Key Point
Fondaparinux costs less and confers more benefits than argatroban in patients with suspected heparin-induced thrombocytopenia.
Visual Abstract
Abstract
Heparin-induced thrombocytopenia (HIT) is a life-threatening complication associated with high medical costs. Factor Xa inhibitors gradually replace approved treatment with intravenous direct thrombin inhibitors despite their off-label indication, because of easier management and favorable economic profile. Whether they are cost-effective remains unclear. We evaluated the cost-effectiveness of approved and off-label anticoagulants in patients with suspected HIT, based on census data from the largest Swiss hospital between 2015 and 2018. We constructed a decision tree model that reflects important clinical events associated with HIT. Relevant cost data were obtained from the finance department or estimated based on the Swiss-wide cost tariff. We estimated averted adverse events (AEs) and incremental cost-effectiveness ratio as primary outcome parameters. We performed deterministic and probabilistic sensitivity analyses with 2000 simulations to assess the robustness of our results. In the base-case analysis, the total cost of averting 1 AE was 49 565 Swiss francs (CHF) for argatroban, 30 380 CHF for fondaparinux, and 30 610 CHF for rivaroxaban; after adjusting for 4Ts score: 41 152 CHF (argatroban), 27 710 CHF (fondaparinux), and 37 699 CHF (rivaroxaban). Fondaparinux and rivaroxaban were more clinically effective than argatroban, with AEs averted of 0.820, 0.834, and 0.917 for argatroban, fondaparinux, and rivaroxaban, respectively. Treatment with fondaparinux resulted in less cost and more AEs averted, hence dominating argatroban. Results were most sensitive to AE rates and prolongation of stay. Monte Carlo simulations affirmed our base-case analysis. This is the first cost-effectiveness analysis comparing argatroban with fondaparinux and rivaroxaban using primary data. Fondaparinux and rivaroxaban resulted in more averted AEs, but fondaparinux had greater cost savings. Fondaparinux could be a viable alternative to argatroban.
Introduction
Immune heparin-induced thrombocytopenia (HIT) is a life-threatening condition with an incidence of 0.2 to 5% and 0.3 to 1% in patients exposed for >1 week to unfractionated heparin1-3 and low-molecular-weight heparin,4 respectively. The immune reaction is triggered by complexes of heparin and platelet factor 4 (PF4).1 Antibodies directed against neoepitopes on these complexes activate platelets with the adverse effect of venous and arterial thromboembolic complications and thrombocytopenia due to platelet consumption.
The diagnosis of HIT is made by clinical features in combination with laboratory testing.5,6 4Ts score consists of characteristic clinical and laboratory features and helps to determine pretest probability for underlying HIT: severity of thrombocytopenia, timing of platelet count decrease, thrombosis or other sequelae, and other causes of thrombocytopenia.6,7 Upon HIT suspicion, it is mandatory to switch therapy from heparin to non–heparin-based alternative anticoagulants. Diagnosis is confirmed by a 2-step procedure6: a sensitive immunoassay for presence of anti–PF4-heparin antibodies with high negative predictive value8 and a functional platelet activation assay with a longer turnover of results.5
Approved alternatives to heparin include direct thrombin inhibitors such as argatroban, bivalirudin, or danaparoid9,10 (however, danaparoid is not approved in the United States). These are administered intravenously and require close laboratory monitoring. In addition to these disadvantages, thromboembolic and hemorrhagic complications are common during therapy with thrombin inhibitors.10-12 Therefore, physicians increasingly prescribe off-label subcutaneously or orally administered factor Xa inhibitors, such as fondaparinux (F),13 rivaroxaban (R), or apixaban.14,15 The use of factor Xa inhibitors is not approved in acute or suspected HIT,6,16 however promising treatment results12,15,17-19 encourage physicians to deviate from recommended treatment.20 Further rationale for the use of alternative off-label anticoagulants is their favorable economic profile: these are cheaper and easier to apply and to monitor.21,22 This is particularly useful because HIT and its complications are associated with high medical costs.23-27
Aside from clinical effectiveness, cost-effectiveness of prescribed HIT treatment should be part of the clinical decision-making process. Cost-effectiveness considers direct costs of drugs, hospitalization, complications, additional diagnostics, and health benefits gained. A hypothetical estimation based in the United States suggests a favorable cost-effectiveness profile of fondaparinux compared with argatroban or bivalirudin.28 To our knowledge, there have been no cost-effectiveness analyses of alternative HIT treatments in European countries.
In this study we summarized actual prescription practices upon HIT suspicion in the largest university hospital in Switzerland, adverse event rates per anticoagulation used and estimated costs of drugs and treatment of adverse events. Based on these figures, we calculated incremental cost-effectiveness ratios to determine the cost-effectiveness of the alternative anticoagulants used in treating patients suspected with HIT.
Methods
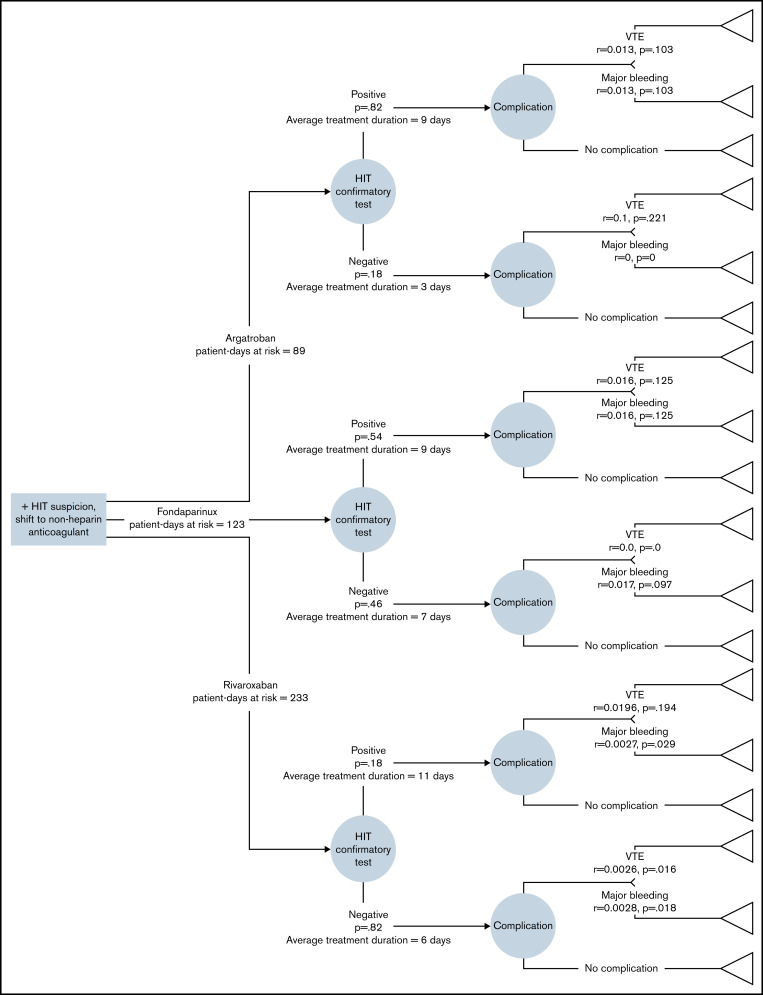
We performed this economic evaluation according to Consolidated Health Economic Evaluation Reporting Standards statement.29 For the cost-effectiveness estimation, we constructed the decision tree model simulating scenarios expected to occur once HIT is suspected (Figure 2). The primary outcomes of interest are adverse events. The primary parameter of interest was incremental cost per adverse event averted. This evaluation uses a Swiss tertiary university hospital perspective. All participants gave consent for the analysis and anonymized data publication. This study was approved by the local ethics committee of the canton Bern (ID: 2018-00426).
Figure 2.
Analytical decision tree model used in this economic evaluation. The decision tree model depicts the most important clinical and cost considerations in patients suspected of having HIT in whom heparins have been suspended. At the decision point, 3 nonheparin anticoagulants were considered: argatroban, fondaparinux, and rivaroxaban. Patients who received any of these medications underwent laboratory HIT diagnostics. Differences in the eventual costs and outcomes (ie, complications or no complications) per drug form the basis of this analysis. All model inputs and their references are explained in the Supplementary Table 1. p, standardized probability of event; r, incidence rate; VTE, venous thromboembolism.
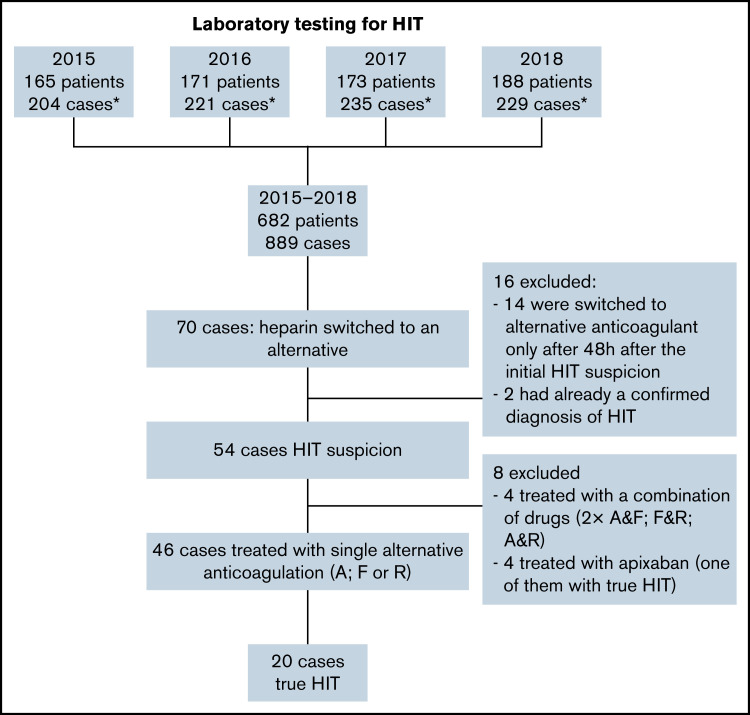
Population
We performed a retrospective analysis of patients having suspected HIT in Bern University Hospital between 2015-2018. Relevant clinical data of all inpatient adults who were tested for presence of HIT antibodies and subsequently switched to a nonheparin anticoagulation within 48 hours were included in this study. Figure 1 illustrates our study sample selection.
Figure 1.
Flowchart of study population. *One case refers to 1 hospital admission; some patients had >1 admission with HIT suspicion in a year. A, argatroban; F, fondaparinux; R, rivaroxaban.
Model structure
We constructed a decision tree model that reflects important clinical events likely to occur once HIT is suspected (Figure 2). All suspected HIT cases were switched from heparin to any of the 3 comparator drugs: A, F, or R. There were no cases of danaparoid or bivalirudin use in our census. Single uses of apixaban and any drug combination were excluded. Patients were treated with alternative anticoagulants until the confirmatory, functional assay results were available. The allocated medicine was then continued or discontinued depending on the result of the test. If HIT was confirmed, those treated with A were subsequently switched to vitamin K antagonists. Those treated with F or R were treated continuously until discharge.
The primary outcomes considered at the end of the decision tree were adverse events such as VTE or major bleeding, and no adverse event scenario. The major bleeding complications observed in the cohort were predominantly upper gastrointestinal bleedings. Thus, we approximated that the costs of managing upper gastrointestinal bleeding equal the costs of managing major bleeding.30 VTE included pulmonary embolism and deep venous thrombosis, and we excluded arterial complications as they are less frequent in HIT patients, also reflected in our cohort.31 Between each treatment arm, the difference in primary outcomes (incremental effectiveness) and the difference in costs (incremental costs) were calculated, and the incremental cost-effectiveness ratio (ICER) was expressed as cost per adverse event averted.
Estimation of probabilities
The probability of HIT confirmed (positive) or excluded (negative) equaled the actual number of confirmed HIT in each medication subgroup divided by total number of patients treated with this medication. To estimate the probability of adverse events, we converted incident rates of adverse events using the formula:
Where:
pi = probability of adverse event i,
r = incidence rate of adverse event i
t = period of interest
In our model, it is assumed that the adverse event incidence rates are constant over a period of time. The incidence rate of adverse events was calculated based on days of exposure with nonheparin anticoagulation as follows: number of events (VTE or major bleeding)/patient-days of exposure to nonheparin anticoagulant.
Estimation of costs
We obtained available in-hospital and Swiss-wide financial data to estimate direct medical costs in Swiss francs (CHF). The costs of the drugs and total and average daily costs of hospitalization were obtained from the financial department of the hospital. Accordingly, the costs associated in each intervention are presented in Table 1.
Table 1.
Costs of drugs and hospitalization in the patients with suspected HIT
| Argatroban (n = 11) | Fondaparinux (n = 13) | Rivaroxaban (n = 22) | |
|---|---|---|---|
| HIT excluded | |||
| Total costs of drugs per patient | 1 884* (628; 2 198) | 43.2 (9.30; 43.2) | 15.4 (6.60; 30.6) |
| Total costs of hospitalization | 92 280 (32 296; 113 844) | 65 507 (44 862; 100 652) | 59 316 (32 309; 126 008) |
| Daily costs of hospitalization | 4 292 (3 797; 6 325) | 3 586 (2 054; 4 874) | 3 106 (2 437; 4 624) |
| HIT confirmed | |||
| Total costs of drugs per patient | 1 884* (942; 2 198) | 43.2 (43.2; 43.4) | 24.2 (15.3; 41.8) |
| Total costs of hospitalization | 102 531 (58 331;114 547) | 103 994 (44 862;171 506) | 111 586 (71 533; 148 504) |
| Daily costs of hospitalization | 4 292 (4 037; 4 564) | 3 657 (2 991; 5 039) | 3 491 (2 840; 4 624) |
Costs are in CHF. We estimated the costs of adverse events using TARMED Tariff.32
Approximates for 1 ampule (250 mg/2.5 mL) of argatroban per day for an 80 kg patient.
One (1) TARMED point in the Swiss-wide billing system for inpatient services, including imaging and laboratory examinations, costs 1 CHF. In our cost calculations, we assumed the costs of managing bleeding complications to be the costs of gastroscopy with procedures for stopping bleeding, costs of 4 laboratory testing for blood count, and associated transfusion of erythrocyte concentrates amounting to 1260 CHF.30 We assumed the costs of managing VTE to be the standardized costs of duplex ultrasound of legs and computerized tomography scan for pulmonary embolism protocol with use of contrast agent and fees for d-dimer measurement, amounting to 1349 CHF.32
In addition to drug costs and costs of treating complications, we also estimated the costs of prolongation of stay of the patients. We assumed that the costs of prolongation of stay depend solely on the number of days of prolongation of stay, which was calculated as a difference between average length of stay for main diagnosis of each patient based on 2019 hospitalization episodes statistics and the actual length of stay in our sample population for this diagnosis using Swiss statistical data, which provides mean and 90% confidence interval of the expected length of hospital stay per case.33 To facilitate calculations, we assume this 90% confidence interval to be the minimum and maximum prolongation of stay in our model.
Calculation of expected values
Expected clinical outcomes and corresponding total costs for each terminal node (triangle node) were calculated by multiplying probabilities arising from each chance node (circle node). The costs of intervention are the sum of costs before HIT confirmation (total costs of drugs and costs of hospital care) and costs after confirmation (costs of hospital care, including treatment of adverse events, if any). We calculated the expected costs associated per terminal node as follows:
Where:
ci = estimated costs of treating adverse event i
pi = probability of adverse event i per terminal node
ph = probability of HIT status
pi|h = probability of adverse event i, given HIT status h
All costs relevant to each intervention arm are added (), resulting in expected costs of each intervention.
Statistical and sensitivity analyses
To account for differences in the likelihood of prescribing on-label drugs based on clinical profile of patients, we adjusted the costs for 4Ts score. We used the same method to adjust for the primary outcome (adverse events averted).
Where:
Ci,a = adjusted total costs associated with treating patients using drug i
Ci,u = unadjusted costs of treating patients using drug i, given a particular t score
p(Di|t) = probability of being prescribed drug Di, given 4Ts score t
Ci,u|l = unadjusted costs of treating patients using drug i, given low 4Ts score
Ci,u|m = unadjusted costs of treating patients using drug i, given moderate 4Ts score
Ci,u|h = unadjusted costs of treating patients using drug i, given high 4Ts score
p(Di|l) = probability of being prescribed drug Di, given low 4Ts score l
p(Di|m) = probability of being prescribed drug Di, given moderate 4Ts score m
p(Di|h) = probability of being prescribed drug Di, given high 4Ts score h
i = (fondaparinux, argatroban, rivaroxaban)
We performed deterministic sensitivity analysis accounting for variations of parameters 1 or few at a time and with absolute certainty. To account for the random distribution of multiple key parameters all at once, we performed probabilistic sensitivity analysis (PSA) with 2 000 simulations utilizing γ distribution for costs, β distribution for clinical probabilities, and normal distribution for outcomes (prolongation of hospital stay). To illustrate decision uncertainty surrounding cost-effectiveness thresholds, we presented the cost-effectiveness acceptability curves of fondaparinux and rivaroxaban vs argatroban in suspected HIT. We performed calculations and Monte Carlo simulations using Microsoft Excel 2016 with Visual Basic for Applications (VBA).
Results
We had a total of 54 patients suspected of having HIT in our institution, which were treated with argatroban in 11 (20%), fondaparinux in 13 (24%), rivaroxaban in 22 (41%), a mix of these drugs in 4 (7%), or with apixaban in 4 (7%) patients. Both monotherapies with A, F, or R and drug combinations were used to calculate the adverse events rates. Monotherapies with A, F, and R were included in the cost estimation and subsequent analyses. Twenty patients (43%) were confirmed of having HIT, whereas 26 (57%) tested negative. Prescription practice varied among patients according to the available 4Ts score (Table 2).
Table 2.
Distribution of treatment allocation according to clinical probability of HIT assessed using 4Ts score in patients with available 4Ts score (43 of 46 patients)
| Clinical probability of HIT | A | F | R |
|---|---|---|---|
| Low 4Ts <4 | 2 | 2 | 8 |
| < medium 4Ts 4-5 | 7 | 7 | 7 |
| High 4Ts >5 | 2 | 4 | 4 |
A total of 445 patient-days at risk were observed in patients with suspected and confirmed HIT. In this period, we observed 3 thromboembolic events and 3 major and 22 minor bleedings. There were no deaths during the treatment of HIT, but we recorded 3 deaths within 3 months after the HIT suspicion.
Patients in whom HIT was ruled out were exposed to nonheparin anticoagulants for 3 to 7 days. If HIT was confirmed, patients were treated with argatroban for 7 to 9 days in total and switched to vitamin K antagonists afterward. Patients treated with fondaparinux or rivaroxaban were treated continuously until discharge, ranging from 9 to 11 days in total.
We calculated the prolongation of stay for each outcome. For all HIT− patients, we assumed the same average prolongation of stay of 2.5 days per each drug given.
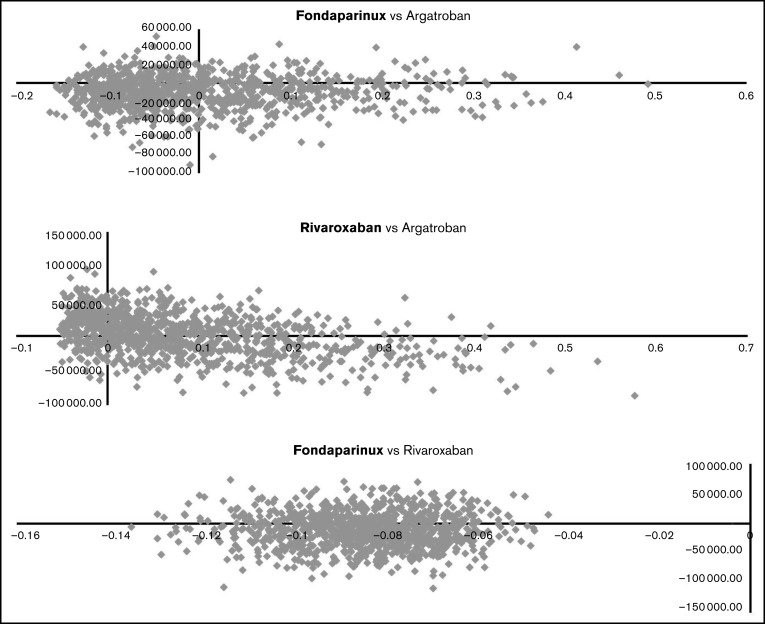
Using our estimates in the base case scenario, the total costs of averting 1 adverse event were 49 565 CHF for A, 30 380 CHF for F, and 30 610 CHF for R, and adverse events averted were 0.791, 0.820, and 0.932 for A, F, and R, respectively. Adjusted for 4Ts scores, the total cost of averting an adverse event amount to 41 152 CHF for A, 27 710 CHF for F, and 37 699 CHF for R. In terms of clinical outcomes, F and R were more effective than A, with adverse events averted of 0.820, 0.834, and 0.917 for A, F, and R, respectively. Hence, F was cheaper than A and R in managing suspected HIT, and F and R were more effective in terms of adverse events averted (Table 3). Adjusting the costs and outcomes for 4Ts scores yielded similar results: fondaparinux was dominant compared with argatroban (ie, lower incremental costs and higher incremental benefits), whereas rivaroxaban was more expensive but conferred more benefits in comparison with argatroban (Table 3).
Table 3.
Base case and adjusted costs and outcomes of 3 comparator drugs used to treat patients suspected of having HIT
| Unadjusted | Adjusted | |||
|---|---|---|---|---|
| Drugs | Total costs | Total benefits (adverse events averted) | Total costs | Total benefits (adverse events averted) |
| Fondaparinux | CHF 24 923 | 0.820 | CHF 23 097 | 0.834 |
| Argatroban | CHF 39 207 | 0.791 | CHF 33 749 | 0.820 |
| Rivaroxaban | CHF 28 542 | 0.932 | CHF 34 585 | 0.917 |
| Incremental costs | Incremental benefits | Incremental costs | Incremental benefits | |
|---|---|---|---|---|
| Fondaparinux vs Argatroban | −CHF 14 284 | 0.029 | −CHF 10 652 | 0.013 |
| Fondaparinux vs Rivaroxaban | −CHF 3 602 | −0.112 | −CHF 11 488 | −0.084 |
| Rivaroxaban vs Argatroban | −CHF 10 682 | 0.141 | CHF 835 | 0.097 |
Deterministic sensitivity analysis
We performed deterministic sensitivity analyses to test the robustness of the cost-effectiveness analysis results. In these analyses, we assumed the following scenarios (Table 4): (1) Base case incidence rates decreased by 50%. (2) Base case incidence rates increased by 50%. (3) Event rates obtained from the study by Al-jabri et al. (2016)28. (4) Event rates obtained from largest published studies on relevant medication and adverse events (Kang et al. (2015),34 ARTEMIS trial,35 Lewis et al. (2006),36 Hursting et al. (2010),37 Warkentin et al. (2017),19 Linkins et al. (2016),15 MAGELLAN trial38). In the supplemental sensitivity analyses in supplemental Table 2, we assumed further: (1) Hospital costs decreased by 50% from base case. (2) Hospital costs increased by 50% from base case. (3) Length of drug exposure is the same as in the study by Aljabri et al. (2016)28 (4) Prolongation of stay decreased by 50% from base case. (5) Prolongation of stay increased by 50% from base case. All these scenarios showed congruent dominance of fondaparinux vs argatroban. The comparison between rivaroxaban and argatroban showed variable results. In most cases, rivaroxaban was more expensive but more effective depending on duration of the hospitalization and on the adverse event incidence rates used in the model. The comparison between fondaparinux vs rivaroxaban consistently showed that fondaparinux was less expensive but less beneficial (Table 4; supplemental Table 2). However, one has to take into account the lower case numbers in our study. When applying incidence rates from the largest published studies, sensitivity analysis showed that fondaparinux dominated rivaroxaban.
Table 4.
Deterministic sensitivity analysis results
| Scenario | Fondaparinux vs Argatroban | Fondaparinux vs Rivaroxaban | Rivaroxaban vs Argatroban |
|---|---|---|---|
| Base case | Dominant | Trade-off* | Trade-off† |
| Incremental Cost (CHF) | −10 653 | −11 488 | 835 |
| Incremental Effectiveness (AEA) | 0.013 | −0.084 | 0.097 |
| ICER (CHF/AEA) | 136 968 | 8 586 | |
| Base case incidence rates − 50% | Dominant | Trade-off* | Dominant |
| Incremental Cost (CHF) | −7 010 | −15 230 | −8 219 |
| Incremental Effectiveness (AEA) | 0.007 | −0.043 | 0.050 |
| ICER (CHF/AEA) | 351 595 | ||
| Base case incidence rates + 50% | Dominant | Trade-off* | Dominant |
| Incremental Cost (CHF) | −14 144 | −7 988 | −6 156 |
| Incremental Effectiveness (AEA) | 0.019 | −0.122 | 0.141 |
| ICER (CHF/AEA) | 65 606 | ||
| Event rates from Al-jabri et al 28 | Dominant | Rivaroxaban was not assessed in the study | |
| Incremental Cost (CHF) | −18 142 | ||
| Incremental Effectiveness (AEA) | 0.061 | ||
| ICER (CHF/AEA) | |||
| Event rates obtained from other published studies (Kang et al. (2015),34 ARTEMIS trial,35 Lewis et al. (2006),36 Hursting et al. (2020),37 Warkentin et al. (2017),19 Linkins et al. (2016),15 MAGELLAN trial38) | Trade-off* | Dominant | Dominated |
| Incremental Cost (CHF) | −881 | −15 963 | 15 081 |
| Incremental Effectiveness (AEA) | −0.042 | 0.029 | −0.071 |
| ICER (CHF/AEA) | 21 107 | ||
Dominant = the first drug (ie, before "vs") costed less and was more effective in preventing adverse events than the comparator.
Dominated = the first drug (ie, before "vs") costed more and was less effective in preventing adverse events than the comparator.
AEA, adverse events averted.
Trade-off indicates “less costly but also less effective”; interpretation of cost-effectiveness depends on threshold: costs of averting 1 adverse event
Trade-off indicates “more costly but also more effective”; interpretation of cost-effectiveness depends on threshold: costs of averting 1 adverse event
Probabilistic sensitivity analysis
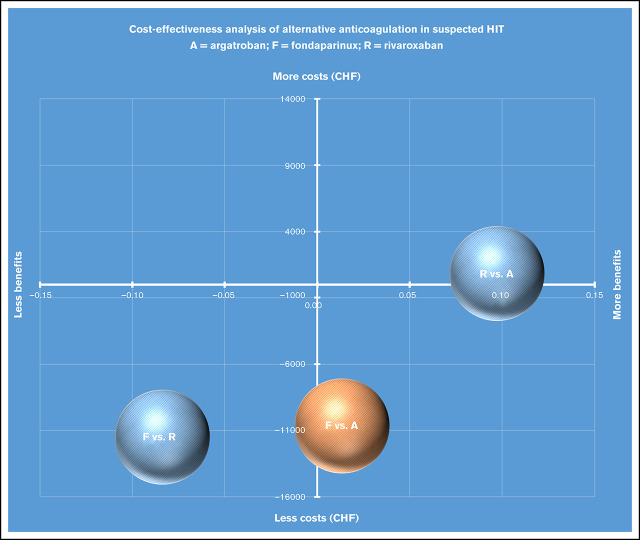
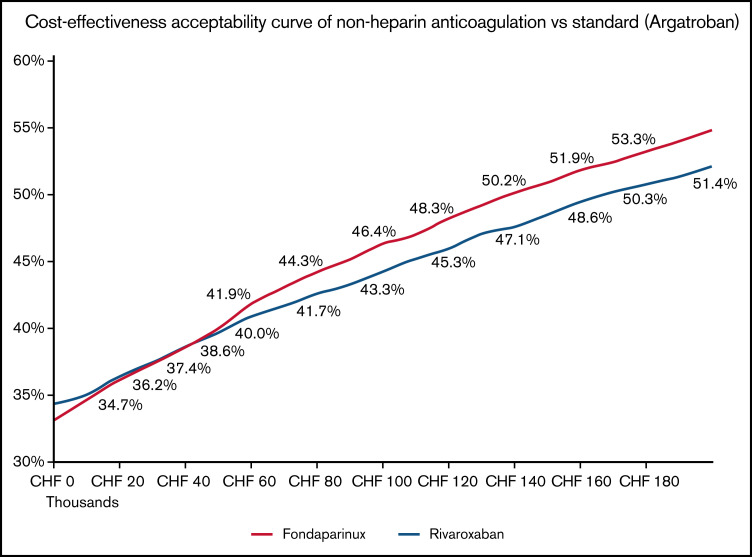
Based on institutional and published data on various parameters and their uncertainty distributions, we performed Monte Carlo simulations using the parameters and their probability distributions as inputs and performed 2000 simulations for each comparison: F vs A, R vs A, and F vs R. PSA results affirm our base-case findings where fondaparinux have high probability of dominating argatroban. (Figure 3).
Figure 3.
Probabilistic sensitivity analyses (2000 Monte Carlo simulations). Each dot in the plot represents the results of 1 Monte Carlo simulation. X-axes represent incremental benefits (adverse events averted), and y-axes represent incremental costs in CHF. Dots on the southeast quadrant means the drug in bold typeface is dominant (ie, less costs and more benefits). Dots on the northwest means the drug in bold typeface is dominated (more costs and less benefits). Dots on either northeast and southwest quadrants mean that trade-offs between costs and benefits of the drugs being compared exist, and dots below the threshold (slope of line from the origin) are considered cost-effective.
There are no established cost-effectiveness thresholds for specific health measures such as adverse events averted. To take this uncertainty into account, we constructed a cost-effectiveness acceptability curve to estimate the probability that an intervention is cost-effective vs a comparator drug, over a wide range of cost-effectiveness thresholds. For example, when assessed against argatroban at a threshold of 100 000 CHF per adverse event averted, the probability that fondaparinux is cost-effective is 46.4% and rivaroxaban 44.3% (Figure 4). Rivaroxaban has higher probability of cost-effectiveness compared with fondaparinux at about <30 000 CHF threshold; at higher threshold (>30 000 CHF), fondaparinux has higher probability of cost-effectiveness than rivaroxaban.
Figure 4.
Cost-effectiveness acceptability curve of fondaparinux and rivaroxaban compared with argatroban.
Discussion
We designed and conducted this study to assess the actual prescribing practices for suspected HIT and to estimate the cost-effectiveness of therapies used at the largest university hospital in Switzerland. We found that physicians prescribe not only approved and guidelines-recommended argatroban for patients with suspected HIT (used only in 20% of patients in our cohort) but also off-label anticoagulants fondaparinux and rivaroxaban. These were predominantly (75%) used in patients with low and moderate risk for HIT based on 4Ts score (ie, 4Ts score <6 points). To our knowledge, this is the first pharmacoeconomic analysis that compared cost-effectiveness of argatroban, fondaparinux, and rivaroxaban in suspected HIT from a tertiary university hospital perspective in Europe. We found that fondaparinux had lower treatment costs and greater benefits in terms of adverse events averted in the base case scenario, hence dominating argatroban. We did not estimate ICER in the primary analysis because of this dominance. Our findings are robust across several deterministic sensitivity analyses and these were confirmed by probabilistic sensitivity analyses. Based on our results, fondaparinux is a viable clinical and economic alternative to approved argatroban by demonstrating 2 benefits: reductions in hospital costs and aversion of more adverse events. In our analysis, rivaroxaban is more expensive than argatroban but confers more benefits, hence its cost-effectiveness depends on the threshold cost for an adverse event averted. Compared with argatroban, the cost of averting 1 extra adverse event averted in using rivaroxaban remains relatively low at 8 586 CHF in the base case scenario. According to our PSA and cost-effectiveness acceptability curve results, the probability of cost-effectiveness for rivaroxaban ranges between 34% and 49.5% in the tested thresholds (0-1 mln CHF) and is close to our findings for fondaparinux. At least from a safety standpoint, rivaroxaban is a more beneficial alternative to argatroban.
The rationale for their use in HIT for (1) fondaparinux, although its antithrombin-binding pentasaccharide sequence is derived from heparin’s natural pentasaccharide sequence, is based on its lower antigenicity (ie, almost exclusive binding of antithrombin; length of <10 saccharides units render PF4 binding and formation of ultralarge complexes unlikely; synthetic derivative; little or no cross-reactivity with anti-PF4/heparin antibodies for platelet activation) and for (2) rivaroxaban is based on its nonheparin molecular structure.12 Further advantages of the use of factor Xa inhibitors over direct thrombin inhibitors are (1) avoidance of activated partial thromboplastin time (aPTT) confounding39-41 (ie, systematic under-dosing of direct thrombin inhibitors [DTIs] in a patient with HIT-associated consumptive coagulopathy that leads to elevation of the aPTT), (2) lower interference with thrombin-induced protein C activation (a potential risk factor for microvascular thrombosis in patients with severe HIT-associated disseminated intravascular coagulopathy), and (3) the graded range of available doses of fondaparinux including prophylactic, intermediate, and therapeutic doses (2.5 mg, 5 mg, 7.5 mg, and 10 mg) would allow rapid therapy adaptation in accordance to the clinical situation (ie, bleeding or thrombotic risk, depending on HIT risk). This fact could have underestimated the dominance of fondaparinux over argatroban. Similar, but not yet established in therapy of HIT, the doses of rivaroxaban could be adopted (2.5 mg, 5 mg, 10 mg, 15 mg, or 20 mg).
In this study, we found that fondaparinux was clinically more effective than argatroban, which is in line with the results of previous studies.12,15,17-19 Clinical data for rivaroxaban use in HIT are limited. To date, no approval studies for either of the 2 anticoagulants have been initiated, although both drugs are frequently applied in the context of suspected and acute HIT. Currently, their use for this indication is “off-label.”
In our study population, patients with high pretest probability for HIT (ie, 4Ts score ≥6) were more likely prescribed fondaparinux, although it is not approved for HIT therapy. Patients with low and moderate risk for HIT (4Ts score <6) were more likely prescribed rivaroxaban, in 8/19 patients with low risk and 7/19 patients with moderate risk for HIT (Table 2). To account for potential confounding by indication, we adjusted costs and outcome estimates by assigning probability weights of treatment assignment per risk group. In our adjusted analysis that accounted for the imbalance in treatment assignment, fondaparinux still dominated argatroban.
The cost-effectiveness results are robust across a range of model assumptions, including a variety of adverse events incidence rates, daily costs of hospitalization, days of prolongation of hospital stay, allocation of patients to a particular alternative anticoagulant according to risk of HIT as evaluated by 4Ts scores, and by using input parameters from other studies. The analyses were most sensitive to incidence rates and length of prolongation of stay per drug. To check for robustness of our model, we performed PSA. PSA results confirmed our main findings, wherein fondaparinux dominated argatroban, whereas cost-effectiveness of rivaroxaban depended on the assumed threshold. Currently, it is not known how much the Swiss system is willing to pay to avoid a major adverse event arising from HIT suspicion, so we modeled the cost-effectiveness of fondaparinux and rivaroxaban against argatroban across a range of theoretical thresholds. Indeed, probability of fondaparinux dominating argatroban was higher in higher ICER range (at above 30 000 CHF).
In a United States study comparing Food and Drug Administration–approved argatroban and bivalirudin with fondaparinux, fondaparinux was the cost-effective strategy in comparison with both comparator drugs across a wide range of model assumptions.28 In our model, we considered average daily hospitalization costs and prolongation of stay as relevant variables for each drug. Aljabri and colleagues did not include daily costs of hospitalization in the estimation of overall costs, and this could partly explain why in our study, the absolute costs remain higher.28 In their model, they assumed that daily hospital costs are equal in each drug (hence were not included) and prolongation of stay is equal for each comparator drug in two scenarios: HIT (additonal 6 days) and not-HIT (additional 2 days). We included daily costs of hospitalization because we expected that each drug will have different clinical effects, including effects on prolongation of hospital stay after HIT suspicion, which influences total hospital costs more strongly than total drug costs. For example, patients who receive the approved DTI treatment (classic paradigm of HIT therapy) may be more likely to transition to a vitamin K antagonist (VKA) such as warfarin (with a mandatory minimum 5-day overlap between DTI and VKA), thus potentially prolonging costly hospitalization, including the incurring risk of VKA toxicity (microvascular thrombosis) and of bleeding complications. This is supported by the longer duration of hospitalization of patients receiving DTI. In contrast, the use of the nonapproved factor Xa inhibitors (modern paradigm of HIT therapy) might involve in clinical practice simply discharging the patient on ongoing factor Xa inhibitor therapy (eg, fondaparinux injections, abrupt transition from fondaparinux to rivaroxaban, direct transition from DTI to a factor Xa inhibitor). This would avoid several days of costly hospitalization for managing the above-mentioned overlap and might make the practical cost effectiveness differences between DTI and factor Xa inhibitors even greater. However, the results remained the same, even if we considered no overlap in DTI and VKA treatment, as in Aljabri study (supplemental Table 2). Furthermore, the no-overlap scenario is not seen in practice, at least in our institution. Morbidity and likelihood of HIT could influence the choice of drug and thus have an impact on daily costs of hospitalization. This was reflected by argatroban and rivaroxaban showing the highest and lowest cost per day of hospital stay, respectively, for both before and after HIT confirmation. Indeed, our model was most sensitive to daily costs of hospitalization and prolongation of stay, and the effect of their interaction (ie., daily costs of hospitalization times days of prolongation) has much greater weight than the effect of drug costs on total hospital costs, which is in line with other studies.25,42 This implies that the costs are driven by the effectiveness of each drug in shortening the days of hospital stay after HIT suspicion.
Our study results suggest that fondaparinux merits consideration as primary treatment options for patients with suspected HIT. This applies all the more because approvals of other nonheparin anticoagulants (ie, argatroban, lepirudin, danaparoid) for treatment of HIT have been based on historical control studies with relatively small numbers of patients included.9,10,43-48
Several strengths of our study are worth pointing out. To our knowledge, this is the first pharmacoeconomic evaluation study that assessed the cost-effectiveness of off-label nonheparin anticoagulants among patients with suspected HIT that modeled costs and outcomes using data from our cohort of patients. Other studies used data from cohorts of trial participants. We used primary data from our institution to calculate event rates and institutional costs and minimally relied on data from other sources to populate the parameters needed to operate our economic evaluation model, hence the modeling parameters are more likely to be appropriate. We distinguished between different parameters, including costs and length of hospital stay, and performed sensitivity analyses that allowed us to account for uncertainties in the parameters used and demonstrated the robustness of our results. We were able to confirm our results using probabilistic sensitivity analysis that integrates uncertainties in the distribution of parameters we used in the model. We found similarities in the estimate of our study with other studies done in other countries.25,26 Nevertheless, some limitations warrant mentioning. In spite of our institution being the largest university hospital in Switzerland, we had only 54 patients and 6 adverse events, hence our model may have been underpowered, and adverse events may have been underestimated. To address this, we performed sensitivity analyses including changing inputs from the largest studies in HIT and non-HIT context, respectively. Those supported use of fondaparinux vs argatroban at low trade-off (12 207 CHF per adverse event averted) and showed dominance of both fondaparinux and argatroban against rivaroxaban. A potential limitation may be the exclusion of costs for arterial thrombotic events and amputations, but there is no obvious reason why Xa inhibitors vs DTIs would have a difference in the expected frequency of arterial thrombotic events.28 Confounding by indication may have affected the cost-effectiveness results, and despite risk-weighted adjustments, we cannot fully eliminate treatment allocation bias. The costs considered in this analysis are limited to institutional costs, hence the cost-effectiveness results may only represent value-for-money within the perspective of the institution and not the society at large. Future studies can address this by expanding analysis to include other institutions. Results may have less generalizability in different settings because of different factors, including treatment protocols, costs of drugs, costs of hospitalization, and modes of health financing. Nonetheless, our model provides a structure that can be replicated by others in different settings.
Conclusions
This is the first cost-effectiveness analysis that compared off-label fondaparinux and rivaroxaban with approved argatroban using primary data in suspected HIT. Fondaparinux resulted in cost savings and more adverse events averted than argatroban; rivaroxaban is safer but is connected with higher medical costs. Our study suggests that fondaparinux is a viable alternative to argatroban and should be considered. Future studies involving more participants by expanding the modeling to a national population are needed to confirm our findings.
Supplementary Material
The full-text version of this article contains a data supplement.
Acknowledgments
D.S. has received funding from the European Union’s Horizon 2020 research and innovation program under the Marie Skłodowska-Curie grant agreement No. 801076. The funder had no role in the design and conduct, including collection, analysis, and interpretation of data; or in the preparation, review, or approval of the manuscript.
Authorship
Contribution: A.T., D.S., and M.S. contributed to the conception and design of the study; A.T., D.S., M.S., T.M., I.B., A.L., and S.B. contributed to analysis and interpretation; A.T. contributed to data collection; A.T., D.S., and M.S. wrote the article; A.T., D.S., T.M., S.B., A.L., I.B., and M.S. critically revised the article; A.T., D.S., T.M., S.B., A.L., I.B., and M.S. gave final approval of the article; D.S. and A.L. provided statistical analysis; and M.S. had overall responsibility.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Marc Schindewolf, Division of Angiology, Swiss Cardiovascular Center, Inselspital / Bern University Hospital, Freiburgstrasse, CH-3010 Bern, Switzerland; e-mail: marc.schindewolf@insel.ch.
References
- 1.Amiral J, Bridey F, Dreyfus M, et al. Platelet factor 4 complexed to heparin is the target for antibodies generated in heparin-induced thrombocytopenia. Thromb Haemost. 1992;68(1):95-96. [PubMed] [Google Scholar]
- 2.Visentin GP, Ford SE, Scott JP, Aster RH. Antibodies from patients with heparin-induced thrombocytopenia/thrombosis are specific for platelet factor 4 complexed with heparin or bound to endothelial cells. J Clin Invest. 1994;93(1):81-88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Girolami B, Prandoni P, Stefani PM, et al. The incidence of heparin-induced thrombocytopenia in hospitalized medical patients treated with subcutaneous unfractionated heparin: a prospective cohort study. Blood. 2003;101(8):2955-2959. [DOI] [PubMed] [Google Scholar]
- 4.Prandoni P, Siragusa S, Girolami B, Fabris F; BELZONI Investigators Group . The incidence of heparin-induced thrombocytopenia in medical patients treated with low-molecular-weight heparin: a prospective cohort study. Blood. 2005;106(9):3049-3054. [DOI] [PubMed] [Google Scholar]
- 5.Warkentin TE. Laboratory diagnosis of heparin-induced thrombocytopenia. Int J Lab Hematol. 2019;41(S1 Suppl 1):15-25. [DOI] [PubMed] [Google Scholar]
- 6.Cuker A, Arepally GM, Chong BH, et al. American Society of Hematology 2018 guidelines for management of venous thromboembolism: heparin-induced thrombocytopenia. Blood Adv. 2018;2(22):3360-3392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cuker A, Gimotty PA, Crowther MA, Warkentin TE. Predictive value of the 4Ts scoring system for heparin-induced thrombocytopenia: a systematic review and meta-analysis. Blood. 2012;120(20):4160-4167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Warkentin TE, Cook RJ, Marder VJ, et al. Anti-platelet factor 4/heparin antibodies in orthopedic surgery patients receiving antithrombotic prophylaxis with fondaparinux or enoxaparin. Blood. 2005;106(12):3791-3796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lewis BE, Wallis DE, Berkowitz SD, et al. ; ARG-911 Study Investigators . Argatroban anticoagulant therapy in patients with heparin-induced thrombocytopenia. Circulation. 2001;103(14):1838-1843. [DOI] [PubMed] [Google Scholar]
- 10.Lewis BE, Wallis DE, Leya F, Hursting MJ, Kelton JG; Argatroban-915 Investigators . Argatroban anticoagulation in patients with heparin-induced thrombocytopenia. Arch Intern Med. 2003;163(15):1849-1856. [DOI] [PubMed] [Google Scholar]
- 11.Kondo LM, Wittkowsky AK, Wiggins BS. Argatroban for prevention and treatment of thromboembolism in heparin-induced thrombocytopenia. Ann Pharmacother. 2001;35(4):440-451. [DOI] [PubMed] [Google Scholar]
- 12.Schindewolf M, Steindl J, Beyer-Westendorf J, et al. Use of Fondaparinux off-label or approved anticoagulants for management of heparin-induced thrombocytopenia. J Am Coll Cardiol. 2017;70(21):2636-2648. [DOI] [PubMed] [Google Scholar]
- 13.Schindewolf M, Steindl J, Beyer-Westendorf J, et al. Frequent off-label use of fondaparinux in patients with suspected acute heparin-induced thrombocytopenia (HIT)--findings from the GerHIT multi-centre registry study. Thromb Res. 2014;134(1):29-35. [DOI] [PubMed] [Google Scholar]
- 14.Walenga JM, Prechel M, Hoppensteadt D, et al. Apixaban as an alternate oral anticoagulant for the management of patients with heparin-induced thrombocytopenia. Clin Appl Thromb Hemost. 2013;19(5):482-487. [DOI] [PubMed] [Google Scholar]
- 15.Linkins LA, Warkentin TE, Pai M, et al. Rivaroxaban for treatment of suspected or confirmed heparin-induced thrombocytopenia study. J Thromb Haemost. 2016;14(6):1206-1210. [DOI] [PubMed] [Google Scholar]
- 16.Linkins LA, Dans AL, Moores LK, et al. Treatment and prevention of heparin-induced thrombocytopenia: antithrombotic therapy and prevention of thrombosis, 9th ed: american college of chest physicians evidence-based clinical practice guidelines [published correction appears in Chest. 2015;148(6):1529]. Chest. 2012;141(2 Suppl):e495S-e530S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Snodgrass MN, Shields J, Rai H. Efficacy and safety of fondaparinux in patients with suspected heparin-induced thrombocytopenia. Clin Appl Thromb Hemost. 2016;22(8):712-717. [DOI] [PubMed] [Google Scholar]
- 18.Davis KA, Davis DO. Direct acting oral anticoagulants for the treatment of suspected heparin-induced thrombocytopenia. Eur J Haematol. 2017;99(4):332-335. [DOI] [PubMed] [Google Scholar]
- 19.Warkentin TE, Pai M, Linkins LA. Direct oral anticoagulants for treatment of HIT: update of Hamilton experience and literature review. Blood. 2017;130(9):1104-1113. [DOI] [PubMed] [Google Scholar]
- 20.Tran PN, Tran MH. Emerging role of direct oral anticoagulants in the management of heparin-induced thrombocytopenia. Clin Appl Thromb Hemost. 2018;24(2):201-209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Efird LE, Kockler DR. Fondaparinux for thromboembolic treatment and prophylaxis of heparin-induced thrombocytopenia. Ann Pharmacother. 2006;40(7-8):1383-1387. [DOI] [PubMed] [Google Scholar]
- 22.Lobo B, Finch C, Howard A, Minhas S. Fondaparinux for the treatment of patients with acute heparin-induced thrombocytopenia. Thromb Haemost. 2008;99(1):208-214. [DOI] [PubMed] [Google Scholar]
- 23.Smythe MA, Koerber JM, Fitzgerald M, Mattson JC. The financial impact of heparin-induced thrombocytopenia. Chest. 2008;134(3):568-573. [DOI] [PubMed] [Google Scholar]
- 24.Frame JN. The heparin-induced thrombocytopenia task force model: implementing quality improvement and economic outcome initiatives. Semin Hematol. 2005;42(3 Suppl 3):S28-S35. [DOI] [PubMed] [Google Scholar]
- 25.Nanwa N, Mittmann N, Knowles S, et al. The direct medical costs associated with suspected heparin-induced thrombocytopenia. PharmacoEconomics. 2011;29(6):511-520. [DOI] [PubMed] [Google Scholar]
- 26.Creekmore FM, Oderda GM, Pendleton RC, Brixner DI. Incidence and economic implications of heparin-induced thrombocytopenia in medical patients receiving prophylaxis for venous thromboembolism. Pharmacotherapy. 2006;26(10):1438-1445. [DOI] [PubMed] [Google Scholar]
- 27.Riedel R, Schmieder A, Koster A, Kim S, Baumgarten G, Schewe JC. [Heparin-induced thrombocytopenia type II (HIT II): A medical-economic view]. Med Klin Intensivmed Notfmed. 2017;112(4):334-346. [DOI] [PubMed] [Google Scholar]
- 28.Aljabri A, Huckleberry Y, Karnes JH, et al. Cost-effectiveness of anticoagulants for suspected heparin-induced thrombocytopenia in the United States. Blood. 2016;128(26):3043-3051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Husereau D, Drummond M, Petrou S, et al. ; CHEERS Task Force . Consolidated health economic evaluation reporting standards (CHEERS) statement. BMJ. 2013;346:f1049. [DOI] [PubMed] [Google Scholar]
- 30.Campbell HE, Stokes EA, Bargo D, et al. ; TRIGGER investigators . Costs and quality of life associated with acute upper gastrointestinal bleeding in the UK: cohort analysis of patients in a cluster randomised trial. BMJ Open. 2015;5(4):e007230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Arepally GM. Heparin-induced thrombocytopenia. Blood. 2017;129(21):2864-2872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tarifstruktur für ärztliche Leistungen (TARMED), Version 1.08,Tarifsystem TARMED. Iesundheit Bf, ed. 2018. tarmed-1.08-dt (1).pdf [Google Scholar]
- 33.Bundesamt für Statistik, Schweizerische Eidgenossenschaft, Departement des Innern, Abteilung Gesundheit und Soziales, Medizinische Statistik der Krankenhäuser 2017 : Anzahl Fälle und durchschnittliche Aufenthaltsdauer (DAD) nach Altersklasse und Diagnosekode; published on November 23, 2018 https://www.bfs.admin.ch/bfs/de/home/statistiken/gesundheit/gesundheitswesen/spitaeler/patienten-hospitalisierungen.assetdetail.6406957.html
- 34.Kang M, Alahmadi M, Sawh S, Kovacs MJ, Lazo-Langner A. Fondaparinux for the treatment of suspected heparin-induced thrombocytopenia: a propensity score-matched study. Blood. 2015;125(6):924-929. [DOI] [PubMed] [Google Scholar]
- 35.Cohen AT, Davidson BL, Gallus AS, et al. ; ARTEMIS Investigators . Efficacy and safety of fondaparinux for the prevention of venous thromboembolism in older acute medical patients: randomised placebo controlled trial. BMJ. 2006;332(7537):325-329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lewis BE, Wallis DE, Hursting MJ, Levine RL, Leya F. Effects of argatroban therapy, demographic variables, and platelet count on thrombotic risks in heparin-induced thrombocytopenia. Chest. 2006;129(6):1407-1416. [DOI] [PubMed] [Google Scholar]
- 37.Hursting MJ, Jang IK. Impact of renal function on argatroban therapy during percutaneous coronary intervention. J Thromb Thrombolysis. 2010;29(1):1-7. [DOI] [PubMed] [Google Scholar]
- 38.Cohen AT, Spiro TE, Büller HR, et al. ; MAGELLAN Investigators . Rivaroxaban for thromboprophylaxis in acutely ill medical patients. N Engl J Med. 2013;368(6):513-523. [DOI] [PubMed] [Google Scholar]
- 39.Warkentin TE. Anticoagulant failure in coagulopathic patients: PTT confounding and other pitfalls. Expert Opin Drug Saf. 2014;13(1):25-43. [DOI] [PubMed] [Google Scholar]
- 40.Warkentin TE. How I diagnose and manage HIT. Hematology (Am Soc Hematol Educ Program). 2011;2011(1):143-149. [DOI] [PubMed] [Google Scholar]
- 41.Greinacher A, Selleng K, Warkentin TE. Autoimmune heparin-induced thrombocytopenia. J Thromb Haemost. 2017;15(11):2099-2114. [DOI] [PubMed] [Google Scholar]
- 42.Wilke T, Tesch S, Scholz A, Kohlmann T, Greinacher A. The costs of heparin-induced thrombocytopenia: a patient-based cost of illness analysis. J Thromb Haemost. 2009;7(5):766-773. [DOI] [PubMed] [Google Scholar]
- 43.Chong BH, Gallus AS, Cade JF, et al. ; Australian HIT Study Group . Prospective randomised open-label comparison of danaparoid with dextran 70 in the treatment of heparin-induced thrombocytopaenia with thrombosis: a clinical outcome study. Thromb Haemost. 2001;86(5):1170-1175. [PubMed] [Google Scholar]
- 44.Magnani HN. Heparin-induced thrombocytopenia (HIT): an overview of 230 patients treated with orgaran (Org 10172). Thromb Haemost. 1993;70(4):554-561. [PubMed] [Google Scholar]
- 45.Greinacher A, Völpel H, Janssens U, et al. Recombinant hirudin (lepirudin) provides safe and effective anticoagulation in patients with heparin-induced thrombocytopenia: a prospective study. Circulation. 1999;99(1):73-80. [DOI] [PubMed] [Google Scholar]
- 46.Greinacher A, Janssens U, Berg G, et al. Lepirudin (recombinant hirudin) for parenteral anticoagulation in patients with heparin-induced thrombocytopenia. Heparin-associated thrombocytopenia study (HAT) investigators. Circulation. 1999;100(6):587-593. [DOI] [PubMed] [Google Scholar]
- 47.Lubenow N, Eichler P, Lietz T, Greinacher A; Hit Investigators Group . Lepirudin in patients with heparin-induced thrombocytopenia - results of the third prospective study (HAT-3) and a combined analysis of HAT-1, HAT-2, and HAT-3. J Thromb Haemost. 2005;3(11):2428-2436. [DOI] [PubMed] [Google Scholar]
- 48.Warkentin TE, Greinacher A. Heparin-induced thrombocytopenia: recognition, treatment, and prevention: the seventh ACCP conference on antithrombotic and thrombolytic therapy. Chest. 2004;126(3 Suppl):311S-337S. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.