Abstract
Using nationally representative longitudinal data from Wave 1 to Wave 4 of the Population Assessment of Tobacco and Health Study in the United States, we examined whether the association between menthol cigarette use and smoking cessation was modified by race/ethnicity and e-cigarette use. Multivariable discrete-time survival models were fit to an unbalanced person-period data set (person n=7423, risk period n=18,897) for adult respondents (ages 25+) who were current established cigarette smokers at baseline. We found that adults who smoke menthol cigarettes had lower odds of smoking cessation, but the effect was modified by race/ethnicity as non-Hispanic (NH) Black menthol smokers had lower odds of quitting smoking than NH White or Hispanic menthol smokers. We also found that e-cigarette use was associated with higher odds of smoking cessation among both menthol and non-menthol smokers, but the association was stronger among menthol smokers. Our results suggest that a menthol smoking ban may have a favorable impact on smoking cessation for NH Black adults. In addition, our results also suggest that a menthol smoking ban may be more effective if menthol smokers have access to e-cigarettes as a way to quit cigarette use.
Keywords: Menthol, Cessation, Disparities, E-cigarettes
INTRODUCTION
Despite large decreases in the prevalence of cigarette smoking in recent decades, tobacco use remains the leading cause of preventable death in the United States.1 Further reducing cigarette use therefore remains a key priority for improving population health. One way the Food and Drug Administration (FDA) may achieve this reduction is by banning menthol in cigarettes.2 In the US, menthol cigarette use accounts for nearly 40% of cigarette smoking,3 and the market share for menthol cigarettes has grown by 10% since 2000.4 Because menthol cigarettes are designed to mask the harshness of smoking, it is believed that menthol cigarette use facilitates smoking initiation, leads to higher levels of smoking dependence and decreases the likelihood of smoking cessation.5
Several studies have examined the association between menthol cigarette use and smoking cessation in the United States. While the strength of this association has come into question,6,7 the weight of evidence suggests that menthol cigarette use is associated with a lower likelihood of smoking cessation.8–11 Research from clinical trials and cessation clinics provides additional evidence suggesting that smoking cessation may be lower for menthol smokers than for non-menthol smokers.12–14
There also appears to be racial/ethnic disparities in the association between menthol cigarette use and smoking cessation. These disparities are reflected in the FDA’s 2013 evaluation of the scientific literature where they concluded that the impact of menthol flavoring on cigarette use cessation was strongest among Black menthol smokers who were the least likely to quit.5 Other research has drawn similar conclusions,8,14–16 providing further evidence that racial/ethnic differences in smoking cessation for menthol smokers result in tobacco use disparities. A recent meta-analysis found that 47% of the explainable heterogeneity between studies on the menthol-cessation association was due to racial/ethnic differences and that smoking cessation was 12% lower among non-Hispanic (NH) Black smokers than NH White smokers.17
While a relatively large body of evidence has associated menthol cigarette use with lower levels of cessation, especially among NH Black smokers, very little research has established this relationship using nationally representative longitudinal data. However, two longitudinal studies using data from the Population Assessment of Tobacco Health Study (PATH) have recently been published. In the first study, Schneller et al18 examined the longitudinal association between different menthol delivery systems (i.e., menthol in cigarette tobacco, crushable menthol capsules in the cigarette filter) and smoking cessation for adult smokers over a one-year interval (Waves 1 and 2). They found no statistically significant differences in cessation for menthol and non-menthol smokers after adjusting for sociodemographic characteristics, but they did not test for effect modification by race/ethnicity.18 In the second study, Mills et al19 used data from Waves 1 through 4 of PATH to examine the relationship between menthol cigarettes, cessation and relapse for non-daily and daily adult smokers. They found that smoking cessation (measured as non-current past 30-day cigarette use) was lower among daily menthol smokers but not among non-daily menthol smokers, and menthol smokers were no more likely than non-menthol smokers to relapse. The authors also stratified the results by race/ethnicity, and found that the odds of smoking cessation was lower among non-Hispanic Black and non-Hispanic White daily menthol smokers but not for Hispanic or Other racial/ethnic group members.19
Much of the research on the menthol-cessation association has focused on identifying disparities in cessation while very little research has examined whether other characteristics, such as e-cigarette use, can affect smoking cessation among menthol smokers. There is conflicting epidemiological evidence on the role of e-cigarette use in smoking cessation,20,21 but a growing body of research has found that e-cigarette use facilitates smoking cessation.22–25 Studies have yet to explore the differential role that e-cigarette use may play in smoking cessation for menthol and non-menthol smokers, although one community-based study found that menthol smokers were more likely to consider using e-cigarettes to help them quit smoking compared to non-menthol smokers.26 These findings are consistent with the results from a discrete choice experiment where menthol smokers reported they would be willing to switch to e-cigarettes, but only if flavored e-cigarettes are not banned.27 Recent population-based evidence further demonstrates that menthol cigarette users switched to e-cigarettes at high rates, especially for menthol/mint flavored e-cigarettes, relative to non-menthol smokers.28 Given that one of the primary motivations for e-cigarette use among adults smokers is to help facilitate smoking cessation,29,30 it is plausible that menthol smokers may find e-cigarettes more appealing than non-menthol smokers, and thus use them more effectively as a smoking cessation aid.
Our study uses data from the first four waves of the PATH Study, an ongoing longitudinal cohort study, to examine the association between menthol cigarette use and smoking cessation. Our study adds to the literature on menthol cigarette cessation by: (1) examining whether smoking cessation differs by race/ethnicity using a nationally representative longitudinal sample of US adults; (2) testing whether e-cigarette use has a differential impact on smoking cessation for menthol and non-menthol smokers. To our knowledge, this is the first study to investigate whether the menthol-cessation relationship is modified by e-cigarette use, accounting for time-varying patterns of menthol smoking and e-cigarette use.
MATERIALS AND METHODS
Data
The PATH Study is a nationally representative, longitudinal cohort study of the civilian US population. Wave 1 data were collected from September 2013 to December 2014; Wave 2 data were collected from October 2014 to October 2015; Wave 3 data were collected from October 2015 to October 2016; Wave 4 data were collected from December 2016 to January 2018. Further details about the design of the PATH Study are available elsewhere.31 Since we used de-identified publicly available PATH data, this study was classified as not regulated human subjects research by the University of Michigan Institution Review Board.
The analytic sample for the current study was restricted to adult respondents age 25 or older at Wave 1 (to capture respondents’ highest level of education and to exclude ages during which smoking patterns have not yet been established),32 who were current established smokers and responded to at least one of the subsequent follow-up interviews. Current established cigarette smokers were defined as respondents who smoked at least 100 cigarettes in their lifetime and reported smoking every day or some days at the baseline interview. A flowchart summarizing the stages of sample selection can be found in Figure 1.
Figure 1.
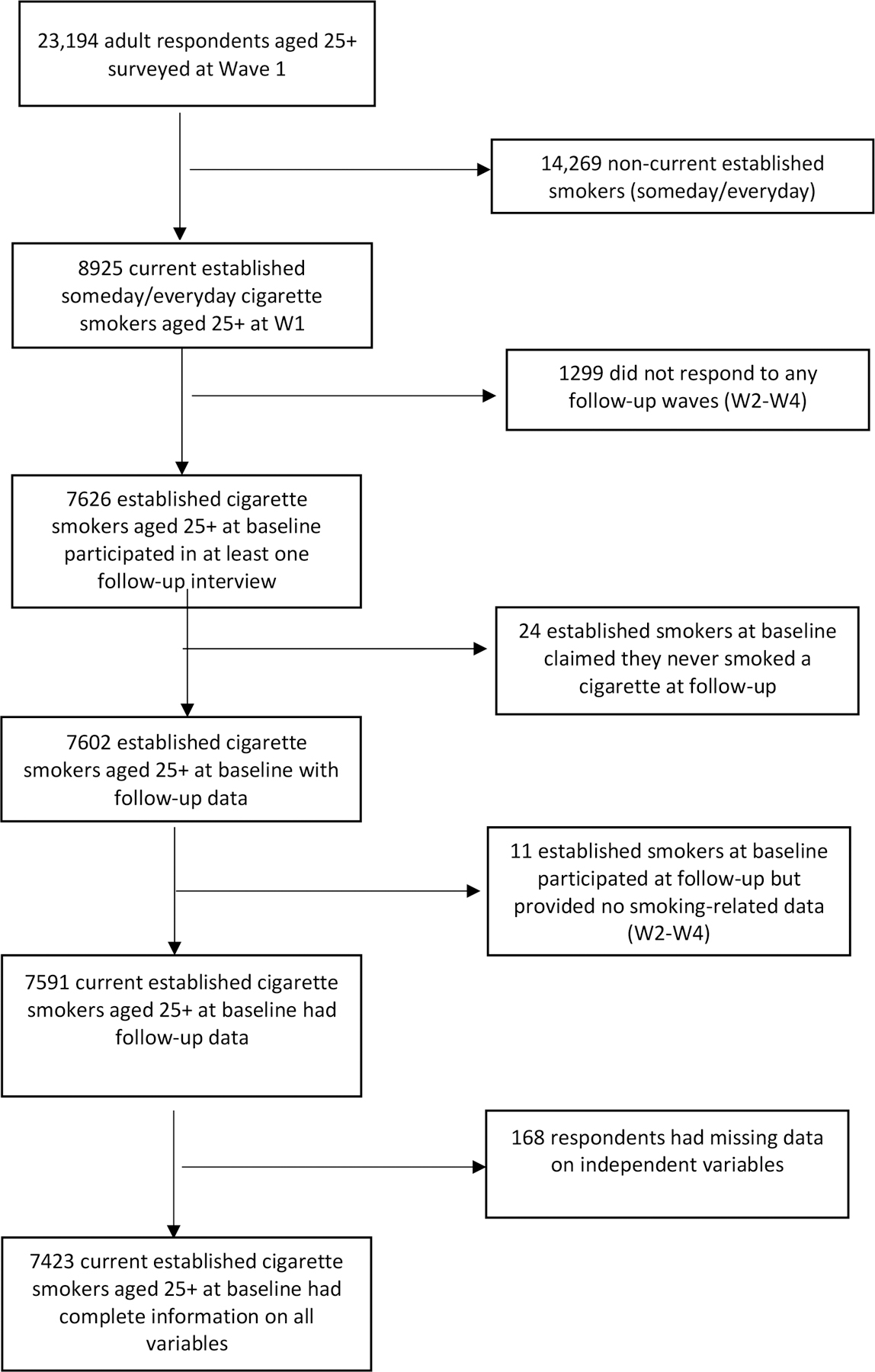
Flowchart of Sample Selection, PATH Adult (W1-W4)
Measures
We operationalized smoking cessation as discontinued cigarette smokers who self-reported completely quitting smoking. Discontinued smoking status was defined as current established cigarette smokers at baseline (Wave 1) who reported no past 30-day cigarette use at any follow-up. Discontinued cigarette smokers were also asked the following question, “have you completely quit smoking cigarettes?” Respondents were categorized as continuing smokers if they reported current smoking at follow-up or if they were discontinued smokers who reported they had not completely quit smoking at follow-up (n=225). Discontinued cigarette smokers who reported they completely quit smoking were considered to have successfully quit smoking cigarettes.
Menthol cigarette flavoring was the exposure variable, and consistent with other research,8,13,17,33 respondents were classified as menthol cigarette smokers if their regular brand was “flavored to taste like menthol or mint.” Current smokers were asked this question at each wave, and we found evidence that menthol cigarette use did change over time as 4.4% of nonmenthol smokers transitioned to menthol cigarette use, while 8.3% of menthol smokers transitioned to non-menthol cigarette use between Wave 1 and Wave 4. To capture changes in cigarette flavoring preference, menthol cigarette use was included as a time-varying measure that was lagged (t-1) to ensure that the menthol exposure variable preceded the outcome.
To examine sociodemographic differences, we included age (25–34, 35–54, 55+), sex (0=female, 1=male), race/ethnicity (NH White, NH Black, NH Other, Hispanic), education (high school/GED or less, some college, college degree or higher), and household income (0=less than $49,999, 1 = $50,000 +) as baseline sociodemographic variables. Missing values for baseline sociodemographic variables were updated with data from other waves when available to reduce item non-response. We also included tobacco dependence, derived based on a validated 16-item scale,34 at baseline to control for differences in nicotine addiction among respondents. The tobacco dependence scale was standardized with a mean of 0 and a standard deviation of 1. As is commonly done in other research21, we examined current e-cigarette use, which was then included as a time-varying covariate to allow for changes in e-cigarette use over time. We found that 7.3% of non-cigarette users transitioned to e-cigarette users, while 57.5% of e-cigarette users at baseline transitioned away from e-cigarette use between Wave 1 and Wave 4. Respondents who reported using e-cigarettes every day or some days were defined as current e-cigarette users at each wave (0=no e-cigarette use; 1=every day or some days). For a sensitivity analysis, we also included current frequent e-cigarette use (measured as 10+ days in the past 30 days).
Statistical Analysis
Descriptive statistics were first calculated for sociodemographic and tobacco-related characteristics according to respondent’s menthol cigarette use at baseline. Chi-square tests or Fisher’s exact tests were used to test for statistically significant differences between these groups. Lifetables were then used to describe the distribution of event occurrence.35 The lifetable provides unweighted counts of smoking cessation or censoring at each time interval and unadjusted survival and hazard probability estimates.
We fitted a series of multivariable discrete-time survival models predicting smoking cessation over three one-year time intervals through Wave 2 to Wave 4 (W2-W4). Discrete-time models are appropriate when the exact timing until an event is not known.35 Our models were fit to an unbalanced person-period data set where each individual contributed a number of rows equal to the time period until they quit smoking or were censored.36 Respondents were removed from the risk set at the time of quitting and respondents who did not quit smoking were right censored at their last observation point. This means that each of the 7423 respondents in our study had a separate row of data for each risk period, with a maximum of three rows per person, resulting in a person-period dataset with 18,897 observations. The structure of the reorganized person-period dataset allowed for an examination of the conditional probability of smoking cessation at each discrete time interval. Four discrete-time survival models were estimated using a general linear modelling (GLM) approach with a binomial distribution and logit link function on the person-period data set. Model 1 included a measure for the main effect of time (i.e., baseline hazard) and the menthol cigarette exposure variable. Model 2 added the sociodemographic control variables and Model 3 added tobacco dependence and e-cigarette use. Model 4 tested the interactions between menthol cigarette use and both race/ethnicity and e-cigarette use separately. The marginal interactive effects represent whether the change in the probability of smoking cessation was statistically different across the categorical independent variables.37 We graphed the predicted probabilities for the statistically significant interactions (P <0.05).
Data were weighted using Wave 1 weights, including full-sample and 100 replicate weights, to ensure that our respondents were representative of non-institutionalized adult population in the United States at baseline.38 As a sensitivity analysis, the multivariable models were also estimated with the longitudinal cohort of respondents who participated in all waves of the PATH Study using the “all waves weights” (person-period n=5741, risk period n=15,869). Additionally, we conducted a second sensitivity analysis including all respondents aged 18–24 (person-period n=9468, risk period n=23,890) to ensure that restricting our analytic sample to adults aged 25 and older at baseline did not bias the results. For all analyses, variances were computed using the balanced repeated replication methods with Fay’s adjustment set to 0.3 as recommended by the PATH study.38,39 All analyses were conducted using Stata 16.1.
RESULTS
Table 1 shows the population weighted sociodemographic characteristics and smoking behaviours at baseline. Current established smokers were most likely to be between 35 and 54 years old (45.9%), male (53%), and NH White (67.8%). The majority of current established smokers also reported a household income of less than $50,000 (74.5%) and did not report any postsecondary education (54.5%). At baseline, approximately one third of current established smokers (36.2%) reported menthol cigarette use, and one fifth (20.3%) reported using e-cigarettes some days or every day.
Table 1.
Weighted Sociodemographic and Smoking Behaviors of Current, Established Adult (25+) Cigarette Smokers at baseline in the Population Assessment of Tobacco Health (PATH) Study (n=7423)
| N | % | 95% CI | |
|---|---|---|---|
| Age Group | |||
| 25–34 | 2177 | 28.6% | [27.4–29.8] |
| 35–54 | 3452 | 45.9% | [44.7–47.1] |
| 55+ | 1794 | 24.3% | [24.3–26.8] |
| Sex | |||
| Female | 3731 | 47.0% | [45.7–48.2] |
| Male | 3692 | 53.0% | [51.8–54.3] |
| Race/Ethnicity | |||
| Hispanic | 858 | 10.4% | [9.6–11.3] |
| NH White | 4094 | 67.8% | [68.3–71.3] |
| NH Black | 1075 | 14.4% | [13.4–15.5] |
| NH Other | |||
| Education | 496 | 5.4% | [4.9–6.0] |
| HS degree or less | 3817 | 54.5% | [53.2–55.9] |
| Some college | 2710 | 33.5% | [32.2–34.8] |
| College or more | 896 | 12.0% | [11.2–12.8] |
| Household Income | |||
| $49,999 or less | 5613 | 74.5% | [59.7–63.5] |
| $50,000 or more | 1811 | 25.5% | [67.9–72.4] |
| E-cigarette use (every/someday) | |||
| No | 5883 | 79.7% | [78.6–80.7] |
| Yes | 1540 | 20.3% | [19.3–21.4] |
| Menthol Smoking Status | |||
| No | 4672 | 63.8% | [62.3–65.3] |
| Yes | 2751 | 36.2% | [34.7–37.7] |
Lifetables describing the distribution of smoking cessation are shown in Table 2. The overall rate for continued smoking among established smokers at baseline was 78.8% through Wave 4 (95% CI 77.8,79.7), and differences in the rate were observed for menthol and non-menthol smokers. At the end of Wave 4, 77.8% (95% CI: 76.5,79.0) of non-menthol smokers continued smoking cigarettes while 80.4% (95% CI: 78.8,81.9) of menthol smokers continued smoking cigarettes. The hazard rate for smoking cessation decreased for both menthol and non-menthol smokers over time, meaning that the conditional probability of cessation was lower at each subsequent wave regardless of baseline menthol status.
Table 2:
Life Table Describing Quitting Smoking for Menthol and Nonmenthol Smokers (n=7423)
| Interval | Smokers | Cessation | Censored | Survival (95% CI) | Hazard Rate (95% CI) |
|---|---|---|---|---|---|
| Non-Menthol Smokers | |||||
| Period 1 (W1-W2) | 4671 | 406 | 642 | 0.913 [.905–.921] | 0.087 [.079–.096] |
| Period 2 (W2-W3) | 3923 | 320 | 415 | 0.839 [.828–.849] | 0.082 [.073–.091] |
| Period 3 (W3-W4) | 3188 | 231 | 2957 | 0.778 [.765–.790] | 0.073 [.063–.082] |
| Menthol Smokers | |||||
| Period 1 (W1-W2) | 2752 | 222 | 168 | 0.919 [.908–.929] | 0.087 [.070–.092] |
| Period 2 (W2-W3) | 2362 | 162 | 206 | 0.856 [.842–.869] | 0.069 [.058–.079] |
| Period 3 (W3-W4) | 2007 | 121 | 1873 | 0.804 [.788–.819] | 0.061 [.050–.072] |
| Total Sample | |||||
| Period 1 (W1-W2) | 7423 | 628 | 510 | 0.915 [.909–.922] | 0.085 [.078–.091] |
| Period 2 (W2-W3) | 6285 | 482 | 621 | 0.845 [.837–.853] | 0.077 [.070–.084] |
| Period 3 (W3-W4) | 5182 | 352 | 4830 | 0.788 [.778–.797] | 0.068 [.061–.075] |
Table 3 presents the results from four multivariable discrete-time survival analyses models predicting smoking cessation. The exposure variable, menthol cigarette use in the prior year, was associated with decreased odds of smoking cessation in Model 1 (AOR=0.83; 95% CI: 0.73,0.94). This association was attenuated once we added sociodemographic and tobacco-related control variables in Model 2 (AOR=0.89; 95% CI: 0.78,1.02) and e-cigarette use and tobacco dependence in Model 3 (AOR=0.88; 95% CI: 0.76,1.00). Several other covariates were also associated with smoking cessation. In the multivariable main effect model (Model 3), we found that respondents between ages 35 and 54 at baseline (compared to 25–34) had lower odds of reporting smoking cessation (AOR=0.76; 95% CI: 0.66,0.87), and that having a family income of $50,000 or more (AOR=1.28; 95% CI: 1.13,1.45) and having started (AOR=1.35; 95% CI: 1.17,1.57) or completed a college education (AOR=1.62; 95% CI: 1.37,1.92) were associated with higher odds of smoking cessation, compared to having a family income of less than $50,000 or high school education or less, respectively. In addition, for every standard deviation increase in tobacco dependence, the odds of smoking cessation were reduced by 36% (AOR=0.64; 95% CI: 0.59,0.69).
Table 3.
Discrete Time Survival Analysis Predicting Smoking Cessation (W1 Weights), PATH Adult (25+) W1-W4
| Model 1a | Model 2b | Model 3c | Model 4d | |||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| AOR | CI | AOR | 95% CI | AOR | 95% CI | AOR | 95% CI | |
| Period 1 | 0.10*** | [.09–.11] | 0.08*** | [.07–.10] | 0.08*** | [.06–.09] | 0.08*** | [.06–.09] |
| Period 2 | 0.09*** | [.08–.10] | 0.07*** | [.06–.09] | 0.07*** | [.06–.08] | 0.07*** | [.06–.08] |
| Period 3 | 0.08*** | [.07–.09] | 0.07*** | [.05–.08] | 0.06*** | [.05–.08] | 0.06*** | [.05–.08] |
| Menthol cig use TVC | 0.83** | [.73–.94] | 0.89 | [.78–1.02] | 0.88* | [.76–1.00] | 0.89 | [.73–1.07] |
| Age group | ||||||||
| 25–34 | REF | REF | REF | REF | REF | REF | ||
| 35–54 | 0.69*** | [.61–.80] | 0.76*** | [.66–.87] | 0.76*** | [.66–.88] | ||
| 55+ | 0.88 | [.75–1.03] | 0.95 | [.81–1.11] | 0.95 | [.81–1.12] | ||
| Sex (male=1) | 1.1 | [.97–1.24] | 1.05 | [.93–1.19] | 1.05 | [.93–1.19] | ||
| Race/Ethnicity | ||||||||
| Hispanic | 1.46*** | [1.22–1.74] | 1.20* | [1.00–1.43] | 1.17 | [.92–1.48] | ||
| NH White | REF | REF | REF | REF | REF | REF | ||
| NH Black | 0.77* | [.61–.99] | 0.72** | [.56–.92] | 0.97 | [.64–1.46] | ||
| NH Other | 1.05 | [.83–1.34] | 1.01 | [.78–1.29] | 1.25 | [.94–1.66] | ||
| Education | ||||||||
| High School or less | REF | REF | REF | REF | REF | REF | ||
| Some college | 1.41*** | [1.22–1.63] | 1.35*** | [1.17–1.57] | 1.36*** | [1.17–1.57] | ||
| College or more | 1.95*** | [1.63–2.32] | 1.62*** | [1.37–1.92] | 1.61*** | [1.36–1.91] | ||
| Household Income | ||||||||
| <$49,999 | REF | REF | REF | REF | REF | REF | ||
| 50,000 > | 1.35*** | [1.19–1.53] | 1.28*** | [1.13–1.45] | 1.28*** | [1.13–1.45] | ||
| Tobacco Dependence | 0.64*** | [.59–.69] | 0.64*** | [.59–.69] | ||||
| E-cigarette use (every/some days) | 1.34** | [1.13–1.59] | 1.17 | [.94–1.45] | ||||
| Menthol*e-cig Interaction | 1.49* | [1.10–2.02] | ||||||
| Menthol*race/ethnicity | ||||||||
| Hispanic | 1.02 | [.71–1.45] | ||||||
| NH White | REF | REF | ||||||
| NH Black | 0.64* | [.41–.98] | ||||||
| NH Other | 0.45* | [.23–.86] | ||||||
Notes: Person N =7423; Risk Period N= 18,897
p<0.05
p<0.01
p<0.001
Tobacco use exposure
sociodemographic variables added
tobacco dependence added
interaction model
We examined effect modification of the association between menthol smoking and cessation by race/ethnicity and e-cigarette use in Model 4. We found statistically significant differences by race/ethnicity (F=3.72, P<0.05) and by e-cigarette use (F=6.82, P<0.05). Displayed in Figure 2, we found that the predicted probability of smoking cessation was lower for NH Black and NH Other adults who used menthol versus non-menthol cigarettes, while there were no differences in cessation for menthol versus non-menthol cigarette use for NH White or Hispanic adults. We also found that current everyday/someday e-cigarette use increased the predicted probability of smoking cessation among both non-menthol and menthol smokers, but that the association was more pronounced among menthol smokers (Figure 3). In the sensitivity analysis, the association of e-cigarette use on smoking cessation was greater when we defined e-cigarette use as 10+ days in the past 30 days rather than every day or someday use. However, the menthol by e-cigarette interaction using both e-cigarette definitions produced similar results (see Figure A1 and Table A1, Appendix).
Figure 2.
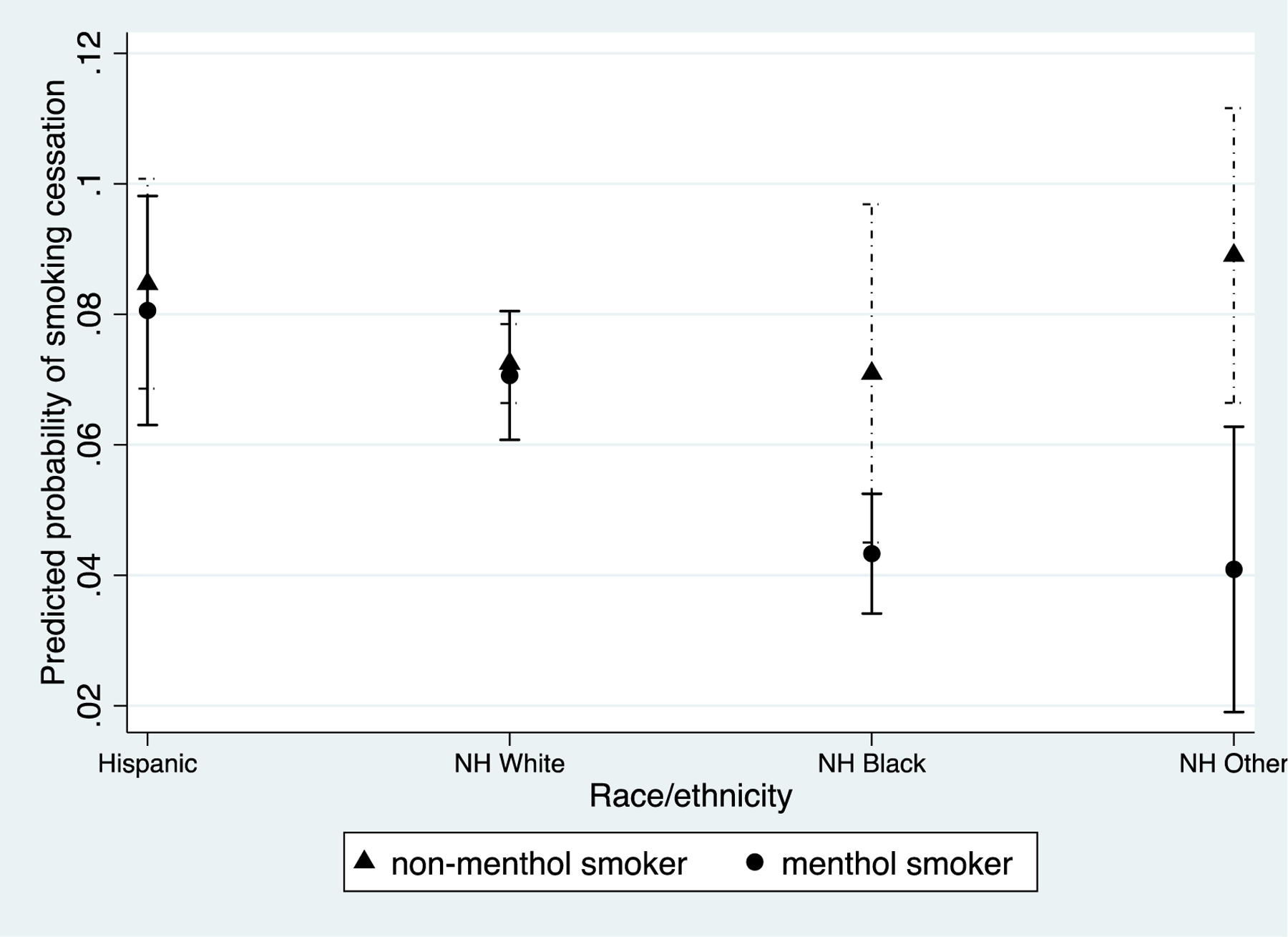
Predicted Probability of Smoking Cessation for Menthol and Non-Menthol Smokers by Race/Ethnicity.
Figure 3.
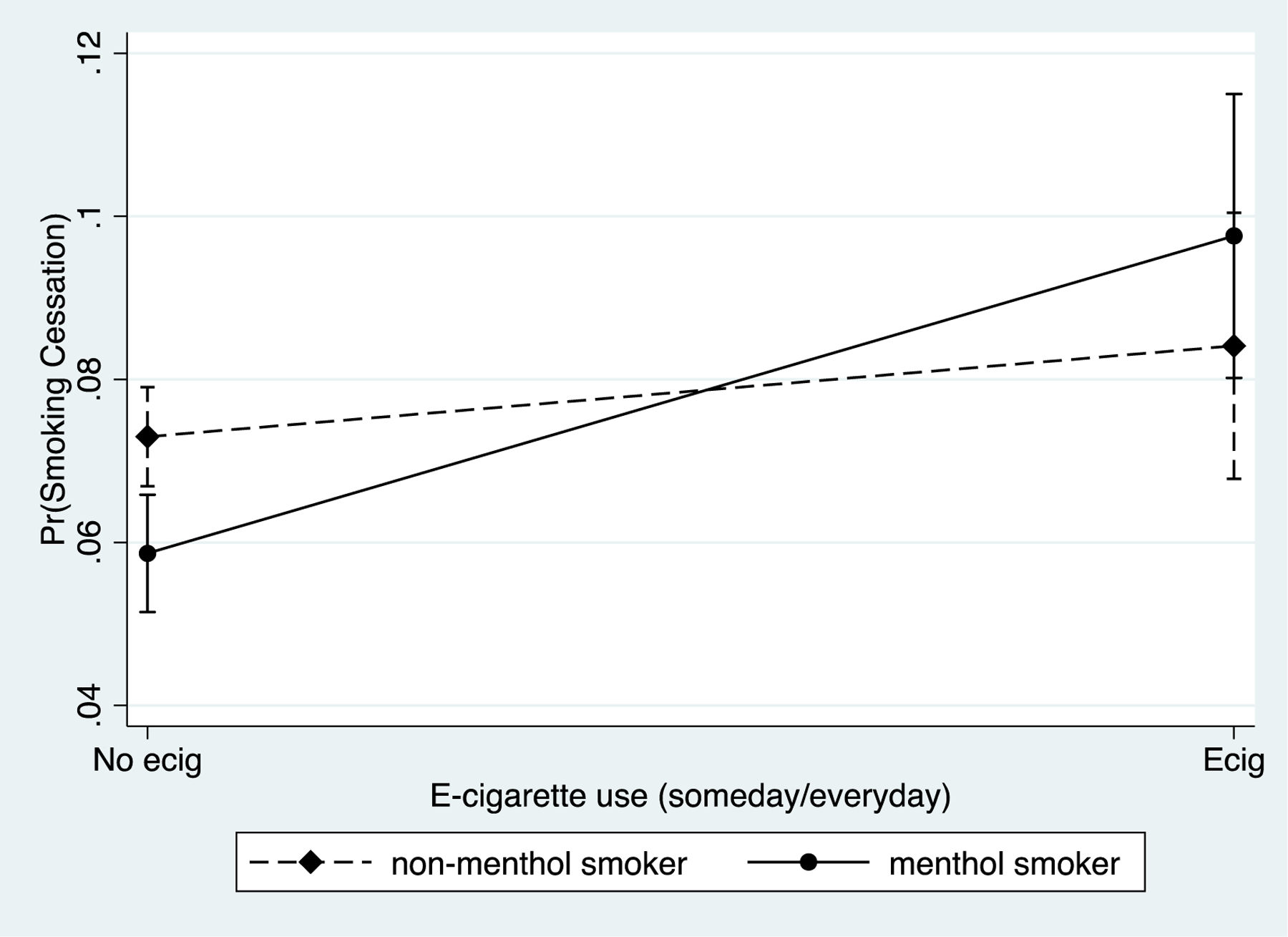
Predicted Probability of Smoking Cessation for Menthol and Non-Menthol Smokers by E-cigarette use
As a sensitivity analysis, the multivariable discrete-time models were estimated using the longitudinal cohort with the ‘all waves’ weights,’ which resulted in a reduced sample size because participation was required for all four waves (see Table A2, Appendix). The substantive results were nearly identical compared to the models estimated with Wave 1 weights with one notable exception. In the longitudinal cohort sample, the odds of smoking cessation for menthol smokers were slightly lower after controlling for sociodemographic factors (Model 2; AOR=0.82, 95% CI: 0.70,0.95) and tobacco dependence and e-cigarette use (Model 3; AOR=0.81, 95% CI: 0.69,0.94) compared to the model using Wave 1 weights. The results for the menthol by race/ethnicity interaction and menthol by e-cigarette interaction were nearly identical regardless of the analytic sample. As a secondary sensitivity analysis, discrete time-models were estimated with all adult respondents aged 18 or older at baseline (see Table A3, Appendix). While the main effect of menthol cigarette use on smoking cessation was a bit more conservative (AOR=0.88, p<0.05 vs AOR=0.92, p>0.05), the substantive interpretation of the interaction effects remained unchanged. The predicted probability of smoking cessation was lower for NH Black and NH Other respondents and the predicted probability of smoking cessation was more pronounced for menthol than for non-menthol smokers.
DISCUSSION
This study examined the longitudinal relationship between menthol cigarette flavoring and smoking cessation among a representative sample of US adults who smoke. We found that menthol smokers had lower odds of smoking cessation relative to non-menthol smokers, but the strength of this relationship was reduced when sociodemographic and tobacco-related controls were included in multivariable models. Moreover, we identified low odds of smoking cessation among NH Black and NH Other smokers, annual household income (less than $50,000), and education (high school or less). These findings remained after controlling for tobacco dependence and verify the important role those sociodemographic characteristics play in smoking cessation using nationally representative longitudinal data.
Previous research has demonstrated a considerable amount of heterogeneity in the menthol–cessation relationship,17 and we found that this relationship was modified by race/ethnicity. NH Black and NH Other menthol smokers had lower odds of quitting smoking than NH White or Hispanic menthol smokers, relative to non-menthol smokers in their respective racial/ethnic groups. These findings are consistent with other studies of racial/ethnic differences in smoking cessation for menthol smokers8,17,40 and provide further evidence that the impact of menthol cigarette use on cessation varies across racial/ethnic groups.17 Longitudinal analyses that adjust for race/ethnicity without testing for effect modification may conceal potentially important racial/ethnic disparities,18 and the findings from our study reaffirm the need to carefully test for these disparities. While it is expected that a menthol cigarette ban will generally reduce the prevalence of cigarette use for menthol smokers,41 the impact of a menthol ban may be strongest among NH Black smokers, which may improve cessation for this group. In addition, our findings highlight the continued need for identifying culturally-specific cessation programs that incorporate ethnocultural factors42 to help facilitate cessation across all groups and ameliorate racial/ethnic disparities in cessation.
We also found that current e-cigarette use was associated with a higher odds of smoking cessation among both menthol and non-menthol adult smokers. These findings are consistent with research showing that many smokers use e-cigarettes as an aid to help them quit smoking,22–24 at least in the short-term.43 However, a key finding in our study was that the association between e-cigarette use and smoking cessation was stronger for menthol smokers than for non-menthol smokers, even after adjusting for racial/ethnic and other determinants of menthol smoking. We also examined this association using a measure of regular e-cigarette use (10+ days used in the past 30 days) as a sensitivity analysis and we obtained similar results for the effect modification. These results suggest that e-cigarettes may be an especially important cessation aid for menthol smokers who want to quit smoking. E-cigarettes may be an alternative product for menthol smokers, and their availability to current smokers may help to reduce the public health harms associated with tobacco use. Furthermore, a menthol ban may be particularly effective in reducing smoking among menthol smokers, especially if mint and menthol flavored e-cigarettes are available as an option for menthol smokers affected by such a ban. Further research is needed to substantiate these findings as more recent data on transitions between products and patterns of dual and exclusive use becomes available.
The findings from this study are not without limitation, and several caveats are important to note when interpreting the results. First, our study examined short-term smoking cessation, and we did not examine longer term smoking cessation or relapse. While recent longitudinal research did not identify differences in smoking relapse for former menthol and non-menthol smokers,19 future research would benefit from examining disparities in both smoking relapse and smoking cessation for menthol smokers. Future research would also benefit from incorporating longer-term measures of smoking cessation. Second, while we identified racial/ethnic disparities in cessation for menthol smokers, small sample sizes prevented us from disentangling differences within the NH Other group 44 which includes NH American Indian/Alaskan Native, Asian, Native Hawaiian/Pacific Islander, and multiracial individuals. Future research, with bigger sample sizes, is needed to disaggregate the NH Other group to understand its racial/ethnic heterogeneity in smoking cessation among menthol smokers. Third, our measure of e-cigarette use was a dichotomous predictor based on past 30-day use and did not capture heterogeneity in frequency of e-cigarette use, which may also impact the likelihood of smoking cessation.25 However, we accounted for time-varying use, which is important as e-cigarette use has been shown to be transient.45 While the data in this study were collected at a time when rates of e-cigarette use were beginning to rise (2013–2017)46, the data are largely prior to the widespread use of pod-based devices; the prevalence of e-cigarette use has continued to increase among adult smokers, especially among those trying to quit smoking.47 More recent longitudinal data is needed to better understand how the frequency of e-cigarette use is associated with smoking cessation for menthol smokers in this rapidly evolving marketplace. Future research would also benefit from assessing the impact of frequency and intensity of e-cigarette use on smoking cessation outcomes. Finally, all longitudinal studies carry a risk that attrition is selective rather than random, and survival analysis techniques assume that right censoring is non-informative. We included a sensitivity analysis using the sample of respondents who participated at all waves because the ‘all-waves weights’ adjust for respondent non-response. While the results were nearly identical, giving us confidence that there were not any systematic non-response biasing our results, it remains possible that they still may be unaccounted for selection bias due to non-random attrition.
Conclusions
Using nationally representative longitudinal data among adult smokers in the US, we found that smoking cessation varied across racial/ethnic groups and by e-cigarette use status. These results contribute to the existing literature on the role of menthol on smoking cessation among adult smokers in two ways. First, the results provide longitudinal evidence that a menthol smoking ban may have a favorable impact on smoking cessation for NH Black and NH Other racial/ethnic groups. These results also point to the need for culturally specific public health strategies to help menthol smokers quit smoking. Second, the results from this study suggest that menthol smokers who use e-cigarettes are more likely to quit smoking. This finding suggests that a menthol smoking ban may be more effective if menthol smokers have access to e-cigarettes as a way to quit cigarette use or as a way to transition to exclusive e-cigarette use.
Highlights.
We found disparities in smoking cessation among adults who smoke menthol cigarettes
Non-Hispanic Black menthol smokers had low odds of smoking cessation
Smoking cessation was higher for menthol smokers who used e-cigarettes
Disclosure of Funding
Support for this study was provided by grant U54CA229974 from the National Institutes of Health, National Cancer Institute and Food and Drug Administration (FDA).
All authors provided feedback and helped shape the research, analysis and manuscript.
Appendix
Table A1.
Discrete time Models Predicting Smoking Cessation with Regular E-Cigarette Use (10 + Days Per Month), PATH Adult (25+) W1-W4
| Model 1a | Model 2b | Model 3c | Model 4d | |||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| AOR | 95% CI | AOR | 95% CI | AOR | 95% CI | AOR | 95% CI | |
| Period 1 | 0.10*** | [.09–.11] | 0.08*** | [.07–.10] | 0.07*** | [.06–.08] | 0.07*** | [.06–.08] |
| Period 2 | 0.09*** | [.08–.10] | 0.07*** | [.06–.09] | 0.06*** | [.05–.07] | 0.06*** | [.05–.07] |
| Period 3 | 0.08*** | [.07–.09] | 0.07*** | [.05–.08] | 0.06*** | [.05–.07] | 0.06*** | [.05–.07] |
| Menthol cig use TVC | 0.83** | [.73–.94] | 0.89 | [.78–1.02] | 0.86* | [.76–.99] | 0.87 | [.72–1.05] |
| Age group | ||||||||
| 25–34 | REF | REF | REF | REF | REF | REF | ||
| 35–54 | 0.69*** | [.61–.80] | 0.78*** | [.68–.91] | 0.79*** | [.68–.91] | ||
| 55+ | 0.88 | [.75–1.03] | 1 | [.85–1.18] | 1 | [.85–1.19] | ||
| Sex (male=1) | 1.1 | [.97–1.24] | 1.03 | [.92–1.16] | 1.03 | [.92–1.17] | ||
| Race/Ethnicity | ||||||||
| Hispanic | 1.46*** | [1.22–1.74] | 1.27* | [1.06–1.52] | 1.23 | [.98–1.54] | ||
| NH White | REF | REF | REF | REF | REF | REF | ||
| NH Black | 0.77* | [.61–.99] | 0.76* | [.59–.97] | 0.98 | [.65–1.48] | ||
| NH Other | 1.05 | [.83–1.34] | 1.03 | [.92–1.16] | 1.28 | [.96–1.69] | ||
| Education | ||||||||
| High School or less | REF | REF | REF | REF | REF | REF | ||
| Some college | 1.41*** | [1.22–1.63] | 1.33*** | [1.14–1.54] | 1.33*** | [1.15–1.54] | ||
| College or more | 1.95*** | [1.63–2.32] | 1.62*** | [1.36–1.92] | 1.61*** | [1.36–1.91] | ||
| Household Income | ||||||||
| <$49,999 | REF | REF | REF | REF | REF | REF | ||
| 50,000 > | 1.35*** | [1.19–1.53] | 1.27*** | [1.12–1.44] | 1.27*** | [1.12–1.42] | ||
| Tobacco Dependence | 0.62*** | [.58–.68] | 0.62*** | [.58–.67] | ||||
| E-cigarette use (10+ days) | 3.40*** | [2.86–4.05] | 2.90*** | [2.33–3.61] | ||||
| Menthol*e-cig Interaction | 1.59** | [1.14–2.22] | ||||||
| Menthol*race/ethnicity | ||||||||
| Hispanic | 1.04 | [.71–1.45] | ||||||
| NH White | REF | REF | ||||||
| NH Black | 0.65* | [.41–.98] | ||||||
| NH Other | 0.45* | [.23–.86] | ||||||
Notes: Person N =7423; Risk Period N= 18,897
p<0.05
p<0.01
p<0.001
Tobacco use exposure
sociodemographic variables added
tobacco dependence added
interaction model
Table A2.
Discrete Time Models Predicting Smoking Cessation on Longitudinal Cohort (‘all waves weights’), Path Adult (25+) W1-W4
| Model 1a | Model 2b | Model 3c | Model 4d | |||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Variable | AOR | 95% CI | AOR | 95% CI | AOR | 95% CI | AOR | 95% CI |
| Period 1 | 0.10*** | [.09–.11] | 0.09*** | [.07–.10] | 0.08*** | [.06–.09] | 0.08*** | [.06–.09] |
| Period 2 | 0.09*** | [.08–.10] | 0.08*** | [.06–.09] | 0.07*** | [.06–.09] | 0.07*** | [.06–.09] |
| Period 3 | 0.08*** | [.07–.09] | 0.07*** | [.05–.08] | 0.06*** | [.05–.08] | 0.06*** | [.05–.08] |
| Menthol cig use TVC | 0.78** | [.68–.89] | 0.82** | [.70–.95] | 0.81** | [.69–.94] | 0.84 | [.73–1.07] |
| Age group | ||||||||
| 25–34 | REF | REF | REF | REF | REF | REF | ||
| 35–54 | 0.64*** | [.55–.74] | 0.70*** | [.60–.81] | 0.7*** | [.61–.82] | ||
| 55+ | 0.82* | [.69–.98] | 0.89 | [.74–1.07] | 0.9 | [.74–1.08] | ||
| Sex (male=1) | 1.07 | [.94–1.23] | 1.03 | [.90–1.18] | 1.04 | [.91–1.19] | ||
| Race/Ethnicity | ||||||||
| Hispanic | 1.43*** | [1.18–1.74] | 1.18 | [.97–1.45] | 1.21 | [.95–1.55] | ||
| NH White | REF | REF | REF | REF | REF | REF | ||
| NH Black | 0.79 | [.60–1.02] | 0.73* | [.56–.95] | 1.04 | [.67–1.62] | ||
| NH Other | 1.15 | [.87–1.51] | 1.11 | [.83–1.47] | 1.38* | [.99–1.92] | ||
| Education | ||||||||
| High School or less | REF | REF | REF | REF | REF | REF | ||
| Some college | 1.45*** | [1.23–1.72] | 1.40*** | [1.19–1.65] | 1.41*** | [1.16–1.66] | ||
| College or more | 1.94*** | [1.61–2.34] | 1.60*** | [1.33–1.94] | 1.59*** | [1.31–1.92] | ||
| Household Income | ||||||||
| <$49,999 | REF | REF | REF | REF | REF | REF | ||
| 50,000 > | 1.36*** | [1.17–1.58] | 1.29*** | [1.11–1.50] | 1.28** | [1.12–1.49] | ||
| Tobacco Dependence | 0.65*** | [.60–.71] | 0.65*** | [.60–.71] | ||||
| E-cigarette use (every/some days) | 1.47*** | [1.20–1.79] | 1.27 | [.99–1.65] | ||||
| Menthol*e-cig Interaction | 1.49* | [1.10–2.02] | ||||||
| Menthol*race/ethnicity | ||||||||
| Hispanic | 0.91 | [.61–1.36] | ||||||
| NH White | REF | REF | ||||||
| NH Black | .57* | [.34–.97] | ||||||
| NH Other | 0.37** | [.17–.77] | ||||||
Notes: Person N =5741; Risk Period N=15,869
p<0.05
p<0.01
p<0.001
Tobacco use exposure
sociodemographic variables added
tobacco dependence added
interaction model
Table A3.
Discrete Time Survival Analysis Predicting Smoking Cessation Among Adult Respondents (18+), PATH W1-W4
| Model 1a | Model 2b | Model 3c | Model 4d | |||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Variable | AOR | 95% CI | AOR | 95% CI | AOR | 95% CI | AOR | 95% CI |
| Period 1 | 0.11*** | [.10–.12] | 0.10*** | [.09–.12] | 0.09*** | [.08–.11] | 0.09*** | [.08–.10] |
| Period 2 | 0.09*** | [.08–.10] | 0.09*** | [.07–.10] | 0.08*** | [.07–.10] | 0.08*** | [.07–.09] |
| Period 3 | 0.08*** | [.07–.09] | 0.08*** | [.07–.10] | 0.08** | [.06–.09] | 0.07*** | [.06–.09] |
| Menthol cig use TVC | 0.89* | [.80,1. 00] | 0.93 | [.82–1.04] | 0.92 | [.81–1.03] | 0.93 | [.80–1.09] |
| Age group | ||||||||
| 18–24 | REF | REF | REF | REF | REF | REF | ||
| 25–34 | 0.80** | [.69–.94] | 0.88 | [.75–1.03] | 0.88 | [.76–1.03] | ||
| 35–54 | 0.56*** | [.49–.65] | 0.66*** | [.58–.76] | 0.67*** | [.59–.78] | ||
| 55+ | 0.71*** | [.60–.84] | 0.83* | [.70–.98] | 0.84* | [.71–.99] | ||
| Sex (male=1) | 1.08 | [.97–1.20] | 1.02 | [.92–1.14] | 1.03 | [.92–1.15] | ||
| Household Income | ||||||||
| <$49,999 | REF | REF | REF | REF | REF | REF | ||
| 50,000 > | 1.30*** | [1.17–1.46] | 1.24*** | [1.11–1.39] | 1.24** | [1.11–1.39] | ||
| Race/Ethnicity | ||||||||
| Hispanic | 1.44** | [1.24–1.68] | 1.19* | [1.02–1.40] | 1.18 | [.96–1.46] | ||
| NH White | REF | REF | REF | REF | REF | REF | ||
| NH Black | 0.79* | [.64–.98] | 0.72** | [.58–.90] | 1 | [.68–1.46] | ||
| NH Other | 0.95 | [.76–1.18] | 0.91 | [.72–1.14] | 1.09 | [.85–1.41] | ||
| Education | ||||||||
| High School or less | REF | REF | REF | REF | REF | REF | ||
| Some College | 1.49*** | [1.32–1.68] | 1.42*** | [1.26–1.61] | 1.43*** | [.1.26–1.61] | ||
| College or more | 2.05*** | [1.74–2.41] | 1.70*** | [1.44–2.00] | 1.69*** | [1.43–1.98] | ||
| Tobacco Dependence | 0.65*** | [.61–.70] | 0.65*** | [.61–.70] | ||||
| E-cigarette use (every/some days) | 1.23** | [1.08–1.41] | 1.09 | [.9–1.32] | ||||
| Menthol*e-cig Interaction | 1.39* | [1.06–1.82] | ||||||
| Menthol*race/ethnicity | ||||||||
| Hispanic | 1 | [.74–1.36] | ||||||
| NH White | REF | REF | ||||||
| NH Black | 0.62* | [.42–.91] | ||||||
| NH Other | 0.53* | [.32–.88] | ||||||
Notes: Person N =9,468 ; Risk Person N =23,890
p,0.05
p<0.01
p<0.001
Tobacco use exposure
sociodemographic variables added
tobacco dependence added
interaction model
Figure A1.
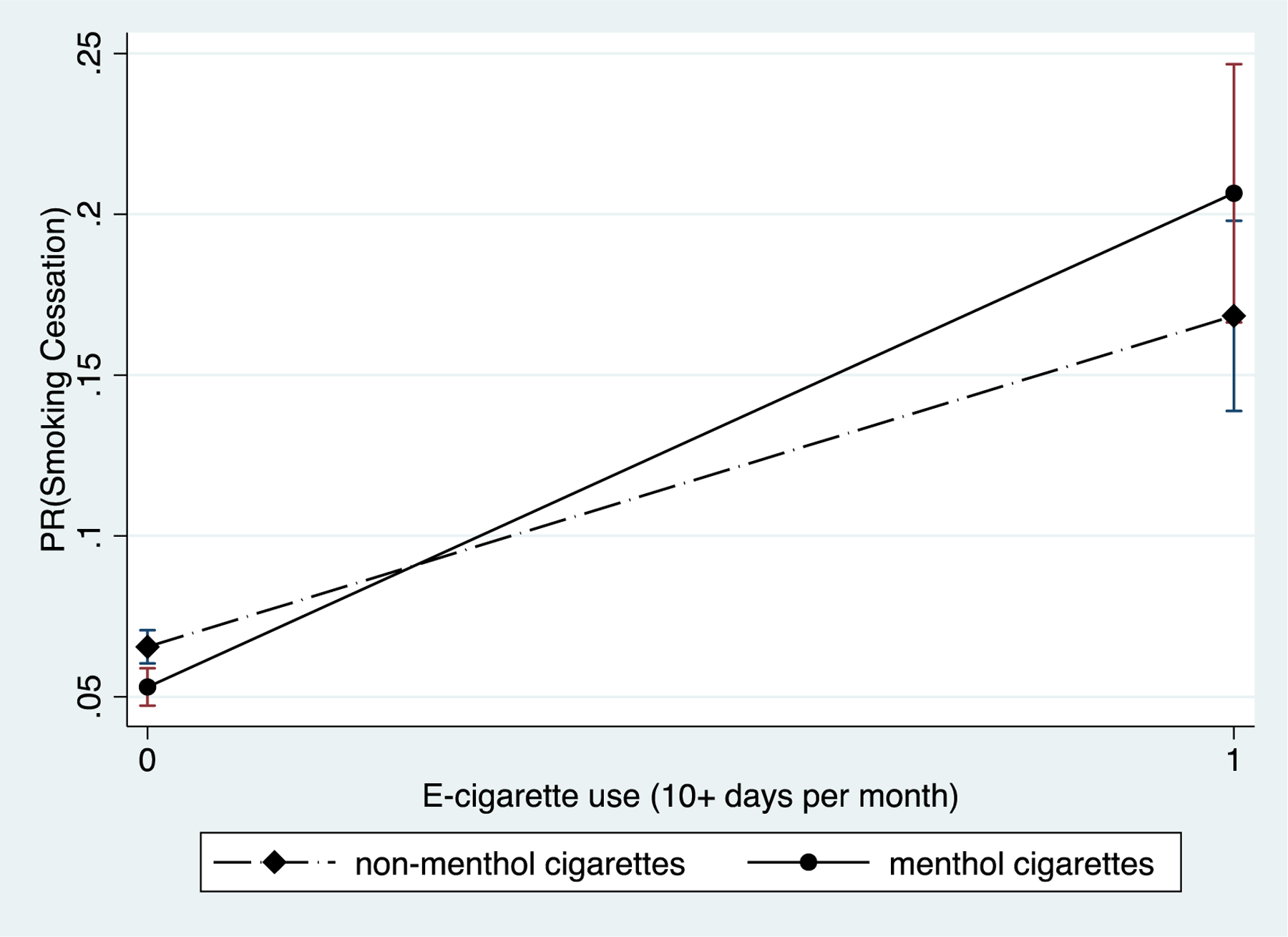
Predicted Probability of Smoking Cessation for Menthol and Non-Menthol Smokers by Regular E-cigarette Use (10+ Days Per Month)
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflicts of Interest
The authors declare that they have no known or competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Declaration of interests
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.Carter BD, Abnet CC, Feskanich D, et al. Smoking and mortality—beyond established causes. New England journal of medicine. 2015;372(7):631–640. [DOI] [PubMed] [Google Scholar]
- 2.Schroth KR, Villanti AC, Kurti M, Delnevo CD. Why an FDA ban on menthol is likely to survive a tobacco industry lawsuit. Public Health Reports. 2019;134(3):300–306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Villanti AC, Mowery PD, Delnevo CD, Niaura RS, Abrams DB, Giovino GA. Changes in the prevalence and correlates of menthol cigarette use in the USA, 2004–2014. Tobacco control. 2016;25(Suppl 2):ii14–ii20. [DOI] [PubMed] [Google Scholar]
- 4.Delnevo CD, Giovenco DP, Villanti AC. Assessment of Menthol and Nonmenthol Cigarette Consumption in the US, 2000 to 2018. JAMA Network Open. 2020;3(8):e2013601–e2013601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Food, Administration D. Preliminary scientific evaluation of the possible public health effects of menthol versus nonmenthol cigarettes. Food and Drug Administration. 2013. [Google Scholar]
- 6.Fu SS, Okuyemi KS, Partin MR, et al. Menthol cigarettes and smoking cessation during an aided quit attempt. Nicotine & Tobacco Research. 2008;10(3):457–462. [DOI] [PubMed] [Google Scholar]
- 7.Keeler C, Max W, Yerger V, Yao T, Ong MK, Sung H-Y. The association of menthol cigarette use with quit attempts, successful cessation, and intention to quit across racial/ethnic groups in the United States. Nicotine & Tobacco Research. 2017;19(12):1450–1464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Delnevo CD, Gundersen DA, Hrywna M, Echeverria SE, Steinberg MB. Smoking-cessation prevalence among US smokers of menthol versus non-menthol cigarettes. American journal of preventive medicine. 2011;41(4):357–365. [DOI] [PubMed] [Google Scholar]
- 9.Foulds J, Hooper MW, Pletcher MJ, Okuyemi KS. Do smokers of menthol cigarettes find it harder to quit smoking? Nicotine & Tobacco Research. 2010;12(suppl_2):S102–S109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hoffman AC, Miceli D. Menthol cigarettes and smoking cessation behavior. Tobacco induced diseases. 2011;9(S1):S6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Villanti AC, Collins LK, Niaura RS, Gagosian SY, Abrams DB. Menthol cigarettes and the public health standard: a systematic review. BMC Public Health. 2017;17(1):983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Foulds J, Gandhi KK, Steinberg MB, et al. Factors associated with quitting smoking at a tobacco dependence treatment clinic. American Journal of Health Behavior. 2006;30(4):400–412. [DOI] [PubMed] [Google Scholar]
- 13.Jao NC, Veluz-Wilkins AK, Smith MJ, et al. Does menthol cigarette use moderate the effect of nicotine metabolism on short-term smoking cessation? Experimental and clinical psychopharmacology. 2017;25(3):216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Smith SS, Fiore MC, Baker TB. Smoking cessation in smokers who smoke menthol and non‐menthol cigarettes. Addiction. 2014;109(12):2107–2117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gandhi K, Foulds J, Steinberg M, Lu SE, Williams J. Lower quit rates among African American and Latino menthol cigarette smokers at a tobacco treatment clinic. International journal of clinical practice. 2009;63(3):360–367. [DOI] [PubMed] [Google Scholar]
- 16.Stahre M, Okuyemi KS, Joseph AM, Fu SS. Racial/ethnic differences in menthol cigarette smoking, population quit ratios and utilization of evidence‐based tobacco cessation treatments. Addiction. 2010;105:75–83. [DOI] [PubMed] [Google Scholar]
- 17.Smith PH, Assefa B, Kainth S, Salas-Ramirez KY, McKee SA, Giovino GA. Use of mentholated cigarettes and likelihood of smoking cessation in the United States: a meta-analysis. Nicotine and Tobacco Research. 2020;22(3):307–316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Schneller LM, Bansal-Travers M, Mahoney MC, McCann SE, O’Connor RJ. Menthol Cigarettes and Smoking Cessation among Adult Smokers in the US. American Journal of Health Behavior. 2020;44(2):252–256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mills SD, Hao Y, Ribisl KM, Wiesen CA, Hassmiller Lich K. The Relationship between Menthol Cigarette Use, Smoking Cessation and Relapse: Findings from Waves 1 to 4 of the Population Assessment of Tobacco and Health Study. Nicotine & Tobacco Research. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Brose LS, Hitchman SC, Brown J, West R, McNeill A. Is the use of electronic cigarettes while smoking associated with smoking cessation attempts, cessation and reduced cigarette consumption? A survey with a 1‐year follow‐up. Addiction. 2015;110(7):1160–1168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kalkhoran S, Glantz SA. E-cigarettes and smoking cessation in real-world and clinical settings: a systematic review and meta-analysis. The Lancet Respiratory Medicine. 2016;4(2):116–128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Biener L, Hargraves JL. A longitudinal study of electronic cigarette use among a population-based sample of adult smokers: association with smoking cessation and motivation to quit. Nicotine & Tobacco Research. 2015;17(2):127–133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Levy DT, Yuan Z, Luo Y, Abrams DB. The relationship of e-cigarette use to cigarette quit attempts and cessation: insights from a large, nationally representative US survey. Nicotine and Tobacco Research. 2018;20(8):931–939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zhu S-H, Zhuang Y-L, Wong S, Cummins SE, Tedeschi GJ. E-cigarette use and associated changes in population smoking cessation: evidence from US current population surveys. bmj. 2017;358:j3262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zhuang Y-L, Cummins SE, Sun JY, Zhu S-H. Long-term e-cigarette use and smoking cessation: a longitudinal study with US population. Tobacco control. 2016;25(Suppl 1):i90–i95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hooper MW, Smiley SL. Comparison of e-cigarette use among menthol and non-menthol smokers: Findings from a community based sample. Ethnicity & disease. 2018;28(3):153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Buckell J, Marti J, Sindelar JL. Should flavours be banned in cigarettes and e-cigarettes? Evidence on adult smokers and recent quitters from a discrete choice experiment. Tobacco Control. 2019;28(2):168–175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rostron BL, Chang JT, Chang CM, Jackson RA, Ambrose BK. ENDS Flavor Preference by Menthol Cigarette Smoking Status among US Adults, 2018–2019. International Journal of Environmental Research and Public Health. 2021;18(1):240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Berg CJ, Haardoerfer R, Escoffery C, Zheng P, Kegler M. Cigarette users’ interest in using or switching to electronic nicotine delivery systems for smokeless tobacco for harm reduction, cessation, or novelty: a cross-sectional survey of US adults. Nicotine & Tobacco Research. 2015;17(2):245–255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Patel D, Davis KC, Cox S, et al. Reasons for current E-cigarette use among US adults. Preventive medicine. 2016;93:14–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hyland A, Ambrose BK, Conway KP, et al. Design and methods of the Population Assessment of Tobacco and Health (PATH) Study. Tobacco control. 2017;26(4):371–378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Giovino GA, Villanti AC, Mowery PD, et al. Differential trends in cigarette smoking in the USA: is menthol slowing progress? Tobacco control. 2015;24(1):28–37. [DOI] [PubMed] [Google Scholar]
- 33.Blot WJ, Cohen SS, Aldrich M, McLaughlin JK, Hargreaves MK, Signorello LB. Lung cancer risk among smokers of menthol cigarettes. Journal of the National Cancer Institute. 2011;103(10):810–816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Strong DR, Pearson J, Ehlke S, et al. Indicators of dependence for different types of tobacco product users: Descriptive findings from Wave 1 (2013–2014) of the Population Assessment of Tobacco and Health (PATH) study. Drug and alcohol dependence. 2017;178:257–266. [DOI] [PubMed] [Google Scholar]
- 35.Singer JD, Willett JB, Willett JB. Applied longitudinal data analysis: Modeling change and event occurrence. Oxford university press; 2003. [Google Scholar]
- 36.Jenkins SP. Introduction to the analysis of spell duration data. ISER, University of Essex. 2004. [Google Scholar]
- 37.Dow WH, Norton EC, Donahoe JT. Stata tip 134: Multiplicative and marginal interaction effects in nonlinear models. The Stata Journal. 2019;19(4):1015–1020. [Google Scholar]
- 38.Piesse A, Opsomer J, Dohrmann S, et al. Longitudinal Uses of the Population Assessment of Tobacco and Health Study. Tobacco Regulatory Science. 2021;7(1):3–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Judkins DR. Fay’s method for variance estimation. Journal of Official Statistics. 1990;6(3):223–239. [Google Scholar]
- 40.Kulak JA, Cornelius ME, Fong GT, Giovino GA. Differences in quit attempts and cigarette smoking abstinence between whites and African Americans in the United States: literature review and results from the International Tobacco Control US Survey. Nicotine & Tobacco Research. 2016;18(suppl_1):S79–S87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Cadham CJ, Sanchez-Romero LM, Fleischer NL, et al. The actual and anticipated effects of a menthol cigarette ban: a scoping review. BMC Public Health. 2020;20(1):1–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Webb Hooper M, Antoni MH, Okuyemi K, Dietz NA, Resnicow K. Randomized controlled trial of group-based culturally specific cognitive behavioral therapy among African American smokers. Nicotine & Tobacco Research. 2017;19(3):333–341. [DOI] [PubMed] [Google Scholar]
- 43.Everard CD, Silveira ML, Kimmel HL, Marshall D, Blanco C, Compton WM. Association of Electronic Nicotine Delivery System Use With Cigarette Smoking Relapse Among Former Smokers in the United States. JAMA Network Open. 2020;3(6):e204813–e204813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Mattingly DT, Hirschtick JL, Fleischer NL. Unpacking the Non-Hispanic Other Category: Differences in Patterns of Tobacco Product Use Among Youth and Adults in the United States, 2009–2018. Journal of immigrant and minority health. 2020:1–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Brouwer AF, Jeon J, Hirschtick JL, et al. Transitions between cigarette, ENDS and dual use in adults in the PATH study (waves 1–4): multistate transition modelling accounting for complex survey design. Tobacco control. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Bandi P, Cahn Z, Sauer AG, et al. Trends in E-Cigarette Use by Age Group and Combustible Cigarette Smoking Histories, US Adults, 2014–2018. American Journal of Preventive Medicine. 2020. [DOI] [PubMed] [Google Scholar]
- 47.Mayer M, Reyes-Guzman C, Grana R, Choi K, Freedman ND. Demographic Characteristics, Cigarette Smoking, and e-Cigarette Use Among US Adults. JAMA Network Open. 2020;3(10):e2020694–e2020694. [DOI] [PMC free article] [PubMed] [Google Scholar]


