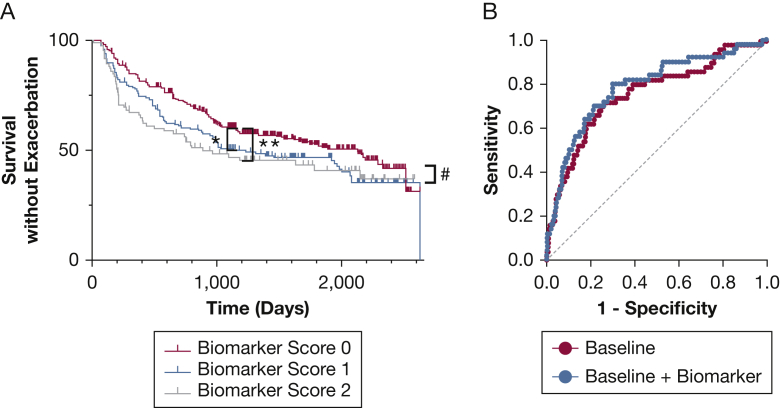
Figure 4.
A, B, Predictive ability of biomarkers. A, Time to exacerbation based on biomarker score reflecting elevated sialic acid or hypoxanthine levels, or both in patients with COPD (n = 562). In the full data set, exacerbations occurred sooner in those with a biomarker score of 2 relative to those with a biomarker score of 0 (P = .02 for the model by log-rank Mantel-Cox test, with P = .02 by log-rank after test after Tukey-Kramer adjustment). Analyses also were performed with data censored at 3 years to assess shorter-term predictions, and in this model, both biomarker scores 1 and 2 were predictive of time to exacerbation (P = .008 for model, P = .027 for score 1, and P = .002 for score 2 in after test). ∗P < .05 and ∗∗P < .01 by after test for model censored at 3 years, and #P < .05 by after test for full model. B, Receiver operating characteristic (ROC) curves from logistic regression to predict those with multiple future exacerbations. The baseline model (red) used prior number of exacerbations, percent predicted FEV1, age, and sex as variables (area under the ROC curve [AUC], 0.758; 95% CI, 0.683-0.834; P < .001). The baseline plus biomarker model (blue) adding a biomarker score showed modest but significant improvement (AUC, 0.785; 95% CI, 0.713-0.857; P < .001; P = .0059 vs baseline model by likelihood ratio test). Differences were confirmed using cross-validated AUC analyses (see text).