloperoxidase (MPO), an enzyme belonging to the heme peroxidases superfamily, is produced by activated neutrophils, monocytes, and tissue macrophages. Once activated it catalyses the formation of ROS (such as hypochlorous acid, tyrosyl radical, and nitrogen dioxide) leading to oxidative damage of lipids and proteins in the body [141]. This enzyme is useful combating infectious diseases and can also be used to predict the onset and progression of atherosclerosis [198, 199]. MPO attaches to glycosaminoglycans in vasculature and impairs endothelial-derived NO release leading to endothelial dysfunction [198].
High MPO levels are linked to endothelial dysfunction and coronary artery disease, whereas low plasma levels and some MPO polymorphisms are cardioprotective [141, 199]. In turn, oxidative stress can promote endothelial dysfunction through various mechanisms; the most prominent involves the reduction of NO bioavailability [6]. The vicious cycle associated with the production of ROS can exceed the antioxidant defences, and ultimately, an increment in oxidized biomolecules and tissue damage may happen. Oxidative stress plays a central role in the development of endothelial dysfunction and atherogenesis [5, 6].
Pentraxin-3
Pentraxin 3 (PTX3), an inflammatory biomarker, belongs to the C-reactive protein family. PTX3 is considered a predictor of functional recovery in cardiac surgery patients [200].
Proinflammatory stimuli, injury, or infection, proinflammatory cytokines, toll-like receptor engagement, and microbial moieties induce PTX3 production by various cell types of the myeloid lineage, fibroblasts, epithelial cells, mesangial cells, vascular and lymphatic ECs, smooth muscle cells, adipocytes, astrocytes, and cells of microglia. PTX3 involved in matrix remodelling, plays a role in the resistance to some pathogens, and has a regulatory role in inflammation and in fertility. Once released, PTX3, a biomarker of inflammation and tissue damage, has a potential role in the diagnostic and prognostic of cardiovascular disease. In addition, PTX3 is a crucial player in innate immunity, interacting with various microbial or endogenous ligands, regulating inflammation as well as tissue remodelling and repair. The multiple functional properties of PTX3 relate to the ability to interact with diverse ligands.
Others
Atherothrombotic events are characterised by an increment in oxidative stress, endothelial cell activation, increment in several pro-inflammatory cytokines/chemokines, platelet activation, increment in acute phase proteins, angiogenic growth factors, among other systemic biomarkers (Fig. 10). Oxidized LDL (oxLDL) is pro-inflammatory molecules implicated in several atherosclerotic events. oxLDL is involved in early processes (increment in adhesion molecule expression and activation of the immune system) and late events (platelet aggregation and destabilization of atherosclerotic plaque) [198]. Oxidative stress modifies LDL particles during the migration in the blood vessel wall; oxLDL are a proposed marker of endothelial dysfunction and atherogenesis [143].
Fig. 10.
Biomarkers of atherothrombotic events. CCL2, CC-chemokine ligand 2; COX, cyclooxygenase; CRP, C-reactive protein; HGF, hepatocyte growth factor; IL, interleukin; Lp-PLA2, lipoprotein-associated phospholipase A2; MMPs, metalloproteinases; MPO, myeloperoxidase; NOX, NADPH oxidases; oxLDL, oxidized low density lipoprotein; PAPP-A, pregnancy-associated plasma protein-A; PIGF, placental growth factor; PPAR receptors, peroxisome proliferator-activated receptors; sCD40L, soluble CD40 ligand; sFasL, soluble Fas ligand; sICAM-1, soluble intercellular adhesion molecule 1; sVCAM-1, soluble vascular cellular adhesion molecule 1; TGF-β, transforming growth factor β; TIMP1,2, tissue inhibitor of metalloproteinases 1, 2; TNF-α, tumor necrosis factor α; VEGF, vascular endothelial growth factor; vW, von Willebrand factor
Free fatty acids promote increment in ROS levels and promote activation of nuclear factor-κB proinflammatory pathways being considered an early biomarker for endothelial damage and atherosclerosis [141].
Increased homocysteine levels and endothelin 1 overproduction are also linked with endothelial dysfunction and increment in vascular stiffness suggesting a major role in 3P medicine [64, 201, 202].
Following endothelial cell activation, an unbalance between tissue plasminogen activator and its endogenous inhibitor, plasminogen activation inhibitor-1, promotes a pro-coagulant state. In addition, von Willebrand factor, a glycoprotein released by ECs, nurtures coagulation and platelet activation. Fibrinogen, a glycoprotein and biomarker of endothelial function, is synthesised mainly in liver cells and megakaryocytes. Fibrinogen can attach to the surface of glycoprotein (GP) IIb/IIIa, linking platelets between them. Fibrinogen promotes platelet aggregation and smooth muscle cell migration, and enhances blood viscosity, and early events in the atherosclerotic process [5].
Increased renalase serum levels were recently linked with symptomatic coronary microvascular disease in patients with acute chest pain and suggested as a novel biomarker of coronary microvascular disease [203].
In COVID-19 patients, markers of endothelial activation as von Willebrand factor, thrombomodulin [204], angiopoietin-2 [151, 205], and endoglin, a transforming growth factor β receptor, have been described.
Cellular biomarkers
Circulating endothelial cells and endothelial microparticles
Endothelial function reveals the equilibrium between vascular endothelial damage and repair. There are several techniques to quantify the detachment of mature ECs and derived microparticles as an index of endothelium damage. Endothelial cell activation or injury fosters circulating endothelial cells (CEC) detachment leading to its increment in the circulation. Flow cytometry or fluorescence microscopy can be used to quantify CEC. The increment in CEC in the peripheral circulation is directly associated with the extent of endothelial damage in patients with vascular inflammation, atherosclerosis, and COVID-19 [162, 206].
Microparticles, the membrane vesicles (0.1 to 1 µm) released by different cell types and CEC, are novel biomarkers of endothelial injury, linked with atherosclerosis and related vascular complications (inflammation, thrombosis, and apoptosis). Microparticles are potential biomarkers of vascular damage and inflammation [207]. The number of circulating microparticles may provide a crucial clinical data in healthy individuals or patients with cardiovascular disease as a surrogate marker of vascular function [207, 208].
Endothelial microparticles (EMP) are small vesicles originated and released by the plasma membrane of activated or damaged ECs [162]. EMP carries adhesion molecules, enzymes, and their surface receptors, in addition to expressing a variety of constitutive antigens [209]. High levels of EMP occur when endothelial cells are activated and apoptotic and are directly related to thrombogenesis and atheromatous plaque formation [210], also participating in the processes of inflammation, vascular damage, and angiogenesis [211]. EMPs derived from activated endothelial cells may regulate monocyte/macrophage function stimulating the production of pro-inflammatory cytokines [212]. High EMP levels have been linked with endothelial dysfunction in coronary artery disease patients [212, 213].
Platelet microparticles
Platelet microparticles (PMP) are very abundant in human plasma [214]. Numerous studies have described a relation between PMP and inflammation [215], blood coagulation [216], thrombosis, and tumour progression [217]. They have a role in tissue regeneration and angiogenesis [218]. Their levels are high in myocardial infarction, type 2 diabetes, or pulmonary hypertension [25, 219, 220].
Monocyte microparticles
Microparticles derived from monocytes (MMP) are related to endothelial dysfunction [221]. MPM can activate endothelial cells, due to IL-1β increasing inflammation [222]. Treatment of ApoE − / − mice with MPM led to the accumulation of macrophages in the vascular wall and promoted atherosclerotic plaque formation. The interaction between MPM and inflammatory cells fosters the atherosclerotic disease in ApoE − / − mice [223].
Conclusions and expert recommendations
The importance of endothelial dysfunction for the development and progression of cardiovascular disease is unquestionable. Endothelial function can be evaluated in vivo, in vitro, with invasive, or non-invasive methodologies. It is noteworthy that these techniques are widely used in clinical research, but they are still not used in diagnosis, because they are too invasive, too expensive, or difficult to be standardised. We emphasize, therefore, the importance of further studies and investments in the area to make them applicable in clinical practice and, therefore, minimize public health problems related to cardiovascular diseases, through early diagnosis of endothelial dysfunction.
Endothelial dysfunction predicts the severity of cardiovascular diseases, and pharmacological and lifestyle changes can reverse it. Monitoring endothelial function can provide information regarding the efficacy of therapeutics, and progression of a vascular disease effectively contributes to the paradigm shift from reactive medical services to 3P medicine. However, the determination of endothelial function routinely is difficult, technically demanding, and not generally available in the clinical practice. Blood-based biomarkers of endothelial function are a minimally invasive diagnosis and a mean of predict response to therapies and an opportunity for early intervention to avoid the development of more life-threatening diseases. Novel, non-invasive, and more reliable techniques to evaluable endothelial function will be a helpful tool for the clinical in the process of early diagnosis, stratification, and follow-up of the patients.
Limitations
The present article is a narrative review and, therefore, does not present an established and reproducible method of production, leaving the authors responsible for identifying and selecting studies, analysing, and interpreting them. Noteworthy, the purpose of this review is to provide an update on the methods currently used to assess endothelial function, and to highlight new viewpoints in this area of knowledge that may effectively contribute towards a shift from reactive medical services to predictive, preventive, and personalised medicine.
Acknowledgements
Some of the figures presented in this article were created using templates from the Servier Medical Art (http://smart.servier.com), under a Creative Commons Attribution 3.0 Unported License.
Author contribution
CS developed the conceptual framework and drafted the manuscript. LG, RS suggested topics, references, items, and revised the manuscript. All authors contributed to the article and approved the submitted version.
Funding
CS was funded by FCT-Foundation for Science and Technology: UIDB/04539/2020 and by COMPETE-FEDER: POCI-01–0145-FEDER-007440.
Availability of data and material
Data sharing is not applicable to this article as no datasets were generated or analysed during the current study.
Code availability
Not applicable.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Golubnitschaja O, Baban B, Boniolo G, Wang W, Bubnov R, Kapalla M, Krapfenbauer K, Mozaffari MS, Costigliola V. Medicine in the early twenty-first century: paradigm and anticipation - EPMA position paper 2016. EPMA J. 2016;7:23. doi: 10.1186/s13167-016-0072-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Aird WC. Phenotypic heterogeneity of the endothelium: I. Structure, function, and mechanisms. Circ Res. 2007;100:158–73. doi: 10.1161/01.RES.0000255691.76142.4a. [DOI] [PubMed] [Google Scholar]
- 3.Aird WC. Phenotypic heterogeneity of the endothelium: II. Representative vascular beds Circ Res. 2007;100:174–190. doi: 10.1161/01.RES.0000255690.03436.ae. [DOI] [PubMed] [Google Scholar]
- 4.Soehnlein O, Libby P. Targeting inflammation in atherosclerosis — from experimental insights to the clinic. Nat Rev Drug Discov. 2021;20:589–610. doi: 10.1038/s41573-021-00198-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Deanfield JE, Halcox JP, Rabelink TJ. Endothelial function and dysfunction: testing and clinical relevance. Circulation. 2007;115:1285–1295. doi: 10.1161/CIRCULATIONAHA.106.652859. [DOI] [PubMed] [Google Scholar]
- 6.Sena CM, Pereira AM, Seiça R. Endothelial dysfunction - a major mediator of diabetic vascular disease. Biochim Biophys Acta. 2013;1832:2216–2231. doi: 10.1016/j.bbadis.2013.08.006. [DOI] [PubMed] [Google Scholar]
- 7.Jannaway M, Yang X, Meegan JE, Coleman DC, Yuan SY. Thrombin-cleaved syndecan-3/-4 ectodomain fragments mediate endothelial barrier dysfunction. PLoS ONE. 2019;14:e0214737. doi: 10.1371/journal.pone.0214737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Piotti A, Novelli D, Meessen JMTA, Ferlicca D, Coppolecchia S, Marino A, Salati G, Savioli M, Grasselli G, Bellani G, Pesenti A, Masson S, Caironi P, Gattinoni L, Gobbi M, Fracasso C, Latini R, ALBIOS Investigators Endothelial damage in septic shock patients as evidenced by circulating syndecan-1, sphingosine-1-phosphate and soluble VE-cadherin: a substudy of ALBIOS. Crit Care. 2021;25:113. doi: 10.1186/s13054-021-03545-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wettschureck N, Strilic B, Offermanns S. Passing the vascular barrier: endothelial signaling processes controlling extravasation. Physiol Rev. 2019;99:1467–1525. doi: 10.1152/physrev.00037.2018. [DOI] [PubMed] [Google Scholar]
- 10.Vanhoutte PM, Zhao Y, Xu A, Leung SW. Thirty years of saying NO: sources, fate, actions, and misfortunes of the endothelium-derived vasodilator mediator. Circ Res. 2016;119:375–396. doi: 10.1161/CIRCRESAHA.116.306531. [DOI] [PubMed] [Google Scholar]
- 11.Zamora R, Vodovotz Y, Billiar TR. Inducible nitric oxide synthase and inflammatory diseases. Mol Med. 2000;6:347–73. doi: 10.1007/BF03401781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Park-Windhol C, D’Amore PA. Disorders of vascular permeability. Annu Rev Pathol. 2016;11:251–281. doi: 10.1146/annurev-pathol-012615-044506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wenceslau CF, McCarthy CG, Szasz T, Goulopoulou S, Webb RC. Mitochondrial N-formyl peptides induce cardiovascular collapse and sepsis-like syndrome. Am J Physiol Heart Circ Physiol. 2015;308:H768–H777. doi: 10.1152/ajpheart.00779.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kumar P, Shen Q, Pivetti CD, Lee ES, Wu MH, Yuan SY. Molecular mechanisms of endothelial hyperpermeability: implications in inflammation. Exp Rev Mol Med. 2009;11:e19. doi: 10.1017/S1462399409001112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rodrigues EB, Farah ME, Maia M, Penha FM, Regatieri C, Melo GB, Pinheiro MM, Zanetti CR. Therapeutic monoclonal antibodies in ophthalmology. Prog Retin Eye Res. 2009;28:117–144. doi: 10.1016/j.preteyeres.2008.11.005. [DOI] [PubMed] [Google Scholar]
- 16.Alves NG, Trujillo AN, Breslin JW, Yuan SY. Sphingosine-1-phosphate reduces hemorrhagic shock and resuscitation-induced microvascular leakage by protecting endothelial mitochondrial integrity. Shock. 2019;52:423–433. doi: 10.1097/SHK.0000000000001280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Alves NG, Yuan SY, Breslin JW. Sphingosine-1-phosphate protects against brain microvascular endothelial junctional protein disorganization and barrier dysfunction caused by alcohol. Microcirculation. 2019;26:e12506. doi: 10.1111/micc.12506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yonekawa K, Harlan JM. Targeting leukocyte integrins in human diseases. J Leukoc Biol. 2005;77:129–140. doi: 10.1189/jlb.0804460. [DOI] [PubMed] [Google Scholar]
- 19.Zampetaki A, Kirton JP, Xu Q. Vascular repair by endothelial progenitor cells. Cardiovasc Res. 2008;78:413–421. doi: 10.1093/cvr/cvn081. [DOI] [PubMed] [Google Scholar]
- 20.Ludmer PL, Selwyn AP, Shook TL, Wayne RR, Mudge GH, Alexander RW, Ganz P. Paradoxical vasoconstriction induced by acetylcholine in atherosclerotic coronary arteries. N Engl J Med. 1986;315:1046–1051. doi: 10.1056/NEJM198610233151702. [DOI] [PubMed] [Google Scholar]
- 21.Tousoulis D, Davies G, Lefroy DC. Variable coronary vasomotor responses to acetylcholine in patients with normal coronary arteriograms: evidence for localised endothelial dysfunction. Heart. 1996;75:261–266. doi: 10.1136/hrt.75.3.261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ding D, Yang J, Westra J, Chen Y, Chang Y, Sejr-Hansen M, Zhang S, Christiansen EH, Holm NR, Xu B, Tu S. Accuracy of 3-dimensional and 2-dimensional quantitative coronary angiography for predicting physiological significance of coronary stenosis: a FAVOR II substudy. Cardiovasc Diagn Ther. 2019;9:481–91. doi: 10.21037/cdt.2019.09.07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lee J, Seo KW, Yang HM, Lim HS, Choi BJ, Choi SY, Tahk SJ, Yoon MH. Comparison of three-dimensional quantitative coronary angiography and intravascular ultrasound for detecting functionally significant coronary lesions. Cardiovasc Diagn Ther. 2020;10:1256–63. doi: 10.21037/cdt-20-560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zhang YJ, Zhu H, Shi SY, Muramatsu T, Pan DR, Ye F, Zhang JJ, Tian NL, Bourantas CV, Chen SL. Comparison between two-dimensional and three-dimensional quantitative coronary angiography for the prediction of functional severity in true bifurcation lesions: insights from the randomized DK-CRUSH II, III, and IV trials. Catheter Cardiovasc Interv. 2016;87(Suppl 1):589–598. doi: 10.1002/ccd.26405. [DOI] [PubMed] [Google Scholar]
- 25.Porto I, Biasucci LM, De Maria GL, Leone AM, Niccoli G, Burzotta F, Trani C, Tritarelli A, Vergallo R, Liuzzo G, Crea F. Intracoronary microparticles and microvascular obstruction in patients with ST elevation myocardial infarction undergoing primary percutaneous intervention. Eur Heart J. 2012;33:2928–2938. doi: 10.1093/eurheartj/ehs065. [DOI] [PubMed] [Google Scholar]
- 26.Voros S, Rinehart S, Vazquez-Figueroa JG, Kalynych A, Karmpaliotis D, Qian Z, Joshi PH, Anderson H, Murrieta L, Wilmer C, Carlson H, Ballard W, Brown C. Prospective, head-to-head comparison of quantitative coronary angiography, quantitative computed tomography angiography, and intravascular ultrasound for the prediction of hemodynamic significance in intermediate and severe lesions, using fractional flow reserve as reference standard (from the ATLANTA I and II Study) Am J Cardiol. 2014;113:23–29. doi: 10.1016/j.amjcard.2013.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Libby P, Buring JE, Badimon L, Hansson GK, Deanfield J, Bittencourt MS, Tokgözoğlu L, Lewis EF. Atherosclerosis Nat Rev Dis Primers. 2019;5:56. doi: 10.1038/s41572-019-0106-z. [DOI] [PubMed] [Google Scholar]
- 28.Hewlett AW, Van Zwaluwenburg JG. Method for estimating the blood flow in the arm: PRELIMINARY REPORT. Arch Intern Med (Chic) 1909;III(3):254–256. doi: 10.1001/archinte.1909.00050140084007. [DOI] [Google Scholar]
- 29.Joannides R, Haefeli WE, Linder L, Richard V, Bakkali EH, Thuillez C, Lüscher TF. Nitric oxide is responsible for flow-dependent dilatation of human peripheral conduit arteries in vivo. Circulation. 1995;91:1314–1319. doi: 10.1161/01.cir.91.5.1314. [DOI] [PubMed] [Google Scholar]
- 30.Kraemer-Aguiar LG, de Miranda ML, Bottino DA, Lima Rde A, de Souza Md, Balarini Mde M, Villela NR, Bouskela E. Increment of body mass index is positively correlated with worsening of endothelium-dependent and independent changes in forearm blood flow. Front Physiol. 2015;6:223. doi: 10.3389/fphys.2015.00223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Salisbury DL, Brown RJ, Bronas UG, Kirk LN, Treat-Jacobson D. Measurement of peripheral blood flow in patients with peripheral artery disease: methods and considerations. Vasc Med. 2018;23:163–171. doi: 10.1177/1358863X17751654. [DOI] [PubMed] [Google Scholar]
- 32.Petrie JR, Ueda S, Morris AD, Murray LS, Elliott HL, Connell JM. How reproducible is bilateral forearm plethysmography? Br J Clin Pharmacol. 1998;45:131–139. doi: 10.1046/j.1365-2125.1998.00656.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sena CM, Nunes E, Louro T, Proença T, Fernandes R, Boarder MR, Seiça RM. Effects of alpha-lipoic acid on endothelial function in aged diabetic and high-fat fed rats. Br J Pharmacol. 2008;153:894–906. doi: 10.1038/sj.bjp.0707474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sena CM, Matafome P, Louro T, Nunes E, Fernandes R, Seiça RM. Metformin restores endothelial function in aorta of diabetic rats. Br J Pharmacol. 2011;163:424–437. doi: 10.1111/j.1476-5381.2011.01230.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Pereira A, Fernandes R, Crisóstomo J, Seiça RM, Sena CM. The sulforaphane and pyridoxamine supplementation normalize endothelial dysfunction associated with type 2 diabetes. Sci Rep. 2017;7:14357. doi: 10.1038/s41598-017-14733-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sena CM, Louro T, Matafome P, Nunes E, Monteiro P, Seiça R. Antioxidant and vascular effects of gliclazide in type 2 diabetic rats fed high-fat diet. Physiol Res. 2009;58:203–9. doi: 10.33549/physiolres.931480. [DOI] [PubMed] [Google Scholar]
- 37.Ford TJ, Rocchiccioli P, Good R, McEntegart M, Eteiba H, Watkins S, Shaukat A, Lindsay M, Robertson K, Hood S, Yii E, Sidik N, Harvey A, Montezano AC, Beattie E, Haddow L, Oldroyd KG, Touyz RM, Berry C. Systemic microvascular dysfunction in microvascular and vasospastic angina. Eur Heart J. 2018;39:4086–4097. doi: 10.1093/eurheartj/ehy529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ives SJ, Park SY, Kwon OS, Gifford JR, Andtbacka RHI, Hyngstrom JR, Richardson RS. TRPV1 channels in human skeletal muscle feed arteries: implications for vascular function. Exp Physiol. 2017;102:1245–1258. doi: 10.1113/EP086223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Queiroz M, Sena CM. Perivascular adipose tissue in age-related vascular disease. Ageing Res Rev. 2020;59:101040. doi: 10.1016/j.arr.2020.101040. [DOI] [PubMed] [Google Scholar]
- 40.Celermajer DS, Sorensen KE, Gooch VM, Spiegelhalter DJ, Miller OI, Sullivan ID, Lloyd JK, Deanfield JE. Non-invasive detection of endothelial dysfunction in children and adults at risk of atherosclerosis. Lancet. 1992;340:1111–1115. doi: 10.1016/0140-6736(92)93147-f. [DOI] [PubMed] [Google Scholar]
- 41.Tarkin JM, Joshi FR, Rudd JH. PET imaging of inflammation in atherosclerosis. Nat Rev Cardiol. 2014;11:443–457. doi: 10.1038/nrcardio.2014.80. [DOI] [PubMed] [Google Scholar]
- 42.Dalla Pozza R, Ehringer-Schetitska D, Fritsch P, Jokinen E, Petropoulos A, Oberhoffer R, Association for European Paediatric Cardiology Working Group Cardiovascular Prevention Intima media thickness measurement in children: a statement from the Association for European Paediatric Cardiology (AEPC) Working Group on Cardiovascular Prevention endorsed by the Association for European Paediatric Cardiology. Atherosclerosis. 2015;238:380–7. doi: 10.1016/j.atherosclerosis.2014.12.029. [DOI] [PubMed] [Google Scholar]
- 43.Simova I. Intima-media thickness: appropriate evaluation and proper measurement. J Cardiol Pract. 2015;13:1–14. [Google Scholar]
- 44.Stein JH, Korcarz CE, Hurst RT, Lonn E, Kendall CB, Mohler ER, Najjar SS, Rembold CM, Post WS, American Society of Echocardiography Carotid Intima-Media Thickness Task Force Use of carotid ultrasound to identify subclinical vascular disease and evaluate cardiovascular disease risk: a consensus statement from the American Society of Echocardiography Carotid Intima-Media Thickness Task Force. Endorsed by the Society for Vascular Medicine. J Am Soc Echocardiogr. 2008;21:93–111. doi: 10.1016/j.echo.2007.11.011. [DOI] [PubMed] [Google Scholar]
- 45.Martins P, Pires A, Santos JL, Sena C, Seiça R. Atherosclerotic process in seroreverter children and adolescents exposed to fetal antiretroviral therapy. Curr HIV Res. 2021;19:216–224. doi: 10.2174/1570162X18999201118155026. [DOI] [PubMed] [Google Scholar]
- 46.Pires A, Martins P, Pereira AM, Silva PV, Marinho J, Marques M, Castela E, Sena C, Seiça R. Insulin resistance, dyslipidemia and cardiovascular changes in a group of obese children. Arq Bras Cardiol. 2015;104:266–273. doi: 10.5935/abc.20140206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Lorenz MW, Markus HS, Bots ML, Rosvall M, Sitzer M. Prediction of clinical cardiovascular events with carotid intima-media thickness: a systematic review and meta-analysis. Circulation. 2007;115:459–467. doi: 10.1161/CIRCULATIONAHA.106.628875. [DOI] [PubMed] [Google Scholar]
- 48.Pires A, Martins P, Pereira AM, Marques M, Castela E, Sena C, Seiça R. Childhood adiposity: being male is a potential cardiovascular risk factor. Eur J Pediatr. 2016;175:63–69. doi: 10.1007/s00431-015-2599-0. [DOI] [PubMed] [Google Scholar]
- 49.Bersi MR, Bellini C, Wu J, Montaniel KRC, Harrison DG, Humphrey JD. Excessive adventitial remodeling leads to early aortic maladaptation in angiotensin-induced hypertension. Hypertension. 2016;67:890–896. doi: 10.1161/HYPERTENSIONAHA.115.06262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Doshi SN, Naka KK, Payne N, Jones CJ, Ashton M, Lewis MJ, Goodfellow J. Flow-mediated dilatation following wrist and upper arm occlusion in humans: the contribution of nitric oxide. Clin Sci. 2001;101:629–635. doi: 10.1042/cs1010629. [DOI] [PubMed] [Google Scholar]
- 51.Maruhashi T, Iwamoto Y, Kajikawa M, Oda N, Kishimoto S, Matsui S, Hashimoto H, Aibara Y, Yusoff FM, Hidaka T, Kihara Y, Chayama K, Noma K, Nakashima A, Goto C, Hida E, Higashi Y. Interrelationships among flow-mediated vasodilation, nitroglycerin-induced vasodilation, baseline brachial artery diameter, hyperemic shear stress, and cardiovascular risk factors. J Am Heart Assoc. 2017;7:e006797. doi: 10.1161/JAHA.117.006797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Shimbo D, Grahame-Clarke C, Miyake Y, Rodriguez C, Sciacca R, Di Tullio M, Boden-Albala B, Sacco R, Homma S. The association between endothelial dysfunction and cardiovascular outcomes in a population-based multi-ethnic cohort. Atherosclerosis. 2007;192:197–203. doi: 10.1016/j.atherosclerosis.2006.05.005. [DOI] [PubMed] [Google Scholar]
- 53.Fathi R, Haluska B, Isbel N, Short L, Marwick TH. The relative importance of vascular structure and function in predicting cardiovascular events. J Am Coll Cardiol. 2004;43:616–623. doi: 10.1016/j.jacc.2003.09.042. [DOI] [PubMed] [Google Scholar]
- 54.Gokce N, Keaney JF, Jr, Hunter LM, Watkins MT, Nedeljkovic ZS, Menzoian JO, Vita JA. Predictive value of noninvasively determined endothelial dysfunction for long-term cardiovascular events in patients with peripheral vascular disease. J Am Coll Cardiol. 2003;41:1769–1775. doi: 10.1016/s0735-1097(03)00333-4. [DOI] [PubMed] [Google Scholar]
- 55.Sorensen KE, Celermajer DS, Spiegelhalter DJ, Georgakopoulos D, Robinson J, Thomas O, Deanfield JE. Non-invasive measurement of human endothelium dependent arterial responses: accuracy and reproducibility. Br Heart J. 1995;74:247–253. doi: 10.1136/hrt.74.3.247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Idei N, Ukawa T, Kajikawa M, Iwamoto Y, Fujimura N, Maruhashi T, Mikami S, Matsumoto T, Kihara Y, Chayama K, Noma K, Nakashima A, Takayanagi T, Morimoto H, Tsuji T, Higashi Y. A novel noninvasive and simple method for assessment of endothelial function: enclosed zone flow-mediated vasodilation (ezFMD) using an oscillation amplitude measurement. Atherosclerosis. 2013;229:324–330. doi: 10.1016/j.atherosclerosis.2013.05.016. [DOI] [PubMed] [Google Scholar]
- 57.Morimoto H, Kajikawa M, Oda N, Idei N, Hirano H, Hida E, Maruhashi T, Iwamoto Y, Kishimoto S, Matsui S, Aibara Y, Hidaka T, Kihara Y, Chayama K, Goto C, Noma K, Nakashima A, Ukawa T, Tsuji T, Higashi Y. Endothelial function assessed by automatic measurement of enclosed zone flow-mediated vasodilation using an oscillometric method is an independent predictor of cardiovascular events. J Am Heart Assoc. 2016;5:e004385. doi: 10.1161/JAHA.116.004385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Pierce GL. Mechanisms and subclinical consequences of aortic stiffness. Hypertension. 2017;70:848–853. doi: 10.1161/HYPERTENSIONAHA.117.08933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Van Bortel LM, Laurent S, Boutouyrie P, Chowienczyk P, Cruickshank JK, De Backer T, Filipovsky J, Huybrechts S, Mattace-Raso FU, Protogerou AD, Schillaci G, Segers P, Vermeersch S, Weber T. Expert consensus document on the measurement of aortic stiffness in daily practice using carotid-femoral pulse wave velocity. J Hypertens. 2012;30:445–448. doi: 10.1097/HJH.0b013e32834fa8b0. [DOI] [PubMed] [Google Scholar]
- 60.Kim YJ, Kim YJ, Cho BM, Lee S. Metabolic syndrome and arterial pulse wave velocity. Acta Cardiol. 2010;65:315–321. doi: 10.2143/AC.65.3.2050348. [DOI] [PubMed] [Google Scholar]
- 61.Pizzi O, Brandão AA, Magalhães MEC, Pozzan R, Brandão AP. Pulse wave velocity - methodology and prognostic implications in hypertension. Rev Bras Hipertens. 2006;13:59–62. [Google Scholar]
- 62.Chirinos JA, Segers S, Hughes T, Townsend R. Large-Artery Stiffness in Health and Disease. J Am Coll Cardiol. 2019;74:1237–1263. doi: 10.1016/j.jacc.2019.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Zhang S, Bai YY, Luo LM, Xiao WK, Wu HM, Ye P. Association between serum homocysteine and arterial stiffness in elderly: a community-based study. J Geriatr Cardiol. 2014;11:32–38. doi: 10.3969/j.issn.1671-5411.2014.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Koklesova L, Mazurakova A, Samec M, Biringer K, Samuel SM, Büsselberg D, Kubatka P, Golubnitschaja O. Homocysteine metabolism as the target for predictive medical approach, disease prevention, prognosis, and treatments tailored to the person. EPMA J. 2021;12:1–29. doi: 10.1007/s13167-021-00263-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Aristizábal-Ocampo D, Espíndola-Fernández D, Gallo-Villegas J. Pulse wave velocity reference values in 3,160 adults referred to a hypertension clinic for 24-hour ambulatory blood pressure monitoring. Clin Exp Hypertens. 2019;41:759–765. doi: 10.1080/10641963.2018.1545853. [DOI] [PubMed] [Google Scholar]
- 66.Laurent S, Cockcroft J, Van Bortel L, Boutouyrie P, Giannattasio C, Hayoz D, Pannier B, Vlachopoulos C, Wilkinson I, Struijker-Boudier H, European network for non-invasive investigation of large arteries Expert consensus document on arterial stiffness: methodological issues and clinical applications. Eur Heart J. 2006;27:2588–605. doi: 10.1093/eurheartj/ehl254. [DOI] [PubMed] [Google Scholar]
- 67.Park YC, Kang HC, Lee DC, Kim SH, Kim JK. Correlation between abnormal pap smear finding and brachial-ankle pulse wave velocity in Korean women. J Lifestyle Med. 2013;3:68–72. [PMC free article] [PubMed] [Google Scholar]
- 68.Husmann M, Jacomella V, Thalhammer C, Amann-Vesti BR. Markers of arterial stiffness in peripheral arterial disease. Vasa. 2015;44:341–348. doi: 10.1024/0301-1526/a000452. [DOI] [PubMed] [Google Scholar]
- 69.Tomiyama H, Matsumoto C, Shiina K, Yamashina A. Brachial-ankle PWV: current status and future directions as a useful marker in the management of cardiovascular disease and/or cardiovascular risk factors. J Atheroscler Thromb. 2016;23:128–146. doi: 10.5551/jat.32979. [DOI] [PubMed] [Google Scholar]
- 70.Spronck B, Avolio AP, Tan I, Butlin M, Reesink KD, Delhaas T. Arterial stiffness index beta and cardio-ankle vascular index inherently depend on blood pressure but can be readily corrected. J Hypertens. 2017;35:98–104. doi: 10.1097/HJH.0000000000001132. [DOI] [PubMed] [Google Scholar]
- 71.Axtell AL, Gomari FA, Cooke JP. Assessing endothelial vasodilator function with the Endo-PAT 2000. J Vis Exp. 2010;44:2167. doi: 10.3791/2167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Bonetti PO, Barsness GW, Keelan PC, Schnell TI, Pumper GM, Kuvin JT, Schnall RP, Holmes DR, Higano ST, Lerman A. Enhanced external counterpulsation improves endothelial function in patients with symptomatic coronary artery disease. J Am Coll Cardiol. 2003;41:1761–1768. doi: 10.1016/s0735-1097(03)00329-2. [DOI] [PubMed] [Google Scholar]
- 73.Allan RB, Vun SV, Spark JI. A comparison of measures of endothelial function in patients with peripheral arterial disease and age and gender matched controls. Int J Vasc Med. 2016;2016:2969740. doi: 10.1155/2016/2969740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Hamburg NM, Palmisano J, Larson MG, Sullivan LM, Lehman BT, Vasan RS, Levy D, Mitchell GF, Vita JA, Benjamin EJ. Relation of brachial and digital measures of vascular function in the community: the Framingham heart study. Hypertension. 2011;57:390–396. doi: 10.1161/HYPERTENSIONAHA.110.160812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Woo JS, Jang WS, Kim HS, Lee JH, Choi EY, Kim JB, Kim WS, Kim KS, Kim W. Comparison of peripheral arterial tonometry and flow-mediated vasodilation for assessment of the severity and complexity of coronary artery disease. Coron Artery Dis. 2014;25:421–426. doi: 10.1097/MCA.0000000000000094. [DOI] [PubMed] [Google Scholar]
- 76.Bonetti PO, Pumper GM, Higano ST, Holmes DR, Jr, Kuvin JT, Lerman A. Noninvasive identification of patients with early coronary atherosclerosis by assessment of digital reactive hyperemia. J Am Coll Cardiol. 2004;44:2137–2141. doi: 10.1016/j.jacc.2004.08.062. [DOI] [PubMed] [Google Scholar]
- 77.Hamburg NM, Keyes MJ, Larson MG, Vasan RS, Schnabel R, Pryde MM, Mitchell GF, Sheffy J, Vita JA, Benjamin EJ. Cross-sectional relations of digital vascular function to cardiovascular risk factors in the Framingham Heart Study. Circulation. 2008;117:2467–2474. doi: 10.1161/CIRCULATIONAHA.107.748574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Matsuzawa Y, Kwon TG, Lennon RJ, Lerman LO, Lerman A. Prognostic value of flow-mediated vasodilation in brachial artery and fingertip artery for cardiovascular events: a systematic review and meta-analysis. J Am Heart Assoc. 2015;4:e002270. doi: 10.1161/JAHA.115.002270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Rubinshtein R, Kuvin JT, Soer M, Lennon RJ, Lavi S, Nelson RE, Pumper GM, Lerman LO, Lerman A. Assessment of endothelial function by non-invasive peripheral arterial tonometry predicts late cardiovascular adverse events. Eur Heart J. 2010;31:1142–1148. doi: 10.1093/eurheartj/ehq010. [DOI] [PubMed] [Google Scholar]
- 80.Nohria A, Gerhard-Herman M, Creager MA, Hurley S, Mitra D, Ganz P. Role of nitric oxide in the regulation of digital pulse volume amplitude in humans. J Appl Physiol. 1985;2006(101):545–548. doi: 10.1152/japplphysiol.01285.2005. [DOI] [PubMed] [Google Scholar]
- 81.Cooper LL, Wang N, Beiser AS, Romero JR, Aparicio HJ, Lioutas VA, Benjamin EJ, Larson MG, Vasan RS, Mitchell GF, Seshadri S, Hamburg NM. Digital peripheral arterial tonometry and cardiovascular disease events: the Framingham heart study. Stroke. 2021;52:2866–2873. doi: 10.1161/STROKEAHA.120.031102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Nil M, Schäfer D, Radtke T, Saner H, Wilhelm M, Eser P. Reproducibility of peripheral arterial tonometry measurements in male cardiovascular patients. Eur J Clin Invest. 2014;44:1065–1071. doi: 10.1111/eci.12341. [DOI] [PubMed] [Google Scholar]
- 83.Weisrock F, Fritschka M, Beckmann S, Litmeier S, Wagner J, Tahirovic E, Radenovic S, Zelenak C, Hashemi D, Busjahn A, Krahn T, Pieske B, Dinh W, Düngen HD. Reliability of peripheral arterial tonometry in patients with heart failure, diabetic nephropathy and arterial hypertension. Vasc Med. 2017;22:292–300. doi: 10.1177/1358863X17706752. [DOI] [PubMed] [Google Scholar]
- 84.Houben AJHM, Martens RJH, Stehouwer CDA. Assessing microvascular function in humans from a chronic disease perspective. J Am Soc Nephrol. 2017;28:3461–3472. doi: 10.1681/ASN.2017020157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Carter HH, Gong P, Kirk RW, Es’haghian S, Atkinson CL, Sampson DD, Green DJ, McLaughlin RA. Optical coherence tomography in the assessment of acute changes in cutaneous vascular diameter induced by heat stress. J Appl Physiol (1985) 2016;121:965–72. doi: 10.1152/japplphysiol.00918.2015. [DOI] [PubMed] [Google Scholar]
- 86.Kim J, Brown W, Maher JR, Levinson H, Wax A. Functional optical coherence tomography: principles and progress. Phys Med Biol. 2015;60:R211–R237. doi: 10.1088/0031-9155/60/10/R211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Kim K, Kim ES, Yu SY. Optical coherence tomography angiography analysis of foveal microvascular changes and inner retinal layer thinning in patients with diabetes. Br J Ophthalmol. 2018;102:1226–1231. doi: 10.1136/bjophthalmol-2017-311149. [DOI] [PubMed] [Google Scholar]
- 88.Kim M, Choi SY, Park YH. Quantitative analysis of retinal and choroidal microvascular changes in patients with diabetes. Sci Rep. 2018;8:12146. doi: 10.1038/s41598-018-30699-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Men S, Wong JM, Welch EJ, Xu J, Song S, Deegan AJ, Ravichander A, Casavant B, Berthier E, Wang RK. OCT-based angiography of human dermal microvascular reactions to local stimuli: Implications for increasing capillary blood collection volumes. Lasers Surg Med. 2018;50:908–916. doi: 10.1002/lsm.22944. [DOI] [PubMed] [Google Scholar]
- 90.Li W, Schram MT, Sörensen BM, van Agtmaal MJM, Berendschot TTJM, Webers CAB, Jansen JFA, Backes WH, Gronenschild EHBM, Schalkwijk CG, Stehouwer CDA, Houben AJHM. Microvascular phenotyping in the Maastricht study: design and main findings, 2010–2018. Am J Epidemiol. 2020;189:873–884. doi: 10.1093/aje/kwaa023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Heslinga F, Pluim J, Dashtbozorg B, Berendschot T, Houben A, Henry R, Veta M. Approximation of a pipeline of unsupervised retina image analysis methods with a CNN. In: Proc. SPIE 10949, Medical Imaging 2019: Image Processing, 109491N, 2019. 10.1117/12.2512393
- 92.Poplin R, Varadarajan AV, Blumer K, Liu Y, McConnell MV, Corrado GS, Peng L, Webster DR. Prediction of cardiovascular risk factors from retinal fundus photographs via deep learning. Nat Biomed Eng. 2018;2:158–164. doi: 10.1038/s41551-018-0195-0. [DOI] [PubMed] [Google Scholar]
- 93.Günthner R, Hanssen H, Hauser C, Angermann S, Lorenz G, Kemmner S, Matschkal J, Braunisch MC, Kuechle C, Renders L, Moog P, Wassertheurer S, Baumann M, Hammes HP, Mayer CC, Haller B, Stryeck S, Madl T, Carbajo-Lozoya J, Heemann U, Kotliar K, Schmaderer C. Impaired retinal vessel dilation predicts mortality in end-stage renal disease. Circ Res. 2019;124:1796–1807. doi: 10.1161/CIRCRESAHA.118.314318. [DOI] [PubMed] [Google Scholar]
- 94.Nägele MP, Barthelmes J, Ludovici V, Cantatore S, Frank M, Ruschitzka F, Flammer AJ, Sudano I. Retinal microvascular dysfunction in hypercholesterolemia. J Clin Lipidol. 2018;12:1523–31.e2. doi: 10.1016/j.jacl.2018.07.015. [DOI] [PubMed] [Google Scholar]
- 95.Sörensen BM, Houben AJ, Berendschot TT, Schouten JS, Kroon AA, van der Kallen CJ, Henry RM, Koster A, Sep SJ, Dagnelie PC, Schaper NC, Schram MT, Stehouwer CD. Prediabetes and type 2 diabetes are associated with generalized microvascular dysfunction: the Maastricht study. Circulation. 2016;134:1339–1352. doi: 10.1161/CIRCULATIONAHA.116.023446. [DOI] [PubMed] [Google Scholar]
- 96.Honkura N, Richards M, Laviña B, Sáinz-Jaspeado M, Betsholtz C, Claesson-Welsh L. Intravital imaging-based analysis tools for vessel identification and assessment of concurrent dynamic vascular events. Nat Commun. 2018;9:2746. doi: 10.1038/s41467-018-04929-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Ince C, Boerma EC, Cecconi M, De Backer D, Shapiro NI, Duranteau J, Pinsky MR, Artigas A, Teboul JL, Reiss IKM, Aldecoa C, Hutchings SD, Donati A, Maggiorini M, Taccone FS, Hernandez G, Payen D, Tibboel D, Martin DS, Zarbock A, Monnet X, Dubin A, Bakker J, Vincent JL, Scheeren TWL. Cardiovascular Dynamics Section of the ESICM. Second consensus on the assessment of sublingual microcirculation in critically ill patients: results from a task force of the European Society of Intensive Care Medicine. Intensive Care Med. 2018;44:281–99. doi: 10.1007/s00134-018-5070-7. [DOI] [PubMed] [Google Scholar]
- 98.Lukasz A, Hillgruber C, Oberleithner H, Kusche-Vihrog K, Pavenstädt H, Rovas A, Hesse B, Goerge T, Kümpers P. Endothelial glycocalyx breakdown is mediated by angiopoietin-2. Cardiovasc Res. 2017;113:671–680. doi: 10.1093/cvr/cvx023. [DOI] [PubMed] [Google Scholar]
- 99.Margraf A, Herter JM, Kühne K, Stadtmann A, Ermert T, Wenk M, Meersch M, Van Aken H, Zarbock A, Rossaint J. 6% Hydroxyethyl starch (HES 130/0.4) diminishes glycocalyx degradation and decreases vascular permeability during systemic and pulmonary inflammation in mice. Crit Care. 2018;22:111. doi: 10.1186/s13054-017-1846-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Boushel R, Langberg H, Olesen J, Gonzales-Alonzo J, Bülow J, Kjaer M. Monitoring tissue oxygen availability with near infrared spectroscopy (NIRS) in health and disease. Scand J Med Sci Sports. 2001;11:213–222. doi: 10.1034/j.1600-0838.2001.110404.x. [DOI] [PubMed] [Google Scholar]
- 101.Charlton M, Sims M, Coats T, Thompson JP. The microcirculation and its measurement in sepsis. J Intensive Care Soc. 2017;18:221–227. doi: 10.1177/1751143716678638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Emanuel AL, Meijer RI, van Poelgeest E, Spoor P, Serné EH, Eringa EC. Contrast-enhanced ultrasound for quantification of tissue perfusion in humans. Microcirculation. 2020;27:e12588. doi: 10.1111/micc.12588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Corban MT, Lerman LO, Lerman A. Endothelial dysfunction. Arterioscler Thromb Vasc Biol. 2019;39:1272–1274. doi: 10.1161/atvbaha.119.312836. [DOI] [PubMed] [Google Scholar]
- 104.Redon J. Measurement of microalbuminuria - what the nephrologist should know. Nephrol Dial Transplant. 2006;21:573–576. doi: 10.1093/ndt/gfk014. [DOI] [PubMed] [Google Scholar]
- 105.Kashani K, Al-Khafaji A, Ardiles T, Artigas A, Bagshaw SM, Bell M, Bihorac A, Birkhahn R, Cely CM, Chawla LS, Davison DL, Feldkamp T, Forni LG, Gong MN, Gunnerson KJ, Haase M, Hackett J, Honore PM, Hoste EA, Joannes-Boyau O, Joannidis M, Kim P, Koyner JL, Laskowitz DT, Lissauer ME, Marx G, McCullough PA, Mullaney S, Ostermann M, Rimmelé T, Shapiro NI, Shaw AD, Shi J, Sprague AM, Vincent JL, Vinsonneau C, Wagner L, Walker MG, Wilkerson RG, Zacharowski K, Kellum JA. Discovery and validation of cell cycle arrest biomarkers in human acute kidney injury. Crit Care. 2013;17:R25. doi: 10.1186/cc12503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Alexander Y, Osto E, Schmidt-Trucksäss A, Shechter M, Trifunovic D, Duncker DJ, Aboyans V, Bäck M, Badimon L, Cosentino F, De Carlo M, Dorobantu M, Harrison DG, Guzik TJ, Hoefer I, Morris PD, Norata GD, Suades R, Taddei S, Vilahur G, Waltenberger J, Weber C, Wilkinson F, Bochaton-Piallat ML, Evans PC. Endothelial function in cardiovascular medicine: a consensus paper of the European Society of Cardiology Working Groups on Atherosclerosis and Vascular Biology, Aorta and Peripheral Vascular Diseases, Coronary Pathophysiology and Microcirculation, and Thrombosis. Cardiovasc Res. 2021;117:29–42. doi: 10.1093/cvr/cvaa085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Newman EA. Functional hyperemia and mechanisms of neurovascular coupling in the retinal vasculature. J Cereb Blood Flow Metab. 2013;33:1685–1695. doi: 10.1038/jcbfm.2013.145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Roustit M, Cracowski J-L. Assessment of endothelial and neurovascular function in human skin microcirculation. Trends Pharmacol Sci. 2013;34:373–384. doi: 10.1016/j.tips.2013.05.007. [DOI] [PubMed] [Google Scholar]
- 109.Jonasson H, Bergstrand S, Fredriksson I, Larsson M, Östgren CJ, Strömberg T. Normative data and the influence of age and sex on microcirculatory function in a middle-aged cohort: results from the SCAPIS study. Am J Physiol Heart Circ Physiol. 2020;318:H908–H915. doi: 10.1152/ajpheart.00668.2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Tan TE, Nguyen Q, Chua J, Schmetterer L, Tan GSW, Wong CW, Tsai A, Cheung GCM, Wong TY, Ting DSW. Global assessment of retinal arteriolar, venular and capillary microcirculations using fundus photographs and optical coherence tomography angiography in diabetic retinopathy. Sci Rep. 2019;9:11751. doi: 10.1038/s41598-019-47770-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Gardiner TA, Archer DB, Curtis TM, Stitt AW. Arteriolar involvement in the microvascular lesions of diabetic retinopathy: implications for pathogenesis. Microcirculation. 2007;14:25–38. doi: 10.1080/10739680601072123. [DOI] [PubMed] [Google Scholar]
- 112.Nieuwdorp M, Meuwese MC, Mooij HL, Ince C, Broekhuizen LN, Kastelein JJ, Stroes ES, Vink H. Measuring endothelial glycocalyx dimensions in humans: a potential novel tool to monitor vascular vulnerability. J Appl Physiol. 1985;2008(104):845–852. doi: 10.1152/japplphysiol.00440.2007. [DOI] [PubMed] [Google Scholar]
- 113.Goedhart PT, Khalilzada M, Bezemer R, Merza J, Ince C. Sidestream dark field (SDF) imaging: a novel stroboscopic LED ring-based imaging modality for clinical assessment of the microcirculation. Opt Express. 2007;15:15101–15114. doi: 10.1364/OE.15.015101. [DOI] [PubMed] [Google Scholar]
- 114.Celi LA, Lokhandwala S, Montgomery R, Moses C, Naumann T, Pollard T, Spitz D, Stretch R. Datathons and software to promote reproducible research. J Med Internet Res. 2016;18:e230. doi: 10.2196/jmir.6365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Dekker NAM, Veerhoek D, Koning NJ, van Leeuwen ALI, Elbers PWG, van den Brom CE, Vonk ABA, Boer C. Postoperative microcirculatory perfusion and endothelial glycocalyx shedding following cardiac surgery with cardiopulmonary bypass. Anaesthesia. 2019;74:609–618. doi: 10.1111/anae.14577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Koning NJ, Vonk AB, Vink H, Boer C. Side-by-side alterations in glycocalyx thickness and perfused microvascular density during acute microcirculatory alterations in cardiac surgery. Microcirculation. 2016;23:69–74. doi: 10.1111/micc.12260. [DOI] [PubMed] [Google Scholar]
- 117.Rovas A, Lukasz AH, Vink H, Urban M, Sackarnd J, Pavenstädt H, Kümpers P. Bedside analysis of the sublingual microvascular glycocalyx in the emergency room and intensive care unit - the GlycoNurse study. Scand J Trauma Resusc Emerg Med. 2018;26:16. doi: 10.1186/s13049-018-0483-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Rovas A, Seidel LM, Vink H, Pohlkötter T, Pavenstädt H, Ertmer C, Hessler M, Kümpers P. Association of sublingual microcirculation parameters and endothelial glycocalyx dimensions in resuscitated sepsis. Crit Care. 2019;23:260. doi: 10.1186/s13054-019-2542-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Drost CC, Rovas A, Kusche-Vihrog K, Van Slyke P, Kim H, Hoang VC, Maynes JT, Wennmann DO, Pavenstädt H, Linke W, Lukasz A, Hesse B, Kümpers P. Tie2 activation promotes protection and reconstitution of the endothelial glycocalyx in human sepsis. Thromb Haemost. 2019;119:1827–1838. doi: 10.1055/s-0039-1695768. [DOI] [PubMed] [Google Scholar]
- 120.Low DA, Jones H, Cable NT, Alexander LM, Kenney WL. Historical reviews of the assessment of human cardiovascular function: interrogation and understanding of the control of skin blood flow. Eur J Appl Physiol. 2020;120:1–16. doi: 10.1007/s00421-019-04246-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Eun HC. Evaluation of skin blood flow by laser Doppler flowmetry. Clin Dermatol. 1995;13:337–347. doi: 10.1016/0738-081x(95)00080-y. [DOI] [PubMed] [Google Scholar]
- 122.Roustit M, Cracowski JL. Non-invasive assessment of skin microvascular function in humans: an insight into methods. Microcirculation. 2012;19:47–64. doi: 10.1111/j.1549-8719.2011.00129.x. [DOI] [PubMed] [Google Scholar]
- 123.Farkas K, Kolossváry E, Járai Z, Nemcsik J, Farsang C. Non-invasive assessment of microvascular endothelial function by laser Doppler flowmetry in patients with essential hypertension. Atherosclerosis. 2004;173:97–102. doi: 10.1016/j.atherosclerosis.2003.11.015. [DOI] [PubMed] [Google Scholar]
- 124.Rossi M, Matteucci E, Pesce M, Consani C, Franzoni F, Santoro G, Giampietro O. Peripheral microvascular dysfunction as an independent predictor of atherosclerotic damage in type 1 diabetes patients: a preliminary study. Clin Hemorheol Microcirc. 2013;54:381–391. doi: 10.3233/CH-2012-1628. [DOI] [PubMed] [Google Scholar]
- 125.Roustit M, Blaise S, Millet C, Cracowski JL. Reproducibility and methodological issues of skin post-occlusive and thermal hyperemia assessed by single-point laser Doppler flowmetry. Microvasc Res. 2010;79:102–108. doi: 10.1016/j.mvr.2010.01.001. [DOI] [PubMed] [Google Scholar]
- 126.Tew GA, Klonizakis M, Crank H, Briers JD, Hodges GJ. Comparison of laser speckle contrast imaging with laser Doppler for assessing microvascular function. Microvasc Res. 2011;82:326–332. doi: 10.1016/j.mvr.2011.07.007. [DOI] [PubMed] [Google Scholar]
- 127.Hecht N, Woitzik J, Dreier JP, Vajkoczy P. Intraoperative monitoring of cerebral blood flow by laser speckle contrast analysis. Neurosurg Focus. 2009;27:E11. doi: 10.3171/2009.8.FOCUS09148. [DOI] [PubMed] [Google Scholar]
- 128.Mennes OA, van Netten JJ, van Baal JG, Steenbergen W. Assessment of microcirculation in the diabetic foot with laser speckle contrast imaging. Physiol Meas. 2019;40:065002. doi: 10.1088/1361-6579/ab2058. [DOI] [PubMed] [Google Scholar]
- 129.de Matheus AS, Clemente EL, de Lourdes Guimarães Rodrigues M, Torres Valença DC, Gomes MB. Assessment of microvascular endothelial function in type 1 diabetes using laser speckle contrast imaging. J Diabetes Complications. 2017;31:753–7. doi: 10.1016/j.jdiacomp.2016.12.007. [DOI] [PubMed] [Google Scholar]
- 130.Alexandrou ME, Gkaliagkousi Ε, Loutradis C, Dimitriadis C, Mitsopoulos E, Lazaridis A, Nikolaidou B, Dolgiras P, Douma S, Papagianni A, Sarafidis PA. Haemodialysis and peritoneal dialysis patients have severely impaired post-occlusive skin forearm vasodilatory response assessed with laser speckle contrast imaging. Clin Kidney J. 2020;14:1419–1427. doi: 10.1093/ckj/sfaa136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Borges JP, Lopes GO, Verri V, Coelho MP, Nascimento PM, Kopiler DA, Tibirica E. A novel effective method for the assessment of microvascular function in male patients with coronary artery disease: a pilot study using laser speckle contrast imaging. Braz J Med Biol Res. 2016;49:e5541. doi: 10.1590/1414-431X20165541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Mahé G, Rousseau P, Durand S, Bricq S, Leftheriotis G, Abraham P. Laser speckle contrast imaging accurately measures blood flow over moving skin surfaces. Microvasc Res. 2011;81:183–188. doi: 10.1016/j.mvr.2010.11.013. [DOI] [PubMed] [Google Scholar]
- 133.Fearon WF, Aarnoudse W, Pijls NH, De Bruyne B, Balsam LB, Cooke DT, Robbins RC, Fitzgerald PJ, Yeung AC, Yock PG. Microvascular resistance is not influenced by epicardial coronary artery stenosis severity: experimental validation. Circulation. 2004;109:2269–2272. doi: 10.1161/01.CIR.0000128669.99355.CB. [DOI] [PubMed] [Google Scholar]
- 134.Konst RE, Elias-Smale SE, Pellegrini D, Hartzema-Meijer M, van Uden BJC, Jansen TPJ, Vart P, Gehlmann H, Maas AHEM, van Royen N, Damman P. Absolute coronary blood flow measured by continuous thermodilution in patients with ischemia and nonobstructive disease. J Am Coll Cardiol. 2021;77:728–741. doi: 10.1016/j.jacc.2020.12.019. [DOI] [PubMed] [Google Scholar]
- 135.Xaplanteris P, Fournier S, Keulards DCJ, Adjedj J, Ciccarelli G, Milkas A, Pellicano M, Van't Veer M, Barbato E, Pijls NHJ, De Bruyne B. Catheter-based measurements of absolute coronary blood flow and microvascular resistance: feasibility, safety, and reproducibility in humans. Circ Cardiovasc Interv. 2018;11:e006194. doi: 10.1161/CIRCINTERVENTIONS.117.006194. [DOI] [PubMed] [Google Scholar]
- 136.Keulards DCJ, El Farissi M, Tonino PAL, Teeuwen K, Vlaar PJ, van Hagen E, Wijnbergen IF, de Vos A, Brueren GRG, Van't Veer M, Pijls NHJ. Thermodilution-based invasive assessment of absolute coronary blood flow and microvascular resistance: quantification of microvascular (dys)function? J Interv Cardiol. 2020;2020:5024971. doi: 10.1155/2020/5024971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Jones S, Chiesa ST, Chaturvedi N, Hughes AD. Recent developments in near-infrared spectroscopy (NIRS) for the assessment of local skeletal muscle microvascular function and capacity to utilise oxygen. Artery Res. 2016;16:25–33. doi: 10.1016/j.artres.2016.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Dipla K, Triantafyllou A, Koletsos N, Papadopoulos S, Sachpekidis V, Vrabas IS, Gkaliagkousi E, Zafeiridis A, Douma S. Impaired muscle oxygenation and elevated exercise blood pressure in hypertensive patients: links with vascular stiffness. Hypertension. 2017;70:444–451. doi: 10.1161/HYPERTENSIONAHA.117.09558. [DOI] [PubMed] [Google Scholar]
- 139.Lyngbakken MN, Myhre PL, Røsjø H, Omland T. Novel biomarkers of cardiovascular disease: applications in clinical practice. Crit Rev Clin Lab Sci. 2019;56:33–60. doi: 10.1080/10408363.2018.1525335. [DOI] [PubMed] [Google Scholar]
- 140.Ruparelia N, Choudhury R. Inflammation and atherosclerosis: what is on the horizon? Heart. 2020;106:80–85. doi: 10.1136/heartjnl-2018-314230. [DOI] [PubMed] [Google Scholar]
- 141.Badimon L, Romero JC, Cubedo J, Borrell-Pagès M. Circulating biomarkers. Thromb Res. 2012;130(Suppl 1):S12–S15. doi: 10.1016/j.thromres.2012.08.262. [DOI] [PubMed] [Google Scholar]
- 142.Han W, Wei Z, Zhang H, Geng C, Dang R, Yang M, Zhang J, Wang C, Jiang P. The association between sortilin and inflammation in patients with coronary heart disease. J Inflamm Res. 2020;13:71–79. doi: 10.2147/JIR.S240421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Straface E, Lista P, Gambardella L, Franconi F, Malorni W. Gender-specific features of plasmatic and circulating cell alterations as risk factors in cardiovascular disease. Fundam Clin Pharmacol. 2010;24:665–674. doi: 10.1111/j.1472-8206.2010.00860.x. [DOI] [PubMed] [Google Scholar]
- 144.Verma S, Anderson TJ. Fundamentals of endothelial function for the clinical cardiologist. Circulation. 2002;105:546–549. doi: 10.1161/hc0502.104540. [DOI] [PubMed] [Google Scholar]
- 145.Cook-Mills JM, Marchese ME, Abdala-Valencia H. Vascular cell adhesion molecule-1 expression and signaling during disease: regulation by reactive oxygen species and antioxidants. Antioxid Redox Signal. 2011;15:1607–1638. doi: 10.1089/ars.2010.3522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Hubbard AK, Rothlein R. Intercellular adhesion molecule-1 (ICAM-1) expression and cell signaling cascades. Free Radic Biol Med. 2000;28:1379–1386. doi: 10.1016/s0891-5849(00)00223-9. [DOI] [PubMed] [Google Scholar]
- 147.de Lemos JA, Hennekens CH, Ridker PM. Plasma concentration of soluble vascular cell adhesion molecule-1 and subsequent cardiovascular risk. J Am Coll Cardiol. 2000;36:423–426. doi: 10.1016/s0735-1097(00)00742-7. [DOI] [PubMed] [Google Scholar]
- 148.Ridker PM, Hennekens CH, Roitman-Johnson B, Stampfer MJ, Allen J. Plasma concentration of soluble intercellular adhesion molecule 1 and risks of future myocardial infarction in apparently healthy men. Lancet. 1998;351:88–92. doi: 10.1016/S0140-6736(97)09032-6. [DOI] [PubMed] [Google Scholar]
- 149.Li H, Cybulsky MI, Gimbrone MA, Jr, Libby P. An atherogenic diet rapidly induces VCAM-1, a cytokine-regulatable mononuclear leukocyte adhesion molecule, in rabbit aortic endothelium. Arterioscler Thromb. 1993;13:197–204. doi: 10.1161/01.atv.13.2.197. [DOI] [PubMed] [Google Scholar]
- 150.Hidalgo A, Peired AJ, Wild M, Vestweber D, Frenette PS. Complete identification of E-selectin ligands on neutrophils reveals distinct functions of PSGL-1, ESL-1, and CD44. Immunity. 2007;26:477–489. doi: 10.1016/j.immuni.2007.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Spadaro S, Fogagnolo A, Campo G, Zucchetti O, Verri M, Ottaviani I, Tunstall T, Grasso S, Scaramuzzo V, Murgolo F, Marangoni E, Vieceli Dalla Sega F, Fortini F, Pavasini R, Rizzo P, Ferrari R, Papi A, Volta CA, Contoli M. Markers of endothelial and epithelial pulmonary injury in mechanically ventilated COVID-19 ICU patients. Crit Care. 2021;25:74. doi: 10.1186/s13054-021-03499-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Vieceli Dalla Sega F, Fortini F, Spadaro S, Ronzoni L, Zucchetti O, Manfrini M, Mikus E, Fogagnolo A, Torsani F, Pavasini R, Marracino L, Verri M, Morandi L, D’Aniello E, Volta CA, Campo G, Ferrari R, Rizzo P, Contoli M. Time course of endothelial dysfunction markers and mortality in COVID-19 patients: a pilot study. Clin Transl Med. 2021;11:e283. doi: 10.1002/ctm2.283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Du Clos TW. Function of C-reactive protein. Ann Med. 2000;32:274–278. doi: 10.3109/07853890009011772. [DOI] [PubMed] [Google Scholar]
- 154.Yeh ET, Willerson JT. Coming of age of C-reactive protein: using inflammation markers in cardiology. Circulation. 2003;107:370–371. doi: 10.1161/01.cir.0000053731.05365.5a. [DOI] [PubMed] [Google Scholar]
- 155.Verma S, Wang CH, Li SH, Dumont AS, Fedak PW, Badiwala MV, Dhillon B, Weisel RD, Li RK, Mickle DA, Stewart DJ. A self-fulfilling prophecy: C-reactive protein attenuates nitric oxide production and inhibits angiogenesis. Circulation. 2002;106:913–919. doi: 10.1161/01.cir.0000029802.88087.5e. [DOI] [PubMed] [Google Scholar]
- 156.Verma S, Li SH, Badiwala MV, Weisel RD, Fedak PW, Li RK, Dhillon B, Mickle DA. Endothelin antagonism and interleukin-6 inhibition attenuate the proatherogenic effects of C-reactive protein. Circulation. 2002;105:1890–1896. doi: 10.1161/01.cir.0000015126.83143.b4. [DOI] [PubMed] [Google Scholar]
- 157.Pamukcu B, Lip GY, Snezhitskiy V, Shantsila E. The CD40-CD40L system in cardiovascular disease. Ann Med. 2011;43:331–340. doi: 10.3109/07853890.2010.546362. [DOI] [PubMed] [Google Scholar]
- 158.Wenzel F, Baertl A, Zimmermann N, Hohlfeld T, Giers G, Oldenburg J, Assert R. Different behaviour of soluble CD40L concentrations can be reflected by variations of preanalytical conditions. Clin Hemorheol Microcirc. 2008;39:417–22. doi: 10.3233/CH-2008-1112. [DOI] [PubMed] [Google Scholar]
- 159.Henn V, Slupsky JR, Gräfe M, Anagnostopoulos I, Förster R, Müller-Berghaus G, Kroczek RA. CD40 ligand on activated platelets triggers an inflammatory reaction of endothelial cells. Nature. 1998;391:591–594. doi: 10.1038/35393. [DOI] [PubMed] [Google Scholar]
- 160.Chakrabarti S, Varghese S, Vitseva O, Tanriverdi K, Freedman JE. CD40 ligand influences platelet release of reactive oxygen intermediates. Arterioscler Thromb Vasc Biol. 2005;25:2428–2434. doi: 10.1161/01.ATV.0000184765.59207.f3. [DOI] [PubMed] [Google Scholar]
- 161.Navab M, Imes SS, Hama SY, Hough GP, Ross LA, Bork RW, Valente AJ, Berliner JA, Drinkwater DC, Laks H, Fogelman AM. Monocyte transmigration induced by modification of low density lipoprotein in cocultures of human aortic wall cells is due to induction of monocyte chemotactic protein 1 synthesis and is abolished by high density lipoprotein. J Clin Invest. 1991;88:2039–2046. doi: 10.1172/JCI115532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Szmitko PE, Wang CH, Weisel RD, de Almeida JR, Anderson TJ, Verma S. New markers of inflammation and endothelial cell activation: Part I. Circulation. 2003;108:1917–1923. doi: 10.1161/01.CIR.0000089190.95415.9F. [DOI] [PubMed] [Google Scholar]
- 163.Vallance P, Leone A, Calver A, Collier J, Moncada S. Accumulation of an endogenous inhibitor of nitric oxide synthesis in chronic renal failure. Lancet. 1992;339:572–575. doi: 10.1016/0140-6736(92)90865-z. [DOI] [PubMed] [Google Scholar]
- 164.Dowsett L, Higgins E, Alanazi S, Alshuwayer NA, Leiper FC, Leiper J. ADMA: a key player in the relationship between vascular dysfunction and inflammation in atherosclerosis. J Clin Med. 2020;9:3026. doi: 10.3390/jcm9093026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Kielstein JT, Fliser D. The past, presence and future of ADMA in nephrology. Nephrol Ther. 2007;3:47–54. doi: 10.1016/j.nephro.2007.02.002. [DOI] [PubMed] [Google Scholar]
- 166.Wang F, Xiong R, Feng S, Lu X, Li H, Wang S. Association of circulating levels of ADMA with carotid intima-media thickness in patients with CKD: a systematic review and meta-analysis. Kidney Blood Press Res. 2018;43:25–33. doi: 10.1159/000486743. [DOI] [PubMed] [Google Scholar]
- 167.Yilmaz MI, Sonmez A, Saglam M, Qureshi AR, Carrero JJ, Caglar K, Eyileten T, Cakir E, Oguz Y, Vural A, Yenicesu M, Lindholm B, Stenvinkel P, Axelsson J. ADMA levels correlate with proteinuria, secondary amyloidosis, and endothelial dysfunction. J Am Soc Nephrol. 2008;19:388–395. doi: 10.1681/ASN.2007040461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Böger RH, Sullivan LM, Schwedhelm E, Wang TJ, Maas R, Benjamin EJ, Schulze F, Xanthakis V, Benndorf RA, Vasan RS. Plasma asymmetric dimethylarginine and incidence of cardiovascular disease and death in the community. Circulation. 2009;119:1592–1600. doi: 10.1161/CIRCULATIONAHA.108.838268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Caglar K, Yilmaz MI, Sonmez A, Cakir E, Kaya A, Acikel C, Eyileten T, Yenicesu M, Oguz Y, Bilgi C, Oktenli C, Vural A, Zoccali C. ADMA, proteinuria, and insulin resistance in non-diabetic stage I chronic kidney disease. Kidney Int. 2006;70:781–787. doi: 10.1038/sj.ki.5001632. [DOI] [PubMed] [Google Scholar]
- 170.Kobayashi S, Oka M, Maesato K, Ikee R, Mano T, Hidekazu M, Ohtake T. Coronary artery calcification, ADMA, and insulin resistance in CKD patients. Clin J Am Soc Nephrol. 2008;3:1289–1295. doi: 10.2215/CJN.00010108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Leong T, Zylberstein D, Graham I, Lissner L, Ward D, Fogarty J, Bengtsson C, Bjorkelund C, Thelle D, Swedish-Irish-Norwegian C. Asymmetric dimethylarginine independently predicts fatal and nonfatal myocardial infarction and stroke in women: 24-year follow-up of the population study of women in Gothenburg. Arterioscler Thromb Vasc Biol. 2008;28:961–967. doi: 10.1161/ATVBAHA.107.156596. [DOI] [PubMed] [Google Scholar]
- 172.Stühlinger MC, Oka RK, Graf EE, Schmölzer I, Upson BM, Kapoor O, Szuba A, Malinow MR, Wascher TC, Pachinger O, Cooke JP. Endothelial dysfunction induced by hyperhomocyst(e)inemia: role of asymmetric dimethylarginine. Circulation. 2003;108:933–938. doi: 10.1161/01.CIR.0000085067.55901.89. [DOI] [PubMed] [Google Scholar]
- 173.Yoo JH, Lee SC. Elevated levels of plasma homocyst(e)ine and asymmetric dimethylarginine in elderly patients with stroke. Atherosclerosis. 2001;158:425–430. doi: 10.1016/s0021-9150(01)00444-0. [DOI] [PubMed] [Google Scholar]
- 174.Sena CM, Bento CF, Pereira P, Seiça R. Diabetes mellitus: new challenges and innovative therapies. EPMA J. 2010;1:138–163. doi: 10.1007/s13167-010-0010-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Cook S, Hugli O, Egli M, Ménard B, Thalmann S, Sartori C, Perrin C, Nicod P, Thorens B, Vollenweider P, Scherrer U, Burcelin R. Partial gene deletion of endothelial nitric oxide synthase predisposes to exaggerated high-fat diet-induced insulin resistance and arterial hypertension. Diabetes. 2004;53:2067–2072. doi: 10.2337/diabetes.53.8.2067. [DOI] [PubMed] [Google Scholar]
- 176.Asagami T, Abbasi F, Stuelinger M, Lamendola C, McLaughlin T, Cooke JP, Reaven GM, Tsao PS. Metformin treatment lowers asymmetric dimethylarginine concentrations in patients with type 2 diabetes. Metabolism. 2002;51:843–846. doi: 10.1053/meta.2002.33349. [DOI] [PubMed] [Google Scholar]
- 177.Stühlinger MC, Abbasi F, Chu JW, Lamendola C, McLaughlin TL, Cooke JP, Reaven GM, Tsao PS. Relationship between insulin resistance and an endogenous nitric oxide synthase inhibitor. JAMA. 2002;287:1420–1426. doi: 10.1001/jama.287.11.1420. [DOI] [PubMed] [Google Scholar]
- 178.Canzano P, Brambilla M, Porro B, Cosentino N, Tortorici E, Vicini S, Poggio P, Cascella A, Pengo MF, Veglia F, Fiorelli S, Bonomi A, Cavalca V, Trabattoni D, Andreini D, Omodeo Salè E, Parati G, Tremoli E, Camera M. Platelet and endothelial activation as potential mechanisms behind the thrombotic complications of COVID-19 patients. JACC Basic Transl Sci. 2021;6:202–218. doi: 10.1016/j.jacbts.2020.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Lassalle P, Molet S, Janin A, Heyden JV, Tavernier J, Fiers W, Devos R, Tonnel AB. ESM-1 is a novel human endothelial cell-specific molecule expressed in lung and regulated by cytokines. J Biol Chem. 1996;271:20458–20464. doi: 10.1074/jbc.271.34.20458. [DOI] [PubMed] [Google Scholar]
- 180.Balta S, Mikhailidis DP, Demirkol S, Ozturk C, Kurtoglu E, Demir M, Celik T, Turker T, Iyisoy A. Endocan—a novel inflammatory indicator in newly diagnosed patients with hypertension: a pilot study. Angiology. 2014;65:773–777. doi: 10.1177/0003319713513492. [DOI] [PubMed] [Google Scholar]
- 181.Klisić A, Kavaric N, Vujcic S, Spasojevic-Kalimanovska V, Ninic A, Kotur-Stevuljevic J. Endocan and advanced oxidation protein products in adult population with hypertension. Eur Rev Med Pharmacol Sci. 2020;24:7131–7. doi: 10.26355/eurrev_202006_21707. [DOI] [PubMed] [Google Scholar]
- 182.Musialowska D, Zbroch E, Koc-Zorawska E, Musialowski P, Malyszko J. Endocan concentration in patients with primary hypertension. Angiology. 2018;69:483–489. doi: 10.1177/0003319717736158. [DOI] [PubMed] [Google Scholar]
- 183.Ekiz-Bilir B, Bilir B, Aydın M, Soysal-Atile N. Evaluation of endocan and endoglin levels in chronic kidney disease due to diabetes mellitus. Arch Med Sci. 2019;15:86–91. doi: 10.5114/aoms.2018.79488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Kundi H, Balun A, Cicekcioglu H, Karayigit O, Topcuoglu C, Kilinckaya MF, Kiziltunc E, Cetin M, Ornek E. Admission endocan level may be a useful predictor for in-hospital mortality and coronary severity index in patients with ST-segment elevation myocardial infarction. Angiology. 2017;68:46–51. doi: 10.1177/0003319716646932. [DOI] [PubMed] [Google Scholar]
- 185.Qiu CR, Fu Q, Sui J, Zhang Q, Wei P, Wu Y, Zhu K, Lu Y, Zong B. Serum endothelial cell-specific molecule 1 (endocan) levels in patients with acute myocardial infarction and its clinical significance. Angiology. 2017;68:354–359. doi: 10.1177/0003319716651349. [DOI] [PubMed] [Google Scholar]
- 186.Ziaee M, Mashayekhi S, Ghaffari S, Mahmoudi J, Sarbakhsh P, Garjani A. Predictive value of endocan based on TIMI risk score on major adverse cardiovascular events after acute coronary syndrome. Angiology. 2019;70:952–959. doi: 10.1177/0003319718815241. [DOI] [PubMed] [Google Scholar]
- 187.Klisić A, Kavarić N, Abenavoli L, Stanišić V, Spasojević-Kalimanovska V, Kotur-Stevuljević J, Ninić A. Is endocan a novel potential biomarker of liver steatosis and fibrosis? J Med Biochem. 2020;39:363–371. doi: 10.2478/jomb-2019-0042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Arman Y, Akpinar TS, Kose M, Emet S, Yuruyen G, Akarsu M, Ozcan M, Yegit O, Cakmak R, Altun O, Aydin S, Alibeyoğlu A, Ugurlu B, Akcan T, Tukek T. Effect of glycemic regulation on endocan levels in patients with diabetes: a preliminary study. Angiology. 2016;67:239–244. doi: 10.1177/0003319715585664. [DOI] [PubMed] [Google Scholar]
- 189.Klisić A, Kavaric N, Stanisic V, Vujcic S, Spasojevic-Kalimanovska V, Ninic A, Kotur-Stevuljevic J. Endocan and a novel score for dyslipidemia, oxidative stress and inflammation (DOI score) are independently correlated with glycated hemoglobin (HbA1c) in patients with prediabetes and type 2 diabetes. Arch Med Sci. 2020;16:42–50. doi: 10.5114/aoms.2019.87541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Lv Y, Zhang Y, Shi W, Liu J, Li Y, Zhou Z, He Q, Wei S, Liu J, Quan J. The association between endocan levels and subclinical atherosclerosis in patients with type 2 diabetes mellitus. Am J Med Sci. 2017;353:433–438. doi: 10.1016/j.amjms.2017.02.004. [DOI] [PubMed] [Google Scholar]
- 191.Balta S, Demirkol S, Ozturk C, Yildirim AO, Demir M, Celik T. The relation between endocan levels and subclinic atherosclerosis. Clin Appl Thromb Hemost. 2016;22:495–496. doi: 10.1177/1076029616639701. [DOI] [PubMed] [Google Scholar]
- 192.He XW, Ke SF, Bao YY, Hong WJ, Shen YG, Li C, Zhu F, Wang E, Jin XP. Serum levels of endocan and endoglin are associated with large-artery atherosclerotic stroke. Clin Chim Acta. 2018;478:157–161. doi: 10.1016/j.cca.2017.12.040. [DOI] [PubMed] [Google Scholar]
- 193.Oktar SF, Guney I, Eren SA, Oktar L, Kosar K, Buyukterzi Z, Alkan E, Biyik Z, Erdem SS. Serum endocan levels, carotid intima-media thickness and microalbuminuria in patients with newly diagnosed hypertension. Clin Exp Hypertens. 2019;41:787–794. doi: 10.1080/10641963.2019.1652632. [DOI] [PubMed] [Google Scholar]
- 194.Poon PY, Ng JK, Fung WW, Chow KM, Kwan BC, Li PK, Szeto CC. Relationship between plasma endocan level and clinical outcome of Chinese peritoneal dialysis patients. Kidney Blood Press Res. 2019;44:1259–1270. doi: 10.1159/000502961. [DOI] [PubMed] [Google Scholar]
- 195.Bar A, Targosz-Korecka M, Suraj J, Proniewski B, Jasztal A, Marczyk B, Sternak M, Przybyło M, Kurpińska A, Walczak M, Kostogrys RB, Szymonski M, Chlopicki S. Degradation of glycocalyx and multiple manifestations of endothelial dysfunction coincide in the early phase of endothelial dysfunction before atherosclerotic plaque development in apolipoprotein E/low-density lipoprotein receptor-deficient mice. J Am Heart Assoc. 2019;8:e011171. doi: 10.1161/JAHA.118.011171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Kartik Kumar S, Muthusamy S, Kadhirvel S, Mani KP. In-silico and invitro analysis of endocan interaction with statins. Int J Biol Macromol. 2020;146:1087–1099. doi: 10.1016/j.ijbiomac.2019.09.235. [DOI] [PubMed] [Google Scholar]
- 197.Efe SC, Demirci K, Ozturk S, Gurbuz AS, Poci N, Kilicgedik A, Guler A, Yilmaz MF, Izgi IA, Kirma C. Serum endocan levels in patients with cardiac syndrome X. Herz. 2018;43:359–363. doi: 10.1007/s00059-017-4580-3. [DOI] [PubMed] [Google Scholar]
- 198.Pennathur S, Heinecke JW. Oxidative stress and endothelial dysfunction in vascular disease. Curr Diab Rep. 2007;7:257–264. doi: 10.1007/s11892-007-0041-3. [DOI] [PubMed] [Google Scholar]
- 199.Tsimikas S. Oxidative biomarkers in the diagnosis and prognosis of cardiovascular disease. Am J Cardiol. 2006;98:9P–17P. doi: 10.1016/j.amjcard.2006.09.015. [DOI] [PubMed] [Google Scholar]
- 200.Ferratini M, Ripamonti V, Masson S, Grati P, Racca V, Cuccovillo I, Raimondi E, Capomolla S, Macchi C, Coruzzi P, Vago T, Calvo M, Mantovani A, Latini R. Pentraxin-3 predicts functional recovery and 1-year major adverse cardiovascular events after rehabilitation of cardiac surgery patients. J Cardiopulm Rehabil Prev. 2012;32:17–24. doi: 10.1097/HCR.0b013e31823be0f4. [DOI] [PubMed] [Google Scholar]
- 201.Golubnitschaja O, Liskova A, Koklesova L, Samec M, Biringer K, Büsselberg D, Podbielska H, Kunin AA, Evsevyeva ME, Shapira N, Paul F, Erb C, Dietrich DE, Felbel D, Karabatsiakis A, Bubnov R, Polivka J, Polivka J, Jr, Birkenbihl C, Fröhlich H, Hofmann-Apitius M, Kubatka P. Caution, “normal” BMI: health risks associated with potentially masked individual underweight-EPMA Position Paper 2021. EPMA J. 2021;12:243–264. doi: 10.1007/s13167-021-00251-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Torres Crigna A, Link B, Samec M, Giordano FA, Kubatka P, Golubnitschaja O. Endothelin-1 axes in the framework of predictive, preventive and personalised (3P) medicine. EPMA J. 2021;12:1–41. doi: 10.1007/s13167-021-00248-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Safdar B, Guo X, Johnson C, D'Onofrio G, Dziura J, Sinusas AJ, Testani J, Rao V, Desir G. Elevated renalase levels in patients with acute coronary microvascular dysfunction - a possible biomarker for ischemia. Int J Cardiol. 2019;279:155–161. doi: 10.1016/j.ijcard.2018.12.061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Goshua G, Pine AB, Meizlish ML, Chang CH, Zhang H, Bahel P, Baluha A, Bar N, Bona RD, Burns AJ, Dela Cruz CS, Dumont A, Halene S, Hwa J, Koff J, Menninger H, Neparidze N, Price C, Siner JM, Tormey C, Rinder HM, Chun HJ, Lee AI. Endotheliopathy in COVID-19-associated coagulopathy: evidence from a single-centre, cross-sectional study. Lancet Haematol. 2020;7:e575–e582. doi: 10.1016/S2352-3026(20)30216-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Smadja DM, Guerin CL, Chocron R, Yatim N, Boussier J, Gendron N, Khider L, Hadjadj J, Goudot G, Debuc B, Juvin P, Hauw-Berlemont C, Augy JL, Peron N, Messas E, Planquette B, Sanchez O, Charbit B, Gaussem P, Duffy D, Terrier B, Mirault T, Diehl JL. Angiopoietin-2 as a marker of endothelial activation is a good predictor factor for intensive care unit admission of COVID-19 patients. Angiogenesis. 2020;23:611–620. doi: 10.1007/s10456-020-09730-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Guervilly C, Burtey S, Sabatier F, Cauchois R, Lano G, Abdili E, Daviet F, Arnaud L, Brunet P, Hraiech S, Jourde-Chiche N, Koubi M, Lacroix R, Pietri L, Berda Y, Robert T, Degioanni C, Velier M, Papazian L, Kaplanski G, Dignat-George F. Circulating endothelial cells as a marker of endothelial injury in severe COVID -19. J Infect Dis. 2020;222:1789–1793. doi: 10.1093/infdis/jiaa528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Mahajan K. Microparticles in atherosclerosis: biomarkers of disease. J Clin Exp Cardiolog. 2015;6:1. doi: 10.4172/2155-9880.1000356. [DOI] [Google Scholar]
- 208.Boulanger CM, Loyer X, Rautou PE, Amabile N. Extracellular vesicles in coronary artery disease. Nat Rev Cardiol. 2017;14:259–272. doi: 10.1038/nrcardio.2017.7. [DOI] [PubMed] [Google Scholar]
- 209.Hoyer FF, Nickenig G, Werner N. Microparticles-messengers of biological information. J Cell Mol Med. 2010;14:2250–2256. doi: 10.1111/j.1582-4934.2010.01114.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.Jansen F, Yang X, Baumann K, Przybilla D, Schmitz T, Flender A, Paul K, Alhusseiny A, Nickenig G, Werner N. Endothelial microparticles reduce ICAM-1 expression in a microRNA-222-dependent mechanism. J Cell Mol Med. 2015;19:2202–2214. doi: 10.1111/jcmm.12607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.Coronado-Velázquez D, Betanzos A, Serrano-Luna J, Shibayama M. An in vitro model of the blood-brain barrier: Naegleria fowleri affects the tight junction proteins and activates the microvascular endothelial cells. J Eukaryot Microbiol. 2018;65:804–819. doi: 10.1111/jeu.12522. [DOI] [PubMed] [Google Scholar]
- 212.Wang Y, Liu J, Chen X, Sun H, Peng S, Kuang Y, Pi J, Zhuang T, Zhang L, Yu Z, Tomlinson B, Chan P, Chen Y, Zhang Y, Li Y. Dysfunctional endothelial-derived microparticles promote inflammatory macrophage formation via NF-кB and IL-1β signal pathways. J Cell Mol Med. 2019;23:476–486. doi: 10.1111/jcmm.13950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Werner N, Wassmann S, Ahlers P, Kosiol S, Nickenig G. Circulating CD31+/annexin V+ apoptotic microparticles correlate with coronary endothelial function in patients with coronary artery disease. Arterioscler Thromb Vasc Biol. 2006;26:112–116. doi: 10.1161/01.ATV.0000191634.13057.15. [DOI] [PubMed] [Google Scholar]
- 214.Berckmans RJ, Nieuwland R, Böing AN, Romijn FP, Hack CE, Sturk A. Cell-derived microparticles circulate in healthy humans and support low grade thrombin generation. Thromb Haemost. 2001;85:639–646. doi: 10.1055/s-0037-1615646. [DOI] [PubMed] [Google Scholar]
- 215.Williams MS, Rogers HL, Wang NY, Ziegelstein RC. Do platelet-derived microparticles play a role in depression, inflammation, and acute coronary syndrome? Psychosomatics. 2014;55:252–260. doi: 10.1016/j.psym.2013.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Toth B, Liebhardt S, Steinig K, Ditsch N, Rank A, Bauerfeind I, Spannagl M, Friese K, Reininger AJ. Platelet-derived microparticles and coagulation activation in breast cancer patients. Thromb Haemost. 2008;100:663–669. doi: 10.1160/TH07-10-0602. [DOI] [PubMed] [Google Scholar]
- 217.Mezouar S, Mege D, Darbousset R, Farge D, Debourdeau P, Dignat-George F, Panicot-Dubois L, Dubois C. Involvement of platelet-derived microparticles in tumor progression and thrombosis. Semin Oncol. 2014;41:346–358. doi: 10.1053/j.seminoncol.2014.04.010. [DOI] [PubMed] [Google Scholar]
- 218.Brill A, Dasheysky O, Rivo J, Gozal Y, Varon D. Platelet derived microparticles induce angiogenesis and stimulate post-ischemic revascularization. Cardiovasc Res. 2005;67:30–38. doi: 10.1016/j.cardiores.2005.04.007. [DOI] [PubMed] [Google Scholar]
- 219.Diehl P, Aleker M, Helbing T, Sossong V, Germann M, Sorichter S, Bode C, Moser M. Increased platelet, leukocyte and endothelial microparticles predict enhanced coagulation and vascular inflammation in pulmonary hypertension. J Thromb Thrombolysis. 2011;31:173–179. doi: 10.1007/s11239-010-0507-z. [DOI] [PubMed] [Google Scholar]
- 220.Ogata N, Imaizumi M, Nomura S, Shozu A, Arichi M, Matsuoka M, Matsumura M. Increased levels of platelet-derived microparticles in patients with diabetic retinopathy. Diabetes Res Clin Pract. 2005;68:193–201. doi: 10.1016/j.diabres.2004.10.010. [DOI] [PubMed] [Google Scholar]
- 221.Wen B, Combes V, Bonhoure A, Weksler BB, Couraud PO, Grau GE. Endotoxin-induced monocytic microparticles have contrasting effects on endothelial inflammatory responses. PLoS ONE. 2014;9:e91597. doi: 10.1371/journal.pone.0091597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Wang JG, Williams JC, Davis BK, Jacobson K, Doerschuk CM, Ting JP, Mackman N. Monocytic microparticles activate endothelial cells in an IL-1β-dependent manner. Blood. 2011;118:2366–2374. doi: 10.1182/blood-2011-01-330878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223.Hoyer FF, Giesen MK, França CN, Lütjohann D, Nickenig G, Werner N. Monocytic microparticles promote atherogenesis by modulating inflammatory cells in mice. J Cell Mol Med. 2012;16:2777–2788. doi: 10.1111/j.1582-4934.2012.01595.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing is not applicable to this article as no datasets were generated or analysed during the current study.
Not applicable.