Abstract
Objective: The purpose of this study is to describe a population of individuals with chronic spinal cord injury (SCI), who underwent lower limb amputations, identify indications for amputations, medical co-morbidities and summarize resulting complications and functional changes.
Design: Retrospective observational cohort study.
Setting: SCI Service, Department of Veterans Affairs (VA) Health Care System.
Participants: Veterans with SCI of greater than one-year duration who underwent amputation at a VA Medical Center over a 15-year period, using patient registry and electronic health records. Diagnosis and procedure codes were utilized to identify amputations.
Interventions: Not applicable.
Outcome measures: Amputation level, complications, functional status, change in prescribed mobility equipment and mortality.
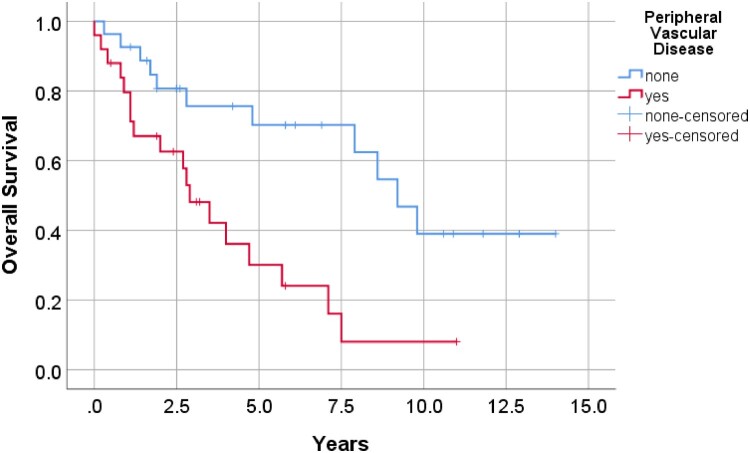
Results: 52 individuals with SCI received amputation surgery with a mean age of 62.9 years at time of amputation. Thirty-seven (71.2%) had paraplegia, and 34 (65.3%) had motor-complete SCI. Pressure injuries and osteomyelitis were most common indications for amputation. Amputations were primarily (83%) at the transtibial level or more proximal, with the most common amputation level at transfemoral/through-knee (29;55.8%). Postoperative complications occurred in five individuals. Seven of nine individuals who were ambulatory pre-surgery remained ambulatory. Equipment modifications were required in 37 (71%) of individuals. Five-year survival following amputations was 52%, and presence of peripheral vascular disease was significantly associated with mortality (P = 0.006).
Conclusions: Pressure injuries and osteomyelitis were most common etiologies for limb loss. Less than half experienced functional change after amputation; more than half required new or modified mobility equipment. An increase in mortality may reflect overall health deterioration over time.
Keywords: Spinal cord injuries, Amputation, Peripheral vascular disease
Introduction
Limb loss can occur at time of acute traumatic spinal cord injury (SCI), but it may also occur later as a consequence of secondary complications resulting from chronic SCI, such as pressure injuries, lower limb fracture, or osteomyelitis, Many individuals with SCI also have chronic health conditions that affect morbidity and mortality similar to the general population, including: diabetes, hypertension, coronary artery disease (CAD), peripheral vascular disease (PVD), and chronic renal disease. The presence of chronic wounds contributes to pain, loss of function, and negatively impacts quality of life. Further, in the setting of PVD and impaired sensation, chronic infection and osteomyelitis can lead to sepsis and death.
The prevalence of limb amputation in individuals with chronic SCI is approximately 4%, and amputation is associated with an increased risk of mortality.1,2 Limb amputations are often considered after trials of extensive wound care interventions and antibiotic use, surgical debridement, and vascular surgeries. Little information is available on the functional consequences of limb loss in individuals with SCI.
The purpose of this study was to describe clinical characteristics and outcomes of Veterans with chronic SCI who received lower limb amputation surgery, including the indications for surgery, medical co-morbidities and post-surgical complications, length of hospitalization, functional change and mortality. It was anticipated that amputation would have only a minor impact on mobility status at long-term follow-up, since the majority of individuals with SCI who undergo amputation were anticipated to be non-ambulatory at baseline.
Methods
Study design and participants
A locally maintained registry of individuals with traumatic or non-traumatic SCI who received care through the SCI Service at a VA Medical Center was used to identify the study population. Over a 15-year period, the registry contained approximately 1104 individuals with SCI, including 364 who expired during the record review time period (1/1/2000-12/31/2014). The population was restricted to individuals who received a discharge diagnosis code (International Classification of Disease; Ninth Revision (ICD-9) V49.70–V49.77) or a procedure code (84.1×) for lower limb amputation surgery, and further restricted to limb loss events that occurred more than one-year post SCI. If an individual received more than one amputation during the study period, only the most recent amputation was abstracted for inclusion in the primary analyses. For one individual who required revision to a more proximal amputation during the post-op period, the amputation level of the second surgery was recorded, and the individual was recorded as having experienced a post-up complication.
The medical records of the study population were reviewed by investigators. Individual demographical data collected included age at time of limb loss surgery, date and cause of death (if applicable), days from surgery to death or end of chart review interval, race, ethnicity, sex, date of SCI, and neurological classification for injury level and American Spinal Injury Association Impairment Scale (AIS) grade.3 Additional information collected included date of limb loss surgery, indications for surgery, level of amputation (grouping through-knee with transfemoral level), major post-operative complications, prior lower limb amputations, medical co-morbidities, living situation, level of independence for transfers as measured by the Functional Independence Measure (FIM), ambulatory status, length of hospitalization, type of residence upon discharge following surgery, and new or modified equipment prescribed, including prosthetic limbs.
Statistical analysis
Statistical analysis was performed using SPSS version 26 (SPSS Inc., Chicago, IL). A P-value <0.05 was set to indicate statistical significance. The Friedman test was used to assess for difference in transfer FIM sub-score across pre-surgery, discharge, and one-year post-surgery timepoints, with the Wilcoxon signed rank test used post-hoc to identify significant differences between pairs of timepoints. The Cox proportional hazards model was used to analyze factors potentially associated with survival as an exploratory analysis, as there was no a priori hypothesis that a specific comorbidity would be associated with survival. Individual medical comorbidities were selected as factors for inclusion in the model if on univariable analysis (Fisher’s exact test) they were associated with five-year survival at a significance of P<0.1, assessed on the subpopulation with at least 5 years of post-surgery follow-up. Age at time of surgery and neurological classifications (tetraplegia versus paraplegia; motor-complete versus motor-incomplete) were also included in the model since both are recognized to be strongly associated with survival. This study received approval by the institutional review board of the participating VA Medical Center.
Results
Fifty-two individuals with SCI underwent lower limb amputation over the course of 15 years (Table 1). Over this time period, these individuals received 58 amputation surgeries. The mean age at the time of amputation was 62.9 years (+/− 12.1 years standard deviation) and the mean duration of SCI was 17.1 years (+/− 13.5 years). All individuals were male, and the majority (80.8%) were white. Thirty-seven (71.2%) of individuals had paraplegia, and 34 (65.3%) had motor-complete SCI AIS A or B. Common comorbidities included hypertension (61.5%), active tobacco use (61.5%) chronic wounds (57.7%), PVD (48.1%; all were classified as peripheral arterial disease), and diabetes mellitus (42.3%). For the 10 comorbidity categories reviewed, the median number present per individual was four. Twenty-one (40.4%) individuals had ever undergone prior lower limb amputation surgery.
Table 1. Demographics for 52 study individuals.
| Years (SD) | ||
|---|---|---|
| Mean age at time of surgery | 62.9 (+/− 12.1) | |
| Mean injury duration | 17.1 (+/−13.5) | |
| n | Percent | |
| Sex | ||
| Male | 52 | 100 |
| Race | ||
| White | 42 | 80.8 |
| African American | 2 | 3.8 |
| Other or unknown | 8 | 15.4 |
| Ethnicity | ||
| Non-Hispanic | 44 | 84.6 |
| Unknown | 8 | 15.4 |
| Comorbidities | ||
| Smoking | 32 | 61.5 |
| Hypertension | 32 | 61.5 |
| Chronic wounds | 30 | 57.7 |
| PVD | 25 | 48.1 |
| Diabetes mellitus | 22 | 42.3 |
| CAD/CHF | 18 | 34.6 |
| Dyslipidemia | 16 | 30.8 |
| Chronic renal disease | 11 | 21.2 |
| CVA | 8 | 15.4 |
| Peripheral neuropathy | 6 | 11.5 |
| Prior lower limb amputations | ||
| Hip disarticulation | 3 | 5.8 |
| Transfemoral or through knee | 12 | 23.1 |
| Transtibial | 2 | 3.5 |
| Foot or ankle | 6 | 11.5 |
| Any prior lower limb amputation | 21 | 40.4 |
| Any prior ipsilateral amputation | 7 | 13.5 |
| Living Situation prior to Surgery | ||
| Private residence; independent | 18 | 34.6 |
| Private residence; receiving assistance | 30 | 57.7 |
| Adult family home | 1 | 1.9 |
| Skilled nursing facility | 3 | 5.8 |
SD: standard deviation; PVD-peripheral vascular disease, CAD-coronary artery disease, CHF-congestive heart failure, CVA-cerebrovascular accident.
Indications for surgery and the levels of amputation performed are shown in Table 2. Lower limb wounds, including pressure injuries, were an indication for surgery in 59.6%, and 53.8% had osteomyelitis. The most common amputation surgery levels were trans-femoral (55.8%), followed by ankle/foot/toes (17.3%) and transtibial (15.4%). Each of the six individuals (11.5%) who received hip disarticulation had large pelvic region pressure injuries. For three of these six individuals, proximal amputation was required due lack of options for local flap surgeries due to prior flap surgeries in the same region. The remaining three individuals who received hip disarticulations had these additional indications: severe hip and knee contracture; acute proximal femur fracture with gross contamination of fracture site from a chronic ischial pressure injury; severe PVD with low likelihood of healing a more distal amputation level.
Table 2. Indications for surgery and level of amputation.
| Indications for amputation | n | Percent |
|---|---|---|
| Chronic lower limb or pelvic wound, including pressure injury | 31 | 59.6 |
| Osteomyelitis | 28 | 53.8 |
| PVD | 13 | 25.0 |
| Lower limb fracture | 6 | 11.5 |
| Acute infection/sepsis | 5 | 9.6 |
| Pain | 2 | 3.8 |
| Contractures | 1 | 1.9 |
| Level of amputation | ||
| Hip disarticulation | 6 | 11.5 |
| Transfemoral or through the knee | 29 | 55.4 |
| Transtibial | 8 | 15.4 |
| Foot | 9 | 17.3 |
PVD: Peripheral vascular disease.
Note: Some individuals had more than one indication for amputation.
Five of 52 individuals (9.6%) experienced significant post-op complications. Two individuals developed wound dehiscence and delayed healing, and one had a pulmonary embolism 10 days post-surgery. One individual experienced a gastrointestinal bleed and myocardial infarction. One individual had post-operative limb ischemia necessitating conversion from a transtibial to transfemoral amputation two months later. Mean length of stay after surgery was 56.6 days (+/− 7.8 days), and the mean total length of stay was 105 days (+/− 16 days). Each individual was able to discharge to their pre-hospital residence, which for 48 of 52 individuals (92.3%) was a private residence.
Nine of 52 individuals (17%) ambulated for at least short household distances with assistive devices (lower limb orthoses and or upper limb mobility aids) prior to amputation. The amputation levels for the nine ambulatory individuals were transtibial for five and more distal for four individuals. Seven of nine individuals regained the ability to ambulate at least short distances using assistive devices, including three of the five ambulatory individuals who received transtibial amputation. Data on functional status for transfers at pre-surgery, discharge, and one-year post-amputation timepoints were available for 43 of the 52 individuals. For these individuals, independence for transfers as measured by the FIM transfer sub-score differed significantly across the 3 timepoints (P = 0.003; Friedman test). The score declined significantly from pre-surgery baseline to time of discharge, did not differ significantly between discharge and one-year post-surgery, and was significantly lower than baseline at one-year post-surgery (P = 0.008; P = 0.92; and P = 0.004, respectively; Wilcoxon signed ranks test). For these 43 individuals, the percentage requiring assistance for transfers increased from 19% (8 of 43) pre-surgery to 37% (16 of 43) at discharge and 33% (14 of 43) one year following surgery. Across the entire study population there were 11 individuals who developed a new requirement for transfer assistance at discharge, 10 of whom had paraplegia and nine with motor-complete injuries. All individuals with a new requirement for assisted transfers at discharge had received amputation at the transfemoral or hip level.
Equipment changes or modifications were required by 37 of 52 (71%) individuals. Fourteen individuals required a new or modified wheelchair cushion or backrest, eight required some type of wheelchair modification (installation of anti-tips, seat modification, or addition of weights), and four required prescription of new wheelchairs (two power, two manual). Seven individuals were prescribed prosthetic limbs (three for functional reasons, four for cosmetic reasons), four were prescribed lower limb orthotics, and two were prescribed new upper limb assistive devices. Nine individuals were prescribed a lift for transfers, and three individuals required additional bathroom equipment.
Survival rates at one, two and five-years post-amputation were 86%, 74%, and 52%, respectively. All individuals survived until hospital discharge. One individual died 10 days after surgery (nine days after hospital discharge) due to pulmonary embolism. He had undergone amputation of the left third, fourth, and fifth digits of his foot. Univariable analysis (Fisher’s exact test) of comorbidities for the 40 individuals whose surgery had occurred at least five years earlier showed the following factors to be associated with 5-year survival at a P value of 0.1 or greater: PVD (P = 0.025) and diabetes (P = 0.004). None of the following factors were associated with 5-year survival on univariable analysis: CAD (P = .332), dyslipidemia (P = .315), renal disease (P = .318), stroke (P = .427), hypertension (P = 1.0), neuropathy (P = .114), chronic wounds (P = 0.200), and smoking (P = 0.517). Survival analysis using Cox regression demonstrated that mortality was significantly associated with presence of PVD (P = 0.006) but not significantly associated with age (P = 0.61), tetraplegia versus paraplegia (P = 0.15), motor-complete versus motor-incomplete (P = 0.42), or presence of diabetes (P = 0.15) (Table 3). The overall model P value was 0.009. Survival at five years post-amputation (Figure 1) was approximately 30% in those with PVD versus 70% in those without PVD.
Table 3. Cox proportional hazards model for mortality following amputation surgery.
| Risk Factor | Regression Coefficient | P value | Hazard Ratio | 95% confidence interval for Hazard Ratio |
|---|---|---|---|---|
| PVD | 1.156 | 0.005 | 3.179 | 1.409-7.171 |
| Diabetes | 0.580 | 0.148 | 1.786 | 0.815-3.917 |
| Age, years | 0.009 | 0.605 | 1.009 | 0.975-1.045 |
| Tetraplegia | 0.774 | 0.149 | 2.168 | 0.758-6.198 |
| Motor-complete | −0.425 | 0.418 | 0.654 | 0.234-1.827 |
PVD: Peripheral vascular disease.
Figure 1.
Kaplan–Meier curves demonstrating survival in individuals with versus without PVD. Presence of PVD was significantly associated with mortality (P = 0.006).
Discussion
Individuals with chronic SCI frequently experience pressures injuries, osteomyelitis, fractures, and PVD impacting the lower limbs, which can lead to amputation.4–7 PVD with lower limb gangrene has been reported as an indication for amputation.6 Amputation is performed for 1.3% of lower limb fractures in individuals with chronic SCI.7 Case reports primarily document proximal limb amputation in individuals with chronic pelvic region wounds,8–10 and in this study 11.5% of amputations were hip disarticulations for management of pelvic region wounds. In a large cohort of individuals with chronic SCI, the estimated prevalence of amputation was 4%.1 The present study was not designed to determine the incidence rate for amputation surgery, since individuals followed at the center may have received amputation at a different hospital that would not have been included in this study. However, based on occurrence of 48 amputation surgeries at or proximal to the transtibial level over 15 years in the dynamic cohort that averaged 660 individuals, the minimum incidence rate for lower limb amputations in this population would be 0.48 per 100 individuals.
The most common level of amputation was transfemoral or though the knee, despite wounds frequently located at the foot. This is in contrast to common practice in individuals without SCI who require amputation, where longer limb length is often desired due to increased levels of energy expenditure with higher levels of amputation.1 It is believed that higher level amputation was performed in individuals with SCI as a residual limb below the level of the knee may be fraught with long-term challenges, such as pronounced knee flexion contracture leading to seating and positioning challenges, wound healing challenges with edema at a residual limb with the knee in a flexed position, and limitations in fitting a prosthetic limb, which may be used for cosmesis, if not for ambulation. When considering exact location along the femur for above the knee amputation, a long residual femoral limb is often preferred, in order to maximize weight distribution throughout the existing limb to minimize the risk of pressure injury and to maintain balance in the seated position.
Amputations are associated with excess mortality in the SCI population,1,2,12 but little research has been conducted to describe clinical characteristics and outcomes in individuals with SCI who receive amputation surgery. As reported by others,13–15 an amputation performed on individuals with SCI did not necessarily lead to loss of ambulatory ability. For individuals who did experience functional loss following surgery, it is possible that they were dependent on the limb for transfers and the amputation directly impacted their function. Alternatively, individuals may have been offered home care resources during the peri-operative period, of which they were unaware prior to surgery; while they were able to perform the activities independently before surgery, additional support may facilitate efficiency in the activity, and therefore benefitting from caregiver assistance.
Most individuals (71%) required equipment changes or modifications following amputation. This underscores the importance of interdisciplinary collaboration and completing a functional reassessment in all individuals after surgery. Balance, positioning, and transfer techniques may be altered following the removal of a limb. Additionally, seating on all types of surfaces (wheelchair, commode, bathing) may need to be adjusted to maximize comfort, function, and safety.16 For example, the rear axle of a manual wheelchair may need to be moved to a more posterior position to prevent rearward tipping resulting from alteration in seated center of mass post-amputation. The reported changes in functional abilities and equipment needs underscores the importance of involving physical and occupational therapy post-surgery to thoroughly address rehabilitation needs.
Four individuals elected to have a cosmetic prosthetic limb fabricated. In the past, some advocated for the amputation of “useless limbs”, arguing that the procedure reduced body weight, thereby facilitated transfers to and from wheelchair, and prevented the development of pressure injuries at the ankles and knees.17 Providers are encouraged to recognize the psychosocial impact of additional injury and disability and the value of body image in individuals with SCI experiencing limb loss. A cosmetic limb, while not used for ambulation, may offer a sense of body “wholeness” to some individuals.6 It is important to ensure the proper fit of a cosmetic limb even in the absence of functional mobility and transfers due to neurogenic skin and wound prevention.
Five years post-amputation, mortality in this population was 48%. This is consistent with a population-based study of mortality risk after SCI by Krause et al.,1,2 showing lower limb amputation to have a hazard ratio of 1.73. In our study, mortality was significantly associated with presence of PVD, and five-year survival in those without PVD was approximately 70%.
Clinical implications of the results reflect the need to emphasize the role of preventive health measures as key to the care of individuals with SCI. The prevention of pressure injuries and onset of osteomyelitis is critical in reducing the need for amputations. This highlights the importance of follow-up visits in seating clinics for management of pelvic anomalies and prescription of appropriate wheelchairs and seating surfaces, wound care clinics for aggressive wound management, and education of individuals and their caregivers on the need for frequent skin checks and for pressure relief. Prevention and management of risk factors for PVD should also be addressed. Counseling and comprehensive support programs for smoking cessation, dietary and nutrition management and comprehensive wellness programs in conjunction with the primary care provider should be part of integrated care for these individuals. Evaluation by the rehabilitation team and access to new or modified mobility equipment to support functional changes after limb loss will allow individuals with SCI to continue to maximize functional abilities and minimize complications, short and long-term.
Study limitations
There are several limitations to the study. Amputation surgeries were identified by retrospective review of administrative data. Amputation surgeries provided in other settings without admission to the study center were not captured by the chart review; therefore, the true incidence rate of amputation surgery in this individual cohort cannot be calculated. The review of postoperative complications was limited to major postoperative complications and excludes minor ones such as urinary tract infections. The impact of amputation on pain disorders including phantom pain, overuse syndromes, and mood disorders was not determined. Due to the high prevalence of chronic pain, overuse syndromes, and mood disorders in individuals with SCI, differentiating new versus old symptoms would require prospective assessment. Length of stay was dependent on post-operative recovery and medical comorbidities, but it also encompasses time needed to address rehabilitation goals and psychosocial factors that may have delayed discharge from a VA setting. The study population was limited to a cohort of Veterans with SCI who received amputation surgery at a single VA Medical Center, were all male, and were older and had longer duration of injury than in prior population-based research on this topic.1
Conclusions
Lower limb amputation in the setting of chronic SCI is often the result of pressure injuries and osteomyelitis. Following surgery, individuals benefit from comprehensive reassessment of equipment and functional abilities. An increase in mortality may reflect overall health deterioration over time.
Disclaimer statements
Contributors None.
Funding The authors report no financial support received for this research.
Conflicts of interest The authors report no conflict of interest.
Acknowledgement
This material is the result of work supported with resources and the use of facilities at VA Puget Sound Health Care System. The contents do not represent the views of the United States Department of Veterans Affairs.
References
- 1.Krause JS, Carter RE, Pickelsimer EE, Wilson D.. A prospective study of health and risk of mortality after spinal cord injury. Arch Phys Med Rehabil. 2008 Aug;89(8):1482–91. doi: 10.1016/j.apmr.2007.11.062. PMID:18674984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Krause JS, Cao Y, Clark JMR.. Pain Intensity, interference, and medication use after spinal cord injury: association with risk of mortality after controlling for socioeconomic and other health factors. Arch Phys Med Rehabil. 2017 Dec;98(12):2464–2470. doi: 10.1016/j.apmr.2017.05.024. Epub 2017 Jun 23. PMID: 28652067. [DOI] [PubMed] [Google Scholar]
- 3.Kirshblum SC, Burns SP, Biering-Sorensen F, Donovan W, Graves DE, Jha A, et al. . International standards for neurological classification of spinal cord injury (revised 2011). J Spinal Cord Med 2011 Nov;34(6):535–46. doi: 10.1179/204577211X13207446293695 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pressure ulcer prevention and treatment following spinal cord injury: a clinical practice guideline for health-care professionals. Consortium for Spinal Cord Medicine Clinical Practice Guidelines. J Spinal Cord Med. Spring 2001;24 Suppl 1:S40–101. [DOI] [PubMed] [Google Scholar]
- 5.Su TW, Chou TY, Jou HJ, Yang PY, Lin CL, Sung FC, et al. . Peripheral arterial disease and spinal cord injury: A retrospective nationwide cohort study. Medicine (Baltimore). 2015 Oct;94(41):e1655. doi: 10.1097/MD.0000000000001655 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Grundy DJ, Silver JR.. Amputation for peripheral vascular disease in the paraplegia and tetraplegic. Paraplegia 1983;21:305–11. [DOI] [PubMed] [Google Scholar]
- 7.Bethel M, Bailey L, Weaver F, Le B, Burns SP, Svircev JN, et al. . Surgical compared with nonsurgical management of fractures in male veterans with chronic spinal cord injury. Spinal Cord 2015 May;53(5):402–14. doi: 10.1038/sc.2015.5 [DOI] [PubMed] [Google Scholar]
- 8.Yusmido YA, Hisamud-Din N, Mazlan M.. Elective proximal lower limb amputation in spinal cord injury patients with chronic pressure ulcers: improve quality of life, function, and shorten hospital stay. Case report. Eur J Phys Rehabil Med 2014 Oct;50(5):557–60. Epub 2014 Apr 3. PubMed PMID: 24694951. [PubMed] [Google Scholar]
- 9.Correa G, Calderón W, Roa R, Guzman LM, Burnier LA, Danilla SE.. Proximal amputation of inferior extremity secondary to recurrent pressure ulcers in patients with spinal cord injuries. Spinal Cord 2008;46:135–139. doi: 10.1038/sj.sc.3102089 [DOI] [PubMed] [Google Scholar]
- 10.Shields RK, Dudley-Javoroski S.. Musculoskeletal deterioration and hemicorporectomy after spinal cord injury. Phys Ther 2003;83(3):263–75. doi: 10.1093/ptj/83.3.263 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Molina CS, Faulk JB.. Lower limb amputation. StatPearls [Internet]. Treasure Island (FL: ): StatPearls Publishing; 2020–2019 Aug 24. [Google Scholar]
- 12.Cao Y., Krause J., DiPiro N.. Risk factors for mortality after spinal cord injury in the USA. Spinal Cord 51, 413–18 (2013). doi: 10.1038/sc.2013.2. [DOI] [PubMed] [Google Scholar]
- 13.Senthilvelkumar T, Chandy BR.. Paraplegia and transtibial amputation: successful ambulation after dual disability: a retrospective case report. Spinal Cord Ser Cases 2017 Feb 2;3:16039. doi: 10.1038/scsandc.2016.39. eCollection 2017. PubMed PMID: 28382211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mustafah NM, Bakar NA, Yang CT.. Prosthetic restoration in patient within complete spinal cord injury. Spinal Cord Ser Cases 2016 Jan 7;2:15031. doi: 10.1038/scsandc.2015.31. eCollection 2016. Erratum in: Spinal Cord Ser Cases. 2016 Jul 21;2:16019. PubMed PMID: 28053733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wang F, Hong Y.. Case series of 6 patients with amputation at or around time of SCI: rehabilitation for patients with paraplegia and lower extremity amputation. J Phys Ther Sci. 2015 Oct;27(10):3049–51. doi: 10.1589/jpts.27.3049. Epub 2015 Oct 30. PubMed PMID: 26644641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Preservation of Upper Limb Function Following Spinal Cord Injury: A Clinical Practice Guideline for Health-Care Professionals. J Spinal Cord Med 2005;28:434–70. [DOI] [PMC free article] [PubMed]
- 17.Ohry A, Heim M, Steinbach TV, Rozin R.. The needs and unique problems facing spinal cord injured persons after limb amputation. Paraplegia 1983;21:260–263. [DOI] [PubMed] [Google Scholar]