Abstract
The aim of the study is to examine the relationship of fear of COVID-19 with well-being and life satisfaction through psychological distress among the college students in India. The study was conducted in two waves of the pandemic—during first and second waves of the COVID-19 among college students. A survey was conducted among 768 and 884 students in first and second waves of COVID-19 respectively for this purpose. Structural equation modeling was used to analyze the data. The study found out that the fear of COVID-19 positively related to psychological distress and negatively to well-being and life satisfaction and the effects were stronger in second wave. Also, the psychological distress mediates the relationship between fear of COVID-19 with well-being and life satisfaction, and the relationships were stronger during second wave. Proper coping strategies and mechanisms can be helpful to overcome the difficulties of such situation.
Keywords: COVID-19; Fear of COVID-19, psychological distress; Life satisfaction
Introduction
The novel coronavirus disease aroused the concerns on both public health and mental health of people around the world (Chan et al., 2021). Rapid spreading of the infection and high morbidity rates fueled up the fear and concerns among the people (El-Bardan & Lathabhavan, 2021). Globally, each country faced unique challenges during the pandemic in terms of psychological distress among the citizens, a high level of depression, anxiety and stress were reported in all country’s population compared to normal scenario (Wang et al., 2021a). Among Asian countries, especially developing economies, higher risk of developing adverse mental health includes women, people younger than 30 years and single and separated status (Wang et al., 2021a). The countries in which government had introduced stringent measures policies promptly during pandemic, the prevalence of depressive symptoms was significantly lower (Lee et al., 2021). Moreover, it was found that individuals with preexisting mood disorders are at higher risk of COVID-19 hospitalization and death and should be categorized as an at-risk group on the basis of a preexisting condition (Ceban et al., 2021). In different waves of COVID-19 and in post-COVID scenario also, high frequency of clinically significant depression and depressive symptoms are evidenced (Renaud-Charest et al., 2021). During the COVID-19 pandemic, students have prone to more psychological distress symptoms such as depression and stress compared to other occupational status (Xiong et al., 2020).
Various restrictions from the government and authorities such as quarantine, social distancing and travel restrictions etc. also taken as precautionary measures to mitigate the severe effects of the pandemic (Rossi et al., 2020). Such restrictions also added up mental health concerns since they have indirectly a lot of socio-economic factors such as loneliness, financial distress etc. (Elmer et al., 2020; Lathabhavan et al., 2021).The measures such as lockdown induced mental health concerns among those who experienced job loss, suspected contact with COVID-19 patient, being associated with larger family etc., in worst cases, the isolation led to loneliness and suicidal ideation (Le et al., 2020a). The face mask use was made compulsory by most of the governments, whereas some lenient policies in implementation and lack proper health education regarding this invited more stress and depressive symptoms among people (Wang et al., 2020a). Social distancing measures of various government including minimizing or suspending many business and job activities resulted in change in income status of majority of people and it enhanced depression and anxiety among them (Tran et al., 2020).
Previous studies have reported the psychological distress intensity varies differently among the population during different stages and time of COVID-19 pandemic due to various reasons. First, preventive measures from the government and the knowledge to take self-preventive measures played a good role in reducing the infection rate and or making it under control and this lead to reduction in mental health concerns (Wang et al., 2020c). Second, subsequent waves of pandemic had more mutated variants of virus and affected large population severely and this enhanced mental health concerns (Lathabhavan & Sudevan, 2022). Third, subsequent waves also witnessed many losses of lives, loss of loved ones etc. which raised mental health issues among adolescents and youth (Lathabhavan, 2021).
The present study was conducted in India where COVID-19 affected severely. Both first and second waves of COVID-19 were equally filled with loss and trauma in India due to high infection rate and death tolls (Lathabhavan, 2021). In such a scenario, fear of COVID-19 makes the people to protect themselves and their loved ones which can lead to depression, anxiety and stress (Kumar & Nayar, 2021). Moreover, media information about the daily infection rates, death tolls, related information and discussion also lead the people into psychological distress. In second wave, as death tolls and causalities were higher, children and adolescents faced more mental health issues as many of their families affected with COVID-19 and some lost their loved ones (Lathabhavan, 2021).
The college students or adolescents were highly vulnerable to mental health concerns during the pandemic, due to the direct or indirect effects of the pandemic. Students having relatives or friends who have been infected, fearing being infected, and having a pessimistic attitude to COVID-19 easily experience anxiety or depression (Ren et al., 2021a). Poor sleep quality during the pandemic also act as another cause for mood disorders among them (Ren et al., 2021b). Internet use and social media information updates frequently also enhances stress among them during pandemic scenario (Lathabhavan & Padhy, 2022).
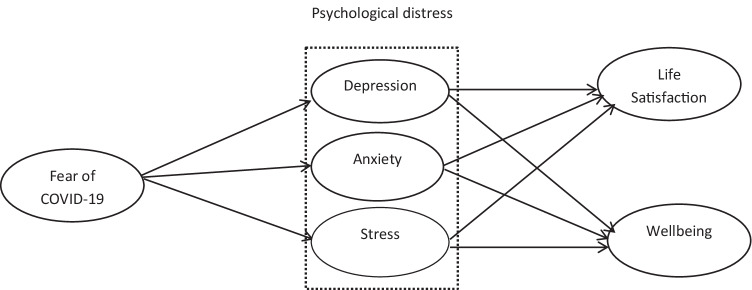
The present study considers SOR (Stimulus-Organism-Response) theory as the grounded theory to explain the mental health concerns among the students during the pandemic. As per the SOR theory, the stimulus effects on the individual leads to the behavioral and psychological outcomes (Mehrabian & Russell, 1974). It describes a process where an external environmental factor (stimulus) influences individual’s internal state (organism), which consequently results in their approach or avoidance behavior (response). In this unexpected pandemic situation, the crisis induced fear act as stimulus due to high infection rates and morbidity (Lathabhavan & Vispute, 2021). This leads to psychological distress among the individuals and unlimitedly increases the mental health concerns (Tandon, 2020). Thus, the study considers that fear of COVID-19( as stimulus), psychological distress (as organism) and life satisfaction and wellbeing (as response) for explaining the mental health concerns among the students. The study also considers mental health concerns of students in two COVID-19 waves as causalities and trauma were severe in India in both waves of infection.
Considering this, the present study aims to investigate the following:
The relationship of Fear of COVID-19 with a) Depression, b) Anxiety and c) Stress in two waves of COVID-19 among students
The relationship of depression with a) life satisfaction and b) Well-being in two waves of COVID-19 among students
The relationship of depression with a) life satisfaction and b) Well-being in two waves of COVID-19 among students
The relationship of anxiety with life satisfaction in two waves of COVID-19 among students
The mediating roles of Depression, Anxiety and Stress between Fear of COVID-19 and life satisfaction
The mediating roles of Depression, Anxiety and Stress between Fear of COVID-19 and Well-being.
The proposed model is depicted in Fig. 1
Fig. 1.
Proposed research model
Method
Participants
A survey was conducted in two waves – June 2020 (during COVID-19 first wave, T1) and May 2021 (during COVID-19 s wave, T2). Survey was conducted among students in various colleges and universities in India. During first wave of COVID-19, in June 2020, 768 students were participated in the survey. Among that, 413 were men (53.77%) and 355 were women (46.22%). During second wave, 884 students responded to survey of which 456 were men (51.58%) and 428 were women (48.42%). 152 students responded to both surveys, consisting of 75 men and 77 women.Survey was collected through online Google forms in both waves and made use of social media platforms for wide reach. Snowball sampling strategy was used for collecting data.
Measures
Fear of COVID-19 scale (FCV-19S) was measured using new scale as developed by Ahorsu et al. (2020). FCV-19S consists of 7 items. Sample item was “I am most afraid of Corona” and “My heart races or palpitate when I think about getting Corona”.
Depression Anxiety Stress Scale: Depression, anxiety, and stress were assessed utilizing the Depression Anxiety Stress Scale(DASS-21) (Lovibond & Lovibond, 1996). DASS-21 comprising 21 items and three dimensions (seven items per dimension) (e.g., “I could not seem to experience any positive feeling at all” for depression; “I was worried about situations in which I might panic” for anxiety; and “I found it difficult to relax” for stress). The participants responded to on a five-point likert scale from 1 (Did not apply to me at all) to 5 (Most of the time). Higher scores on each dimension reflect higher depression, anxiety and stress respectively.
DASS-21 is the most validated psychiatric scale during the COVID-19 pandemic in different countries. A few of the are listed here. Among Chinese population, during the initial breakout of COVID-19, the psychological distress (using DASS-21) found to be moderate to severe (Wang et al., 2020b). Spanish participants reported significantly higher DASS-21 stress and depression scores during the COVID-19 pandemic (Wang et al., 2021b). Americans also reported more DASS-21 stress and depressive symptoms during the pandemic (Wang et al., 2021c). Among Polish respondents, DASS-21 reported higher level of depression, anxiety, and stress (Wang et al., 2020a). A higher level of stress, anxiety, and depression (DASS-21) were visible among Philippines during the pandemic (Tee et al., 2020). In Vietnam also, high level of stress and phycological distress were reported during the pandemic lockdown (Le et al., 2020b).
Wellbeing was measured using WHO-Five Well-being Index (WHO-5). Sample item is “I have felt calm and relaxed”. A seven-point Likert-type scale was used with anchors 1 (strongly disagree) to 5 (strongly agree).
Life satisfaction was measured using Satisfaction with Life Scale. Participants completed the SWLS (Diener et al., 1985), which asked direct questions about life satisfaction (e.g., “In most ways my life is close to my ideal” and “I am satisfied with my life”), which were answered on a 5-point Likert scale.
Data Analysis
Structural equation modeling (SEM) method implemented using AMOS 24.0 (Arbuckle, 2016) were used to test the research model. Confirmatory Factor Analysis was performed with maximum likelihood estimation to examine the goodness of the model. The models’ goodness of fit was evaluated using the criteria: relative χ2: ( χ2/df) < 3, root mean square error of approximation (RMSEA): ⩽0.08, standardized root mean square residual (SRMR): ⩽0.06, Goodness of fit index (GFI) ⩾0.90, comparative fit index (CFI) ⩾0.90, and Tucker-Lewis index (TLI) ⩾0.90 (Byrne, 2013; Hu & Bentler, 1998). Cronbach’s α, average variance extracted (AVE), composite reliability (CR), and average loadings (AL) were also used to check the reliability and validity of the instruments.
Results
Descriptive Statistics
Table 1 describes the descriptive statistics of the study in two waves T1 and T2. All significant relationships were in expected direction.
Table 1.
Means, standard deviations, and intercorrelations among study variables (NT1 = 768, NT2 = 884)
| Mean | SD | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Fear of COVID-19 T1 | 2.32 | 0.87 | 1 | |||||||||||
| 2.Fear of COVID-19 T2 | 2.37 | 0.92 | 0.39 | 1 | ||||||||||
| 3.Depression T1 | 2.54 | 0.86 | 0.24 | 0.23 | 1 | |||||||||
| 4.Depression T2 | 2.56 | 0.82 | 0.27 | 0.27 | 0.38 | 1 | ||||||||
| 5.Anxiety T1 | 2.33 | 1.07 | 0.25 | 0.31 | 0.34 | 0.36 | 1 | |||||||
| 6. Anxiety T2 | 2.45 | 0.87 | 0.23 | 0.31 | 0.29 | 0.39 | 0.49 | 1 | ||||||
| 7.Stress T1 | 3.76 | 0.87 | 0.23 | 0.24 | 0.24 | 0.27 | 0.19 | 0.41 | 1 | |||||
| 8. Stress T2 | 3.67 | 0.85 | 0.26 | 0.27 | 0.27 | 0.33 | 0.21 | 0.24 | 0.42 | 1 | ||||
| 9. Life satisfaction T1 | 4.21 | 0.88 | -0.27 | -0.22 | -0.23 | -0.34 | -0.15 | -0.27 | -0.29 | -0.19 | 1 | |||
| 10. Life satisfaction T2 | 4.14 | 0.97 | -0.28 | -0.24 | -0.25 | -0.39 | -0.17 | -0.29 | -0.33 | -0.17 | 0.43 | 1 | ||
| 11. wellbeing T1 | 4.02 | 0.88 | -0.33 | -0.34 | -0.32 | -0.39 | -0.19 | -0.17 | -0.23 | -0.24 | 0.19 | 0.25 | 1 | |
| 12. Wellbeing T2 | 4.11 | 0.89 | -0.34 | -0.36 | -0.35 | -0.42 | -0.23 | -0.16 | -0.24 | -0.26 | 0.23 | 0.27 | 0.45 | 1 |
Common Method Bias Analysis
On account of a common instrument used for measuring all the variables with different kind of scales, there is a possibility of encountering common method bias issue. To check this, Harman’s single factor test was employed. A factor analysis using SPSS 24.0 was performed, in which all the items were loaded with a threshold to attain one factor. The results showed that a single factor contributes 27.26% of total variance extracted for T1 and 24.24% of total variance extracted for T2, which is below 50%. This confirms that the CMB is not a major concern for this study.
Reliability and Validity Analysis
For this study, the average variance extracted (AVE) values are above 0.50 indicating excellent content and convergent validity of all the measures. The item loadings vary from 0.66 to 0.95, also supporting the validity as all the loadings are above the threshold of 0.60. The composite reliability of all latent variables seems to be above 0.75 and adequate. The Cronbach's alpha values of variables exceeds the threshold value of 0.70 (Nunnally, 1994). Table 2 depicts the discriminant validity details. Discriminant validity is established as the square roots of all AVE scores are more than their corresponding inter-correlations. Based on the above findings, it can be inferred that the measurement model exhibited an adequate level of reliability and validity.
Table 2.
Validity and reliability results
| AL | CR | AVE | Cronbach’s α | |||||
|---|---|---|---|---|---|---|---|---|
| T1 | T2 | T1 | T2 | T1 | T2 | T1 | T2 | |
| Fear of COVID-19 | 0.761 | 0.784 | 0.809 | 0.812 | 0.781 | 0.753 | 0.871 | 0.864 |
| Depression | 0.787 | 0.825 | 0.857 | 0.882 | 0.765 | 0.683 | 0.887 | 0.892 |
| Anxiety | 0.816 | 0.798 | 0.793 | 0.781 | 0.677 | 0.712 | 0.843 | 0.854 |
| Stress | 0.823 | 0.831 | 0.824 | 0.822 | 0.813 | 0.834 | 0.871 | 0.873 |
| Life satisfaction | 0.772 | 0.785 | 0.836 | 0.843 | 0.775 | 0.785 | 0.833 | 0.843 |
| Wellbeing | 0.835 | 0.848 | 0.897 | 0.883 | 0.734 | 0.745 | 0.891 | 0.901 |
Structural Equation Modeling Results
The proposed model found to be perfectly fit with the data in waves. In first wave, model fit was excellent with χ2/df (T1) = 1.76, p < 0.01, CFI T1 = 0.95, TLIT1 = 0.94,RMSEAT1 = 0.04, and SRMRT1 = 0.05. In second wave also, the model fit with data perfectly with χ2/df (T2) = 1.89, p < 0.01, CFI T2 = 0.96, TLIT2 = 0.94,RMSEAT2 = 0.04, and SRMRT2 = 0.05.
The results of structural equation modeling of both waves T1 and T2 depicted in Table 3. In the first wave of COVID-19 (T1), fear of COVID-19 has reported all significant positive relationship with depression (βT1 = 0.31, p < 0.01), anxiety (βT1 = 0.26, p < 0.001) and stress (βT1 = 0.19, p < 0.01). Depression found to be significantly related to life satisfaction (βT1=-0.31, p < 0.05) and wellbeing (βT1 = -0.34, p < 0.001). Anxiety also reported significant negative relationship with life satisfaction (βT1=-0.28, p < 0.05) and wellbeing (βT1 = -0.19, p < 0.001). Stress is also found to be significantly related to life satisfaction (βT1=-0.32, p < 0.05) and wellbeing (βT1 = -0.21, p < 0.05).
Table 3.
Structural equation modeling results
| Relationships | Standardized path coefficient | |
|---|---|---|
| T1(N = 768) | T2(N = 884) | |
| Fear of COVID-19➔ Depression | 0.31** | 0.36*** |
| Fear of COVID-19➔ Anxiety | 0.26*** | 0.29* |
| Fear of COVID-19➔ Stress | 0.19** | 0.24* |
| Depression ➔ Life satisfaction | -0.31* | -0.33* |
| Depression ➔ Wellbeing | -0.34*** | -0.35*** |
| Anxiety➔ Life satisfaction | -0.28* | -0.32** |
| Anxiety➔ Wellbeing | -0.19*** | -0.24** |
| Stress ➔ Life satisfaction | -0.32* | -0.37*** |
| Stress ➔ Wellbeing | -0.21* | -0.24* |
*p < 0.5, **p < 0.01, ***p < 0.001
Direct and Indirect Effects
The partially mediated model was tested for significance using the bootstrap estimation procedure (a bootstrap sample of 2,000 was specified). The mediation effects of psychological distress is shown in Table 4 and Table 5. Table 4 depicts the mediation effects of Fear of COVID-19 on well-being during first and second waves of COVID-19. Table 5 represents the mediation effects of Fear of COVID-19 on life satisfaction during first and second waves of COVID-19.
Table 4.
Direct, indirect and total effects of FCV-19S on well-being
| Model pathways | T1 (N = 768) | T2(N = 884) | ||||
|---|---|---|---|---|---|---|
| Estimates | LL 95% CI | UL 95% CI | Estimates | LL 95% CI | UL 95% CI | |
| Direct effects | ||||||
| Fear of COVID-19Depression | 0.312 | 0.216 | 0.397 | 0.362 | 0.245 | 0.456 |
| Fear of COVID-19 Anxiety | 0.263 | 0.192 | 0.312 | 0.294 | 0.211 | 0.414 |
| Fear of COVID-19Stress | 0.191 | 0.112 | 0.267 | 0.241 | 0.134 | 0.333 |
| Depression Well-being | -0.343 | -0.372 | -0.295 | -0.353 | -0.398 | -0.312 |
| Anxiety Well-being | -0.194 | -0.319 | -0.133 | -0.242 | -0.320 | -0.144 |
| Stress Well-being | -0.210 | -0.322 | -0.111 | -0.244 | -0.357 | -0.112 |
| Fear of COVID-19Well-being | -0.225 | -0.355 | -0.134 | -0.247 | -0.413 | -0.135 |
| Indirect effects | ||||||
| Fear of COVIDDepression Well-being | -0.052 | -0.103 | -0.034 | -0.032 | -0.087 | -0.027 |
| Fear of COVIDAnxietyWell-being | -0.041 | -0.089 | -0.031 | -0.042 | -0.076 | -0.033 |
| Fear of COVIDStressWell-being | -0.053 | -0.079 | -0.041 | -0.062 | -0.098 | -0.047 |
| Total effect | -0.192 | -0.223 | -0.149 | -0.187 | -0.221 | -0.181 |
Bootstrap sample size = 2000; LL Lower limit; UL Upper limit; CI Confidence interval
Table 5.
Direct, indirect and total effects of FCV-19S on life satisfaction
| Model pathways | T1 (N = 768) | T2(N = 884) | ||||
|---|---|---|---|---|---|---|
| Estimates | LL 95% CI | UL 95% CI | Estimates | LL 95% CI | UL 95% CI | |
| Direct effects | ||||||
| Fear of COVID-19➔Depression | 0.312 | 0.216 | 0.397 | 0.362 | 0.245 | 0.456 |
| Fear of COVID-19➔ Anxiety | 0.263 | 0.192 | 0.312 | 0.294 | 0.211 | 0.414 |
| Fear of COVID-19➔Stress | 0.191 | 0.112 | 0.267 | 0.241 | 0.134 | 0.333 |
| Depression➔Life satisfaction | -0.253 | -0.274 | -0.213 | -0.273 | -0.314 | -0.202 |
| Anxiety ➔Life satisfaction | -0.187 | -0.265 | -0.145 | -0.212 | -0.316 | -0.111 |
| Stress ➔Life satisfaction | -0.278 | -0.358 | -0.188 | -0.322 | -0.461 | -0.237 |
| Fear of COVID-19 ➔Life satisfaction | ||||||
| Indirect effects | ||||||
| Fear of COVID➔Depression ➔Life satisfaction | -0.051 | -0.084 | -0.021 | -0.045 | -0.078 | -0.034 |
| Fear of COVID➔Anxiety ➔Life satisfaction | -0.045 | -0.097 | -0.321 | -0.034 | -0.079 | -0.021 |
| Fear of COVID➔Stress ➔Life satisfaction | -0.054 | -0.078 | -0.234 | -0.049 | -0.098 | -0.035 |
| Total effect | -0.212 | -0.319 | -0.132 | -0.195 | -0.298 | -0.113 |
Bootstrap sample size = 2000; LL Lower limit; UL Upper limit; CI Confidence interval
Bootstrap sample size = 2000; LL Lower limit; UL Upper limit; CI Confidence interval. * Total effect
Apart from the direct effects depicted in Table 3, the indirect effects of fear of COVID-19 on wellbeing via depression, anxiety and stress were -0.052, -0.041 and -0.053 respectively during T1 and -0.032, -0.042 and -0.062 respectively during T2 (Refer Table 4). Therefore, higher fear of COVID-19 was also associated with higher depression, anxiety and stress, in turn this higher depression, anxiety and stress were related with lower wellbeing during both waves of COVID-19 in India. Likewise the indirect effects of fear of COVID-19 on wellbeing via depression, anxiety and stress were -0.051, -0.045 and -0.054 respectively during T1 and -0.045, -0.034 and -0.049 respectively during T2 (Refer Table 5). Therefore, higher fear of COVID-19 was also associated with higher depression, anxiety and stress, in turn this higher depression, anxiety and stress were related with lower life satisfaction among students during both waves of COVID-19 in India.
Discussion
The main aim of the study was to investigate the mental health concerns of college students during the pandemic. For the theoretical support, the study considered SOR (Stimulus-Organism-Response) theory as the grounded theory. Based on that, the study has chosen fear of COVID-19( as stimulus), psychological distress (as organism) and life satisfaction and wellbeing (as response) for explaining the mental health concerns among the students. Thus, the study specifically aimed to investigate the effects of fear of COVID-19 on depression, anxiety and stress among the college students in India. The study also aimed to analyze the pandemic fear effects on life satisfaction and wellbeing. The study also focused on the mediating effects of psychological distress in the relationships of fear of COVID-19 with life satisfaction and wellbeing. For this two studies were conducted- June 2020 (during COVID-19 first wave, T1) and May 2021 (during COVID-19 s wave,T2). During COVID-19 first wave, 768 students were participated, and 884 students were participated in the second wave of COVID-19. Online surveys were conducted for obtaining the responses.
The novel contributions of the study to theory are multifold. First, the study adds its valuable contribution to the literature of pandemic fear studies by finding out the significant positive relationships of fear of COVID-19 with psychological distress in both first wave and second wave of COVID-19 among the college students in India. This implies the pandemic fear induces psychological distress among the individuals (Duong, 2021). The pandemic changes also brought up depressive and anxiety behavior among the adolescents (Ren et al., 2021a). The study thus supports the findings of the research in this area (Duong, 2021).
Second, the study adds valuables results to the psychological distress literature during the pandemic. The study revealed a significant negative relationship between the psychological distress with life satisfaction and wellbeing. The sudden and unexpected changes of pandemic around the globe have resulted in psychological distress among the population, leading to reduced wellbeing and life satisfaction (Duong, 2021). The previous studies had reported that different antecedents of the psychological distress including pandemic fear (Duong, 2021), loss of loved ones (Le et al., 2020a), government policies (Wang et al., 2020c), media/internet influence (Lathabhavan & Padhy, 2022) and social restrictions (Ren et al., 2021b) etc.
Third, another novel contribution of the study is the introduction of psychological distress as mediator to find the relationship between the fear of COVID-19 with life satisfaction and wellbeing. The study revealed that the psychological distress—ie. depression, anxiety and stress – mediates the relationships of fear of COVID-19 with life satisfaction and wellbeing. This supports the previous results in the area of fear of COVID-19 and life satisfaction (Duong, 2021).
Last, the study has found that fear of COVID-19 and psychological distress during the COVID-19 s wave is more severe compared to the first wave in India. Also, the negative effects of the same on life satisfaction and well-being seem to be severe during the second wave. It might be due to the rapid spread of the COVID-19 and high death tolls during this period. Moreover, issues like oxygen shortage and unavailability of patient bed etc. also might have caused increasing fear and psychological distress and leading to lower life satisfaction and wellbeing. The study stands among previous studies which conducted two waves studies and supports with similar outcomes (Wang et al., 2020c).
The practical implication of study requires special discussion, as mental health concerns are huge during the pandemic, and a positive mental health is the need of the hour. As COVID-19 s wave severely affected India with high rate of death tolls, the mental health concerns were more among adolescents. The fear of getting affected to self and family members seems high as may bereavements in many families (Lathabhavan, 2021). Stress coping mechanisms and counseling during such difficult situations will be helpful to an extent to overcome such trauma. A collective mechanism of individual, kin and kith, authorities, health and psychological practitioners can bring up change to this difficult situation and help for the needy. Discussing about more specific treatment methods, the most evidence-based treatment is cognitive behaviour therapy (CBT), especially Internet CBT that can prevent the spread of infection during the pandemic (Ho Su Hui et al., 2020). Moreover, this is cost-effective, and can treat different psychiatric symptoms (Soh et al., 2020; Zhang & Ho, 2017).
Limitations and Future Research Directions
The study has some limitations. First, the analysis in this study is based on cross sectional data. Future studies can concentrate on longitudinal studies and responses from secondary sources may be analyzed. Second, this study mainly used self-reported questionnaires to measure psychiatric symptoms and did not make clinical diagnosis. The gold standard for establishing psychiatric diagnosis involved structured clinical interview and functional neuroimaging, and future studies may follow that (Ho et al., 2020; Ho et al., 2021; Husain et al., 2020a, b). Future research in this area can focus on different psychological variables, focusing more on positive psychology and mental health, such as to assess how Indian students feel about COVID-19 vaccine, and prospective researchers can follow potential similar studies (Nguyen et al., 2021).
Conclusion
COVID -19 pandemic associated with mental health concerns. The present study found out that fear of COVID-19 induces the psychological distress and in turn affect negatively with life satisfaction and wellbeing. The study also revealed that during second wave infection of COVID-19, the pandemic fear effects were stronger on psychological distress and thus its relations on life satisfaction and wellbeing. Coping mechanisms and strategies to cope up with stress will be helpful in such situation to overcome issues. Future studies can focus on different psychological outcomes and on different geographical locations.
Data Availability' Statement
The data available on request for research purpose.
Declarations
Ethical Statement
The research confined to the highest level of ethics
Conflict of Interest
None
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Ahorsu, D. K., Lin, C. Y., Imani, V., Saffari, M., Griffiths, M. D., & Pakpour, A. H. (2020). The fear of COVID-19 scale: development and initial validation. International Journal of Mental Health and Addiction, 1–9. [DOI] [PMC free article] [PubMed]
- Arbuckle, J. L. (2016). IBM® SPSS® User’s Guide AmosTM 24. IBM, Chicago, IL., 1–720.
- Byrne BM. Structural Equation Modeling with AMOS: Basic Concepts, Applications, and Programming. Routledge; 2013. [Google Scholar]
- Ceban, F., Nogo, D., Carvalho, I. P., Lee, Y., Nasri, F., Xiong, J., Lui, L. M. W., Subramaniapillai, M., Gill, H., Liu, R. N., Joseph, P., Teopiz, K. M., Cao, B., Mansur, R. B., Lin, K., Rosenblat, J. D., Ho, R. C., & McIntyre, R. S. (2021). Association between Mood Disorders and Risk of COVID-19 Infection, Hospitalization, and Death: A Systematic Review and Meta-analysis. In JAMA Psychiatry (vol. 78, Issue 10, pp. 1079–1091). American Medical Association. 10.1001/jamapsychiatry.2021.1818 [DOI] [PMC free article] [PubMed]
- Chan DKC, Zhang CQ, Weman-Josefsson K. Why people failed to adhere to COVID-19 preventive behaviors? Perspectives from an integrated behavior change model. Infection Control and Hospital Epidemiology. 2021;42(3):375–376. doi: 10.1017/ice.2020.245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diener E, Emmons RA, Larsem RJ, Griffin S. The satisfaction with life scale. Journal of Personality Assessment. 1985;49(1):71–75. doi: 10.4324/9781003035312-41. [DOI] [PubMed] [Google Scholar]
- Duong, C. D. (2021). The impact of fear and anxiety of Covid-19 on life satisfaction: Psychological distress and sleep disturbance as mediators. Personality and Individual Differences, 178. 10.1016/j.paid.2021.110869 [DOI] [PMC free article] [PubMed]
- El-Bardan, M. F., & Lathabhavan, R. (2021). Fear of COVID-19 scale: Psychometric properties, reliability and validity in Egyptian population. Diabetes & Metabolic Syndrome: Clinical Research & Reviews,15(4), 102153. [DOI] [PubMed]
- Elmer T, Mepham K, Stadtfeld C. Students under lockdown: Comparisons of students’ social networks and mental health before and during the COVID-19 crisis in Switzerland. PLoS One. 2020;15(7 July):1–22. doi: 10.1371/journal.pone.0236337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ho, C. S., Lim, L. J., Lim, A. Q., Chan, N. H., Tan, R. S., Lee, S. H., & Ho, R. (2020). Diagnostic and predictive applications of functional near-infrared spectroscopy for major depressive disorder: a systematic review. Frontiers in psychiatry,378, 1–28. [DOI] [PMC free article] [PubMed]
- Ho, R. C., Sharma, V. K., Tan, B. Y. Q., Ng, A. Y. Y., Lui, Y. S., Husain, S. F., Ho, C. S., Tran, B. X., Pham, Q. H., McIntyre, R. S., & Chan, A. C. Y. (2021). Comparison of brain activation patterns during olfactory stimuli between recovered COVID-19 patients and healthy controls: A functional near-infrared spectroscopy (fNIRS) study. Brain Sciences, 11(8). 10.3390/brainsci11080968 [DOI] [PMC free article] [PubMed]
- Ho Su Hui, C., Ho, C. S., Chee, C. Y., & Ho, R. C. (2020). Mental Health Strategies to Combat the Psychological Impact of COVID-19 Beyond Paranoia and Panic. Annals Academy of Medicine Singapore, 49(1). [PubMed]
- Hu LT, Bentler PM. Fit indices in covariance structure modeling: Sensitivity to underparameterized model misspecification. Psychological Methods. 1998;3(4):424–453. doi: 10.1037/1082-989X.3.4.424. [DOI] [Google Scholar]
- Husain, S. F., Tang, T. B., Yu, R., Tam, W. W., Tran, B., Quek, T. T., Hwang, S. H., Chang, C. W., Ho, C. S., & Ho, R. C. (2020a). Cortical haemodynamic response measured by functional near infrared spectroscopy during a verbal fluency task in patients with major depression and borderline personality disorder. EBioMedicine, 51. 10.1016/j.ebiom.2019.11.047 [DOI] [PMC free article] [PubMed]
- Husain, S. F., Yu, R., Tang, T. B., Tam, W. W., Tran, B., Quek, T. T., Hwang, S. H., Chang, C. W., Ho, C. S., & Ho, R. C. (2020b). Validating a functional near-infrared spectroscopy diagnostic paradigm for Major Depressive Disorder. Scientific Reports, 10(1). 10.1038/s41598-020-66784-2 [DOI] [PMC free article] [PubMed]
- Kumar A, Nayar KR. COVID 19 and its mental health consequences. Journal of Mental Health. 2021;30(1):1–2. doi: 10.1080/09638237.2020.1757052. [DOI] [PubMed] [Google Scholar]
- Lathabhavan, R. (2021). First and second waves of COVID-19 : A comparative study on the impact of pandemic fear on the mental health of university students in India. Journal of Loss and Trauma, 1–2. 10.1080/15325024.2021.1950432
- Lathabhavan R, Barami.A N, Kurikkal MPMM, Manoj N. Mental health concerns of small business entrepreneurs in India due to COVID-19 financial distress. Asian Journal of Psychiatry. 2021 doi: 10.1080/13518040701205365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lathabhavan R, Padhy PC. Role of fear of COVID-19 in the relationship of problematic internet use and stress : A retrospective cohort study among Gen X, Y and Z. Asian Journal of Psychiatry. 2022;67:102937. doi: 10.1016/j.ajp.2021.102937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lathabhavan, R., & Sudevan, S. (2022). The impacts of psychological distress on life satisfaction and wellbeing of the indian general population during the first and second waves of COVID-19: A comparative study. International Journal of Mental Health and Addiction, 0123456789. 10.1007/s11469-021-00735-4 [DOI] [PMC free article] [PubMed]
- Lathabhavan, R., & Vispute, S. (2021). Examining the mediating effects of stress on fear of COVID-19 and well-being using structural equation modeling. International Journal of Mental Health and Addiction, 1–9. [DOI] [PMC free article] [PubMed]
- Le, H. T., Lai, A. J. X., Sun, J., Hoang, M. T., Vu, L. G., Pham, H. Q., Nguyen, T. H., Tran, B. X., Latkin, C. A., Le, X. T. T., Nguyen, T. T., Pham, Q. T., Ta, N. T. K., Nguyen, Q. T., Ho, R. C. M., & Ho, C. S. H. (2020a). Anxiety and depression among people under the nationwide partial lockdown in Vietnam. Frontiers in Public Health, 8. 10.3389/fpubh.2020.589359 [DOI] [PMC free article] [PubMed]
- Le, X. T. T., Dang, A. K., Toweh, J., Nguyen, Q. N., Le, H. T., Do, T. T. T., Phan, H. B. T., Nguyen, T. T., Pham, Q. T., Ta, N. K. T., Nguyen, Q. T., Nguyen, A. N., van Duong, Q., Hoang, M. T., Pham, H. Q., Vu, L. G., Tran, B. X., Latkin, C. A., Ho, C. S. H., & Ho, R. C. M. (2020b). Evaluating the psychological impacts related to COVID-19 of Vietnamese people under the first nationwide partial lockdown in Vietnam. Frontiers in Psychiatry, 11. 10.3389/fpsyt.2020.00824 [DOI] [PMC free article] [PubMed]
- Lee, Y., Lui, L. M. W., Chen-Li, D., Liao, Y., Mansur, R. B., Brietzke, E., Rosenblat, J. D., Ho, R., Rodrigues, N. B., Lipsitz, O., Nasri, F., Cao, B., Subramaniapillai, M., Gill, H., Lu, C., & McIntyre, R. S. (2021). Government response moderates the mental health impact of COVID-19: A systematic review and meta-analysis of depression outcomes across countries. In Journal of Affective Disorders (vol. 290, pp. 364–377). Elsevier B.V. 10.1016/j.jad.2021.04.050 [DOI] [PMC free article] [PubMed]
- Lovibond, S. H., & Lovibond, P. F. (1996). Manual for the depression anxiety stress scales. In Psychology Foundation of Australia.
- Mehrabian A, Russell James A. An approach to environmental psychology. The MIT Press; 1974. [Google Scholar]
- Nguyen LH, Hoang MT, Nguyen LD, Ninh LT, Nguyen HTT, Nguyen AD, Vu LG, Vu GT, Doan LP, Latkin CA, Tran BX, Ho CSH, Ho RCM. Acceptance and willingness to pay for COVID-19 vaccines among pregnant women in Vietnam. Tropical Medicine and International Health. 2021;26(10):1303–1313. doi: 10.1111/tmi.13666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nunnally, J. C. (1994). Psychometric theory. Tata McGraw-hill education.
- Ren, Z., Xin, Y., Ge, J., Zhao, Z., Liu, D., Ho, R. C. M., & Ho, C. S. H. (2021a). Psychological impact of COVID-19 on college students after school reopening: A cross-sectional study based on machine learning. Frontiers in Psychology, 12. 10.3389/fpsyg.2021.641806 [DOI] [PMC free article] [PubMed]
- Ren, Z., Xin, Y., Wang, Z., Liu, D., Ho, R. C. M., & Ho, C. S. H. (2021b). What factors are most closely associated with mood disorders in adolescents during the COVID-19 pandemic? A cross-sectional study based on 1,771 adolescents in Shandong Province, China. Frontiers in Psychiatry, 12. 10.3389/fpsyt.2021.728278 [DOI] [PMC free article] [PubMed]
- Renaud-Charest, O., Lui, L. M. W., Eskander, S., Ceban, F., Ho, R., di Vincenzo, J. D., Rosenblat, J. D., Lee, Y., Subramaniapillai, M., & McIntyre, R. S. (2021). Onset and frequency of depression in post-COVID-19 syndrome: A systematic review. In Journal of Psychiatric Research (vol. 144, pp. 129–137). Elsevier Ltd. 10.1016/j.jpsychires.2021.09.054 [DOI] [PMC free article] [PubMed]
- Rossi R, Socci V, Talevi D, Mensi S, Niolu C, Pacitti F, Di Marco A, Rossi A, Siracusano A, Di Lorenzo G. COVID-19 Pandemic and Lockdown Measures Impact on Mental Health Among the General Population in Italy. Frontiers in Psychiatry. 2020;11(August):7–12. doi: 10.3389/fpsyt.2020.00790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soh HL, Ho RC, Ho CS, Tam WW. Efficacy of digital cognitive behavioural therapy for insomnia: A meta-analysis of randomised controlled trials. Sleep Medicine. 2020;75:315–325. doi: 10.1016/j.sleep.2020.08.020. [DOI] [PubMed] [Google Scholar]
- Tandon, R. (2020). COVID-19 and mental health: preserving humanity, maintaining sanity, and promoting health. Asian journal of psychiatry,51, 102256. [DOI] [PMC free article] [PubMed]
- Tee ML, Tee CA, Anlacan JP, Aligam KJG, Reyes PWC, Kuruchittham V, Ho RC. Psychological impact of COVID-19 pandemic in the Philippines. Journal of Affective Disorders. 2020;277:379–391. doi: 10.1016/j.jad.2020.08.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tran, B. X., Nguyen, H. T., Le, H. T., Latkin, C. A., Pham, H. Q., Vu, L. G., Le, X. T. T., Nguyen, T. T., Pham, Q. T., Ta, N. T. K., Nguyen, Q. T., Ho, C. S. H., & Ho, R. C. M. (2020). Impact of COVID-19 on economic well-being and quality of life of the vietnamese during the national social distancing. Frontiers in Psychology, 11. 10.3389/fpsyg.2020.565153 [DOI] [PMC free article] [PubMed]
- Wang, C., Chudzicka-Czupała, A., Grabowski, D., Pan, R., Adamus, K., Wan, X., Hetnał, M., Tan, Y., Olszewska-Guizzo, A., Xu, L., McIntyre, R. S., Quek, J., Ho, R., & Ho, C. (2020a). The association between physical and mental health and face mask use during the COVID-19 pandemic: A comparison of two countries with different views and practices. Frontiers in Psychiatry, 11. 10.3389/fpsyt.2020.569981 [DOI] [PMC free article] [PubMed]
- Wang, C., Chudzicka-Czupała, A., Tee, M. L., Núñez, M. I. L., Tripp, C., Fardin, M. A., Habib, H. A., Tran, B. X., Adamus, K., Anlacan, J., García, M. E. A., Grabowski, D., Hussain, S., Hoang, M. T., Hetnał, M., Le, X. T., Ma, W., Pham, H. Q., Reyes, P. W. C., … Sears, S. F. (2021a). A chain mediation model on COVID-19 symptoms and mental health outcomes in Americans, Asians and Europeans. Scientific Reports, 11(1). 10.1038/s41598-021-85943-7 [DOI] [PMC free article] [PubMed]
- Wang, C., López-Núñez, M. I., Pan, R., Wan, X., Tan, Y., Xu, L., Choo, F., Ho, R., Ho, C., & Aparicio García, M. E. (2021b). The impact of the COVID-19 pandemic on physical and mental health in China and Spain: Cross-sectional study. JMIR Formative Research, 5(5). 10.2196/27818 [DOI] [PMC free article] [PubMed]
- Wang, C., Pan, R., Wan, X., Tan, Y., Xu, L., Ho, C. S., & Ho, R. C. (2020b). Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. International Journal of Environmental Research and Public Health, 17(5). 10.3390/ijerph17051729 [DOI] [PMC free article] [PubMed]
- Wang C, Pan R, Wan X, Tan Y, Xu L, McIntyre RS, Choo FN, Tran B, Ho R, Sharma VK, Ho C. A longitudinal study on the mental health of general population during the COVID-19 epidemic in China. Brain, Behavior, and Immunity. 2020;87:40–48. doi: 10.1016/j.bbi.2020.04.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang C, Tripp C, Sears SF, Xu L, Tan Y, Zhou D, Ma W, Xu Z, Chan NA, Ho C, Ho R. The impact of the COVID-19 pandemic on physical and mental health in the two largest economies in the world: A comparison between the United States and China. Journal of Behavioral Medicine. 2021;44(6):741–759. doi: 10.1007/s10865-021-00237-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiong, J., Lipsitz, O., Nasri, F., Lui, L. M. W., Gill, H., Phan, L., Chen-Li, D., Iacobucci, M., Ho, R., Majeed, A., & McIntyre, R. S. (2020). Impact of COVID-19 pandemic on mental health in the general population: A systematic review. In Journal of Affective Disorders (vol. 277, pp. 55–64). Elsevier B.V. 10.1016/j.jad.2020.08.001 [DOI] [PMC free article] [PubMed]
- Zhang, M. W. B., & Ho, R. C. M. (2017). Moodle: The cost effective solution for internet cognitive behavioral therapy (I-CBT) interventions. In Technology and Health Care (vol. 25, issue 1, pp. 163–165). IOS Press. 10.3233/THC-161261 [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data available on request for research purpose.