SUMMARY
Only a few studies have assessed smell and taste in Coronavirus Disease 2019 (COVID-19) patients with psychophysical tests, while the majority performed self-rating evaluations. Given the heterogeneity of the published literature, the aim of this review was to systematically analyse the articles on this topic with a focus on psychophysical testing. A search on PubMed and Web of Science from December 2019, to November 2021, with cross-references, was executed. The main eligibility criteria were English-language articles, investigating the clinical features of olfaction and gustation in COVID-19 patients using self-rating assessment, psychophysical testing and imaging techniques. A total of 638 articles were identified and 66 were included. Self-rating assessment was performed in 31 studies, while psychophysical testing in 30 and imaging techniques in 5. The prevalence of chemosensory dysfunction was the most investigated topic, followed by the recovery time. About the psychophysical assessment, the extended version of the Sniffin’ Sticks was used in 11 articles and the Connecticut Chemosensory Clinical Research Center test in another 11. The olfactory threshold performance was the most impacted compared to the discrimination and identification capacities in accordance with the hypothesis of a tropism of SARS-CoV-2 for the olfactory mucosa. The timing significantly influenced the results of the psychophysical testing with 20% of patients presenting olfactory dysfunction at one month after infection.
KEY WORDS: smell, olfaction disorders, taste, anosmia, rhinology, COVID-19, infections
RIASSUNTO
La maggioranza degli studi ha valutato la capacità olfattiva e gustativa nei pazienti COVID-19 con questionari e autovalutazione. Data l’eterogeneità della letteratura pubblicata, lo scopo di questa ‘review’ è stato quello di analizzare gli articoli sull’argomento, focalizzando l’attenzione sui test psicofisici. È stata eseguita una ricerca su PubMed e Web of Science da dicembre 2019 a novembre 2021. I principali criteri di inclusione sono stati articoli in lingua inglese, che studiavano le caratteristiche cliniche dell’olfatto e del gusto nei pazienti COVID-19 utilizzando test soggettivi, psicofisici e ‘imaging’ radiologico. In totale sono stati identificati 638 articoli e di questi ne sono stati inclusi 66. In 31 studi è stata eseguita una valutazione soggettiva, mentre in 30 sono stati utilizzati test psicofisici e in 5 tecniche di ‘imaging’ radiologico. La prevalenza della disfunzione chemosensoriale è stata l’argomento più studiato, seguita dal tempo di recupero. Per quanto riguarda la valutazione psicofisica, gli Sniffin’ Sticks sono stati utilizzati in 11 articoli e il test del Connecticut Chemosensory Clinical Research Center in altri 11. La performance della soglia olfattiva è stata la più intaccata rispetto alle capacità di discriminazione e identificazione in linea con l’ipotesi di un tropismo del virus COVID-19 per la mucosa olfattoria. La tempistica ha influenzato significativamente i risultati del test psicofisico con solo il 20% dei pazienti affetti da disfunzione olfattiva dopo un mese dall’infezione.
PAROLE CHIAVE: olfatto, disturbi olfattivi, gusto, anosmia, COVID-19, infezioni
Introduction
Chemosensory dysfunction due to upper respiratory tract infection (URTI) can be caused by many common cold viruses, namely rhinovirus, adenovirus, influenza virus and coronavirus, including Coronavirus Disease 2019 (COVID-19), firstly detected in December 2019 in Central China, in the city of Wuhan 1. After China, Italy was the first European country to experience a large-scale outbreak in February 2020 with 4,757,231 confirmed cases and 132,004 deaths as of October 2021 according to the World Health Organization (WHO). Since the beginning of this pandemic, otolaryngologists have had a key role in the treatment of many symptoms of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection, such as fever, cough, sore throat and smell and taste disorders, which suddenly became known to everyone thanks to media attention and massive release of publications about this topic 2. However, quantity does not always imply quality, and COVID-19 articles in the field of otolaryngology have been often related to poorer evidence levels than non-COVID-19 and pre-COVID-19 articles 3,4. This is even truer in the case of publications about smell and taste dysfunction which were often based on subjective findings 5 and case reports/small case series 6, with most of the studies using self-administered tests or screening tests of olfactory function, especially in the first wave of pandemic because of the cancellation of hospital visits and elective procedures 7. Conversely, only a few studies have evaluated smell and taste in COVID-19 patients with psychophysical tests 8,9.
Given the high heterogeneity of the published literature and the increasing interest in olfaction and taste before, during and after SARS-CoV-2 infection, the aim of this review was to systematically analyse the articles on this topic with a focus on publications where smell and taste in COVID-19 patients has been assessed with psychophysical tests.
Materials and methods
This systematic review was conceived according to the Primary Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) Guidelines 10,11.
Search strategy and article selection process
The National Library of Medicine through PubMed and Web of Science were searched for the following keywords: “Smell” OR “Olfaction” OR “Taste” OR “Gustation” OR “Olfaction disorders” OR “Anosmia” OR “Rhinology” AND “COVID-19” OR “SARS-CoV-2 infection”. The first author collected articles published between December 2019, and November 2021. Also, references of the collected articles were considered potentially eligible for this systematic review, as well as records identified through websites and other organizations.
The main eligibility criteria were English-language articles, randomised and controlled trials in humans investigating the clinical features of olfaction and gustation in COVID-19 patients using self-rating assessment, psychophysical testing and/or imaging techniques. Articles using psychophysical tests of any type (i.e., Sniffin’ Sticks extended test, 16-item Sniffin’ Sticks identification test, Connecticut Chemosensory Clinical Research Center - CCCRC, University of Pennsylvania Smell Identification Test - UPSIT) and quality, including validated screening tests, were assessed for eligibility. Literature reviews, technical notes, letters to the editor, case reports, case series or trials including less than 12 participants, instructional courses and conference papers were excluded from this systematic review. Papers not focusing on smell and taste in COVID-19 patients, and where the methodology was inconsistent, were also excluded.
Data extraction and quality assessment
Two authors (E.M.C.T., M.C.) independently screened the full-text version of each publication, conducted data extraction and excluded those whose content was judged not to be relevant for the purpose of this review. When agreement could not be reached, another author from the group (M.G.) was consulted, and another (F.L.) was asked for data extraction and quality assessment.
Publications were classified according to the olfactory/gustatory assessment in self-rating evaluation, psychophysical testing, and imaging techniques. Articles where psychophysical testing was used were further analysed according to the threshold, discrimination and identification olfactory performance.
Among these three groups, topics of interest, such as recovery from chemosensory dysfunction, treatment outcomes and recovery time, were identified.
The general features of each article (i.e., journal, first author, country, year of publication, population, methods, prevalence, topic of the paper, and study quality) were recorded in a spreadsheet. The quality of the included studies was assessed using “The Strengthening the Reporting of Observational Studies in Epidemiology” (STROBE) Statement with a score interval from 0 to 22, with a higher score indicating a better study quality 12. To mitigate the risks of bias, papers of all quality were included in this systematic review.
Results
Seventy-eight articles were identified through other methods (i.e., websites, organisations, citation searching), and 1018 via databases (i.e., PubMed, Web of Science). After excluding duplicates, 638 articles were considered potentially eligible for screening. Out of these, 72 publications were not retrieved and 500 were eliminated for the following reasons (Fig. 1): written in languages other than English (n = 41); other than original articles (i.e., reviews, editorials, case reports etc.: n = 280); not being directly relevant to the topic (n = 68) and methodology inconsistent (n = 111). After these exclusions, 66 papers were included for final analysis.
Figure 1.
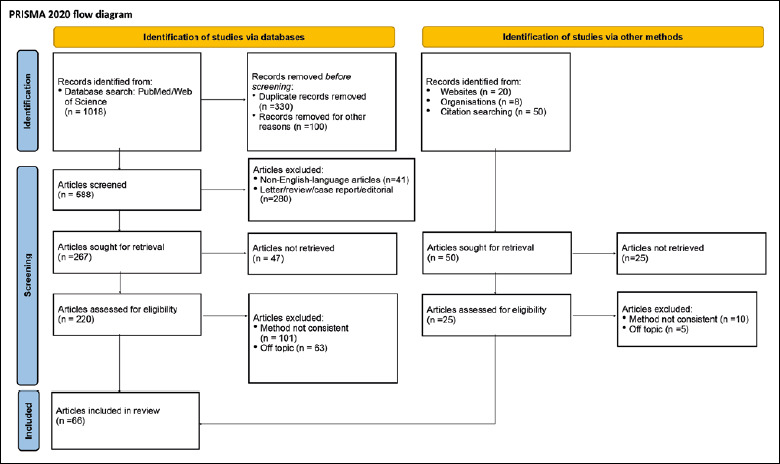
PRISMA (Primary Reporting Items for Systematic Reviews and Meta-analyses) flow diagram.
Regarding the olfactory/gustatory testing used, self-rating assessment was used in 31 studies 13-42 (Tab. I), and psychophysical testing in 30 9,43-70 (Tab. II). Lastly, imaging techniques were used in 5 articles 71-75 (Tab. III).
Table I.
Features of the studies using self-rating assessment.
| Source | Year | Country | Study population | Methods | Prevalence | Recovery time | Topic | STROBE score* | |
|---|---|---|---|---|---|---|---|---|---|
| 1 | Altundag A 13 | 2021 | Turkey, USA | 135 COVID-19 patients | Structured questionnaire | OD: 59.3%; Mean recovery: 7.8 days | N/A | Prevalence and recovery of chemosensory dysfunction | 20 |
| 2 | Bagheri SH 14 | 2020 | Iran | 10 069 COVID-19 patients | Structured questionnaire | OD: anosmia 60.9%, 80.4% combined dysfunction | N/A | Prevalence of chemosensory dysfunction | 20 |
| 3 | Barillari MR 15 | 2020 | Italy | 294 COVID-19 patients | Validated questionnaires | OD: 70.4%; GD: 59.2% | N/A | Prevalence of chemosensory dysfunction | 21 |
| 4 | Boscolo Rizzo P 16 | 2021 | Multicentric | 268 COVID-19 patients | Validated questionnaires | Combined chemosensory dysfunction: 81.3%; OD: 10.2%; GD 8.6% | N/A | Prevalence of chemosensory dysfunction | 22 |
| 5 | Boscolo-Rizzo P 18 | 2020 | Italy, UK | 187 COVID-19 patients | Validated questionnaires | Baseline: - OD or GD: 60.4%; 4 weeks: - complete resolution or improvement: 89% | N/A | Prevalence of chemosensory dysfunction and recovery time | 21 |
| 6 | Boscolo-Rizzo P 17 | 2020 | Italy | 296 household contacts of home-isolated COVID-19 patients | Structured questionnaire | OD or GD: 25% | N/A | Prevalence of chemosensory dysfunction | 21 |
| 7 | Chapurin N 19 | 2021 | USA | 1003 COVID-19 patients | Validated questionnaires | OD and GD: 73% | 19.7 days | Prevalence of chemosensory dysfunction | 20 |
| 8 | Chiesa-Estomba CM 20 | 2020 | Multicentric | 751 COVID-19 patients | Validated questionnaires | OD: 82.7%; anosmia 83%, hyposmia 17% | N/A | Prevalence and recovery of chemosensory dysfunction | 22 |
| 9 | Cho RHW 21 | 2020 | Hong Kong | 83 COVID-19 patients; 60 controls | Structured questionnaire | OD: 47%; GD: 43.4% | OD: 10.3 days; GD: 9.5 days | Correlation between olfactory dysfunction and viral load | 22 |
| 10 | Gerkin RC 22 | 2021 | Multicentric | 4148 COVID-19 patients | Validated questionnaires; VAS | N/A | N/A | Predictive value of olfactory loss in COVID-19 | 22 |
| 11 | Gorzkowski V 23 | 2020 | France | 229 COVID-19 patients | Structured questionnaire | OD: 70.3% | 11.6 days | Prevalence of chemosensory dysfunction and recovery time | 22 |
| 12 | Haehner A 24 | 2020 | Germany | 500 patients suspected for COVID-19: 34 confirmed cases | Structured questionnaire; VAS for OD/GD | Smell and/or taste loss: 13.8% | N/A | Predictive value of olfactory loss in COVID-19 | 19 |
| 13 | Hopkins C 25 | 2021 | Multicentric | 434 responders; 114 COVID-19 patients | Structured questionnaire | 6 months: 40.9% patients normosmic; 97.2% normogeusic | N/A | Prevalence of chemosensory dysfunction | 20 |
| 14 | Iravani B 26 | 2020 | Multicentric | 2440 patients | Data collection website smelltracker.org | Relationship between the COVID-19 prediction model and odour intensity ratings over time, ρ = -0.83, P < 0.001 | N/A | Predictive value of olfactory loss in COVID-19 | 21 |
| 15 | Jalessi M 27 | 2021 | Iran, UK | 243 COVID-19 patients | Validated questionnaires | OD: 88.5% anosmia at the onset. | N/A | Prevalence of chemosensory dysfunction | 20 |
| 16 | Konstantinidis I 28 | 2020 | Greece | 79 COVID-19 patients | VAS; olfactory and gustatory home test | OD: 36.7%; GD: 27.8% | N/A | Prevalence of chemosensory dysfunction | 22 |
| 17 | Lal P 83 | 2021 | India | 435 COVID-19 patients | Structured questionnaire | OD and/or GD: 10.8% | - OD 12.1 days; - GD 10.8 days | Recovery time | 15 |
| 18 | Lechien JR 29 | 2020 | Multicentric | 417 COVID-19 patients | Validated questionnaires | OD: 85.6%. GD: 88.0% | N/A | Prevalence of chemosensory dysfunction | 21 |
| 19 | Lechien JR 32 | 2021 | Multicentric | 2581 COVID-19 patients | Validated questionnaires; Sniffin’ sticks identification test (233 patients) | OD: 85.9% (mild forms) moderate-to-critical forms (4.5-6.9%). Psychophysical testing: 54.7% hyposmia/anosmia | - OD 21.6 days | Prevalence and recovery of chemosensory dysfunction | 20 |
| 20 | Lechien JR 31 | 2021 | Multicentric | 2579 COVID-19 patients | Validated questionnaires; Sniffin’ sticks identification test (231 patients) | OD: 73.7%. GD: 46.8%. Psychophysical testing: 23.5% anosmia; 18.6% hyposmia | N/A | Prevalence of chemosensory dysfunction | 20 |
| 21 | Lechien JR 30 | 2020 | Multicentric European | 1420 COVID-19 patients | Validated questionnaires | OD: 70.2%; GD: 54.2% | N/A | Prevalence of chemosensory dysfunction | 20 |
| 22 | Locatello LG 33 | 2021 | Italy | 101 COVID-19 patients | Validated questionnaires | Chemosensory dysfunction; - One month: 44%; -Three months: 37% | N/A | Treatment outcomes | 21 |
| 23 | Lucidi D 34 | 2020 | Italy | 110 COVID-19 patients | Validated questionnaires | N/A | Complete recovery: 7-14 days in 63% patients. Partial recovery: 1-3 months in 22% patients | Prevalence of chemosensory dysfunction | 20 |
| 24 | Maiorano E 35 | 2021 | Italy | 170 COVID-19 patients | Structured questionnaire; VAS for OD/GD | OD and GD: 96% | N/A | Prevalence of chemosensory dysfunction | 19 |
| 25 | Paderno A 36 | 2020 | Italy | 508 COVID-19 patients | Structured questionnaire | OD: 56%; GD: 63% | N/A | Prevalence of chemosensory dysfunction | 22 |
| 26 | Parma V 37 | 2020 | Multicentric | 4039 COVID-19 patients | Validated questionnaires | Mean reduction of smell: -79.7%; taste: -69.0%; chemestetic: -37.3% | N/A | Prevalence of chemosensory dysfunction | 22 |
| 27 | Qiu C 38 | 2020 | Multicentric | 394 COVID-19 patients | Validated questionnaires, VAS | Olfactory and/or gustatory dysfunction: 41% | N/A | Prevalence of chemosensory dysfunction | 22 |
| 28 | Raad N 39 | 2021 | Iran | 1299 COVID-19 patients | Validated questionnaires | Parosmia: 10.8% | N/A | Prevalence of parosmia | 20 |
| 29 | Spinato G 40 | 2021 | Italy | 230 COVID-19 patients; 230 controls | Validated questionnaires | N/A | N/A | Validation of a questionnaire | 21 |
| 30 | Vaira LA 41 | 2021 | Multicentric | 153 COVID-19 patients after vaccination | Validated questionnaires | OD: 62.3%. GD: 53.6% | N/A | Prevalence of chemosensory dysfunction in COVID-19 cases after vaccination | 21 |
| 31 | Yan CH 42 | 2020 | USA | 128 COVID-19 patients | Structured questionnaire | OD: -hospitalized 26.9%, outpatients 66.7%; GD: -hospitalized 23.1%, outpatients 62.7% | N/A | Predictive value of olfactory loss in COVID-19 | 19 |
OD: indicates olfactory dysfunction; GD: gustatory dysfunction; N/A: not applicable; VAS: visual analogue scale.
* Scores interval from 0 to 22, with higher scores showing better study quality 12.
Table II.
Features of the studies using psychophysical testing.
| Source | Year | Country | Study population | Methods | Prevalence | Recovery time | Topic | STROBE score* | |
|---|---|---|---|---|---|---|---|---|---|
| 1 | Amadu AM 43 | 2021 | Multicentric | 46 COVID-19 patients | CCCRC | OD: 76.1%; anosmia 26.1%, severe hyposmia 21.7%, moderate hyposmia 28.3% | N/A | Correlation between olfactory dysfunction and lung involvement | 21 |
| 2 | Bordin A 44 | 2021 | Italy | 101 COVID-19 patients | Sniffin’ sticks; validated questionnaires | 6 months: - OD: 55.6% | N/A | Prevalence of chemosensory dysfunction and recovery time | 21 |
| 3 | Boscolo Rizzo P 45 | 2021 | Multicentric | 145 COVID-19 patients | UPSIT | 6 months: -OD 60%, anosmia 6.9%, severe hyposmia 4.8% | N/A | Recovery time | 21 |
| 4 | Boscolo-Rizzo P 46 | 2021 | Multicentric | 100 COVID-19 patients | Sniffin’ sticks, taste strips, screening for intranasal trigeminal dysfunction (visual analogue scale) | Orthonasal smell in COVID-19 patients: OD 46% (7% anosmic). Gustatory function in COVID-19 patients: GD 27%. Nasal trigeminal sensitivity significantly lower in COVID-19 patients | N/A | Prevalence of chemosensory dysfunction | 22 |
| 5 | González C 47 | 2021 | Chile, USA | 100 COVID-19 patients; 63 controls | UPSIT | OD: -Baseline 75%; -One month: 41% | N/A | Prevalence of chemosensory dysfunction | 21 |
| 6 | Iannuzzi L 48 | 2020 | Italy | 30 COVID-19 patients | Sniffin’ sticks; validated questionnaires (VAS, Hyposmia rating scale) | 10% anosmia, > 50% hyposmia | 1 month | Recovery time | 21 |
| 7 | Le Bon SD 51 | 2021 | Multicentric | 72 COVID-19 patients | Sniffin’ sticks, taste strips, screening for intranasal trigeminal dysfunction (identification of menthol) | OD: anosmia 8%, hyposmia 29%, normosmia 63% | N/A | Prevalence of chemosensory dysfunction | 22 |
| 8 | Le Bon SD 49 | 2021 | Multicentric | 93 COVID-19 patients | Sniffin’sticks (identification test); taste strips | OD: 18% hyposmic, 3% anosmic. GD: 12% hypogeusic, no ageusic patients | N/A | Prevalence of chemosensory dysfunction | 20 |
| 9 | Le Bon SD 50 | 2021 | Belgium | 27 COVID-19 patients | Sniffin’ sticks | Improvement in the group oral corticosteroids + olfactory training: 7.7 points; olfactory training: 2.1 points | N/A | Treatment outcomes | 21 |
| 10 | Lechien JR 54 | 2020 | Multicentric | 78 COVID-19 patients | Validated questionnaires; Sniffin’ sticks identification test (46 patients) | OD: 11% anosmia; 24% hyposmia | N/A | Prevalence of chemosensory dysfunction | 20 |
| 11 | Lechien JR 53 | 2020 | Multicentric | 88 COVID-19 patients | Sniffin’ sticks (identification test); validated questionnaires | OD: 44.6%. Recovery at 2 months: 79.5% | N/A | Recovery time | 20 |
| 12 | Lechien JR 52 | 2020 | Multicentric | 47 COVID-19 patients | Sniffin’sticks (identification test); validated questionnaires | OD: 8.5% anosmia, 19.1% hyposmia | N/A | Prevalence of chemosensory dysfunction | 19 |
| 13 | Moein ST 55 | 2020 | Iran | 100 COVID-19 patients | UPSIT | OD: -Baseline: 96%; -after 5 weeks: 63% | N/A | Prevalence of chemosensory dysfunction and recovery time | 22 |
| 14 | Niklassen AS 9 | 2021 | Multicentric | 111 COVID-19 patients | Sniffin’ sticks, taste sprays | OD: 21% anosmia; 49% hyposmia; GD: 26% | 28 days | Prevalence of chemosensory dysfunction and recovery time | 22 |
| 15 | Petrocelli M 56 | 2021 | Multicentric | 300 COVID-19 patients | Evaluation of the ethyl alcohol olfactory threshold and the discriminative function for six groups of common household odorants. Taste sprays | Baseline: anosmia 47%, ageusia 38%; 6 months: anosmia 5%, ageusia 1% | N/A | Recovery time | 19 |
| 16 | Petrocelli M 94 | 2020 | Italy | 300 COVID-19 patients | Validated psychophysical self-administered test | OD and/or GD: 70%; anosmia 47%, ageusia 38% | N/A | Prevalence of chemosensory dysfunction | 19 |
| 17 | Prajapati DP 58 | 2020 | USA | 81 COVID-19 patients | 12-item BSIT; VAS | OD: 66.6% | N/A | Prevalence of chemosensory dysfunction | 21 |
| 18 | Prajapati DP 59 | 2021 | USA | 52 COVID-19 patients | 12-item BSIT; VAS | OD: 63% | 12 days | Prevalence of chemosensory dysfunction and recovery time | 21 |
| 19 | Saussez S 60 | 2021 | Multicentric | 288 COVID-19 patients | Validated questionnaires; Sniffin’ sticks identification test | Baseline: anosmia 39.2%, hyposmia 13.2%; 60 days: anosmia 9.4%, hyposmia 16% | N/A | Recovery time | 20 |
| 20 | Vaira LA 68 | 2021 | Multicentric | 170 COVID-19 patients; 170 controls | Sniffin’ sticks | COVID-19 patients: anosmia in 4.7%, hyposmia in 21.8% cases. Controls: hyposmia in 3.5% cases | N/A | Prevalence of chemosensory dysfunction | 22 |
| 21 | Vaira LA 63 | 2021 | Multicentric | 60 COVID-19 patients | CCCRC | Prevalence of OD = 76.7%; anosmia 20%, severe hyposmia 18.3%, moderate hyposmia 18.3%, mild hyposmia 16.7% | N/A | Correlation between olfactory dysfunction and viral load | 22 |
| 22 | Vaira LA 62 | 2021 | Multicentric | 77 COVID-19 patients | CCCRC | Prevalence of OD= 74%; anosmia 18.1%, severe hyposmia 16.9%, moderate hyposmia 24.7%, mild hyposmia 14.3% | N/A | Correlation between olfactory dysfunction and inflammatory markers | 21 |
| 23 | Vaira LA 61 | 2021 | Multicentric | 74 COVID-19 patients | CCCRC | OD: mild hyposmia 14.9%, moderate hyposmia 24.3%, severe hyposmia 16.2, anosmia 18.9% | N/A | Correlation between olfactory dysfunction and inflammatory markers | 21 |
| 24 | Vaira LA 67 | 2021 | Multicentric | 774 COVID-19 patients | Sniffin-Sticks test, CCCRC | OD = 62.1%: hyposmic 36.2%, anosmic 25.9% | N/A | Prevalence of chemosensory dysfunction | 21 |
| 25 | Vaira LA 66 | 2021 | Multicentric | 18 COVID-19 patients | CCCRC | Median olfactory score: -Baseline: treatment group 10; controls 20 | N/A | Treatment outcomes | 22 |
| 26 | Vaira LA 65 | 2020 | Multicentric | 138 COVID-19 patients | CCCRC | Chemosensory dysfunction: baseline 84.8%; 2 months 7.2% | N/A | Recovery time | 19 |
| 27 | Vaira LA 64 | 2020 | Multicentric | 106 COVID-19 patients | CCCRC | Baseline: OD 67%, GD 65.6% | N/A | Prognostic value of olfactory dysfunction | 19 |
| 28 | Vaira LA 69 | 2020 | Italy | 345 COVID-19 patients | Validated psychophysical self-administered test; CCCRC | OD: mild disease 66.6%; moderate 67%; severe 69.2% GD: mild 70.2%, moderate 71.3%, severe 65.4%. | N/A | Prevalence of chemosensory dysfunction | 20 |
| 29 | Vaira LA 70 | 2020 | Italy | 33 COVID-19 patients | Validated psychophysical self-administered test; CCCRC | N/A | N/A | Validation of a self-administered olfactory and gustatory test | 21 |
| 30 | Vaira LA 57 | 2020 | Italy | 72 COVID-19 patients | CCCRC, taste sprays | OD: anosmia 2.8%, hyposmia 80.6%. GD: ageusia 1.4%, hypogeusia 47.2% | N/A | Prevalence of chemosensory dysfunction | 22 |
Abbreviations: CCCRC: indicates Connecticut Chemosensory Clinical Research Center test; OD: olfactory dysfunction; GD: gustatory dysfunction; UPSIT: University of Pennsylvania Smell Identification test; VAS: Visual Analogue Scale; BSIT: Brief Smell Identification Test.
*Scores interval from 0 to 22, with higher scores showing better study quality 12.
Table III.
Features of the studies using imaging techniques.
| Source | Year | Country | Study population | Methods | Prevalence | Recovery time | Topic | STROBE score* | |
|---|---|---|---|---|---|---|---|---|---|
| 1 | Altundag A 71 | 2020 | Turkey, USA | 91 cases: 24 cases COVID-19 patients, 38 patients with PIOD, and a control group of 29 patients | CT scan, MRI | COVID-19 patients: 100% anosmic | N/A | Radiological study | 22 |
| 2 | Kandemirli SG 72 | 2021 | Turkey, USA | 23 COVID-19 patients | Sniffin’ sticks, CT scan, MRI | COVID-19 patients: 100% anosmic | N/A | Radiological study | 20 |
| 3 | Lechien JR 73 | 2020 | Multicentric | 16 COVID-19 patients | Validated questionnaire, Sniffin’ sticks, olfactory cleft examination, CT scan | COVID-19 patients: 100% anosmic | N/A | Radiological study | 22 |
| 4 | Tekcan Sanli DE 74 | 2021 | Turkey, USA | 50 COVID-19 patients | Sniffin’ sticks, CT scan. | N/A | N/A | Radiological study | 21 |
| 5 | Yildirim D 75 | 2021 | Turkey, USA | 31 COVID-19 patients, 97 patients with PIOD | Olfactory bulb MRI, DTI, and olfactory fMRI | COVID-19 patients: 100% anosmic; PIOD patients: 18.6% hyposmic, 81.4% anosmic | N/A | Radiological study | 21 |
PIOD: indicates post-infectious olfactory disorder; CT: computed tomography; MRI: magnetic resonance imaging; N/A: not applicable.
*Scores interval from 0 to 22, with higher scores showing better study quality 12.
About the olfactory assessment, the extended version of the Sniffin’ Sticks test was used in 11 articles 9,44,46,48,50,51,67,68,72-74, Connecticut Chemosensory Clinical Research Center (CCCRC) olfactory test in 11 43,57,61-67,69,70, the 16-item Sniffin’ Sticks identification test in 7 31,32,49,52-54,60, University of Pennsylvania Smell Identification Test (UPSIT) in 3 45,47,55, a new validated psychophysical self-administered test in 3 57,69,70, 12-item Brief Smell Identification Test (BSIT) in 2 58,59, an olfactory and gustatory home test in one 28 and evaluation of the ethyl alcohol olfactory threshold and discriminative function for six common household odorants in one 56.
Concerning gustatory assessment, taste strips were used in 3 articles 46,49,51 and taste sprays in 3 9,56,57.
Results from psychophysical tests of smell during SARS-CoV-2 infection (Tab. IV) showed that the olfactory threshold score was more impacted than the odour discrimination and identification scores in the studies using the extended version of the Sniffin’ Sticks test. In fact, this group of articles presented an overall threshold, discrimination and identification (TDI) score of 22.5 ± 7.8 indicating moderate hyposmia, while the threshold score was 5.2 ± 1.3 and the discrimination and identification, respectively, were 10.8 ± 0.9 and 10.7 ± 1.0. Similarly, the CCCRC and the UPSIT global scores were, respectively, 40.8 ± 14.7 and 25.2 ± 2.5, indicating moderate hyposmia. With screening tests, scores from the 12-item BSIT were 8.5 ± 0.5 (hyposmia: ≤ 9) 76 and 11.6 ± 0.8 from the 16-item Sniffin’ Sticks identification (normosmia: ≥ 12) 77.
Table IV.
Results from psychophysical tests of smell during SARS-CoV-2 infection. Results are presented as mean plus standard deviation.
| Test | Threshold | Discrimination | Identification | TDI score | CCCRC score |
|---|---|---|---|---|---|
| Sniffin’ sticks extended test | 5.2 ± 1.3 | 10.8 ± 0.9 | 10.7 ± 1.0 | 22.5 ± 7.8 | N/A |
| CCCRC | 18.8* | N/A | 47.6* | N/A | 40.8 ± 14.7 |
| UPSIT | N/A | N/A | 25.2 ± 2.5 | N/A | N/A |
| 16-item Sniffin’ stick identification test | N/A | N/A | 11.6 ± 0.8 | N/A | N/A |
| 12-item brief BSIT | N/A | N/A | 8.5 ± 0.5 | N/A | N/A |
BSIT: indicates Brief Smell Identification Test; N/A: not applicable; CCCRC: Connecticut Chemosensory Clinical Research Center test; UPSIT: The University of Pennsylvania Smell Identification test; TDI score: threshold discrimination identification score.
* Results of CCCRC score according to threshold and identification scores were presented only in the article “Objective evaluation of anosmia and ageusia in COVID-19 patients: Single-center experience on 72 cases”. By Vaira LA et al. 57.
The prevalence of chemosensory dysfunction was the most investigated topic in half of articles (n = 33), followed by recovery time in 8 articles (Fig. 2). Other topics of interest were studies using imaging techniques (n = 5), the predictive value of olfactory loss in COVID-19 (n = 5), miscellaneous (n = 5) and studies investigating both the prevalence of chemosensory dysfunction and recovery time (n = 5). Less explored themes were treatment outcomes (n = 3) and validation of new tests (n = 2).
Figure 2.
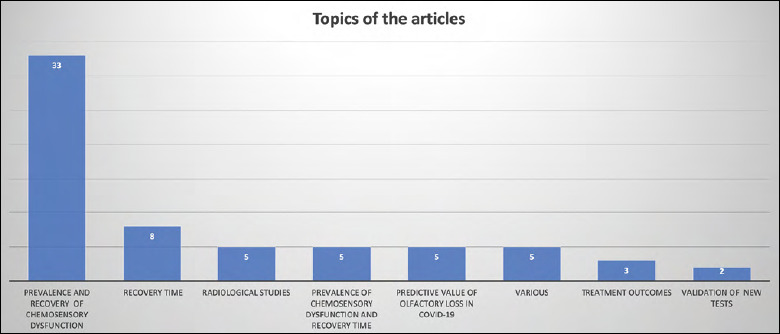
Topics of included articles about COVID-19 chemosensory dysfunction from December 2019 to November 2021. Prevalence of chemosensory dysfunction was the most investigated topic.
About the recovery time (Fig. 3), results from psychophysical tests (i.e., Sniffin’ Sticks extended test, CCCRC) showed a prevalence of olfactory dysfunction about the 70% during SARS-CoV-2 infection, with only 20% of patients still presenting impairment after one month.
Figure 3.
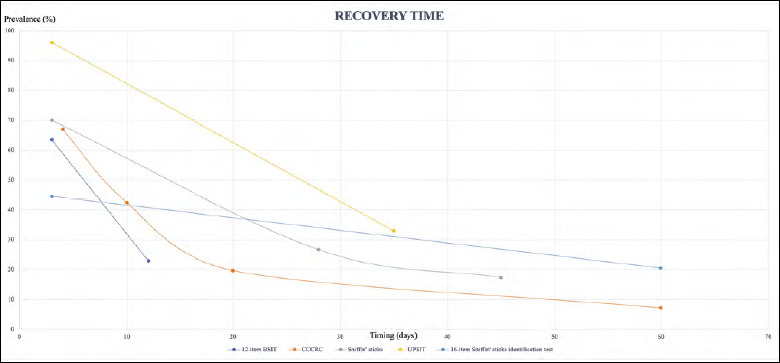
Recovery time of olfactory dysfunction evaluated using psychophysical testing. The figure shows the prevalence of patients suffering from olfactory dysfunction according to the timing of SARS-CoV-2 infection.
Within the included articles, 32 (48.5%) were multicentric.
Discussion
The results of this review demonstrate that the prevalence of olfactory and gustatory dysfunction in COVID-19 patients is highly variable in the current literature and depends on the methodology used. In fact, the prevalence of olfactory dysfunction ranges from 14 to 89% in case of assessments based on self-ratings (Tab. I), while it ranges from 21 to 96% in case of psychophysical assessment (Tab. II). Regarding taste impairment, although generally less present 78, we found rates of 9 to 88% based on self-ratings (Tab. I) and of 12 to 66% based on psychophysical testing. This discrepancy is partly due to the fact that the importance attributed to smell, taste and flavour varies among the general population according to sex, age and sociocultural factors, which is a major bias in response behaviour 79-82. In fact, many studies adopted visual analogue scales (VAS) to rate olfactory/gustatory dysfunction 28,35, as well as ad hoc questions 83. Other studies used only the responses to taste or smell-related questions of certain patient response outcome measures, like the Sinonasal Outcome test 22 (SNOT-22) 16,19. Only a few studies used validated questionnaires specifically investigating smell impairment such as the Questionnaire of Olfactory Dysfunction (QOD) 38 or the short version of the Questionnaire of Olfactory Disorders-Negative Statements (sQOD-NS) 29. However, the prevalence of olfactory/gustatory dysfunction varies remarkably among the studies (Tabs. II, IV) where psychophysical assessment was conducted with a wide range of tests that highly differ from each other (i.e., Sniffin’ Sticks extended version, CCCRC olfactory test, UPSIT, BSIT, home self-administered test, taste sprays, taste strips). Many research groups used only screening tests to assess olfactory function, such as the 12-item BSIT 58,59 or the 16-item smell identification test of the Sniffin’ Sticks battery 53,60. However, the Sniffin’ Sticks test in its full version consists of three subtests aiming at thorough evaluation of the olfactory capacity of individuals. The test results in a comprehensive TDI score 1-48 with scores > 30.5 indicating normosmia 84. Conversely, other olfactory tests are less difficult, less expensive and less time-consuming, but they do not provide such an extensive assessment as the Sniffin’ sticks. In fact, the UPSIT 85 is a smell identification test and the CCCRC 86 includes only the smell detection threshold (using the method of ascending limits) and smell identification assessment. Similarly, for gustatory assessment, the taste sprays used in many of the studies included can be considered just as a screening test. Conversely, the taste strips allow to collect more accurate data about the primary taste which is impacted (i.e., sweet, salty, bitter, and sour) and to classify taste capacity of patients in normogeusia and hypogeusia 87.
Interestingly, results from psychophysical tests of olfactory function presented in Table IV showed that the threshold score was significantly more impacted than the discrimination and identification performances in the studies using the extended version of the Sniffin’ Sticks test (T: 5.2 ± 1.3; D: 10.8 ± 0.9; I: 10.7 ± 1.0). This also appears to be valid in publications using the CCCRC (T: 18.8 versus I: 47.6), although this test does not evaluate the discrimination capacity as the Sniffin’ Sticks. Therefore, the results of psychophysical tests suggest that COVID-19 olfactory dysfunction impacts less the more complex cognitive processing of olfactory information. The SARS-CoV-2 virus has a major tropism for the nasal structures, such as the olfactory epithelium, which may partly explain the stronger effect on odour thresholds than odour identification. For further analysis of global olfactory function, a comprehensive evaluation using the extended version of the Sniffin’ Sticks test is preferable to an odour identification test alone, whenever possible.
The recovery time was the second most investigated parameter with eight articles focusing on this topic 9,45,48,53,56,60,65,83 and another five studying both the prevalence of chemosensory dysfunction and recovery time 18,23,44,55,59. The recovery time was on average 14.3 days for olfactory function and 10.2 days for gustatory function according to the studies included in Table I in which self-ratings of smell function were performed. Similarly, it was 23.3 days for olfaction according to the articles included in Table II in which psychophysical testing was executed. Studies investigating the long-term outcomes of olfactory dysfunction showed chemosensory dysfunction in 7% of patients at 2 months 65 with the 80% of COVID-19 patients reporting olfactory recovery 53. Using the UPSIT another article suggested severe microsmia in 2% and anosmia in 5% of COVID-19 patients after 6-month follow-up 45. Hence, the timing of the evaluation during and after SARS-CoV-2 infection significantly influences the results of the psychophysical tests. This is important as patients who show persistent dysfunction after 15-20 days should be referred to an otolaryngologist to be tested and to start timely treatment that includes safety counselling (e.g., maintain smoke and gas detectors, monitor spoiled food), olfactory training and possible adjuvant medication (e.g., intranasal vitamin A, systemic omega 3) 88. Regarding treatment, a pilot study in a small sample of patients included in Table II of this review using the Sniffin’ sticks test reported that a 10-day treatment of oral corticosteroids associated with olfactory training led to significant improvement of the olfactory score compared to olfactory training alone 50. However, there is skepticism in the current literature about the use of systemic corticosteroids to treat COVID-19 olfactory impairment as documented in an international consensus article 89. In fact, the experts have called for caution against the use of oral corticosteroids because of the lack of solid scientific evidence and the potential side effects (i.e., glaucoma, hip fractures). Moreover, COVID-19-related olfactory impairment tends to spontaneously recover in one month. Additionally, conventional intranasal administration of topical steroids does not appear to be an effective therapeutic option since steroid sprays do not appropriately reach the olfactory cleft 90.
The debate concerning the pathogenesis of SARS-CoV-2 chemosensory dysfunction is still open and some studies have postulated that the viral-associated damage might be extended not only to the olfactory epithelium, but also to the olfactory bulb and the central nervous system 8. Five studies 71-75 included in Table III used imaging techniques (i.e., computed tomography-CT scan, magnetic resonance imaging-MRI) to investigate chemosensory dysfunction in COVID-19 patients and contributed to the understanding of the mechanisms underlying smell and taste impairment. In these radiological studies, abnormalities such as higher olfactory cleft width and volume 71,74 and decreased white matter tract integrity of olfactory regions were detected in COVID-19 patients 75. In contrast, a post-mortem study on 85 COVID-19 deceased patients demonstrated that sustentacular cells are the main target in the olfactory mucosa, while olfactory sensory neurons and parenchyma of the olfactory bulb are not affected 91. Another recent review of animal and human studies also suggested that infections of the olfactory epithelium in COVID-19 patients rarely result in a brain infection because of the lack of entry protein expression in olfactory neurons that creates a barrier 92. Therefore, the neurotrophic action of COVID-19 is still uncertain, and this is in accordance with the results of the psychophysical tests of this review showing that olfactory threshold performance is more impacted than discrimination and identification capacities (Tab. IV).
Olfactory dysfunction is now globally recognised as a key symptom of SARS-CoV-2 infection, while its positive prognostic value is still debated. Five studies investigated the predictive value of olfactory loss in the diagnosis and course of COVID-19 22,24,26,42,64. It was found that sudden olfactory loss presents a high specificity of 97% and a sensitivity of 65%, while it has a positive predictive value of 63% and negative predictive value of 97% for SARS-CoV-2 infection 24. Interestingly, the use of olfactory loss as an indicator of COVID-19 in the general population could have important clinical applications in underserved areas with limited access to COVID-19 testing 26. Another four publications studied the correlation between olfactory dysfunction and inflammatory markers 61,62 as well as lung involvement 43 and viral load 21. For inflammatory markers, the level of interleukin 6 (IL-6), which is known to be a proinflammatory cytokine secreted by COVID-19 infected cells, was found to be significantly correlated with the severity of SARS-CoV-2 infection with a directly proportional association, but the correlation between IL-6 plasma concentrations and olfactory performance was not significant 61. Additionally, smell dysfunction seems to have poorer prognostic value in predicting the severity of COVID-19 compared to other systemic inflammatory markers (i.e., D-dimer, ferritin, procalcitonin and neutrophil-to-lymphocyte ratio). These findings could suggest that the pathogenesis of COVID-19 chemosensory dysfunction is more likely due to intranasal local factors rather than to systemic inflammation 62. Lung involvement detected by CT in COVID-19 patients did not exhibit a significant correlation with olfactory performance measured by CCCRC 43.
Finally, new tools were developed and validated to overcome many limitations that arose during various lockdown measures and hospital reorganisation due to the COVID-19 pandemic 7. It is worth mentioning the COVID-19 Questionnaire (COVID-Q) 40, a novel symptom questionnaire specific for COVID-19 to identify patients who are likely to suffer from SARS-CoV-2 infection, and the validation of a self-administered olfactory and gustatory test for the remote evaluation of COVID-19 patients 70. Precisely, the COVID-Q 40 was tested on 230 non-hospitalised COVID-19 patients and 230 controls enrolled at Treviso Hospital. The questionnaire included 27 items in its final version, which relate to “asthenia”, “gastrointestinal symptoms”, “ear and nose symptoms”, “breathing issues”, “throat symptoms”, “anosmia/ageusia” and “muscle pain”. Interestingly, “anosmia/ageusia” items were significantly correlated with rates of positive COVID-19 test positivity. Concerning the self-administered olfactory and gustatory tests for remote evaluation of COVID-19 patients 70, these have been assessed in 33 home-quarantined COVID-19 patients and the results compared with those obtained from the CCCRC and an operator-administered gustatory screening test. The novel self-administered test comprised an olfactory threshold test plus an odour discrimination test and a gustatory screening test with four solutions corresponding to the primary tastes. Although the cohort was made up only of infected health personnel and is not representative of the general population, the preliminary findings appear promising as there were no significant differences between the results of the tests for either smell (p = 0.201) or taste (p = 0.180). Pilot data were later confirmed by another study on 300 COVID-19 patients belonging to the healthcare staff of the Bellaria-Maggiore Hospital in Bologna 94.
Conclusions
The results of this review confirm that smell and taste impairments are key symptoms of SARS-CoV-2 infection, even in asymptomatic and mildly symptomatic patients 29,93, and that the timing significantly influenced the results of the psychophysical testing with a consistent improvement at one month after infection. The olfactory threshold performance was the most impacted compared to odour discrimination and odour identification capacities in accordance with the findings of a major tropism of SARS-CoV-2 for the olfactory mucosa 91,92. Finally, COVID-19 chemosensory dysfunction brought to the attention of the scientific community the central role of the otolaryngologists in the management of chemosensory dysfunction and the importance of performing psychophysical testing to offer smell rehabilitation and valid treatment options to patients with persistent sensory impairment 9.
Conflict of interest statement
The authors declare no conflict of interest.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Authors’ contributions
All authors meet the International Commitee of Medical Journal Editors (ICMJE) criteria:
1) Substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data for the work (EMCT, MC, FL, MG); 2) Drafting the work or revising it critically for important intellectual content (EMCT, TH); 3) Final approval of the version to be published (EMCT, MC, FL, PP, CM, TH, MG); 4) Agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved (EMCT, PP, CM). EMCT and MG were specifically responsible for the data collection.
Ethical consideration
This systematic review was exempted from institutional ethical committee approval.
Figures and tables
References
- 1.Xydakis MS, Dehgani-Mobaraki P, Holbrook EH, et al. Smell and taste dysfunction in patients with COVID-19. Lancet Infect Dis 2020;20:1015-1016. https://doi.org/10.1016/S1473-3099(20)30293-0 10.1016/S1473-3099(20)30293-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Trecca E, Marano PG, Gelardi M, et al. Is 2020 the golden year of otolaryngology research? The impact of COVID-19 on the Italian academic production. Acta Biomed 2021;92:e2021207. https://doi.org/10.23750/abm.v92i2.11557 10.23750/abm.v92i2.11557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chillakuru YR, Gerhard EF, Shim T, et al. Impact of COVID-19 on otolaryngology literature. Laryngoscope 2021. Oct 8:10.1002/lary.29902. https://doi.org/10.1002/lary.29902. Epub ahead of print. 10.1002/lary.29902 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zocchi J, Pietrobon G, Moretto S, et al. Literature in the time of COVID-19: the “phase two.” Oral Oncol 2020. Jun 3;109:104837. https://doi.org/10.1016/j.oraloncology.2020.104837. Epub ahead of print. 10.1016/j.oraloncology.2020.104837 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Vaira LA, Salzano G, Deiana G, et al. Anosmia and ageusia: common findings in COVID-19 patients. Laryngoscope 2020;130:1787. https://doi.org/10.1002/lary.28692 10.1002/lary.28692 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Maniaci A, Iannella G, Vicini C, et al. A case of COVID-19 with late-onset rash and transient loss of taste and smell in a 15-year-old boy. Am J Case Rep 2020;21:e925813. https://doi.org/10.12659/AJCR.925813 10.12659/AJCR.925813 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gelardi M, Iannuzzi L, Trecca EMC, et al. COVID-19: what happened to all of the otolaryngology emergencies? Eur Arch Otorhinolaryngol 2020;277:3231-3232. https://doi.org/10.1007/s00405-020-06046-z 10.1007/s00405-020-06046-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Huart C, Philpott C, Konstantinidis I, et al. Comparison of COVID-19 and common cold chemosensory dysfunction. Rhinology 2020;58:623-625. https://doi.org/10.4193/Rhin20.251 10.4193/Rhin20.251 [DOI] [PubMed] [Google Scholar]
- 9.Niklassen AS, Draf J, Huart C, et al. COVID-19: recovery from chemosensory dysfunction. A multicentre study on smell and taste. Laryngoscope 2021;131:1095-1100. https://doi.org/10.1002/lary.29383 10.1002/lary.29383 [DOI] [PubMed] [Google Scholar]
- 10.Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting Items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 2009;6:e1000097. https://doi.org/10.1371/journal.pmed.1000097 10.1371/journal.pmed.1000097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021;372:n71. https://doi.org/10.1136/bmj.n71 10.1136/bmj.n71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Vandenbroucke JP, von Elm E, Altman DG, et al. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): explanation and elaboration. Int J Surg 2014;12:1500-1524. https://doi.org/10.1016/j.ijsu.2014.07.014 10.1016/j.ijsu.2014.07.014 [DOI] [PubMed] [Google Scholar]
- 13.Altundag A, Saatci O, Sanli DET, et al. The temporal course of COVID-19 anosmia and relation to other clinical symptoms. Eur Arch Otorhinolaryngol 2021;278:1891-1897. https://doi.org/10.1007/s00405-020-06496-5 10.1007/s00405-020-06496-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bagheri SH, Asghari A, Farhadi M, et al. Coincidence of COVID-19 epidemic and olfactory dysfunction outbreak in Iran. Med J Islam Repub Iran 2020;34:62. https://doi.org/10.34171/mjiri.34.62 10.34171/mjiri.34.62 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Barillari MR, Bastiani L, Lechien JR, et al. A structural equation model to examine the clinical features of mild-to-moderate COVID-19: a multicenter Italian study. J Med Virol 2021;93:983-994. https://doi.org/10.1002/jmv.26354 10.1002/jmv.26354 [DOI] [PubMed] [Google Scholar]
- 16.Boscolo-Rizzo P, Guida F, Polesel J, et al. Self-reported smell and taste recovery in coronavirus disease 2019 patients: a one-year prospective study. Eur Arch Otorhinolaryngol 2022;279:515-520. https://doi.org/10.1007/s00405-021-06839-w 10.1007/s00405-021-06839-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Boscolo-Rizzo P, Borsetto D, Spinato G, et al. New onset of loss of smell or taste in household contacts of home-isolated SARS-CoV-2-positive subjects. Eur Arch Otorhinolaryngol 2020;277:2637-2640. https://doi.org/10.1007/s00405-020-06066-9 10.1007/s00405-020-06066-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Boscolo-Rizzo P, Borsetto D, Fabbris C, et al. Evolution of altered sense of smell or taste in patients with mildly symptomatic COVID-19. JAMA Otolaryngol Neck Surg 2020;146:729-732. https://doi.org/10.1001/jamaoto.2020.1379 10.1001/jamaoto.2020.1379 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chapurin N, Totten DJ, Chaballout B, et al. Differential olfactory outcomes in COVID-19: a large healthcare system population study. Int Forum Allergy Rhinol 2022;12:108-111. https://doi.org/10.1002/alr.22870 10.1002/alr.22870 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chiesa-Estomba CM, Lechien JR, Radulesco T, et al. Patterns of smell recovery in 751 patients affected by the COVID-19 outbreak. Eur J Neurol 2020;27:2318-2321. https://doi.org/10.1111/ene.14440 10.1111/ene.14440 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cho RHW, To ZWH, Yeung ZWC, et al. COVID-19 viral load in the severity of and recovery from olfactory and gustatory dysfunction. Laryngoscope 2020;130:2680-2685. https://doi.org/10.1002/lary.29056 10.1002/lary.29056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gerkin RC, Ohla K, Veldhuizen MG, et al. Recent smell loss is the best predictor of COVID-19 among individuals with recent respiratory symptoms. Chem Senses 2021;46:bjaa081. https://doi.org/10.1093/chemse/bjaa081 10.1093/chemse/bjaa081 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gorzkowski V, Bevilacqua S, Charmillon A, et al. Evolution of olfactory disorders in COVID-19 patients. Laryngoscope 2020;130:2667-2673. https://doi.org/10.1002/lary.28957 10.1002/lary.28957 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Haehner A, Draf J, Dräger S, et al. Predictive value of sudden olfactory loss in the diagnosis of COVID-19. ORL J Otorhinolaryngol Relat Spec 2020;82:175-180. https://doi.org/10.1159/000509143 10.1159/000509143 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hopkins C, Surda P, Vaira LA, et al. Six month follow-up of self-reported loss of smell during the COVID-19 pandemic. Rhinology 2021;59:26-31. https://doi.org/10.4193/Rhin20.544 10.4193/Rhin20.544 [DOI] [PubMed] [Google Scholar]
- 26.Iravani B, Arshamian A, Ravia A, et al. Relationship between odor intensity estimates and COVID-19 prevalence prediction in a Swedish population. Chem Senses 2020. May 22:bjaa034. https://doi.org/10.1093/chemse/bjaa034. Epub ahead of print. 10.1093/chemse/bjaa034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Jalessi M, Bagheri SH, Azad Z, et al. The outcome of olfactory impairment in patients with otherwise paucisymptomatic coronavirus disease 2019 during the pandemic. J Laryngol Otol 2021;135:426-435. https://doi.org/10.1017/S0022215121001110 10.1017/S0022215121001110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Konstantinidis I, Delides A, Tsakiropoulou E, et al. Short-term follow-up of self-isolated COVID-19 patients with smell and taste dysfunction in Greece: two phenotypes of recovery. ORL J Otorhinolaryngol Relat Spec 2020;82:295-303. https://doi.org/10.1159/000511436 10.1159/000511436 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lechien JR, Chiesa-Estomba CM, De Siati DR, et al. Olfactory and gustatory dysfunctions as a clinical presentation of mild-to-moderate forms of the coronavirus disease (COVID-19): a multicenter European study. Eur Arch Otorhinolaryngol 2020;277:2251-2261. https://doi.org/10.1007/s00405-020-05965-1 10.1007/s00405-020-05965-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lechien JR, Chiesa-Estomba CM, Place S, et al. Clinical and epidemiological characteristics of 1420 European patients with mild-to-moderate coronavirus disease 2019. J Intern Med 2020;288:335-344. https://doi.org/10.1111/joim.13089 10.1111/joim.13089 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lechien JR, Chiesa-Estomba CM, Vaira LA, et al. Epidemiological, otolaryngological, olfactory and gustatory outcomes according to the severity of COVID-19: a study of 2579 patients. Eur Arch Otorhinolaryngol 2021;278:2851-2859. https://doi.org/10.1007/s00405-020-06548-w 10.1007/s00405-020-06548-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lechien JR, Chiesa-Estomba CM, Beckers E, et al. Prevalence and 6-month recovery of olfactory dysfunction: a multicentre study of 1363 COVID-19 patients. J Intern Med 2021;290:451-461. https://doi.org/10.1111/joim.13209 10.1111/joim.13209 [DOI] [PubMed] [Google Scholar]
- 33.Locatello LG, Trotta B, Bruno C, et al. Systemic steroids may enhance recovery from loss of smell and taste in hospitalized coronavirus disease 2019 (COVID-19) patients: an observational study. Int Forum Allergy Rhinol 2021;11:1689-1693. https://doi.org/10.1002/alr.22848 10.1002/alr.22848 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lucidi D, Molinari G, Silvestri M, et al. Patient-reported olfactory recovery after SARS-CoV-2 infection: a 6-month follow-up study. Int Forum Allergy Rhinol 2021;11:1249-1252. https://doi.org/10.1002/alr.22775 10.1002/alr.22775 [DOI] [PubMed] [Google Scholar]
- 35.Maiorano E, Calastri A, Robotti C, et al. Clinical, virological and immunological evolution of the olfactory and gustatory dysfunction in COVID-19. Am J Otolaryngol 2022;43:103170. https://doi.org/10.1016/j.amjoto.2021.103170 10.1016/j.amjoto.2021.103170 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Paderno A, Schreiber A, Grammatica A, et al. Smell and taste alterations in COVID-19: a cross-sectional analysis of different cohorts. Int Forum Allergy Rhinol 2020;10:955-962. https://doi.org/10.1002/alr.22610 10.1002/alr.22610 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Parma V, Ohla K, Veldhuizen MG, et al. More than smell – COVID-19 is associated with severe impairment of smell, taste, and chemesthesis. Chem Senses 2020;45:609-622. https://doi.org/10.1093/chemse/bjaa041 10.1093/chemse/bjaa041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Qiu C, Cui C, Hautefort C, et al. Olfactory and gustatory dysfunction as an early identifier of COVID-19 in adults and children: an international multicenter study. Otolaryngol Head Neck Surg 2020;163:714-721. https://doi.org/10.1177/0194599820934376 10.1177/0194599820934376 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Raad N, Ghorbani J, Safavi Naeini A, et al. Parosmia in patients with COVID-19 and olfactory dysfunction. Int Forum Allergy Rhinol 2021;11:1497-1500. https://doi.org/10.1002/alr.22818 10.1002/alr.22818 [DOI] [PubMed] [Google Scholar]
- 40.Spinato G, Fabbris C, Conte F, et al. COVID-Q: validation of the first COVID-19 questionnaire based on patient-rated symptom gravity. Int J Clin Pract 2021;75:e14829. https://doi.org/10.1111/ijcp.14829 10.1111/ijcp.14829 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Vaira LA, De Vito A, Lechien JR, et al. New onset of smell and taste loss are common findings also in patients with symptomatic COVID-19 after complete vaccination. Laryngoscope 2022;132:419-421. https://doi.org/10.1002/lary.29964 10.1002/lary.29964 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Yan CH, Faraji F, Prajapati DP, et al. Self-reported olfactory loss associates with outpatient clinical course in COVID-19. Int Forum Allergy Rhinol 2020;10:821-831. https://doi.org/10.1002/alr.22592 10.1002/alr.22592 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Amadu AM, Vaira LA, Lechien JR, et al. Analysis of the correlations between the severity of lung involvement and olfactory psychophysical scores in coronavirus disease 2019 (COVID-19) patients. Int Forum Allergy Rhinol 2022;12:103-107. https://doi.org/10.1002/alr.22869 10.1002/alr.22869 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Bordin A, Mucignat-Caretta C, Gaudioso P, et al. Comparison of self-reported symptoms and psychophysical tests in coronavirus disease 2019 (COVID-19) subjects experiencing long-term olfactory dysfunction: a 6-month follow-up study. Int Forum Allergy Rhinol 2021;11:1592-1595. https://doi.org/10.1002/alr.22828 10.1002/alr.22828 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Boscolo-Rizzo P, Menegaldo A, Fabbris C, et al. Six-month psychophysical evaluation of olfactory dysfunction in patients with COVID-19. Chem Senses 2021;46:bjab006. https://doi.org/10.1093/chemse/bjab006 10.1093/chemse/bjab006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Boscolo-Rizzo P, Hummel T, Hopkins C, et al. High prevalence of long-term olfactory, gustatory, and chemesthesis dysfunction in post-COVID-19 patients: a matched case-control study with one-year follow-up using a comprehensive psychophysical evaluation. Rhinology 2021;59:517-527. https://doi.org/10.4193/Rhin21.249 10.4193/Rhin21.249 [DOI] [PubMed] [Google Scholar]
- 47.González C, García-Huidobro FG, Lagos AE, et al. Prospective assessment of smell and taste impairment in a South-American coronavirus disease 2019 (COVID-19) cohort: association with the need for hospitalization and reversibility of dysfunction. Int Forum Allergy Rhinol 2021;11:1273-1277. https://doi.org/10.1002/alr.22798 10.1002/alr.22798 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Iannuzzi L, Salzo AE, Angarano G, et al. Gaining back what is lost: recovering the sense of smell in mild to moderate patients after COVID-19. Chem Senses 2020;45:875-881. https://doi.org/10.1093/chemse/bjaa066 10.1093/chemse/bjaa066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Le Bon S, Payen L, Prunier L, et al. Making scents of loss of taste in COVID-19: is self-reported loss of taste due to olfactory dysfunction? A prospective study using psychophysical testing. Int Forum Allergy Rhinol 2021;11:1504-1507. https://doi.org/10.1002/alr.22815 10.1002/alr.22815 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Le Bon S-D, Konopnicki D, Pisarski N, et al. Efficacy and safety of oral corticosteroids and olfactory training in the management of COVID-19-related loss of smell. Eur Arch Otorhinolaryngol 2021;278:3113-3117. https://doi.org/10.1007/s00405-020-06520-8 10.1007/s00405-020-06520-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Le Bon SD, Pisarski N, Verbeke J, et al. Psychophysical evaluation of chemosensory functions 5 weeks after olfactory loss due to COVID-19: a prospective cohort study on 72 patients. Eur Arch Otorhinolaryngol 2021;278:101-108. https://doi.org/10.1007/s00405-020-06267-2 10.1007/s00405-020-06267-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Lechien JR, Ducarme M, Place S, et al. Objective olfactory findings in hospitalized severe COVID-19 patients. Pathogens 2020;9:627. https://doi.org/10.3390/pathogens9080627 10.3390/pathogens9080627 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Lechien JR, Journe F, Hans S, et al. Severity of anosmia as an early symptom of COVID-19 infection may predict lasting loss of smell. Front Med (Lausanne) 2020;7:582802. https://doi.org/10.3389/fmed.2020.582802 10.3389/fmed.2020.582802 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Lechien JR, Cabaraux P, Chiesa-Estomba CM, et al. Psychophysical olfactory tests and detection of COVID-19 in patients with sudden onset olfactory dysfunction: a prospective study. Ear Nose Throat J 2020;99:579-583. https://doi.org/10.1177/0145561320929169 10.1177/0145561320929169 [DOI] [PubMed] [Google Scholar]
- 55.Moein ST, Hashemian SM, Tabarsi P, et al. Prevalence and reversibility of smell dysfunction measured psychophysically in a cohort of COVID-19 patients. Int Forum Allergy Rhinol 2020;10:1127-1135. https://doi.org/10.1002/alr.22680 10.1002/alr.22680 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Petrocelli M, Cutrupi S, Salzano G, et al. Six-month smell and taste recovery rates in coronavirus disease 2019 patients: a prospective psychophysical study. J Laryngol Otol 2021;135:436-441. https://doi.org/10.1017/S002221512100116X 10.1017/S002221512100116X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Vaira LA, Deiana G, Fois AG, et al. Objective evaluation of anosmia and ageusia in COVID-19 patients: single-center experience on 72 cases. Head Neck 2020;42:1252-1258. https://doi.org/10.1002/hed.26204 10.1002/hed.26204 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Prajapati DP, Shahrvini B, MacDonald BV, et al. Association of subjective olfactory dysfunction and 12-item odor identification testing in ambulatory COVID-19 patients. Int Forum Allergy Rhino 2020. Sep 10. https://doi.org/10.1002/alr.22688. Epub ahead of print. 10.1002/alr.22688 [DOI] [PubMed] [Google Scholar]
- 59.Prajapati DP, Shahrvini B, Said M, et al. Assessment of patient recognition of coronavirus disease 2019 (COVID-19)-associated olfactory loss and recovery: a longitudinal study. Int Forum Allergy Rhinol 2021;11:1529-1537. https://doi.org/10.1002/alr.22820 10.1002/alr.22820 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Saussez S, Sharma S, Thiriard A, et al. Predictive factors of smell recovery in a clinical series of 288 coronavirus disease 2019 patients with olfactory dysfunction. Eur J Neurol 2021;28:3702-3711. https://doi.org/10.1111/ene.14994 10.1111/ene.14994 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Vaira LA, De Vito A, Deiana G, et al. Correlations between IL-6 serum level and olfactory dysfunction severity in COVID-19 patients: a preliminary study. Eur Arch Otorhinolaryngol 2022;279:811-816. https://doi.org/10.1007/s00405-021-06868-5 10.1007/s00405-021-06868-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Vaira LA, De Vito A, Deiana G, et al. Systemic inflammatory markers and psychophysical olfactory scores in coronavirus disease 2019 patients: is there any correlation? Laryngol Otol 2021;135:723-728. https://doi.org/10.1017/S0022215121001651 10.1017/S0022215121001651 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Vaira LA, Deiana G, Lechien JR, et al. Correlations between olfactory psychophysical scores and SARS-CoV-2 viral load in COVID-19 patients. Laryngoscope 2021;131:2312-2318. https://doi.org/10.1002/lary.29777 10.1002/lary.29777 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Vaira LA, Hopkins C, Petrocelli M, et al. Do olfactory and gustatory psychophysical scores have prognostic value in COVID-19 patients? A prospective study of 106 patients. J Otolaryngol Head Neck Surg 2020;49:56. https://doi.org/10.1186/s40463-020-00449-y 10.1186/s40463-020-00449-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Vaira LA, Hopkins C, Petrocelli M, et al. Smell and taste recovery in coronavirus disease 2019 patients: a 60-day objective and prospective study. J Laryngol Otol 2020;134:703-709. https://doi.org/10.1017/S0022215120001826 10.1017/S0022215120001826 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Vaira LA, Hopkins C, Petrocelli M, et al. Efficacy of corticosteroid therapy in the treatment of long- lasting olfactory disorders in COVID-19 patients. Rhinology 2021;59:21-25. https://doi.org/10.4193/Rhin20.515 10.4193/Rhin20.515 [DOI] [PubMed] [Google Scholar]
- 67.Vaira LA, Lechien JR, Khalife M, et al. Psychophysical evaluation of the olfactory function: European multicenter study on 774 COVID-19 patients. Pathogens 2021;10:62. https://doi.org/10.3390/pathogens10010062 10.3390/pathogens10010062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Vaira LA, Salzano G, Bon S Le, et al. Prevalence of persistent olfactory disorders in patients with COVID-19: a psychophysical case-control study with 1-year follow-up. Otolaryngol Head Neck Surg 2021. Nov 23:1945998211061511. https://doi.org/10.1177/01945998211061511. Epub ahead of print. 10.1177/01945998211061511 [DOI] [PubMed] [Google Scholar]
- 69.Vaira LA, Hopkins C, Salzano G, et al. Olfactory and gustatory function impairment in COVID-19 patients: Italian objective multicenter-study. Head Neck 2020;42:1560-1569. https://doi.org/10.1002/hed.26269 10.1002/hed.26269 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Vaira LA, Salzano G, Petrocelli M, et al. Validation of a self-administered olfactory and gustatory test for the remotely evaluation of COVID-19 patients in home quarantine. Head Neck 2020;42:1570-1576. https://doi.org/10.1002/hed.26228 10.1002/hed.26228 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Altundag A, Yıldırım D, Tekcan Sanli DE, et al. Olfactory cleft measurements and COVID-19-related anosmia. Otolaryngol Head Neck Surg 202;164:1337-1344. https://doi.org/10.1177/0194599820965920 10.1177/0194599820965920 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Kandemirli SG, Altundag A, Yildirim D, et al. Olfactory bulb MRI and paranasal sinus CT Ffndings in persistent COVID-19 anosmia. Acad Radiol 2021;28:28-35. https://doi.org/10.1016/j.acra.2020.10.006 10.1016/j.acra.2020.10.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Lechien JR, Michel J, Radulesco T, et al. Clinical and radiological evaluations of COVID-19 patients with anosmia: preliminary report. Laryngoscope 2020;130:2526-2531. https://doi.org/10.1002/lary.28993 10.1002/lary.28993 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Tekcan Sanli DE, Altundag A, Yıldırım D, et al. Comparison of olfactory cleft width and volumes in patients with COVID-19 anosmia and COVID-19 cases without anosmia. ORL J Otorhinolaryngol Relat Spec 2022;84:1-9. https://doi.org/10.1159/000518672 10.1159/000518672 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Yildirim D, Kandemirli SG, Tekcan Sanli DE, et al. A comparative olfactory MRI, DTI and fMRI study of COVID-19 related anosmia and post viral olfactory dysfunction. Acad Radiol 2022;29:31-41. https://doi.org/10.1016/j.acra.2021.10.019 10.1016/j.acra.2021.10.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Joseph T, Auger SD, Peress L, et al. Screening performance of abbreviated versions of the UPSIT smell test. J Neurol 2019;266:1897-1906. https://doi.org/10.1007/s00415-019-09340-x 10.1007/s00415-019-09340-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Hummel T, Sekinger B, Wolf SR, et al. ‘Sniffin’ Sticks’: olfactory performance assessed by the combined testing of odour identification, odor discrimination and olfactory threshold. Chem Senses 1997;22:39-52. https://doi.org/10.1093/chemse/22.1.39 10.1093/chemse/22.1.39 [DOI] [PubMed] [Google Scholar]
- 78.Hintschich CA, Niv MY, Hummel T. The taste of the pandemic – contemporary review on the current state of research on gustation in coronavirus disease 2019 (COVID-19). Int Forum Allergy Rhinol 2022;12:210-216. https://doi.org/10.1002/alr.22902 10.1002/alr.22902 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Trecca EMC, Fortunato F, Gelardi M, et al. Development of a questionnaire to investigate socio-cultural differences in the perception of smell, taste and flavour. Acta Otorhinolaryngol Ital 2021;41:336-347. https://doi.org/10.14639/0392-100X-N0766 10.14639/0392-100X-N0766 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Croy I, Buschhüter D, Seo H-S, et al. Individual significance of olfaction: development of a questionnaire. Eur Arch Otorhinolaryngol 2010;267:67-71. https://doi.org/10.1007/s00405-009-1054-0 10.1007/s00405-009-1054-0 [DOI] [PubMed] [Google Scholar]
- 81.Landis BN, Hummel T, Hugentobler M, et al. Ratings of overall olfactory function. Chem Senses 2003;28:691-694. https://doi.org/10.1093/chemse/bjg061 10.1093/chemse/bjg061 [DOI] [PubMed] [Google Scholar]
- 82.Lötsch J, Hummel T. Clinical usefulness of self-rated olfactory performance – a data science-based assessment of 6,000 patients. Chem Senses 2019;44:357-364. https://doi.org/10.1093/chemse/bjz029 10.1093/chemse/bjz029 [DOI] [PubMed] [Google Scholar]
- 83.Lal P, Chamoli P, Tuli IP, et al. Olfactory and gustatory dysfunctions in patients with laboratory-confirmed COVID-19 infection: a change in the trend. Indian J Otolaryngol Head Neck Surg 2021. Jul 18:1-7. https://doi.org/10.1007/s12070-021-02752-0. Epub ahead of print. 10.1007/s12070-021-02752-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Oleszkiewicz A, Schriever VA, Croy I, et al. Updated Sniffin’ Sticks normative data based on an extended sample of 9139 subjects. Eur Arch Otorhinolaryngol 2019;276:719-728. https://doi.org/10.1007/s00405-018-5248-1 10.1007/s00405-018-5248-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Doty RL, Shaman P, Kimmelman CP, et al. University of Pennsylvania smell identification test: a rapid quantitative olfactory function test for the clinic. Laryngoscope 1984;94:176-178. https://doi.org/10.1288/00005537-198402000-00004 10.1288/00005537-198402000-00004 [DOI] [PubMed] [Google Scholar]
- 86.Cain WS, Gent JF, Goodspeed RB, et al. Evaluation of olfactory dysfunction in the Connecticut Chemosensory Clinical Research Center. Laryngoscope 1988;98:83-88. https://doi.org/10.1288/00005537-198801000-00017 10.1288/00005537-198801000-00017 [DOI] [PubMed] [Google Scholar]
- 87.Landis BN, Welge-Luessen A, Brämerson A, et al. “Taste Strips” – a rapid, lateralized, gustatory bedside identification test based on impregnated filter papers. J Neurol 2009;256:242-248. https://doi.org/10.1007/s00415-009-0088-y 10.1007/s00415-009-0088-y [DOI] [PubMed] [Google Scholar]
- 88.Whitcroft KL, Hummel T. Olfactory dysfunction in COVID-19. JAMA 2020;323:2512-2514. https://doi.org/10.1001/jama.2020.8391 10.1001/jama.2020.8391 [DOI] [PubMed] [Google Scholar]
- 89.Huart C, Philpott CM, Altundag A, et al. Systemic corticosteroids in coronavirus disease 2019 (COVID-19)-related smell dysfunction: an international view. Int Forum Allergy Rhinol 2021;11:1041-1046. https://doi.org/10.1002/alr.22788 10.1002/alr.22788 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Scheibe M, Bethge C, Witt M, et al. Intranasal administration of drugs. Arch Otolaryngol Head Neck Surg 2008;134:643-646. https://doi.org/10.1001/archotol.134.6.643 10.1001/archotol.134.6.643 [DOI] [PubMed] [Google Scholar]
- 91.Khan M, Yoo S-J, Clijsters M, et al. Visualizing in deceased COVID-19 patients how SARS-CoV-2 attacks the respiratory and olfactory mucosae but spares the olfactory bulb. Cell 2021;184:5932-5949.e15. https://doi.org/10.1016/j.cell.2021.10.027 10.1016/j.cell.2021.10.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Butowt R, Meunier N, Bryche B, et al. The olfactory nerve is not a likely route to brain infection in COVID-19: a critical review of data from humans and animal models. Acta Neuropathol 2021;141:809-822. https://doi.org/10.1007/s00401-021-02314-2 10.1007/s00401-021-02314-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Spinato G, Fabbris C, Polesel J, et al. Alterations in smell or taste in mildly symptomatic outpatients with SARS-CoV-2 infection. JAMA 2020;323:2089-2090. https://doi.org/10.1001/jama.2020.6771 10.1001/jama.2020.6771 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Petrocelli M, Ruggiero F, Baietti AM, et al. Remote psychophysical evaluation of olfactory and gustatory functions in early-stage coronavirus disease 2019 patients: the Bologna experience of 300 cases. J Laryngol Otol 2020;134:571-576. https://doi.org/10.1017/S0022215120001358 10.1017/S0022215120001358 [DOI] [PMC free article] [PubMed] [Google Scholar]


