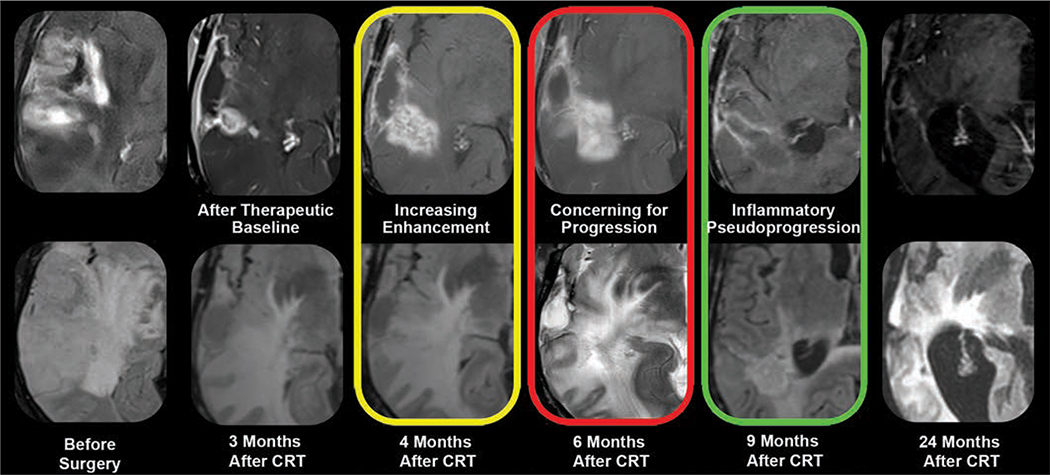
Fig. 5.
MRI appearance of glioblastoma neuroinflammatory pseudoprogression. Stupp protocol (chemoradiotherapy [CRT] and oral temozolomide) combined with fractionated external beam radiation therapy can induce neuroinflammation in patients with glioblastoma. Standard gadolinium-enhanced (top row) and T2-weighted/FLAIR (bottom row) morphologic MRI sequences, performed before and at multiple time points after CRT, are markedly limited for specifically defining therapy-induced neuroinflammatory changes. Both treatment failure and neuroinflammation manifest as enlarging enhancement and T2 hyperintensity (yellow, red). Unlike that of growing tumor, pseudoprogression enhancement spontaneously regresses and resolves without intervention (green). Retrospectively, this is diagnostic of neuroinflammation. However, response assessment in neurooncology criteria would not differentiate findings from those of growing tumor at height of inflammatory process (red), necessitating changes in therapy or biopsy. This exemplifies dilemma of monitoring pseudoprogression with gadolinium-based contrast agent, nonspecific biomarker of neurovascular unit integrity.