Cardiovascular disease (CVD) is the primary cause of morbidity and mortality in chronic kidney disease (CKD). CVD mortality risk doubles and triples in CKD stages 3 and 4, respectively.[1] This relationship is complex and bidirectional, with each condition increasing the incidence and progression of the other.[2,3] Indeed, the heart and kidney are inextricably linked, as exemplified by the cardiorenal syndrome whereby dysfunction of one organ induces and advances dysfunction in the other.[4,5]
CVD assessment and management are complicated by the presence of CKD and its comorbidities. Additional CKD-related risk factors and alternative pathophysiology also contribute to CKD-CVD.[1] CKD patients are largely excluded from clinical studies, resulting in a poor generalisability of assessment tools and a poor evidence base for the safety and efficacy of available treatments. Systematic reviews in 2006 found that CKD patients were excluded from 56–75% of CVD trials. This was even higher for patients with end-stage kidney disease (ESKD).[6,7] Updated reviews in 2018 demonstrated continued underrepresentation with 46–57% of CVD studies excluding CKD patients.[8,9] Recent recommendations to promote inclusion of CKD patients have considered the role for regulatory and financial incentives, modifications to study design and collaboration between cardiologists and nephrologists. These strategies are needed if we are to obtain the essential data to guide management of this vulnerable population.[10] Indeed, current treatment options are associated with a high burden of adverse events, complications and concerns about dose adjustments particularly for renally-excreted medications.[1] Clinicians act with caution, resulting in CVD being under-treated in many cases.[11] This article aims to address the current understanding of CKD-CVD and the limitations. It will focus on coronary artery disease (CAD), arrhythmias, heart failure (HF) and valvular heart disease (VHD).
Risk Factors and Presentation
Traditional cardiovascular risk factors, such as hypertension and diabetes, are very common in CKD. Further CKD-related CVD risk factors also contribute, such as uraemia, anaemia, inflammation, oxidative stress and factors related to dialysis.[1,12] These CKD-related factors contribute more with a decline in estimated glomerular filtration rate (eGFR). This is reflected in the pathophysiology of CVD in CKD patients as non-atherosclerotic cardiac events becoming increasingly common as CKD progresses (Figure 1).[1,13–15]
Figure 1: Changing Cardiovascular Disease Risk in Progressing Chronic Kidney Disease.
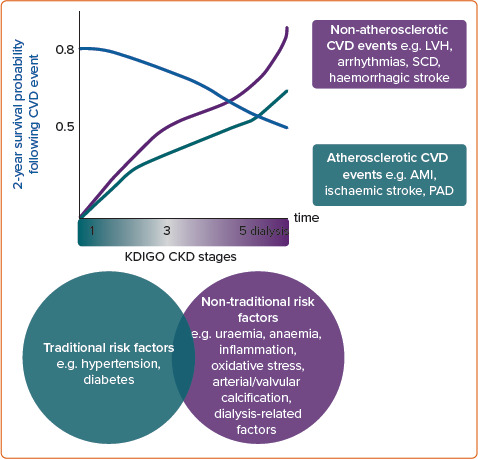
As CKD progresses, the risk of CVD events rises. Mortality following cardiovascular events also increases. Non-atherosclerotic causes contribute more than atherosclerotic causes as CKD progresses. This is reflected in the respective contribution of traditional and non-traditional risk factors in early and late-stage disease. Time is also an important factor – the longer time spent in each stage of CKD before commencing dialysis will result in longer exposure to the risk factors and greater accumulated damage and risk.[1,13–15] AMI = acute MI; CKD = chronic kidney disease; CVD = cardiovascular disease; KDIGO = Kidney Disease: Improving Global Outcomes Group; LVH = left ventricular hypertrophy; PAD = peripheral arterial disease; SCD = sudden cardiac death.
CVD and related events often present atypically in CKD and with fewer symptoms. Only 44% of late-stage CKD patients have classical pain with an acute MI (AMI) compared with preserved renal function.[16] These patients more commonly present with AMI than with stable angina.[17] They also more commonly present with non-ST segment elevation MI than ST-elevation MI.[18] As such, a high clinical suspicion must be maintained.
Assessment
CKD and related variables such as eGFR and albuminuria are rarely included in CVD risk prediction tools, limiting their use for stratification, investigation and management of these patients. Moreover, these tools are believed to underestimate CVD risk in CKD. Recent data-driven evidence has increased utility in early-stage CKD, but generalisability to ESKD remains poor.[1,19]
Biochemical and radiological investigations to stratify risk among patients are also challenging; investigations may cause adverse effects which affects the interpretation of results. Cardiac biomarkers such as troponins and N-terminal pro B-type natriuretic peptide are frequently raised in CKD, limiting their specificity for cardiac abnormality.[1,20,21] Research is needed to elucidate the significance of CKD-specific troponin thresholds and the value of serial measurements for CAD and AMI diagnosis.[22]
Gold standard radiological investigations including CT angiography and pharmacological MRI stress test may cause contrast-induced nephropathy and nephrogenic systemic sclerosis, respectively and the risks must be balanced against diagnostic significance.[23,24] Pharmacological stress echocardiography and nuclear myocardial perfusion scans are more widely available and are not subject to the same risk profiles, however they provide a lower sensitivity and specificity when compared to the gold standard tools, and when used in non-CKD patients.[24–26]
Coronary Artery Disease
CAD is common in CKD, with incidence rising linearly as eGFR declines. Simultaneous management of CAD is challenging and it is associated with a poor prognosis in these patients.[27] The mainstay of CAD management is lipid-lowering medications. Statins become less beneficial with CKD progression, with no clear benefit in dialysis patients. Newer medications are efficacious and safe in mild/moderate CKD, but effects are unclear in advanced disease. The SHARP trial and subsequent studies have argued that concomitant use of statins and ezetimibe may safely attenuate cardiovascular risk even for ESKD, although further investigation is needed.[28,29]
The alternative management of CAD is revascularisation. Although revascularisation reduces cardiovascular symptoms, it only appears to confer survival benefit in CKD patients with a high baseline cardiovascular risk, and is associated with a higher rate of renal failure.[30] The burden of permanent dialysis treatment must therefore be weighed up against the symptomatic benefits of coronary revascularisation.
The ISCHEMIA-CKD trial showed no significant mortality benefit after revascularisation in stable CAD for CKD patients.[31] Revascularisation also poses significant risks that must be considered, including contrast-induced acute kidney injury, poor access sites for cardiac catheterisation, post-procedure infection, potential implications for vascular access for dialysis and duration of dual antiplatelet therapy.[1] CKD patients are also less likely to receive guideline-recommended treatments for acute coronary syndrome. Risk-benefit analyses are challenging as these patients face a higher risk of ischaemic and haemorrhagic complications, and the mortality benefit of invasive strategies declines with worsening eGFR.[20]
Heart Failure
About half of all patients with heart failure (49%) have CKD and the combination is associated with greater mortality and hospitalisation.[3,32] HF and mortality risk worsen as renal function declines and this is independent of age, duration of HF or diabetes.[32] Diagnosis is challenging as symptoms of fluid overload such as dyspnoea and peripheral oedema are common to HF and CKD.[21]
Pharmacological management for HF with reduced ejection fraction (HFrEF) is efficacious in CKD stages 1–3. However, evidence is sparse for their use in CKD stages 4–5 as these patients are largely excluded from clinical trials. Guidelines support use of renin-angiotensin-aldosterone system inhibiting drugs for CKD-HF, yet they are often underused because of the risk of hyperkalaemia.[33] Alternative pharmacological management with diuretics and ß-blockers may cause drug resistance and electrolyte derangement.[21] Additionally, optimising CKD-related conditions can alleviate HF. There is a strong evidence base for using IV iron for iron-deficiency anaemia in CKD-HF.[34]
Notably, empagliflozin has demonstrated efficacy in treatment of HFrEF and HF with preserved ejection fraction, for which there were previously no treatments.[35,36] Empagliflozin is a sodium-glucose cotransporter 2 inhibitor that was primarily used in the treatment of type 2 diabetes, a common CKD cause and comorbidity. It has also been shown to slow the rate of renal function decline, regardless of CKD severity.[35,37]
Arrhythmias
CKD predisposes individuals to arrhythmias, most commonly AF with 16–21% of CKD patients and 15–40% of dialysis patients have AF.[38,39] AF also increases risk of CKD and its progression.[40] The conditions share many risk factors and unlike numerous CVD risk scores, the AF CHA2DS2-VASc and HAS-BLED scores work similarly in CKD as in the general population.[41,42]
Managing AF and stroke risk in these patients is challenging due to the safety and efficacy of available treatments. Direct oral anticoagulants (DOAC) are non-inferior to warfarin when creatinine clearance is 30–50 mL/min, and are markedly safer.[41,43] However, in later-stage CKD, there is conflicting evidence for using DOACs at adjusted dose and insufficient evidence to support warfarin use.[41,44] These patients have a high risk of bleeding and other adverse effects. In these patients, consideration must also be given to the competing risk of death in CKD when assessing risk benefit in AF stroke prevention.[45]
Sudden Cardiac Death
Sudden cardiac death is very common in CKD, particularly in ESKD (Figure 2). Numerous risk factors have been identified, but further research is essential to elucidate the contribution of these risk factors and to facilitate prevention strategies.[41]
Figure 2: Annual Rates of Sudden Cardiac Death.
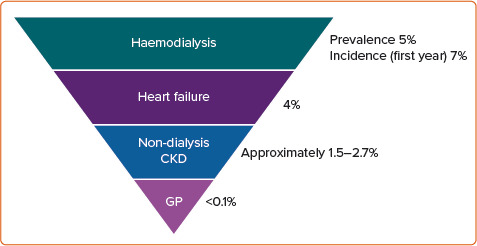
CKD = chronic kidney disease; GP = general population. Source: Turakhia et al. 2019.[41] Reproduced with permission from Oxford University Press.
Valvular Heart Disease
VHD is common in CKD and is associated with significantly reduced survival with 5-year mortality with at least mild aortic stenosis (AS) or mitral regurgitation (MR) being >50% greater than people without CKD.[46] The primary pathophysiological mechanism is valvular calcification, which is more prevalent than in the general population, worsens with declining renal function and is independently associated with adverse cardiovascular outcomes.[47–49] Clinical presentation of VHD can often be mistaken for CKD as symptoms also include dyspnoea and fatigue.
Calcimimetic drugs have been considered for VHD prevention in CKD, but this requires further study. Valvular regurgitation in these patients is often functional and potentially reversible with adjustment of volume status using dialysis. Strict volume status control may prevent the progression of VHD, but no medical intervention has shown benefit.[49]
Surgical and transcutaneous atrial valve replacement are commonly performed in these patients. These procedures carry similar risks and benefits compared to the general population in CKD stages 1–3. While this improves symptoms throughout CKD, rates of complications, progression to dialysis and mortality risk increase unacceptably with worsening eGFR.[50,51]
Percutaneous mitral valve replacement with MitraClip is also commonly performed, improving cardiac function, symptoms and renal function in CKD patients regardless of eGFR at baseline. However, these patients face worse outcomes with higher rates of hospitalisation and mortality. Careful patient selection for these interventions is therefore essential. Additionally, consideration of patients' individual treatment goals, such as symptomatic relief versus life-prolonging treatment, are pivotal to informing risk-benefit analyses and patient-centred shared decision-making.[49]
The Multidisciplinary Approach
The complex bidirectional relationship between CVD and CKD, combined with common multimorbidity and limitations of standardised risk scores, benefit from corroboration between specialists. A multidisciplinary team approach including cardiologist, nephrologists and allied healthcare professionals improves management and patient-centred HF care through joint clinics (Figure 3).[52]
Figure 3: The Delivery and Benefits of the Multidisciplinary Clinic for CKD Patients with HF.
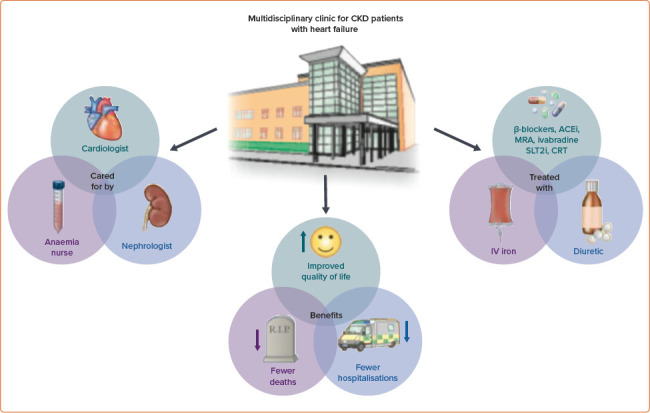
ACEi = angiotensin converting enzyme inhibitor; CRT = cardiac resynchronisation therapy; MRA = mineralocorticoid receptor antagonist; SLT2i = sodium–glucose cotransporter 2 inhibitor. Source: Banerjee and Wang. 2021.[52] Reproduced with permission from Oxford University Press.
Conclusion
CVD is very common in CKD and vice versa. The presence of each condition promotes incidence and progression of the other. Despite the high prevalence, morbidity and mortality of these comorbid conditions, there are significant limitations to our current knowledge and management of this vulnerable group. CKD patients are grossly underrepresented in CVD research, limiting generalisability of available data. Standardised risk scores that are often used to guide investigations and management in CVD are likely to underestimate risk in CKD. Moreover, investigations have poorer sensitivity and specificity and may come with unacceptable adverse effects.
Drug management is complex due to limited evidence, dose adjustments due to renal function and adverse effects. As such, these patients are less likely to receive guideline-recommended management. Interventions are largely safe and effective in CKD stages 1–3, but there is insufficient evidence to support their use in later-stage kidney disease. If interventions are used in CKD stages 4–5, they are more strongly associated with adverse effects and complications.
As CKD progresses and the incidence of CVD rises, we have less knowledge and fewer management options. The complexity of these comorbid conditions necessitates a multidisciplinary approach to improve patient-centred care.
References
- 1.Sarnak MJ, Amann K, Bangalore S et al. Chronic kidney disease and coronary artery disease: JACC state-of-the-art review. J Am Coll Cardiol. 2019;74:1823–38. doi: 10.1016/j.jacc.2019.08.1017. [DOI] [PubMed] [Google Scholar]
- 2.Watanabe H, Watanabe T, Sasaki S et al. Close bidirectional relationship between chronic kidney disease and atrial fibrillation: the Niigata Preventive Medicine study. Am Heart J. 2009;158:629–36. doi: 10.1016/j.ahj.2009.06.031. [DOI] [PubMed] [Google Scholar]
- 3.Damman K, Valente MAE, Voors AA et al. Renal impairment, worsening renal function, and outcome in patients with heart failure: an updated meta-analysis. Eur Heart J. 2014;35:455–69. doi: 10.1093/eurheartj/eht386. [DOI] [PubMed] [Google Scholar]
- 4.Ronco C, Haapio M, House AA et al. Cardiorenal syndrome. J Am Coll Cardiol. 2008;52:1527–39. doi: 10.1016/j.jacc.2008.07.051. [DOI] [PubMed] [Google Scholar]
- 5.Zannad F, Rossignol P. Cardiorenal syndrome revisited. Circulation. 2018;138:929–44. doi: 10.1161/CIRCULATIONAHA.117.028814. [DOI] [PubMed] [Google Scholar]
- 6.Charytan D, Kuntz RE. The exclusion of patients with chronic kidney disease from clinical trials in coronary artery disease. Kidney Int. 2006;70:2021–30. doi: 10.1038/sj.ki.5001934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Coca SG, Krumholz HM, Garg AX, Parikh CR. Underrepresentation of renal disease in randomized controlled trials of cardiovascular disease. JAMA. 2006;296:1377–84. doi: 10.1001/jama.296.11.1377. [DOI] [PubMed] [Google Scholar]
- 8.Konstantinidis I, Nadkarni GN, Yacoub R et al. Representation of patients with kidney disease in trials of cardiovascular Interventions: an updated systematic review. JAMA Int Med. 2016;176:121–4. doi: 10.1001/jamainternmed.2015.6102. [DOI] [PubMed] [Google Scholar]
- 9.Maini R, Wong DB, Addison D et al. Persistent underrepresentation of kidney disease in randomized, controlled trials of cardiovascular disease in the contemporary era. J Am Soc Nephrol. 2018;29:2782–6. doi: 10.1681/ASN.2018070674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ishida JH, Chauhan C, Gillespie B et al. Understanding and overcoming the challenges related to cardiovascular trials involving patients with kidney disease. Clin J Am Soc Nephrol. 2021;16:1435–44. doi: 10.2215/CJN.17561120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gansevoort RT, Correa-Rotter R, Hemmelgarn BR et al. Chronic kidney disease and cardiovascular risk: epidemiology, mechanisms, and prevention. Lancet. 2013;382:339–52. doi: 10.1016/S0140-6736(13)60595-4. [DOI] [PubMed] [Google Scholar]
- 12.Chertow GM, Block GA, Correa-Rotter R et al. Effect of cinacalcet on cardiovascular disease in patients undergoing dialysis. N Engl J Med. 2012;367:2482–94. doi: 10.1056/NEJMoa1205624. [DOI] [PubMed] [Google Scholar]
- 13.Wanner C, Amann K, Shoji T. The heart and vascular system in dialysis. Lancet. 2016;388:276–84. doi: 10.1016/S0140-6736(16)30508-6. [DOI] [PubMed] [Google Scholar]
- 14.United States Renal Data System. Cardiovascular disease in patients with CKD. In: 2020 Annual Data Report. 2020. https://adr.usrds.org/2020/chronic-kidney-disease/4-cardiovascular- disease-in-patients-with-ckd (accessed 24 August 2021)
- 15.Wheeler DC, London GM, Parfrey PS et al. Effects of cinacalcet on atherosclerotic and nonatherosclerotic cardiovascular events in patients receiving hemodialysis: the EValuation Of Cinacalcet HCl Therapy to Lower CardioVascular Events (EVOLVE) trial. J Am Heart Assoc. 2014;3:e001363. doi: 10.1161/JAHA.114.001363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sosnov J, Lessard D, Goldberg RJ et al. Differential symptoms of acute myocardial infarction in patients with kidney disease: a community-wide perspective. Am J Kidney Dis. 2006;47:378–84. doi: 10.1053/j.ajkd.2005.11.017. [DOI] [PubMed] [Google Scholar]
- 17.Go AS, Bansal N, Chandra M et al. Chronic kidney disease and risk for presenting with acute myocardial infarction versus stable exertional angina in adults with coronary heart disease. J Am Coll Cardiol. 2011;58:1600–7. doi: 10.1016/j.jacc.2011.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Shroff GR, Li S, Herzog CA. Trends in discharge claims for acute myocardial infarction among patients on dialysis. J Am Soc Nephrol. 2017;28:1379–83. doi: 10.1681/ASN.2016050560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Anker SD, Gillespie IA, Eckardt KU et al. Development and validation of cardiovascular risk scores for haemodialysis patients. Int J Cardiol. 2016;216:68–77. doi: 10.1016/j.ijcard.2016.04.151. [DOI] [PubMed] [Google Scholar]
- 20.Collet JP, Thiele H, Barbato E et al. 2020 ESC guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation. Eur Heart J. 2021;42:1289–367. doi: 10.1093/eurheartj/ehaa575. [DOI] [PubMed] [Google Scholar]
- 21.House AA, Wanner C, Sarnak MK et al. Heart failure in chronic kidney disease: conclusions from a Kidney Disease: Improving Global Outcomes (KDIGO) Controversies Conference. Kidney Int. 2019;95:1304–17. doi: 10.1016/j.kint.2019.02.022. [DOI] [PubMed] [Google Scholar]
- 22.Banerjee D, Perrett C, Banerjee A. Troponins, acute coronary syndrome and renal disease: from acute kidney injury through end-stage kidney disease. Eur Cardiol. 2019;14:187–90. doi: 10.15420/ecr.2019.28.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rudnick MR, Leonberg-Yoo AK, Litt HI et al. The controversy of contrast-induced nephropathy with intravenous contrast: what is the risk? Am J Kidney Dis. 2020;75:105–13. doi: 10.1053/j.ajkd.2019.05.022. [DOI] [PubMed] [Google Scholar]
- 24.Dilsizian V, Gewirtz H, Marwick TH et al. Cardiac imaging for coronary heart disease risk stratification in chronic kidney disease. JACC Cardiovasc Imaging. 2021;14:669–82. doi: 10.1016/j.jcmg.2020.05.035. [DOI] [PubMed] [Google Scholar]
- 25.Winther S, Svensson M, Jørgensen HS et al. Diagnostic performance of coronary CT angiography and myocardial perfusion imaging in kidney transplantation candidates. JACC Cardiovasc Imaging. 2015;8:553–62. doi: 10.1016/j.jcmg.2014.12.028. [DOI] [PubMed] [Google Scholar]
- 26.Wang LW, Fahim MA, Hayen A et al. Cardiac testing for coronary artery disease in potential kidney transplant recipients. Cochrane Database Syst Rev. 2011;12:CD008691. doi: 10.1002/14651858.CD008691.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sarnak MJ, Amann K, Bangalore S et al. Chronic kidney disease and coronary artery disease: JACC state-of-the-art review. J Am Coll Cardiol. 2019;74:1823–38. doi: 10.1016/j.jacc.2019.08.1017. [DOI] [PubMed] [Google Scholar]
- 28.Baigent C, Landray MJ, Reith C et al. The effects of lowering LDL cholesterol with simvastatin plus ezetimibe in patients with chronic kidney disease (Study of Heart and Renal Protection): a randomised placebo-controlled trial. Lancet. 2011;377:2181–92. doi: 10.1016/S0140-6736(11)60739-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Stanifer JW, Charytan DM, White J et al. Benefit of ezetimibe added to simvastatin in reduced kidney function. J Am Soc Nephrol. 2017;28:3034–43. doi: 10.1681/ASN.2016090957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Charytan DM, Natwick T, Solid CA et al. Comparative effectiveness of medical therapy, percutaneous revascularization, and surgical coronary revascularization in cardiovascular risk subgroups of patients with CKD: a retrospective cohort study of medicare beneficiaries. Am J Kidney Dis. 2019;74:463–73. doi: 10.1053/j.ajkd.2019.04.018. [DOI] [PubMed] [Google Scholar]
- 31.Bangalore S, Maron DJ, O'Brien SM et al. Management of coronary disease in patients with advanced kidney disease. N Engl J Med. 2020;382:1608–18. doi: 10.1056/NEJMoa1915925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Löfman I, Szummer K, Dahlström U et al. Associations with and prognostic impact of chronic kidney disease in heart failure with preserved, mid-range, and reduced ejection fraction. Eur J Heart Fail. 2017;19:1606–14. doi: 10.1002/ejhf.821. [DOI] [PubMed] [Google Scholar]
- 33.Murphy D, Ster IC, Kaski JC et al. The LIFT trial: study protocol for a double-blind, randomised, placebo-controlled trial of K+-binder Lokelma for maximisation of RAAS inhibition in CKD patients with heart failure. BMC Nephrol. 2021;22:254. doi: 10.1186/s12882-021-02439-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Macdougall IC, Bircher AJ, Eckhardt K-U et al. Iron management in chronic kidney disease: conclusions from a Kidney Disease: Improving Global Outcomes (KDIGO) Controversies Conference. Kidney Int. 2016;89:28–39. doi: 10.1016/j.kint.2015.10.002. [DOI] [PubMed] [Google Scholar]
- 35.Packer M, Anker SD, Butler J et al. Cardiovascular and renal outcomes with empagliflozin in heart failure. 2020;383:1413–24. doi: 10.1056/NEJMoa2022190. [DOI] [PubMed] [Google Scholar]
- 36.Anker SD, Butler J, Filippatos G et al. Empagliflozin in heart failure with a preserved ejection fraction. N Engl J Med. 2021;385:1451–61. doi: 10.1056/NEJMoa2107038. [DOI] [PubMed] [Google Scholar]
- 37.Zannad F, Ferreira JP, Pocock SJ et al. Cardiac and kidney benefits of empagliflozin in heart failure across the spectrum of kidney function: insights from EMPEROR-Reduced. Circulation. 2021;143:310–21. doi: 10.1161/CIRCULATIONAHA.120.051685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ananthapanyasut W, Napan S, Rudolph EH et al. Prevalence of atrial fibrillation and its predictors in nondialysis patients with chronic kidney disease. Clin J Am Soc Nephrol. 2010;5:173–81. doi: 10.2215/CJN.03170509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Königsbrügge O, Posch F, Antlanger M et al. Prevalence of atrial fibrillation and antithrombotic therapy in hemodialysis patients: cross-sectional results of the Vienna InVestigation of AtriaL Fibrillation and Thromboembolism in Patients on HemoDIalysis (VIVALDI). PLoS One. 2017;12:e0169400. doi: 10.1371/journal.pone.0169400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Bansal N, Xie D, Kelvin T et al. Atrial fibrillation and risk of ESRD in adults with CKD. Clin J Am Soc Nephrol. 2016;11:1189–96. doi: 10.2215/CJN.10921015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Turakhia MP, Blanksetijn PJ, Carrero JJ et al. Chronic kidney disease and arrhythmias: conclusions from a Kidney Disease: Improving Global Outcomes (KDIGO) Controversies Conference. Eur Heart J. 2018;39:2314–25. doi: 10.1093/eurheartj/ehy060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Bonde AN, Lip GYH, Kamper AN et al. Net clinical benefit of antithrombotic therapy in patients with atrial fibrillation and chronic kidney disease: a nationwide observational cohort study. J Am Coll Cardiol. 2014;64:2471–82. doi: 10.1016/j.jacc.2014.09.051. [DOI] [PubMed] [Google Scholar]
- 43.Hindricks G, Potpara T, Dagres N et al. 2020 ESC guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association for Cardio-Thoracic Surgery (EACTS). Eur Heart J. 2021;42:373–498. doi: 10.1093/eurheartj/ehaa612. [DOI] [PubMed] [Google Scholar]
- 44.Hylek EM. Apixaban for end-stage kidney disease: More questions for the randomized trials. Circulation. 2018;138:1534–6. doi: 10.1161/CIRCULATIONAHA.118.036449. [DOI] [PubMed] [Google Scholar]
- 45.Shih CJ, Ou SM, Chao PW et al. Risks of death and stroke in patients undergoing hemodialysis with new-onset atrial fibrillation: a competing-risk analysis of a nationwide cohort. Circulation. 2016;133:265–72. doi: 10.1161/CIRCULATIONAHA.115.018294. [DOI] [PubMed] [Google Scholar]
- 46.Samad Z, Sivak JA, Phelan M et al. Prevalence and outcomes of left-sided valvular heart disease associated with chronic kidney disease. J Am Heart Assoc. 2017;6:e006044. doi: 10.1161/JAHA.117.006044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Guerraty MA, Chai B, Hsu JY et al. Relation of aortic valve calcium to chronic kidney disease (from the Chronic Renal Insufficiency Cohort study) Am J Cardiol. 2015;115:1281–6. doi: 10.1016/j.amjcard.2015.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Raggi P, Bellasi A, Gamboa C et al. All-cause mortality in hemodialysis patients with heart valve calcification. Clin J Am Soc Nephrol. 2011;6:1990–5. doi: 10.2215/CJN.01140211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Marwick TH, Amann K, Bangalore S et al. Chronic kidney disease and valvular heart disease: conclusions from a Kidney Disease: Improving Global Outcomes (KDIGO) Controversies Conference. Kidney Int. 2019;96:836–49. doi: 10.1016/j.kint.2019.06.025. [DOI] [PubMed] [Google Scholar]
- 50.Thourani VH, Keeling WB, Sarin EL et al. Impact of preoperative renal dysfunction on long-term survival for patients undergoing aortic valve replacement. Ann Thorac Surg. 2011;91:1798–806. doi: 10.1016/j.athoracsur.2011.02.015. [DOI] [PubMed] [Google Scholar]
- 51.Hansen JW, Foy A, Yadav P et al. Death and dialysis after transcatheter aortic valve replacement: an analysis of the STS/ACC TVT Registry. JACC Cardiovasc Interv. 2017;10:2064–75. doi: 10.1016/j.jcin.2017.09.001. [DOI] [PubMed] [Google Scholar]
- 52.Banerjee D, Wang AYM. Personalizing heart failure management in chronic kidney disease patients. Nephrol Dial Transplant. 2021. epub ahead of press. [DOI] [PubMed]


