Abstract
Background
Cerebral oximetry using near-infrared spectroscopy (NIRS) has been shown to reduce neurological dysfunction and hospital length-of-stay after adult cardiac surgery in some but not all studies. We audited maintaining cerebral saturations at or above baseline and showed improved neurological and length-of-stay outcomes. Our hypothesis for this study was that our NIRS protocol would improve neurological and length-of-stay outcomes.
Methods
This prospective, single centre, double-blinded controlled study randomized 182 consecutive patients, scheduled for cardiac surgery using cardiopulmonary bypass. Participants were randomized by concealed envelope prior to anaesthesia. NIRS study group were managed perioperatively using our NIRS protocol of 8 interventions, increase cardiac output, normocapnia, increase mean arterial pressure, increase inspired oxygen, depth of anaesthesia, blood transfusion, correction of bypass cannula, change of surgical plan to restore levels equal to or above baseline. The control group had standard management without NIRS. Primary outcomes were neurological impairment (early and late) and hospital length-of-stay. Secondary outcomes were ventilation times, intensive care length-of-stay, major organ dysfunction and mortality.
Results
91 patients entered each group. There was a significant improvement in self-reported six-month general functionality in the NIRS group (p = 0.016). Early neurological dysfunction and hospital length-of-stay was the same in both groups. Of the secondary outcomes only Intensive Care length-of-stay was statistically significant, being shorter in the NIRS group (p = 0.026).
Conclusion
Maintaining cerebral saturations above baseline reduces time spent in Intensive Care and may improve long term functional recovery but not stroke, major organ dysfunction and mortality.
Keywords: Near infrared spectroscopy, cerebral oxygenation, cognitive dysfunction, adult cardiac surgery, cardiopulmonary bypass
Introduction
Regional Cerebral saturations (rSO2) can be measured using near-infrared spectroscopy (NIRS). A probe on the forehead sends a signal which reaches the cerebral cortex and is reflected off the haemoglobin. Oxy-haemoglobin and deoxy-haemoglobin absorb near infrared light differently and the resultant signal can be detected and processed to give a measure of the percentage oxygen saturation and thus detect cerebral ischaemia.1,2 Although cardiac surgery has become safer there remains an overall 1-3% incidence of stroke and 22% incidence of neurocognitive impairment. 3 It was hoped that NIRS and goal directed interventions, would reduce neurological and organ dysfunction. 4 However, the uptake of NIRS monitoring is inconsistent. 5 A review in 2005 did not confirm the clinical utility of NIRS. 6 Later a Cochrane review remained inconclusive. 7 A review in 2019 concluded post-operative cognitive decline and delirium is reduced by using NIRS in cardiac surgery with a tendency to less organ dysfunction. 8 Hospital and Intensive Care (ICU) length-of-stay (LOS) have been used as surrogates for event free recovery after cardiac surgery. Most studies have focussed on coronary surgery, although valvular and aortic surgery pose a greater risk. This study included coronary, valvular or aortic cardiac surgery. The primary aim was to assess neurological function post-surgery (early and late) and hospital LOS. Secondary aims were; ventilation times, ICU LOS, major organ dysfunction and mortality. The hypothesis: patients actively managed with NIRS, during surgery would have better rSO2 thus improved outcomes compared with patients managed without NIRS.
Method
This was a prospective, double-blind RCT. All data was collected from Castle Hill Hospital, East Yorkshire, UK, a tertiary referral cardiac centre serving a population of approximately 1.2 million.
Patients were enrolled the day before cardiac surgery with cardiopulmonary bypass (CPB). Patient characteristics, type of operation and pre-morbid condition are shown in Table 1.
Table 1.
Patient demographics.
| Variables |
Total patients no. (N = 182) |
P-value 0.05ǂ significant | |
|---|---|---|---|
| NIRS group n = 91 | Control group n = 91 | ||
| Gender (%) | 0.172 | ||
| Male | 72 (52.9) | 64 (47.1) | |
| Female | 19 (41.3) | 27 (58.7) | |
| Age in years (%) | 0.052 | ||
| ≤60 | 16 (42.1) | 22 (57.9) | |
| 61–75 | 60 (57.7) | 44 (42.3) | |
| +76 | 15 (37.5) | 25 (62.5) | |
| Weight in kg (%) | 0.228 | ||
| ≤80 | 46 (47.4) | 51 (52.6) | |
| 81–100 | 36 (58.1) | 26 (41.9) | |
| ≥101 | 9 (39.1) | 14 (60.9) | |
| Operation type (%) | 0.024ǂ | ||
| CABG only | 50 (48.5) | 53 (51.5) | |
| CABG + valve | 16 (69.6) | 7 (30.4) | |
| Valve only | 14 (35) | 26 (65) | |
| Othersa | 11 (68.8) | 5 (31.3) | |
| Logistic Euro-score (%) | 0.251 | ||
| ≤4 | 55 (50.9) | 53 (49.1) | |
| 5–10 | 22 (57.9) | 16 (42.1) | |
| ≥11 | 14 (38.9) | 22 (61.1) | |
| Diabetes (%) | 14 (33.3) | 28 (66.7) | 0.014ǂ |
| Hypertension (%) | 66 (49.6) | 67 (50.4) | 0.867 |
| Neurological history (%) | 11 (50) | 11 (50) | 1.0 |
| Arrhythmias | 17 (50) | 17 (50) | 1.0 |
| Ejection fraction (%) | 0.445 | ||
| ≥50% | 63 (48.5) | 66 (51.2) | |
| 30–49 | 22 (57.9) | 16 (42.1) | |
| ≤30 | 6 (40) | 9 (60) | |
| Creatinine, mmol (%) | 0.265 | ||
| ≤120 | 77 (48.4) | 82 (51.6) | |
| ≥121 | 14 (60.9) | 9 (39.1) | |
aIn the NIRS group: 1 Ventricular septal defect (VSD), 5 aortic valve replacement (AVR) and ascending aortic repair, 2 Atrial Septal Defects (ASD), 1 ventricular aneurysm, 2 tumours. In the control group: 3 AVR and ascending repair, 1 ASD, heart and lung operation.
Patients were recruited and followed-up between 2011–14. All received written and verbal details of the study before enrolment. Written consent was obtained prior to neurocognitive testing the day before surgery. Patients were examined for neurological dysfunction and had routine tests for major organ function.
Inclusion criteria were: elective and stable-urgent, in-patients that were capable and willing to complete the pre-operative neurocognitive tests. Exclusion criteria were: inability to undergo testing or any unstable neurological condition. Consecutive patients were considered pending the availability of a study anaesthetist and research nurse.
All tests were carried out by trained nurses in a quiet room without distraction pre- and post-operatively. The nurses and doctors doing the assessments and recording the ICU outcomes were blinded to the study grouping. The anaesthetist and intraoperative team were aware of the patient group in order to carry out the interventions.
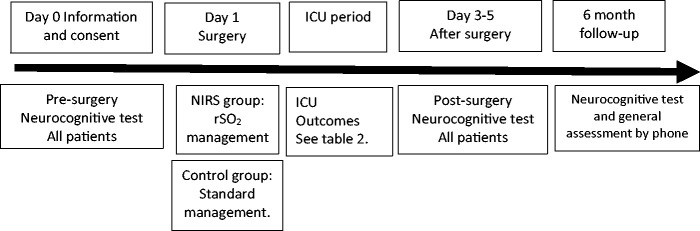
Randomization was by sealed envelope opened immediately before the start of anaesthesia (Figure 1).
Figure 1.
NIRS Study time line.
Regular medications were continued until the day of surgery except for anti-platelets and angiotensin converting enzyme inhibitors which were stopped according to hospital policy. Pre-medication with temazepam 10 mg was given if requested. Lines were inserted awake along with the probes for rSO2 on the left and right side of the patient’s forehead. Patients allocated to cerebral oximetry, NIRS group n = 91, using NIRS to monitor rSO2 were connected to the oximetry monitor (INVOS, 5100, Somanetics Corporation, Troy, MI). Patients allocated to the control group (n = 91) were not connected. Subsequent anaesthetic/surgical management was standard (based on remifentanil, fentanyl, pancuronium, sevoflurane, with isoflurane during CPB), for all patients. The NIRS group were subject to interventions to maintain rSO2 values at or above baseline. The majority of cases were done by the same anaesthetic/surgical team who could see the rSO2 values and act accordingly. Interventions were according to our NIRS protocol Table 2.
Table 2.
Interventions to maintain rSO2 above baseline.
| 1. Pump flow to be re-calculated to ensure flow is 2.4 l/m2/min/ or greater. |
| 2. PaCO2 increased to 5.3 kPa. |
| 3. Mean pressure increased to 60 mmHg using metaraminol in the first instance. |
| 4. FiO2 increased to 1.0 |
| 5. Depth of anaesthesia: all patients will be anaesthetised with a minimum of 1% isoflurane during CPB, this will be increased to 2 and 3%. |
| 6. Transfusion if haematocrit <25%. |
| 7. Correction of aortic and venous cannula position. |
| 8. Change of surgical plan |
| Any readings below baseline of >40 secs and not responding to 1–6 above would be discussed with surgeon and prompt action taken. |
The aim was to keep rSO2 values above baseline until the end of surgery. Baseline being the awake reading breathing air. Any fall from baseline prior to the onset of CPB prompted an assessment of cardiac output, oxygenation and cerebral perfusion pressure with appropriate interventions. The onset of CPB pre-empted patients in whom a fall in rSO2 was anticipated (anaemia or a low blood volume).rSO2 was recorded at six stages as below:
Pre-anaesthesia on air.
Post-intubation.
On administration of heparin.
Lowest during 1st 3 minutes on CPB.
Lowest on CPB.
Sternal closure.
The rSO2 probes were removed before transfer to the ICU. Subsequent management was the same for both groups.
Ethics committee (Newcastle, UK) approval,REC number 10/H0906/72.
UK ClinicalTrials.gov PRS number NCT04463563.
Primary and secondary outcomes
The primary outcomes for the study were neurological impairment, neurocognitive dysfunction (early and late) and hospital LOS measured by 7 days or less, 8–12 days or 13 days or more.
Neurological impairment was considered as: post-operative stroke; transient ischaemic attack (TIA) determined clinically by doctors and acute confusional state (ACS) recorded by the ICU or ward nurse.
Neurocognitive dysfunction was assessed by comparing a battery of 8 tests with a baseline recorded 24 hours pre-operatively and a second test performed after discharge from ICU on the 3-5th post-operative day.
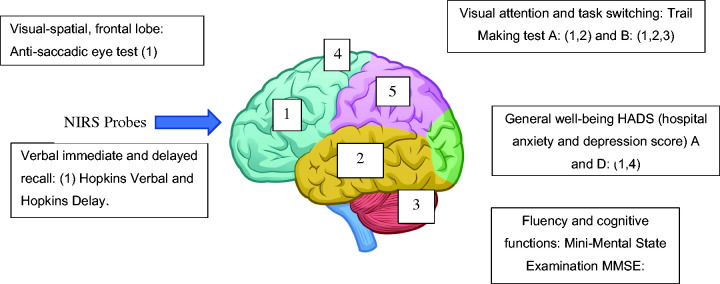
The neurocognitive tests were (Figure 2):
Fluency and cognitive functions: Mini-Mental State Examination (MMSE)
Visual attention and task switching: Trail Making test A and B.
Visual-spatial, frontal lobe: Anti-saccadic eye test.
Executive function/verbal immediate and delayed recall: Hopkins Verbal and Hopkins Delay.
General well-being HADS (hospital anxiety and depression score) A and D.
Figure 2.
Anatomical areas of the brain (numbers) implicated in the Neurocognitive evaluation.
The six-month neurological assessment was a general health, cognition and functionality interview by telephone. (See Supplementary File: 6 month telephone follow-up questionnaire).
Secondary outcomes: Time to extubation, ICU LOS, major organ dysfunction and mortality.
Statistics
The sample size was based on a previous study and finding a 40% incidence of early neurocognitive dysfunction in adult cardiac surgery using CPB. 9 To detect a reduction of 50%, that is to 20% dysfunction, the numbers would be 91 per group, based on 80% power and 5% significance.
Descriptive statistics are presented for each group, mean (standard deviation, SD) and n (%). To compare outcome measures we used, t-test for continuous data, Mann Whitney tests for ordinal or non-normal data and chi-square tests for categorical data. A p-value of <0.05 was considered to indicate statistical significance. Analysis was undertaken on SPSS 23.
Results
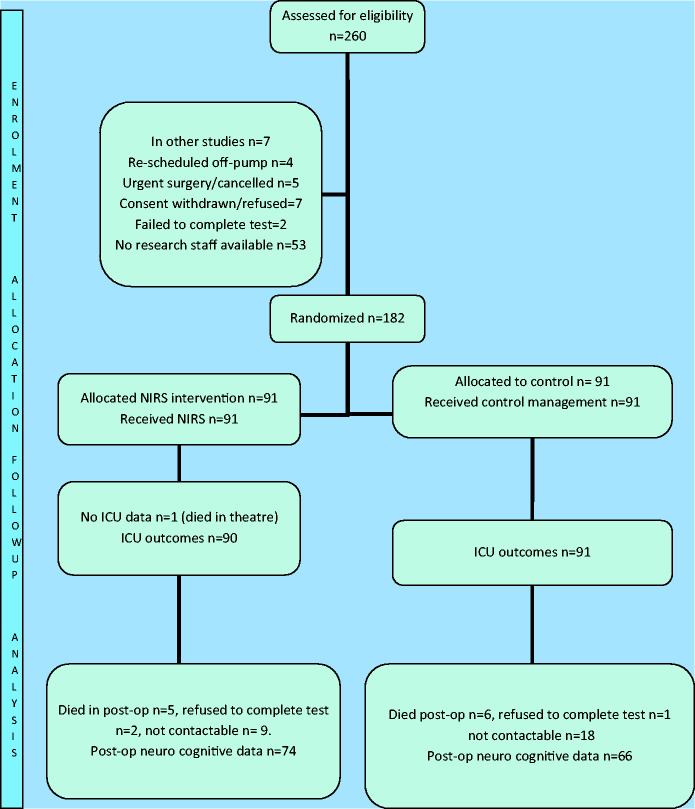
Of the 260 assessed 182 were consented and randomized. There was 1 intraoperative death in the NIRS group from bleeding. In the early post-operative period, there were a further 4 deaths in each group. Thus, the early outcome data was available for 181 to 173 patients but was less complete for later outcomes (Figure 3).
Figure 3.
Patient flow chart.
Table 1 shows more patients in the NIRS group had combined coronary and valve surgery. More controls had valve only surgery. The NIRS group had 11 ‘other’ surgeries of which 2 died. The control group 5 of which 1 died. The precise operations are described with Table 1. These were mostly high-risk operations. Pre-morbid conditions were similar except diabetes, which was more common in the control group.
Primary and secondary outcomes
Table 3 shows no statistically significant difference between the two groups for the in-hospital neurological outcomes and hospital LOS. At the six-month follow-up the functionality questionnaire was improved in the NIRS group (p = 0.016). In the secondary outcomes, ICU LOS showed a statistically significant shorter LOS for the NIRS group (p = 0.026). There was no statistical difference in the other outcomes. Numbers were reduced at follow-up due to refusal, not contactable or death.
Table 3.
Primary and secondary outcomes including 6 month post-operative telephone questionnaire.
| Primary outcomes | NIRS Group n = 90 (%) | Control Group n = 91 (%) | p-value 0.05ǂsign |
|---|---|---|---|
| Neurological dysfunction (%) | n = 90 | n = 91 | 0.600 |
| None | 83 (91) | 82 (90) | |
| Permanent stroke | 2 (2) | 1 (33) | |
| Transient stroke | 1 (1) | 2 (67) | |
| Acute confusional state | 4 (4) | 6 (7) | |
| Neurocognitive post-op tests success/fail | n = 68 | n = 59 | 0.498 |
| Passed all tests | 40 (59) | 38 (64) | |
| Failed 1 test | 26 (38) | 20 (34) | |
| Failed >1 test | 2 (3) | 1 (2) | |
| Cognition 6 months post-operative Adapted MMSE for telephone consultation (maximum score 15) | n = 74 | n = 66 | 0.841 |
| Refused cognitive assessment | 6 (8) | 3 (5) | |
| Completed assessment | 68 (92) | 63 (95) | |
| Mean score (standard deviation) | 13 (1.8) | 12 (1.9) | |
| Functionality 6 months post-operative | n = 74 | n = 66 | 0.016ǂ |
| Better | 15 (20) | 9 (14) | |
| No difference | 51 (69) | 38 (57) | |
| Worse | 8 (11) | 19 (29) | |
| post-operative hospital length-of-stay | n = 90 | n = 90 | 0.544 |
| 7 days or less | 50 (55) | 44 (53) | |
| 8-12 days | 21 (23) | 28 (31) | |
| 13 or more days | 19 (21) | 18 (20) | |
| Secondary outcomes | |||
| Time to extubation, hours | n = 90 | n = 89 | 0.942 |
| 4 or less | 57 (63) | 56 (62) | |
| 5–12 | 23 (25) | 24 (27) | |
| 13–24 | 7 (8) | 2 (2) | |
| >24 | 3 (3) | 7 (8) | |
| First ICU stay, hours | n = 90 | n = 89 | 0.026ǂ |
| <24 | 41 (45) | 25 (28) | |
| 25–48 | 26 (29) | 35 (39) | |
| >48 | 23 (25) | 31 (34) | |
| Renal dysfunction | n = 90 10 (11) |
n = 91 8 (8) |
0.619 |
| Gastrointestinal ischaemia | n = 90 2 (2) |
n = 91 1 (1) |
0.560 |
| Multi-organ failure | n = 90 3 (3) |
n = 91 3 (3) |
1.0 |
| General well being: | n = 74 | n = 66 | 0.207 |
| Better | 42 (56) | 30 (45) | |
| Same | 16 (22) | 18 (27) | |
| Worse | 16 (22) | 18 (27) | |
| How did the study impact your admission? | n = 74 | n = 66 | 0.751 |
| Better | 25 (34) | 20 (30) | |
| No difference | 48 (65) | 46 (70) | |
| Worse | 1 (1) | 0 (0) | |
| Status at discharge | n = 91 | n = 91 | 0.732 |
| Alive | 86 (94) | 87 (96) | |
| Dead | 5 (5) | 4 (4) |
Table 4 (supplementary) shows The results for the individual 8 neurocognitive test performed preoperatively and 3–5 days post-operatively are shown in the Supplementary File: ‘Neurocognitive dysfunction Tests’. There was no statistically significant difference between the groups for any of the tests. A total of 26 patients in the NIRS group and 20 patients in the control group failed one of the six neurocognitive tests. 2 NIRS and 1 control failed more than 1 test. A summary is in Table 3.
Data for CPB, haemoglobin and temperature are shown in Supplementary File: Cardiopulmonary Bypass data.
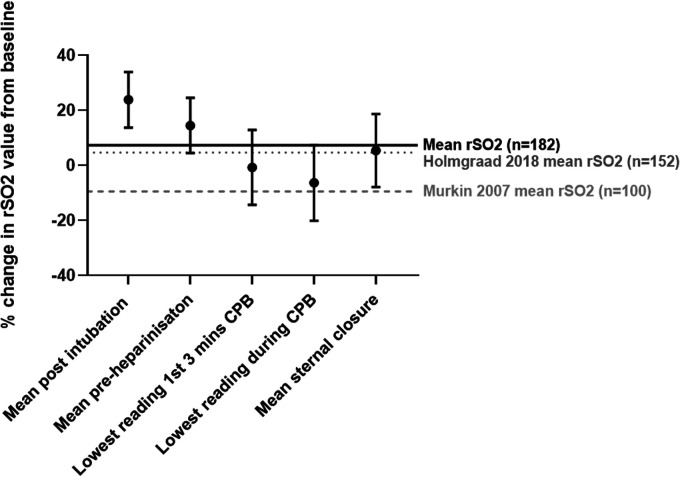
NIRS data
Cerebral oximetry readings were displayed throughout surgery and recorded in hard copy at 6 time-intervals shown in Figure 4. For each patient the awake value represents zero and the next 5 measurement points were recorded as a percentage change above or below zero. The solid line shows the average percentage change for our study group was +7.3% above baseline.
Figure 4.
Percentage change from baseline in our NIRS study patients. y-axis=percentage change from baseline. Bars show SD. Average NIRS values are compared with two other studies. Solid line is the average NIRS value in our study. Dashed line (—-) is average NIRS for Murkin, dotted line (……) average NIRS for Holmgaard study.
Discussion
Neurological damage is multi-factorial. One early RCT showed improvement with NIRS-guided intervention of reduced ICU and hospital LOS and a composite reduction in major organ dysfunction. 4 Since then a review by Zorrilla has shown improved neurocognitive and ICU LOS outcomes using NIRS. 10
Most studies accept a level of cerebral tolerance to hypoxia (allowable percentage fall from baseline). Typically quoted as a 25% relative fall or below 50% as an absolute value. In our previous audit we were able to keep rSO2 at or close to baseline. In that audit, 6/100 patients had episodes of desaturation to 25% below baseline, no critical falls (40% below baseline).
Our study interventions were initiated if rSO2 values fell below the baseline rSO2 breathing air and not waiting for a 25% fall before intervening. Interventions take time to implement and ischaemia is time dependent. Even low baseline patients were kept above baseline. This is seen in Figure 4 showing our NIRS patients stay 7.3% above baseline on average. In the Holmgaard’s study the mean was +4.6% above baseline and in Murkin’s study the mean was negative, –9.5%.4,11 Pre-emptive and early intervention avoided more significant falls in rSO2 at the start of CPB.
Pathological evidence by diffusion weighted MRI scanning has shown that ischaemic changes were detectable with falls in rSO2 of 10% below baseline. 10
There are 3 domains of neurological damage; direct cell death causing stroke, neurocognitive dysfunction and delirium. Watershed strokes are time sensitive and may be prevented if the NIRS signal is over the correct cerebral area at the time. 12 One non-RCT with 1034 patients using NIRS during cardiac surgery showed a significant reduction in stroke. 13
In our NIRS group, 2 patients had strokes. One had NIRS values above baseline throughout surgery but arrested post-operatively because of bleeding and died 5 weeks post-operatively. The 2nd showed NIRS values never more than 4% below baseline but suffered a cerebellar infarction. One patient had a TIA, his baseline rSO2 was 50% and his NIRS values were 22% above baseline during CPB.
The control group had 2 strokes. One stroke was ischaemic occurring peri-operatively, the other occurred after a post-operative cardiac arrest. There were 2 TIAs.
Reducing neurocognitive dysfunction using cerebral oximetry remains elusive. It can occur despite good cerebral oxygenation. Higher baseline NIRS may reduce neurocognitive dysfunction, 8 although it is probably not a modifiable risk. 14 Holmgaard’s most recent study concluded that post-operative cognitive dysfunction was not associated with changes in intra-operative rSO2. Although high doses of norepinephrine (0.4 u/kg/min) were used to maintain blood pressure which can negatively impact neurocognitive outcomes. 15
Within the battery of 6 motor/higher function tests we found 19 (28%) NIRS and 18 (30%) control patients failed one test. Failure of >1 test was seen in 2 (3%) NIRS patients and 1 (2%) control patient. Other studies have taken the cut-off for significance as failure of up to four tests out of six. 15 Our low rate of neurocognitive dysfunction may be explained by the short CPB times and our familiar practice with NIRS. We did find a significant improvement of functional ability at six months with 89% of NIRS recording, the same or better than pre-operatively versus 71% in the control group. An important patient outcome albeit subjective. The patients did not have this questionnaire pre-operatively and it is possible their memory of ‘what they could do’ pre-operatively was inaccurate or was restricted by other factors. All the ‘functionality’ questions are included in the Supplementary File- 6 month telephone questionnaire and all relate to the tasks of daily living which are relatively well remembered.
Neurocognitive function is on a declining trajectory in the elderly. Cardiac surgery steepens the trajectory followed by a halt or improvement in the longer term (12 months). 16 Avoidance of cerebral hypoxia at the time of surgery may avoid the early deterioration.
Delirium or acute confusional syndrome (ACS) is also multifactorial in origin. Low rSO2 pre-operatively is associated with post-operative delirium but it is not modified by increasing rSO2 during surgery.17,18 Pre-operative neurological disorders and loss of cerebral autoregulation may increase post-operative delirium. 19
Our NIRS group had 4 patients with ACS. One had rSO2 14% below baseline on CPB, the 2nd patient was 6% below baseline on CPB. The 3rd and 4th patients stayed above baseline throughout. None fell below 50% as an absolute value in cerebral saturations.
6 patients in the control group had suffered ACS.
Our secondary outcomes focused on the concept of the brain as an index organ. 20 Although we did not show any difference in specific organ dysfunction, we showed shorter ICU LOS for NIRS patients (p = 0.026). The major predictor of post-operative organ dysfunction is pre-operative organ dysfunction. Overall mortality was comparable between the groups. There were more high risk ‘other’ surgeries in the NIRS group. Amongst these high-risk patients, mortality was close to 20% in both groups.
Study limitations; we have been using NIRS for many years and our normal practice is to mitigate low rSO2; stroke is uncommon 1-3% and half cannot be prevented using NIRS; the root cause of many adverse outcomes are acute surgical events, especially haemorrhage. There was wide inter-group variation in blood loss. Patients who bled significantly had worse outcomes; many adverse events occurred post-operatively; the inability to follow-up all the patients.
Our results are consistent with other studies of this size. Even though no statistical improvement was seen in the hospital neurological outcomes or hospital LOS, there was a significant improvement in ICU LOS which has important implications for ICU dependency.
In conclusion using NIRS to maintain cerebral saturations above baseline throughout cardiac surgery reduces ICU LOS and improves long-term functional recovery while early neurological and organ dysfunction were not improved.
Supplemental Material
Supplemental material, sj-pdf-1-inc-10.1177_1751143720977280 for Cerebral oximetry in adult cardiac surgery to reduce the incidence of neurological impairment and hospital length-of-stay: A prospective, randomized, controlled trial by Sean R Bennett, Neil Smith and Miriam R Bennett in Journal of the Intensive Care Society
Supplemental material, sj-pdf-2-inc-10.1177_1751143720977280 for Cerebral oximetry in adult cardiac surgery to reduce the incidence of neurological impairment and hospital length-of-stay: A prospective, randomized, controlled trial by Sean R Bennett, Neil Smith and Miriam R Bennett in Journal of the Intensive Care Society
Supplemental material, sj-pdf-3-inc-10.1177_1751143720977280 for Cerebral oximetry in adult cardiac surgery to reduce the incidence of neurological impairment and hospital length-of-stay: A prospective, randomized, controlled trial by Sean R Bennett, Neil Smith and Miriam R Bennett in Journal of the Intensive Care Society
Acknowledgements
Victoria Algar: Statistics preparing the study.
Dr Basim Alsaywid for statistical review.
Dr F Emperador: reviewed the manuscript.
V Martinson, L Sleight, A Walker, R Bennett: data collection and testing.
Footnotes
Authors’ contribution: SRB: principal investigator, study conception, conduct of study, article writing.
NS: Study design and set-up, data collection.
MRB: data collection, statistics and review of manuscript.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: SRB received honoraria for lecturing on NIRS.
Declaration of conflicting interests: The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: Previously I received honoraria for attending educational meetings and lecturing on the topic of cerebral protection. As Principle Investigator and corresponding author I declare that neither myself or the other authors have any conflict of interest or have received financial reward for the publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Hull and East Yorkshire Cardiac Trust Fund.
ORCID iD: Sean R Bennett https://orcid.org/0000-0003-0571-0338
Supplemental material: Supplemental material for this article is available online.
References
- 1.Murkin JM andArango M.. Near-infrared spectroscopy as an index of brain and tissue oxygenation. Br J Anaesth 2009; 103: 3–13. [DOI] [PubMed] [Google Scholar]
- 2.Green MS Sehgal S andTariq R.. Near-infrared spectroscopy: the new must have tool in the intensive care unit? SEM Cardiothoracic Vasc Semin Cardiothorac Vasc Anesth 2016; 20: 213–224. [DOI] [PubMed] [Google Scholar]
- 3.van Dijk D, Keizer AM, Diephuis JC, et al. Neurocognitive dysfunction after coronary artery bypass surgery: a systematic review. J Thorac Cardiovasc Surg 2000; 120: 632–639. [DOI] [PubMed] [Google Scholar]
- 4.Murkin JM, Adams SJ, Novick RJ, et al. Monitoring brain oxygen saturation during coronary bypass surgery: a randomized, prospective study. Anesth Analg 2007; 104: 51–58. [DOI] [PubMed] [Google Scholar]
- 5.Yoshitani K, Kawaguchi M, Ishida K, et al. Guidelines for the use of cerebral oximetry by near-infrared spectroscopy in cardiovascular anesthesia: academic committee of the Japanese society of cardiovascular anesthesiologists. J Anesth 2019; 33: 167–196. [DOI] [PubMed] [Google Scholar]
- 6.Taillefer MC andDenault AY.. Cerebral near-infrared spectroscopy in adult heart surgery: systematic review of its clinical efficacy. Can J Anaesth 2005; 52: 79–87. [DOI] [PubMed] [Google Scholar]
- 7.Yu Y, Zhang K, Zhang L, et al. Cerebral near-infrared spectroscopy (NIRS) for perioperative monitoring of brain oxygenation in children and adults. Cochrane Database Syst Rev 2018; 2: Art. No. CD010947. [DOI] [PMC free article] [PubMed]
- 8.Ortega-Loubon C, Gomez FH, Guevara CB, et al. Near-infrared spectroscopy monitoring in cardiac and noncardiac surgery: pairwise and network meta-analyses. JCM 2019; 8: 2208–2222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Slater JP, Guarino T, Stack J, et al. Cerebral oxygen desaturation predicts cognitive decline and longer hospital stay after cardiac surgery. Ann Thorac Surg 2009; 87: 36–45. [DOI] [PubMed] [Google Scholar]
- 10.Zorrilla-Vaca A, Healy R, Grant MC, et al. Intraoperative cerebral oximetry-based management for optimizing perioperative outcomes: a meta-analysis of randomized controlled trials. Can J Anaesth 2018; 65: 529–542. [DOI] [PubMed] [Google Scholar]
- 11.Holmgaard F, Vedel AG, Langkilde A, et al. Differences in regional cerebral oximetry during cardiac surgery for patients with or without postoperative cerebral ischaemic lesions evaluated by magnetic resonance imaging. Br J Anaesth 2018; 121: 1203–1211. [DOI] [PubMed] [Google Scholar]
- 12.Gottesman RF, Sherman PM, Grega MA, et al. Watershed strokes after cardiac surgery: diagnosis, etiology and outcome. Stroke 2006; 37: 2306–2311. [DOI] [PubMed] [Google Scholar]
- 13.Heringlake M, Garbers C, Kabler JH, et al. Preoperative cerebral oxygen saturation and clinical outcomes in cardiac surgery. Anesthesiol 2011; 114: 58–69. [DOI] [PubMed] [Google Scholar]
- 14.Rogers CA, Stoica S, Ellis L, et al. Randomized trial of near-infrared spectroscopy for personalized optimization of cerebral tissue oxygenation during cardiac surgery. Br J Anaesth 2017; 119: 384–393. [DOI] [PubMed] [Google Scholar]
- 15.Holmgaard F, Vedel AG, Rasmussen LS, et al. The association between postoperative cognitive dysfunction and cerebral oximetry during cardiac surgery: a secondary analysis of a randomized trial. Br J Anaesth 2019; 123: 196–205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cormack F, Shipolini A, Awad WI, et al. A meta-analysis of cognitive outcome following coronary artery bypass surgery. Neurosci Behav Rev 2012; 36: 2118–2129. [DOI] [PubMed] [Google Scholar]
- 17.Tournay-Jette E, Dupuis G, Bherer L, et al. Postoperative cognitive dysfunction in elderly patients after coronary artery bypass graft surgery. JCTVA 2011; 25: 95–104. [DOI] [PubMed] [Google Scholar]
- 18.Eertmans W, Deyne C, Genbrugge C, et al. Association between postoperative delirium and postoperative cerebral oxygen desaturation in older patients after cardiac surgery. Br J Anaesth 2020; 124: 146–153. [DOI] [PubMed] [Google Scholar]
- 19.Chan B andAneman A.. A prospective, observational study of cerebrovascular autoregulation and its association with delirium following cardiac surgery. Anaesthesia 2019; 74: 33–44. [DOI] [PubMed] [Google Scholar]
- 20.Murkin JM. Cerebral oximetry: monitoring the brain as the index organ. Anesthesiology 2011; 114: 12–13. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-pdf-1-inc-10.1177_1751143720977280 for Cerebral oximetry in adult cardiac surgery to reduce the incidence of neurological impairment and hospital length-of-stay: A prospective, randomized, controlled trial by Sean R Bennett, Neil Smith and Miriam R Bennett in Journal of the Intensive Care Society
Supplemental material, sj-pdf-2-inc-10.1177_1751143720977280 for Cerebral oximetry in adult cardiac surgery to reduce the incidence of neurological impairment and hospital length-of-stay: A prospective, randomized, controlled trial by Sean R Bennett, Neil Smith and Miriam R Bennett in Journal of the Intensive Care Society
Supplemental material, sj-pdf-3-inc-10.1177_1751143720977280 for Cerebral oximetry in adult cardiac surgery to reduce the incidence of neurological impairment and hospital length-of-stay: A prospective, randomized, controlled trial by Sean R Bennett, Neil Smith and Miriam R Bennett in Journal of the Intensive Care Society