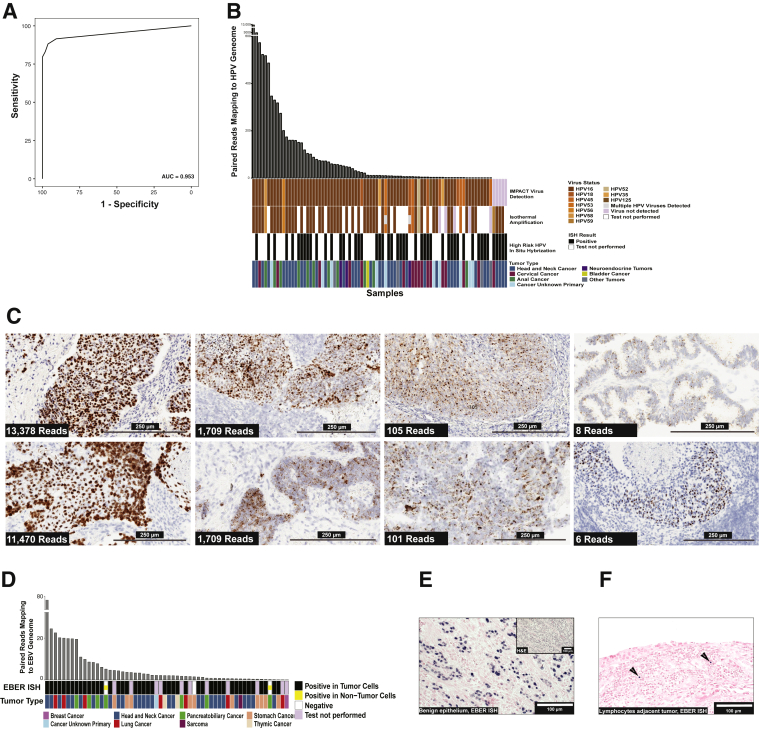
Figure 2.
Validation of virus detection using nonmapping reads. A: Receiver operating characteristic analysis for high-risk (HR) human papilloma virus (HPV) detection with isothermal amplification detection method as the standard. Area under the curve was 0.953, and the optimal threshold for identifying HR HPV was two or more reads. B: Comparison of Memorial Sloan Kettering–Integrated Mutation Profiling of Actionable Cancer Targets (MSK-IMPACT) analysis, isothermal amplification, and in situ hybridization (ISH) results for detection of HR HPV. The figure displays cases where virus was detected by any of the three methods. Each vertical bar represents a single case. The bar plot at top shows the number of paired reads of the virus detected by MSK-IMPACT. The HPV genotype is shown by colors to compare the genotype detection between IMPACT and isothermal amplification. The bottom row shows the tumor type for each case as indicated in the legend. C: Demonstration of increased HR HPV RNA expression (brown signal) in tumor cells with a large dynamic range of HR HPV reads detected by MSK-IMPACT. The number of reads correlates with a combination of the intensity of RNA expression by ISH in tumor cells, the proportion of tumor cells where virus RNA expression was detected, and the proportion of neoplastic cells on the slide. Low tumor proportion is frequently a factor in cases with lower virus reads. D: Comparison of Epstein-Barr Early Region (EBER) ISH and IMPACT for cases with >70 EBV reads detected by next-generation sequencing (NGS) read analysis and the respective tumor types. E: EBER ISH of a case with >70 EBV reads where virus was localized to benign epithelium (blue signal indicates positive cells). F: EBER ISH of tumor tissue with <70 EBER reads by NGS read analysis where virus localized to tumor-associated lymphocytes (arrows point to positive cells). Scale bars: 250 μm (C); 100 μm (E and F). AUROC, area under the receiver operating characteristic curve; H&E, hematoxylin and eosin.