Abstract
Background
A One Health approach has been increasingly mainstreamed by the international community, as it provides for holistic thinking in recognizing the close links and inter-dependence of the health of humans, animals and the environment. However, the dearth of real-world evidence has hampered application of a One Health approach in shaping policies and practice. This study proposes the development of a potential evaluation tool for One Health performance, in order to contribute to the scientific measurement of One Health approach and the identification of gaps where One Health capacity building is most urgently needed.
Methods
We describe five steps towards a global One Health index (GOHI), including (i) framework formulation; (ii) indicator selection; (iii) database building; (iv) weight determination; and (v) GOHI scores calculation. A cell-like framework for GOHI is proposed, which comprises an external drivers index (EDI), an intrinsic drivers index (IDI) and a core drivers index (CDI). We construct the indicator scheme for GOHI based on this framework after multiple rounds of panel discussions with our expert advisory committee. A fuzzy analytical hierarchy process is adopted to determine the weights for each of the indicators.
Results
The weighted indicator scheme of GOHI comprises three first-level indicators, 13 second-level indicators, and 57 third-level indicators. According to the pilot analysis based on the data from more than 200 countries/territories the GOHI scores overall are far from ideal (the highest score of 65.0 out of a maximum score of 100), and we found considerable variations among different countries/territories (31.8–65.0). The results from the pilot analysis are consistent with the results from a literature review, which suggests that a GOHI as a potential tool for the assessment of One Health performance might be feasible.
Conclusions
GOHI—subject to rigorous validation—would represent the world’s first evaluation tool that constructs the conceptual framework from a holistic perspective of One Health. Future application of GOHI might promote a common understanding of a strong One Health approach and provide reference for promoting effective measures to strengthen One Health capacity building. With further adaptations under various scenarios, GOHI, along with its technical protocols and databases, will be updated regularly to address current technical limitations, and capture new knowledge.
Graphical Abstract
Supplementary Information
The online version contains supplementary material available at 10.1186/s40249-022-00979-9.
Keywords: Antimicrobial resistance, Cell-like framework, Climate change, Food security, Global One Health index (GOHI), Global performance assessment, Governance, Zoonotic diseases
Background
Over the past 20 years, the world has encountered several major public health emergencies caused by zoonotic diseases, including severe acute respiratory syndrome (SARS; 2002–2004), Ebola virus disease in West Africa (2013–2016), Zika virus in the Americas (2015–2016), and the ongoing coronavirus disease 2019 (COVID-19) pandemic. Since 1970, zoonotic diseases have accounted for more than 75% of emerging and re-emerging infectious diseases, leading to 2.5 billion infections and 2.7 million deaths each year [1]. As of the end of February 2022, there have been about 440 million confirmed cases of COVID-19, including 5.98 million deaths [2]. While humans have never possessed such a sophisticated arsenal of technologies for surveillance, prevention, treatment and management of diseases as they have available today, the threats of outbreaks of emerging and remerging zoonotic infectious diseases are very real indeed. As highlighted by the COVID-19 pandemic, the lack of cross-cooperation among human, animal and environmental/ecosystem health agencies results in great difficulty in early detection, prevention and containment of epidemics [3, 4].
A One Health approach has been suggested to address complex global health problems at the human–animal–environment interface, coupled with inter- and trans-disciplinary involvement, and transnational collaboration. On December 1, 2021, the Food and Agriculture Organization of the United Nations (FAO), the World Organization for Animal Health (OIE), the World Health Organization (WHO) and the United Nations Environment Programme (UNEP)’s One Health High-Level Expert Panel (OHHLEP) formally defined One Health as “an integrated, unifying approach that aims to sustainably balance and optimize the health of people, animals and ecosystems” [5]. In this definition, we consider that “optimize” refers to a Pareto improvement [6] of the whole system at human–animal–environment interface. Specifically, without sacrificing the benefits of any one of the three (human health, animal health and environmental health), at least one aspect or the human–animal–environment system as a whole is made better [7–9]. Or, with the same effectiveness obtained, the cost of the intervention is reduced, and hence, a higher cost-effectiveness could be achieved [10]. In such a process, a closer cooperation of different sectors is crucial.
In response to the 2002–2004 outbreak of SARS and H5N1 avian influenza, which generated global attention, the World Wildlife Conservation Association officially proposed the concept of One Health and released the Manhattan Twelve Principles encapsulating this approach [11]. In 2005, The Lancet published its first reference to “One Health” in an article about the cooperation between human and animal health to strengthen health systems [12]. In 2008, FAO, OIE, WHO, UNICEF, The World Bank and the United Nations System Influenza Coordination (UNSIC) officially suggested One Health as the approach to deal with global epidemics [13]. In 2009, funded by the Rockefeller Foundation, the One Health Commission was established with the objective of disseminating the One Health approach more widely [14]. In 2020, the OHHLEP was jointly established by FAO, OIE, WHO and UNEP, to provide expert technical guidance on key scientific issues in One Health [15]. At the behest of the international community, countries including the United Kingdom and the United States of America established specific government entities or initiatives [16, 17] to lead administrative coordination, fundraising and policy-making relevant to One Health promotion.
Based on a summary of previous literature, we consider that a One Health approach implies an integrated and unifying approach on several levels: firstly, it unifies human health, animal health and environment health with the aim of achieving the Pareto improvement for human–animal–environment systems [18, 19]; secondly, it mobilizes cross-sectoral and multi-disciplinary cooperation by breaking down barriers in governance [20]; thirdly, it promotes joint cooperation between countries and regions to tackle threats at global, regional and local levels, such as pandemic preparedness and response, climate change, etc. [21]; and fourthly, it promotes broader societal participation and better societal awareness for the sustainable development of human–animal–environment systems [22].
Although the One Health approach has been well-recognized [23], its determinants and practical enablers have yet to be clarified. The dearth of real-world evidence has hindered the identification of gaps in the human–animal–environment health nexus, which hampers the application of a One Health approach in shaping policies and practice. A well-constructed conceptual system, along with an appropriate evaluation scheme, is needed to better understand the current situation and to set goals and strategies for One Health implementation, readily tailored to specific social-ecological settings.
Recognizing this challenge, we propose five steps towards development of a global One Health index (GOHI) as a potential tool for the systematic evaluation of One Health performance. In a next step, our proposed GOHI needs to be validated. A rigorously validated GOHI might then help improve the application of a One Health approach globally. We hope that our proposal and frame of a GOHI will be used to promote effective measures to fill the gaps in One Health practice of each country/territory and promote a wider application of One Health approaches in shaping real-world policies and practices.
In this paper, we describe the essentials of One Health, propose a conceptual framework for GOHI and construct a weighted indicator scheme. With the adaptation of a mixed-methods approach that combines a qualitative assessment with quantitative evaluation, we build up the GOHI database and test the GOHI tool with a pilot analysis on the global performance of One Health.
Methods
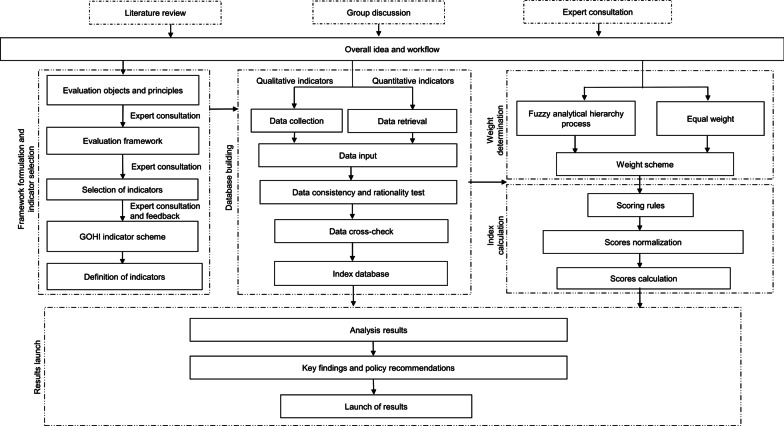
GOHI is constructed in five steps, including (i) framework formulation; (ii) indicator selection; (iii) database building; (iv) weight determination; and (v) GOHI scores calculation (Fig. 1).
Fig. 1.
Flowchart for the construction of a global One Health index (GOHI)
Expert advisory committee
To ensure the reliability of the index, we are committed to incorporating the opinions of experts and have established a GOHI expert advisory committee (Table 1).
Table 1.
Characteristics of the expert advisory committee assisting with the development of a global One Health index (GOHI) [n=29]
| Item | Category | Counts | Percentage (%) |
|---|---|---|---|
| Gender | Male | 16 | 55.2 |
| Female | 13 | 44.8 | |
| Age (years) | 21–30 | 6 | 20.7 |
| 31–40 | 12 | 41.4 | |
| 41–50 | 8 | 27.6 | |
| > 50 | 3 | 10.3 | |
| Education | Doctoral degree | 20 | 69.0 |
| Master degree | 9 | 31.0 | |
| Bachelor degree | 0 | 0.0 | |
| College degree | 0 | 0.0 | |
| Other | 0 | 0.0 | |
| Professional level | Senior level | 10 | 34.5 |
| Vice-senior level | 8 | 27.6 | |
| Middle level | 9 | 31.0 | |
| Primary level | 2 | 6.9 | |
| Type of work | Medical institutions | 11 | 37.9 |
| Colleges and Universities | 15 | 51.7 | |
| Governments | 3 | 10.3 | |
| Working experience (in years) | < 10 years | 14 | 48.3 |
| 10–20 years | 8 | 27.6 | |
| > 20 years | 7 | 24.1 | |
| Primary research area | Human medicine | 12 | 41.4 |
| Veterinary science | 7 | 24.1 | |
| Environmental science | 7 | 24.1 | |
| Social science | 1 | 3.4 | |
| Political science | 1 | 3.4 | |
| Management science | 1 | 3.4 | |
| Secondary research area | Human medicine | 7 | 24.1 |
| Veterinary science | 1 | 3.4 | |
| Environmental science | 1 | 3.4 | |
| Social science | 3 | 10.3 | |
| Political science | 3 | 10.3 | |
| Management science | 5 | 17.2 |
*The committee expansion is under way
The School of Global Health, Chinese Center for Tropical Diseases Research, Shanghai Jiao Tong University School of Medicine, maintains a database of cooperating partners with expertise in relevant research fields. To construct the GOHI expert advisory committee, we selected 10 experts from the expert database by convenience sampling based on professional expertise, research relevance and willingness to participate. Then, we continued to include more experts through snowball sampling, and eventually built up an expert advisory committee of 29 experts from the areas of human medicine, veterinary science, environmental science, social science, political science and management science.
Index framework formulation
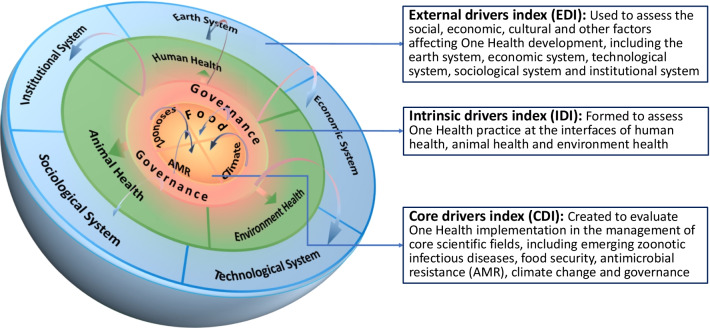
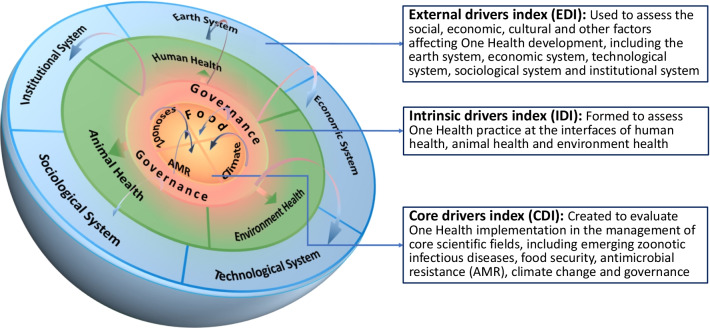
In developing the index framework, we assume three essential components of a One Health approach. Firstly, One Health recognizes the close links among human health, animal health and environment health, and mobilizes multiple sectors, disciplines and communities at varying levels of society; secondly, the use of a One Health approach represents more holistic thinking. In the process of dealing with increasingly complex global health problems, many factors, such as social, cultural, economic and natural factors, should be considered, especially their influence on the human–animal–environment nexus; thirdly, a One Health approach promotes the coordinated development of human–animal–environment systems and improve the ability to more effectively address global challenges.
Based on these essentials of One Health, we use a three-layer structure of external, intrinsic and core layers as the basis of our proposed evaluation framework, which implies structure–process–outcome thinking [24]. The external layer of One Health is to provide a facilitating environment for One Health’s development; the intrinsic layer of One Health composes elements for the integrated development of human–animal–environment system; and the core layer consists of components in the response to the challenges of One Health key issues.
Therefore, a cell-like framework of GOHI (Fig. 2) has been developed, which comprises an external drivers index (EDI), an intrinsic drivers index (IDI) and a core drivers index (CDI). The EDI is used to assess the social, economic, cultural and other factors affecting One Health development, including the earth system, economic system, technological system, sociological system and institutional system [25]. The IDI is formed to assess One Health practice at the interfaces of human health, animal health and environment health. The CDI is created to evaluate One Health implementation in the management of core scientific fields, including emerging zoonotic infectious diseases, food security, antimicrobial resistance (AMR), climate change and governance.
Fig. 2.
Cell-like framework of global One Health index (GOHI)
The selection of the core scientific fields of CDI is mainly based on literature reviews. The report entitled “Contributing to One World, One Health: a strategic framework for reducing risks of infectious diseases at the animal-human-environment interface” jointly released by FAO, OIE, WHO, UNICEF, The World Bank and the UNSIC [26], has identified these core issues at the animal–human–ecosystem interface, including zoonoses, food security, AMR and climate change. The journal Nature published a comment put forth by Kahn [18], which took environmental hazards, infectious diseases and AMR as typical applications of One Health. Another comment, recently published in The Lancet [27], summarized key dimensions of One Health as shared environment, safe food and food systems and shared medicines and intervention, and proposed that these challenges could be further impacted by climate change. Moreover, the role of governance in establishing interdisciplinary and interdepartmental mechanisms for the integrated development of human–animal–environment system has also been elaborated in the literature [28].
Indicator selection
The indicators are selected according to the principles of relevance, authoritative sources, open access, completeness, timeliness, comparability and country-level data (Table 2). Based on the established cell-like framework, we have conducted four rounds of expert advisory committee consultations and several key infomant interviews with experts from multiple UN agencies, including four experts from WHO, two from The World Bank and one each from FAO and World Meteorological Organization (WMO). In the first round, we determined the core data sources based on the main principles for constructing the indicator scheme, and started a large-scale collection of data for indicators. In the second round, we reorganized the indicator scheme based on the collected indicators, and determined the frame of the first-, second- and third-level indicators. In the third round, we explored strategies for integrating indicators and condense the number of indicators. In the fourth round, we discussed the demonstration of the agreed indicator scheme.
Table 2.
Data selection criteria for developing a global One Health index (GOHI)
| Principle | Criteria |
|---|---|
| Relevance | Data should represent the content of corresponding indicators |
| Authoritative sources | Data are retrieved from authoritative global/countries agencies |
| Open access | Data are available from public open sources with transparent collecting/statistical methods and high level of integrity |
| Completeness | Data used for indicators should cover a sufficient number of countries/territories |
| Timeliness | Data should cover recent temporal period and are updated annually |
| Comparability | For single indicator, data should be measured with an established and unified method and peer-reviewed across countries/territories |
| Country-level data | Data should describe the status of indicators at country-level |
Database building
Data generated between 2016 and 2020 were collected for each indicator and used to construct the GOHI database. Our data were mainly extracted from authoritative databases (Table 3). We also developed a few self-designed indicators which were constituted by structured questions, the answers to which were found from results of searching websites or open-access sources by our research team. To ensure quality of the data, we performed cross-checking and consistency testing for data collection.
Table 3.
Data sources utilized for the development of a global One Health index (GOHI)
| Category | Sources |
|---|---|
| External drivers index (EDI) | Databases from FAO, Organization for Economic Cooperation and Development (OECD), The World Bank, Our World in Data, International Energy Agency (IEA), International Telecommunication Union (ITU) |
| Intrinsic drivers index (IDI) | Databases from Sustainable Development Goals (SDGs), WHO-The Global Health Observatory, IHME-Global Burden of Disease (GBD), The World Bank, Environmental Performance Index (EPI), FAO, Global Ocean Health Index scores, Our World in Data |
| Core drivers index (CDI) | |
| Governance | Data from SDGs The World Bank, government website portal |
| Zoonotic diseases | Data from WHO, OIE, The World Bank, Global Health Security Index (GHS), GHDx |
| Food security | Data from FAO, The World Bank, WHO, UN, UNHCR, UNEP |
| Antimicrobial resistance | Data from global antimicrobial resistance and use surveillance system (GLASS), GHS, Tripartite AMR Country Self-Assessment Survey (TrACSS), European Centre for Disease Prevention and Control, The Pan American Health Organization (PAHO)/WHO |
| Climate change | Data from The World Bank, Lancet Countdown, Our World in Data, OECD.Stat |
Weight determination
A fuzzy analytical hierarchy process (FAHP) [29] was adopted to assign the weights for most of the indicators. We used a fuzzy comparison matrix based on the judgments of different experts to generate the weight matrix of indicators. We conducted two rounds of investigations among our expert advisory committee and collected the experts’ opinions by several rounds of interrogation on the comparison of relative importance between indicators. The details on weight determination are described in Additional file 1.
Data preprocessing
For missing data, we interpolated missing values using the mean of the counterparts from three countries with the most similar conditions. If the data of the indicator were missing for more than 160 countries, the indicator was excluded from the calculation; if the country’s data missing rate exceeded 50% in EDI, IDI or any of the five dimensions in CDI (governance, zoonotic diseases, food security, AMR and climate change), the country was excluded from the calculation.
The choice of the missing rate threshold for the inclusion of countries/territories in GOHI was made based on the consideration of prevalent data incompleteness and the number of countries/territories that could be included. GOHI devotes to include as many countries/territories as possible as it aims to provide reference for every country/territory around the world in One Health promotion. However, due to inherent data scarcity, if strict threshold of data missing rate (e.g., 15%) was adopted, most countries/territories would be excluded (in our database, with the threshold of 50% data missing rate, the number of countries/territories included was 146; with the threshold of 15% data missing rate, the number of countries/territories included would have been reduced to only 6). Therefore, we chose a data missing rate of 50% as the inclusion threshold.
For those indicators with values of 0 or 1, we took measures to deal with the bias from over-polarization. For the value 0, we replaced it with a positive number sampled from the normal distribution N(0, 0.162); for the value 1, we replaced it with a number less than 1 sampled from the normal distribution N(1, 0.162). By using the method of continuous processing of discrete random variable, the possible bias from some indicators with only 0 or 1 can be reduced when calculating the weights of our GOHI indicators.
GOHI score calculation
We believe that good One Health performance requires the following: it needs to have a facilitating external environment for development, which should be indicated by a high EDI score; meanwhile, it needs to perform well in the three areas of human health, animal health and environmental health, which should drive a high IDI score; moreover, it needs to be able to cope with the challenges in core issues of a One Health approach, including zoonosis prevention and control, achieving food security, managing AMR, mitigating and adapting to climate change, which–collectively–would be indicated by a high CDI score.
Hence, based on the logic of evaluating One Health performance, the EDI, IDI and CDI scores are weighted and summed to obtain the final total score of GOHI.
For each sub-indicator, we set the best/worst value for it, and used the following equation to normalize the sub-indicator [30, 31]:
where denotes the normalized score for j-th sub-indicator of i-th country; denotes the original values for j-th sub-indicator of i-th country; denotes the original values of best performance for j-th sub-indicator; denotes the original values of worst performance for j-th sub-indicator.
The weighted sum of the scores of the lower level indicators was derived from the following equation to obtain the scores of the upper level indicators:
where denotes the total number of the sub-indicators under h-th indicator; denotes the j-th sub-indicator under h-th indicator; denotes the score of -th sub-indicator in i-th country; denotes the weight of -th sub-indicator.
Framework validation
We used the most recently available data from GOHI database to conduct a pilot analysis of One Health performance at the global, regional and dimensional level. We compared the results from GOHI with findings from the literature, in order to validate the feasibility of our tool.
Results
GOHI indicator and weight scheme
The indictor scheme for GOHI comprises of three first-level indicators, 13 second-level indicators and 57 third-level indicators (Fig. 3). The first- and second-level indicators were determined based on our cell-like framework; the third-level indicators were determined from an extensive literature review and panel discussions with our expert advisory committee. For the indicators A1‒A5, B1‒B3, C3.1‒C3.5 and C4.1‒C4.5, equal weights were assigned as they are assumed to be equally important as their peer indicators; for the other indicators, FAHP was used to determine the weights assigned. Table 4 shows the indicator and weight scheme of GOHI. The full details of the indicators and weights of GOHI are shown in Additional file 2.
Fig. 3.
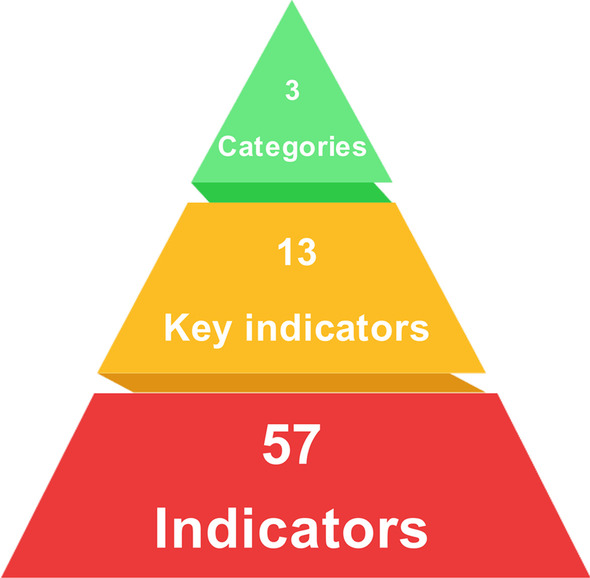
Indicator structure of a global One Health index (GOHI). Categories, Key indicators and Indicators in the figure are comparable to the first-level, second-level and third-level indicators presented in the text, respectively
Table 4.
Indicator and weight scheme of our proposed global One Health index (GOHI)
| Category | Weight (%) | Key indicator | Weight (%) | Indicator | Weight (%) |
|---|---|---|---|---|---|
| A External drivers index (EDI) | 15.2 | A1 Earth system | 20.0 | A1.1 Land | 18.7 |
| A1.2 Forest | 18.3 | ||||
| A1.3 Water | 23.7 | ||||
| A1.4 Air | 22.8 | ||||
| A1.5 Natural disasters | 16.6 | ||||
| A2 Institutional system | 20.0 | A2.1 Justice | 45.5 | ||
| A2.2 Governance | 54.5 | ||||
| A3 Economic system | 20.0 | A3.1 Finance | 37.7 | ||
| A3.2 Work | 30.4 | ||||
| A3.3 Housing | 31.9 | ||||
| A4 Sociological system | 20.0 | A4.1 Demography | 33.0 | ||
| A4.2 Education | 37.7 | ||||
| A4.3 Inequalities | 29.3 | ||||
| A5 Technological system | 20.0 | A5.1 Transport | 30.8 | ||
| A5.2 Technology adoption | 35.1 | ||||
| A5.3 Consumption and production | 34.1 | ||||
| B Intrinsic drivers index (IDI) | 16.3 | B1 Human health | 33.3 | B1.1 Reproductive, maternal, new-born and child health | 20.6 |
| B1.2 Infectious diseases | 19.5 | ||||
| B1.3 Non-communicable diseases and mental health | 15.9 | ||||
| B1.4 Injuries and violence | 13.5 | ||||
| B1.5 Universal health coverage and health systems | 17.5 | ||||
| B1.6 Health risk | 13.0 | ||||
| B2 Animal health and ecosystem diversity | 33.3 | B2.1 Animal epidemic diseases | 31.9 | ||
| B2.2 Animal welfare | 24.7 | ||||
| B2.3 Animal nutritional status | 17.4 | ||||
| B2.4 Animal biodiversity | 26.1 | ||||
| B3 Environmental health | 33.3 | B3.1 Air quality and climate change | 23.8 | ||
| B3.2 Land resources | 19.6 | ||||
| B3.3 Sanitation and water resources | 20.7 | ||||
| B3.4 Hazardous chemicals | 17.5 | ||||
| B3.5 Environmental biodiversity | 18.4 | ||||
| C Core drivers index (CDI) | 68.5 | C1 Governance | 21.7 | C1.1 Participation | 11.0 |
| C1.2 Rule of law | 15.8 | ||||
| C1.3 Transparency | 10.0 | ||||
| C1.4 Responsiveness | 12.6 | ||||
| C1.5 Consensus oriented | 10.8 | ||||
| C1.6 Equity and inclusiveness | 13.8 | ||||
| C1.7 Effectiveness and efficiency | 13.2 | ||||
| C1.8 Political support | 12.9 | ||||
| C2 Zoonotic diseases | 20.3 | C2.1 Source of infection | 23.7 | ||
| C2.2 Route of transmission | 25.3 | ||||
| C2.3 Targeted population | 19.1 | ||||
| C2.4 Capacity building | 16.8 | ||||
| C2.5 Outcomes (case-studies) | 15.1 | ||||
| C3 Food security | 21.4 | C3.1 Food demand and supply | 20.0 | ||
| C3.2 Food safety | 20.0 | ||||
| C3.3 Nutrition | 20.0 | ||||
| C3.4 Natural and social circumstances | 20.0 | ||||
| C3.5 Government support and response | 20.0 | ||||
| C4 Antimicrobial resistance | 18.1 | C4.1 AMR surveillance system | 20.0 | ||
| C4.2 AMR laboratory network and coordination capacity | 20.0 | ||||
| C4.3 Antimicrobial control and optimization | 20.0 | ||||
| C4.4 Improve awareness and understanding | 20.0 | ||||
| C4.5 AMR rate for important antibiotics | 20.0 | ||||
| C5 Climate change | 18.5 | C5.1 Government response | 37.9 | ||
| C5.2 Climate change risks | 29.6 | ||||
| C5.3 Health outcome | 32.5 |
GOHI pilot analysis
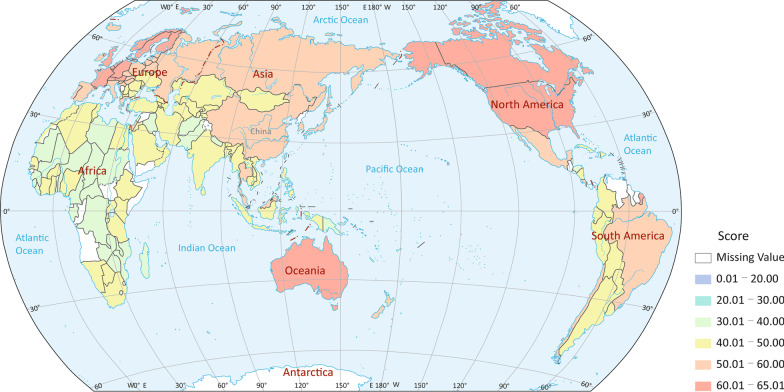
We calculated the GOHI score for the countries/territories included, and show different ranges in performance in different colours on the map in Fig. 4. Overall, the GOHI scores of countries/territories worldwide are far from optimal (100 points), with the highest score of 65.0 (Sweden). The highest score range of 60 and above mainly includes countries in North America, Europe and Oceania, while countries in Africa obtained considerably lower scores in the range of 30‒50.
Fig. 4.
Global score map of a global One Health index (GOHI). Map approval No. GS (2022) 1516. The different colors represent different GOHI score ranges, as shown in the legend
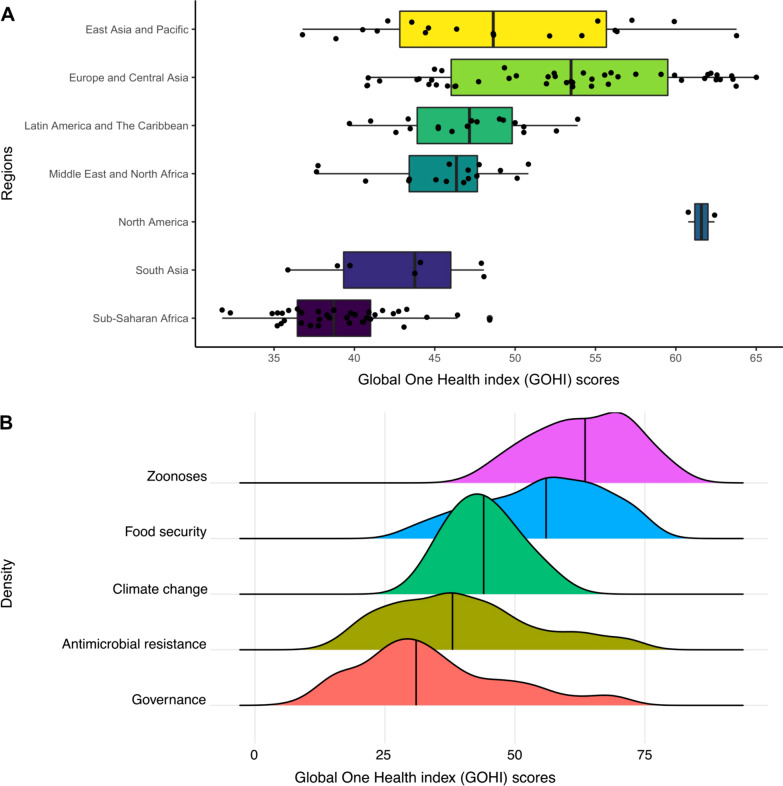
Figure 5A shows that the GOHI scores vary considerably by regions. The regions with GOHI scores, ranked according to their median (median; lower–upper bound), are as follows: North America (61.6; 60.8–62.4), Europe and Central Asia (53.5; 40.8–65.0), East Asia and Pacific (48.6; 36.8–63.8), Latin America and the Caribbean (47.2; 39.7–53.9), Middle East and North Africa (46.4; 37.6–50.8), South Asia (43.8; 35.9–48.1) and sub-Saharan Africa (38.7; 31.8–48.4). North America has the highest median, while sub-Saharan African has the lowest.
Fig. 5.
Regional (A) and dimensional (B) score distribution of a global One Health index (GOHI). A Boxplots of GOHI scores across countries by regions. B Density plots of subgroup GOHI scores across countries by five dimensions of core drivers index (CDI)
Within our framework, the CDI has five dimensions. Figure 5B shows that the dimensions of CDI with the GOHI scores ranked, according to their median, were as follows: zoonotic diseases (63.7), food security (56.3), climate change (43.6), AMR (37.8) and One Health governance (31.5). In addition, for AMR and One Health governance, the distributions of scores were wider, indicating that a large variation exists in the scores among countries/territories.
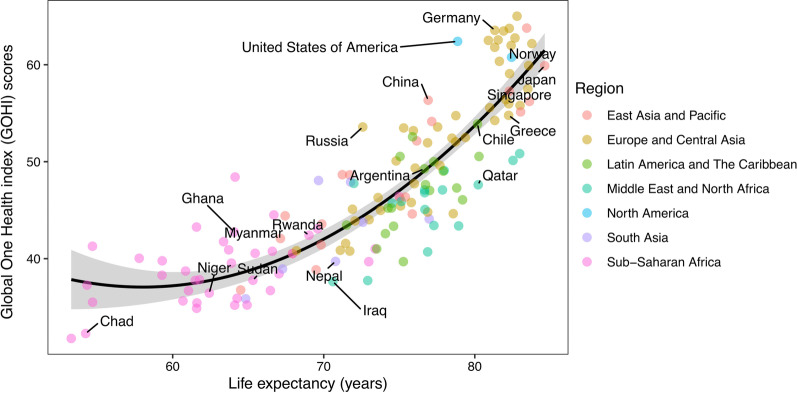
We also conducted a correlation analysis on GOHI score and average life expectancy of each country/territory. Figure 6 shows that the relationship between country GOHI score and average life expectancy was fitted well by a quadratic regression model (r = 0.76, P < 0.001).
Fig. 6.
Correlation analysis of life expectancy and a global One Health index (GOHI) score. The relationship between national GOHI scores and average life expectancy fits the quadratic regression model with adjusted R2 = 0.76 (P < 0.001)
Discussion
Towards a GOHI
The issues highlighted by our pilot analysis, including suboptimal global development, significant regional variations and weak governance capabilities in One Health, are consistent with the literature. This suggests that GOHI is capable of reflecting the current status of One Health development.
The FAO, OIE, UNEP and WHO are working together to mainstream One Health in order to better respond to global health threats and promote sustainable development. There is wide variation in other applications of One Health practices at national level. In 2014, the European Cooperation in Science and Technology funded the Network for Evaluation of One Health, dedicated to providing quantitative evaluation tools and evidence for One Health-related research and practices [16]. In 2019, the United States of America set up the One Health steering committee under FDA, officially responsible for coordinating and organizing One Health research and practice [32]. From 2021, the German government allocated 150 million Euro per annum to facilitate cross-sectoral and international cooperation in One Health [33]. Led by the Shanghai Jiao Tong University-The University of Edinburgh One Health Center and other institutions [34], China is also actively participating in the promotion of the One Health concept in health governance. In many regions, such as sub-Saharan Africa, the One Health approach has yet to be applied by policymakers.
The world is experiencing a series and overlapping challenges arising from zoonotic diseases, climate change, AMR, food insecurity, to name but a few. There is a pressing need for all countries to promote a One Health approach in decision-making practices. Weaknesses in managing AMR and in One Health governance illustrated in the pilot analysis underscore concerns identified by scholars in previous studies. According to the Tripartite AMR Country Self-Assessment Survey, jointly established by FAO, WHO and OIE in 2021 [35], 153 countries around the world have issued national action guidelines on AMR, but only 95 countries have implemented practices according to the guidelines, and more than 70 countries still lack formal cross-sectoral governance or coordination mechanisms on AMR.
The correlation analysis between national GOHI and average life expectancy highlights the potential for application of a GOHI. As an assessment tool, GOHI may be applied to predict the effect of interventions and health outcomes, which will benefit the prioritization of resource input and formulation of relevant strategies.
Potential of a GOHI
With growing needs for effective decision making, there have been several global studies on quantitative evaluation of One Health. For example, the Nuclear Threat Initiative (NTI) and Center for Health Security of the Johns Hopkins Bloomberg School of Public Health jointly developed the global health security index, which assessed 195 countries/territories for several aspects, including prevention, detection and reporting, rapid response, health system, compliance with international norms and risk environment [36]; Yale Center for Environmental Law and Policy (YCELP) and Center for International Earth Science Information Network Earth Institute jointly developed an environmental performance index, and ranked 180 countries on 32 performance indicators of environmental health and ecosystem vitality [31]. However, these studies have primarily focused on one of the components of One Health, rather than the bundle that constitutes One Health.
A number of published reports have discussed the conceptual framework for One Health evaluation. Rüegg et al. [37] analyzed the logical relationship among the elements of One Health, using a system dynamics approach and proposed a formula for the quantification of One Health. Wang et al. [38] established criteria for prioritizing zoonotic diseases, which included disease hazard/severity, epidemic scale and intensity, economic impact, prevention and control, and social impact. However, these studies have focused on the exploration of the One Health evaluation framework and methodology, without using global-level empirical data for analysis.
GOHI is the world’s first research tool that builds an evaluation framework from a holistic perspective of One Health and uses data from more than 200 countries and territories for empirical analysis. Unlike the existing global databases, which either use structured questionnaire scores (e.g. global health security index) or exclusively quantitative data (e.g. environmental performance index), GOHI combines qualitative and quantitative data with a mixed-methods approach in data collection and analysis, which makes GOHI more flexible and applicable to different situations in different countries.
Potential function of GOHI
Firstly, the introduction of the cell-like framework of GOHI provides a clear definition and promotes common understanding of the determinants and functioning of a strong One Health approach, which will serve as the conceptual foundation for policy making. Moreover, the GOHI database enhances the consistency and quality of One Health systems, including via collaboration in data transparency and information sharing.
Secondly, GOHI is able to serve as a tool for the assessment of the performance of One Health approaches at global, continental, country and sub-regional levels. It provides a means for identifying gaps and promoting the adoption of effective measures to strengthen One Health capacity building in countries/territories where it is needed most. GOHI sets out to distill examples of best practice and guides countries to identify potential weaknesses in One Health implementation. This in turn helps identify priorities for international assistance in One Health issues, which is much needed for poverty alleviation and achievement of the SDGs.
Thirdly, the CDI in GOHI focuses on emerging zoonotic infectious diseases, AMR, food security and climate change. All of the countermeasures tackling these global challenges need further development and new technologies, such as surveillance and response technologies, preparedness and early warning systems, prediction and modelling platforms. GOHI aims to support early identification of the gaps in technology development in relevant fields, particularly in the fields of infectious disease control and prevention, emergency response and preparedness and AMR monitoring and control, which are core issues in One Health practice.
Limitations
There are several limitations of our study. Firstly, in order to ensure the validity of data, we use publicly available global official data as the main data sources for GOHI, which may have resulted in limitations on the inclusion of some indicators. Due to lack of data, some sensitive indicators (such as animal disease incidence, animal disease burden, animal vaccine usage, etc.) have not been included in the analysis. In addition, when searching for data from self-designed indicators in different countries, we use English and French as the main search languages, which may introduce collection bias.
Secondly, the experts in our advisory expert committee listed in Table 1 are geographically from China, which may limit the global representativeness of the committee. Nevertheless, our research team includes several experts from international organizations and research institutions outside of China and we have conducted several key informant interviews with experts from various UN agencies during the research process, which have brought about some international perspective to our research. In the next stage of GOHI, we will include more international experts to participate in our research, in order to improve the global representativeness of our expert committee.
Thirdly, our GOHI validation is a preliminary step, which we use as a case study to illustrate potential applications. Our proposed GOHI now needs rigorous validation. For example, we may form a consensus parameter based on data modelling for the judgement of consistency between GOHI scores and previous published work on One Health.
Moreover, in follow-up research, based on the framework and database of GOHI, we plan to conduct further investigations on data mining and extensions of mathematical models, in order to analyze the performance of One Health approach in typical real-world scenarios (e.g. zoonoses control) and to what extent Pareto improvement is achieved in pursuing the overall benefit of human–animal–environment systems.
Conclusions
With the growing recognition of the intimate links of human health, animal health and environment health, a One Health approach is being increasingly applied in decision-making. The formulation of a consolidated evaluation tool is essential for the valid assessment of One Health approaches. Through consulting an expert advisory committee and the adaptation of a mixed-methods approach, we have developed a cell-like framework and a weighted three-level indicator scheme for GOHI, which needs broader validation beyond the GOHI database pursued here.
It is anticipated that GOHI along with its technical protocols, will not remain static but will evolve with more applications in research, practice and policy. Through the establishment of this tool, we aim to contribute a foundation for further improvement and rigorous validation. Moreover, the construction of GOHI has highlighted the significance of producing higher quality global One Health database, and of sharing the data with interested constituencies.
While the application of One Health approaches relies on strong political commitment, GOHI will support the implementation of One Health at national, regional and global levels. Thus far, very few countries have established a government agency specifically responsible for coordination of a One Health approach. The lack of governance mechanisms is still the biggest bottleneck in capacity building for One Health at varying levels. There is a need for a more conducive political environment to promote One Health applications, and to stimulate multi-sectoral and trans-disciplinary cooperation at global, regional and national scales.
Supplementary Information
Additional file 1. Weights calculation of global One Health index (GOHI).
Additional file 2. The indicators and weights for establishment of global One Health index (GOHI).
Acknowledgements
We specially give thanks to experts from World Health Organization, Food and Agriculture Organization of the United Nations, The World Bank, World Meteorological Organization and universities and institutions, involved in the interview for comments and suggestion.
Abbreviations
- GOHI
Global One Health index
- EDI
External drivers index
- IDI
Intrinsic drivers index
- CDI
Core drivers index
- FAHP
Fuzzy analytical hierarchy process
- SARS
Severe acute respiratory syndrome
- COVID-19
Coronavirus disease 2019
- FAO
Food and Agriculture Organization of the United Nations
- OIE
World Organization for Animal Health
- WHO
World Health Organization
- UNEP
United Nations Environment Programme
- OHHLEP
One Health High-Level Expert Panel
- UNSIC
United Nations System Influenza Coordination
- AMR
Antimicrobial resistance
- OECD
Organization for Economic Cooperation and Development
- IEA
International Energy Agency
- ITU
International Telecommunication Union
- SDGs
Sustainable Development Goals
- IHME
Institute for Health Metrics and Evaluation
- GBD
Global burden of disease
- EPI
Environmental performance index
- GHS
Global health security index
- GLASS
Global antimicrobial resistance and use surveillance system
- TrACSS
Tripartite AMR country self-assessment survey
- FDA
Food and Drug Administration
- NTI
Nuclear threat initiative
- YCELP
Yale Center for Environmental Law and Policy
Author contributions
XXZ and JSL are the co-first authors. XNZ and XKG are the co-corresponding authors. Conception and study design: XXZ, JSL, LFH, SX, XKG, XNZ. Data collection: XXZ, JSL, LFH, SX, SZL, OYL, KK, ML, KY, QQH, LSX, YZZ, LYH, XCW, YZ, HQZ, JXY, TGJ, QL, SWF, SYG, FMC, NZ, ZLC, YX, HML, JC, ZYG, JXF, LA, JBX. Data analysis: Global One Health index (GOHI) research team. Supervision: XKG, XNZ. Writing-original draft: XXZ, JSL, LFH, SX. Critique of methods, writing-review and editing: SG, LG, JXS, JU. Writing final draft: XXZ, JSL, XKG, XNZ. All authors read and approved the final manuscript.
Funding
The project was supported by China Medical Board (no. 20-365) and Shanghai Jiao Tong University Integrated Innovation Fund (no. 2020-01).
Availability of data and materials
The full study protocol and the datasets are available, following manuscript publication, upon request from the corresponding author (Xiao-Nong Zhou, zhouxn1@chinacdc.cn).
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
Xiao-Nong Zhou is an Editor-in-Chief of Infectious Diseases of Poverty. Jürg Utzinger is on the editorial board of Infectious Diseases of Poverty. Jin Chen is working at the editorial office of Infectious Diseases of Poverty. They were not involved in the peer-review or handling of the manuscript. The authors have no other competing interests to disclose.
Footnotes
Xiao-Xi Zhang and Jing-Shu Liu contributed equally to this work.
Contributor Information
Xiao-Kui Guo, Email: xkguo@shsmu.edu.cn.
Xiao-Nong Zhou, Email: zhouxn1@chinacdc.cn.
References
- 1.Centers for Disease Control and Prevention. Zoonotic diseases. 2021. https://www.cdc.gov/onehealth/basics/zoonotic-diseases.html. Accessed 24 Jan 2022.
- 2.World Health Organization. WHO COVID-19 dashboard. 2022. https://covid19.who.int. Accessed 28 Feb 2022.
- 3.Sharun K, Tiwari R, Natesan S, Dhama K. SARS-CoV-2 infection in farmed minks, associated zoonotic concerns, and importance of the One Health approach during the ongoing COVID-19 pandemic. Vet Q. 2021;41(1):50–60. doi: 10.1080/01652176.2020.1867776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Karesh W. Championing "One Health". Bull World Health Organ. 2020;98(10):652–653. doi: 10.2471/BLT.20.031020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.World Health Organization. Tripartite and UNEP support OHHLEP's definition of "One Health". 2021. https://www.who.int/news/item/01-12-2021-tripartite-and-unep-support-ohhlep-s-definition-of-one-health. Accessed 27 Dec 2021.
- 6.Mankiw NG. Principles of economics. Beijing: Peking University Press; 1999. [Google Scholar]
- 7.Zinsstag J, Waltner-Toews D, Whittaker M, Tanner M. One Health: the theory and practice of integrated health approaches. 2015. https://www.cabi.org/cabebooks/ebook/20153067399.
- 8.Karesh WB, Osofsky SA, Rocke TE, Barrows PL. Joining forces to improve our world. Conserv Biol. 2002;16(5):1432–4. doi: 10.1046/j.1523-1739.2002.01443.x. [DOI] [Google Scholar]
- 9.Morrison BL. Conservation and development interventions at the wildlife/livestock interface: implications for wildlife, livestock, and human health. J Wildl Dis. 2007;43(2):319–20. doi: 10.7589/0090-3558-43.2.319. [DOI] [Google Scholar]
- 10.Roth F, Zinsstag J, Orkhon D, Chimed-Ochir G, Hutton G, Cosivi O, et al. Human health benefits from livestock vaccination for brucellosis: case study. Bull World Health Organ. 2003;81(12):867–876. [PMC free article] [PubMed] [Google Scholar]
- 11.Wildlife Conservation Society. One World, One Health: building interdisciplinary bridges to health in a globalized world. http://www.oneworldonehealth.org/sept2004/owoh_sept04.html. Accessed 27 Jan 2022.
- 12.Zinsstag J, Schelling E, Wyss K, Mahamat MB. Potential of cooperation between human and animal health to strengthen health systems. Lancet. 2005;366(9503):2142–2145. doi: 10.1016/S0140-6736(05)67731-8. [DOI] [PubMed] [Google Scholar]
- 13.Centers for Disease Control and Prevention. History. https://www.cdc.gov/onehealth/basics/history/index.html. Accessed 27 Jan 2022.
- 14.One Health Commission. About the commission. https://www.onehealthcommission.org/en/why_one_health/about_the_commission/. Accessed 27 Jan 2022.
- 15.The United Nations Environment Programme. UNEP joins three international organizations in expert panel to improve One Health. 2020. https://unep.org/news-and-stories/story/unep-joins-three-international-organizations-expert-panel-improve-one-health. Accessed 27 Jan 2022.
- 16.Network for Evaluation of One Health. What is NEOH: an overview of the structure, activities and future plans. 2014. http://neoh.onehealthglobal.net. Accessed 27 Jan 2022.
- 17.Centers for Disease Control and Prevention. One Health: what we do. https://www.cdc.gov/onehealth/what-we-do/index.html. Accessed 27 Jan 2022.
- 18.Kahn LH. Perspective: the one-health way. Nature. 2017;543(7647):S47. doi: 10.1038/543S47a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Destoumieux-Garzon D, Mavingui P, Boetsch G, Boissier J, Darriet F, Duboz P, et al. The One Health concept: 10 years old and a long road ahead. Front Vet Sci. 2018;5:14. doi: 10.3389/fvets.2018.00014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mackenzie JS, McKinnon M, Jeggo M. One Health: from concept to practice. In: Yamada A, Kahn LH, Kaplan B, Monath TP, Woodall J, Conti L, editors. Confronting emerging zoonoses: the One Health paradigm. Tokyo: Springer; 2014. pp. 163–189. [Google Scholar]
- 21.Sinclair JR. Importance of a One Health approach in advancing global health security and the Sustainable Development Goals. Rev Sci Tech. 2019;38(1):145–154. doi: 10.20506/rst.38.1.2949. [DOI] [PubMed] [Google Scholar]
- 22.Munyua PM, Njenga MK, Osoro EM, Onyango CO, Bitek AO, Mwatondo A, et al. Successes and challenges of the One Health approach in Kenya over the last decade. BMC Public Health. 2019;19(3):465. doi: 10.1186/s12889-019-6772-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mackenzie JS, Jeggo M. The One Health approach—why is it so important? Trop Med Infect Dis. 2019;4(2):88. doi: 10.3390/tropicalmed4020088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Donabedian A. Evaluating the quality of medical care. Milbank Mem Fund Q. 1966;44(3):691–729. doi: 10.2307/3348969. [DOI] [PubMed] [Google Scholar]
- 25.Ye Q. Thoughts on climate change adaptation in cities under the context of the anthropocene. Sustain Dev. 2021;11(1):142–148. doi: 10.12677/SD.2021.111017. [DOI] [Google Scholar]
- 26.FAO, OIE, WHO, UNICEF, the World Bank, and the United Nations System Influenza Coordination (UNSIC). Contributing to One World, One Health: a strategic framework for reducing risks of infectious diseases at the animal-human-ecosystems interface. WHO. 2008. https://www.fao.org/3/aj137e/aj137e00.htm. Accessed 8 Mar 2022.
- 27.Amuasi JH, Lucas T, Horton R, Winkler AS. Reconnecting for our future: The Lancet One Health Commission. Lancet. 2020;395(10235):1469–1471. doi: 10.1016/S0140-6736(20)31027-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Garcia KK, Gostin LO. One Health, One World—the intersecting legal regimes of trade, climate change, food security, humanitarian crises, and migration. Laws. 2012;1(1):4–38. doi: 10.3390/laws1010004. [DOI] [Google Scholar]
- 29.Wang YM, Chin KS. Fuzzy analytic hierarchy process: a logarithmic fuzzy preference programming methodology. Int J Approx Reason. 2011;52(4):541–553. doi: 10.1016/j.ijar.2010.12.004. [DOI] [Google Scholar]
- 30.Sachs J, Kroll C, Lafortune G, Fuller G, Woelm F. Sustainable development report 2021. Cambridge: Cambridge University Press; 2020. [Google Scholar]
- 31.Wendling ZA, Emerson JW, de Sherbinin A, Esty DC, Hoving K, Ospina CD, et al. 2020 Environmental performance index. New Haven: Yale Center for Environmental Law & Policy, Yale University. 2020. https://epi.yale.edu/downloads/epi2020report20210112.pdf. Accessed 20 Feb 2022.
- 32.Dunham B. One Health pandemic prevention and mitigation: the role of FDA. CAPT Brianna Skinner. 2020. https://www.fdli.org/wp-content/uploads/2020/11/11.13-145-230-Skinner.pdf. Accessed 20 Feb 2022.
- 33.Federal Ministry of Economic Cooperation and Development. Initiative area One Health in development cooperation. 2021. https://health.bmz.de/wp-content/uploads/Strategiepapier550_one_health_en.pdf. Accessed 20 Feb 2022.
- 34.He L. 2020 Global “One Health” Hainan demonstration project expert roundtable (Shanghai) meeting held in Shanghai. Shanghai Jiao Tong University School of Medicine. 2020. https://www.shsmu.edu.cn/sgh/info/1225/1746.htm. Accessed 20 Feb 2022 (in Chinese).
- 35.World Health Organization. Global database for the tripartite antimicrobial resistance (AMR) country self-assessment survey (TRACSS). 2021. https://amrcountryprogress.org/#/response-overview. Accessed 20 Feb 2022.
- 36.Johns Hopkins Center for Health Security. Global Health Security Index. 2021. https://www.ghsindex.org/. Accessed 20 Feb 2022.
- 37.Rüegg SR, Nielsen LR, Buttigieg SC, Santa M, Aragrande M, Canali M, et al. A systems approach to evaluate One Health initiatives. Front Vet Sci. 2018;5:23. doi: 10.3389/fvets.2018.00023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wang X, Rainey JJ, Goryoka GW, Liang Z, Wu S, Wen L, et al. Using a One Health approach to prioritize zoonotic diseases in China, 2019. PLoS One. 2021;16(11):e0259706. doi: 10.1371/journal.pone.0259706. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1. Weights calculation of global One Health index (GOHI).
Additional file 2. The indicators and weights for establishment of global One Health index (GOHI).
Data Availability Statement
The full study protocol and the datasets are available, following manuscript publication, upon request from the corresponding author (Xiao-Nong Zhou, zhouxn1@chinacdc.cn).