Abstract
Introduction: Whether mobile-bearing (MB) unicompartmental knee arthroplasty (UKA) performs better than fixed-bearing (FB) implants in patients with monocompartmental osteoarthritis (OA) still remains unclear. Therefore, a meta-analysis comparing MB versus FB for UKA was conducted to investigate the possible advantages of MB versus FB in patient-reported outcome measures (PROMs), range of motion (ROM), and complications. We hypothesised that the MB design performs better than FB. Methods: This systematic review was conducted according to the 2020 PRISMA guidelines. In December 2021, PubMed, Web of Science, Google Scholar, and Embase were accessed, with no time constraints. All the clinical investigations comparing MB versus FB bearing for UKA were accessed. Only studies published in peer-reviewed journals were considered. Studies reporting data on revision settings were excluded, as were those combining unicompartmental and total knee arthroplasty. Results: Data from 25 studies (4696 patients) were collected; 58% (2724 of 4696 patients) were women. The mean length of follow-up was 45.8 ± 43.2. The mean age of the patients was 65.0 ± 5.6 years. No difference was found in range of motion (p = 0.05), Knee Scoring System (p = 0.9), function subscale (p = 0.2), and Oxford Knee Score (p = 0.4). No difference was found in the rate of revision (p = 0.2), aseptic loosening (p = 0.9), deep infections (p = 0.99), fractures (p = 0.6), and further extension of OA to the contralateral joint compartment (p = 0.2). Conclusion: The present meta-analysis failed to identify the possible superiority of the MB implants over the FB for UKA in patients with monocompartmental knee osteoarthritis. Long observational investigations are required to evaluate possible long-term complications and implant survivorship. These results should be interpreted within the limitations of the present study.
Keywords: unicompartmental knee arthroplasty, mobile bearing, fixed bearing
1. Introduction
Monocompartmental osteoarthritis (OA) of the knee is common [1]. Advanced monocompartmental knee OA impairs quality of life and participation in recreational activities [2,3]. Patients with end-stage monocompartmental OA, along with competent cruciate ligaments, varus deformity <5°, range of motion (ROM) greater than 90° without flexion contracture, and body mass index (BMI) <30 kg/m2, are candidates for unicompartmental knee arthroplasty (UKA) [4,5,6,7]. Mobile-bearing (MB) and fixed-bearing (FB) implants are routinely used for UKA [8,9,10]. In FB implants, the polyethylene inlay is fixed into the metal tibial plateau, allowing flexion, extension, and roll-back motion [11]. In MB implants, the polyethylene insert is mobile, allowing some degree of tibial rotation over the femur [11]. Although MB implants demonstrated faster surgical duration and greater range of motion, their superiority over FB implants still remains unclear [12,13,14,15]. Previous systematic reviews and meta-analyses, which compared the two implants, were not exhaustive, finding no clinically relevant differences in patient-reported outcome measures (PROMs), ROM, and rate of complication [8,9,16,17,18,19,20,21]. However, several clinical studies have been recently published, which have not yet been considered in any previous meta-analysis, and an update of the current evidence is required [22,23,24,25,26]. Therefore, a meta-analysis comparing MB versus FB for UKA was conducted to investigate possible advantages in PROMs, ROM, and complications.
2. Material and Methods
2.1. Eligibility Criteria
All the clinical trials comparing mobile versus fixed bearing in UKA for monocompartmental knee OA were accessed. Only studies with levels I and III of evidence, according to the Oxford Centre of Evidence-Based Medicine [27], were considered. Only studies published in peer-reviewed journals were considered. Given the authors’ language capabilities, articles in English, German, Italian, French, and Spanish were eligible. Reviews, opinions, letters, and editorials were not considered. Animal, in vitro, biomechanic, and cadaveric studies were not eligible. Studies that compared the effect of MB versus FB in experimental implants or protocols were excluded, as were those combining UKA with other interventions. Studies reporting data on revision settings were excluded, as were those combining combined results of uni- and bicompartmental arthroplasty. Only studies that clearly reported the number of patients included and the length of follow-up were eligible. Only studies that reported quantitative data under the endpoint of interest were considered for inclusion.
2.2. Search Strategy
This systematic review was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses: the 2020 PRISMA statement [28]. The PICOT algorithm was preliminarily pointed out:
P (Population): end-stage monocompartmental knee OA;
I (Intervention): UKA;
C (Comparison): MB versus FB;
O (Outcomes): PROMs, ROM, and complications.
In December 2021, the following databases were accessed: PubMed, Web of Science, Google Scholar, and Embase. No time constraints were used for the search. The following keywords were used in combination using the Boolean operator AND/OR: knee, unicompartmental, unicondylar, osteoarthritis, arthroplasty, replacement, prosthesis, implant, bearing, mobile, fixed, design, range of motion, ROM, function, patient-reported outcome measures, PROMs, complications, revision, reoperation, function, quality of life, loosening, pain.
2.3. Selection and Data Collection
Two authors (F.C. and K.E.) independently performed the database search. All the resulting titles were screened, and, if suitable, the abstract was accessed. The full text of the articles that matched the topic was accessed. If the full-text article was not available, the study was excluded from the present investigation. A cross-reference of the bibliography of the full-text articles was also performed. Disagreements between the authors were discussed and solved.
2.4. Data Items
Two authors (F.C. and K.E.) independently performed data extraction. Generalities and patient demographics of the included studies were retrieved at baseline: author and year, study design, length of follow-up, number of patients with related mean age, mean BMI, sex, Knee Scoring System (KSS) [29], and ROM. Data on ROM and on the following PROMs at last follow-up were retrieved: KSS and related function subscale (KSFS) [29] and Oxford Knee Score (OKS) [30]. Moreover, the rate of revision, deep infection, aseptic loosening, and fractures were also collected. The rate of patients who develop OA of the other knee compartment was also evaluated.
2.5. Study Risk of Bias Assessment
Two authors (F.C. and K.E.) independently performed the risk of bias assessment using the Review Manager (Rev.Man. 5.3, the Nordic Cochrane Collaboration, Copenhagen, Denmark). To evaluate the quality of the methodological assessment, the risk of bias graph was performed and evaluated. The following biases were evaluated: selection, detection, attrition, reporting, and others. To evaluate the overall risk of publication bias, a funnel plot of the most commonly reported outcome was performed. Asymmetries on the plot were associated with a greater risk of publication bias.
2.6. Synthesis Methods
All statistical analyses were performed by the first author (F.M.). For descriptive statistics, the IBM SPSS software was used. Mean and standard deviation were evaluated. For baseline comparability, the t-test was performed. Values of p > 0.1 indicated baseline comparability. For the meta-analyses, the Review Manager software version 5.3 (the Nordic Cochrane Collaboration, Copenhagen) was used. Continuous data were analysed using the inverse variance method and mean difference (MD) effect measure. Binary data were analysed using the Mantel–Haenszel method and the odds ratio (OR) effect measure. The comparisons were performed with a fixed model effect as set up. Heterogeneity was assessed through the 2 and Higgins-I2 tests. If the 2 < 0.05 and I2 tests > 50%, statistically significant moderate to high heterogeneity was detected, and a random model effect was adopted. The confidence intervals (CI) were set at 95% in all comparisons. The overall effect was considered statistically significant if p < 0.05. Forest and funnel plots were performed.
3. Results
3.1. Study Selection
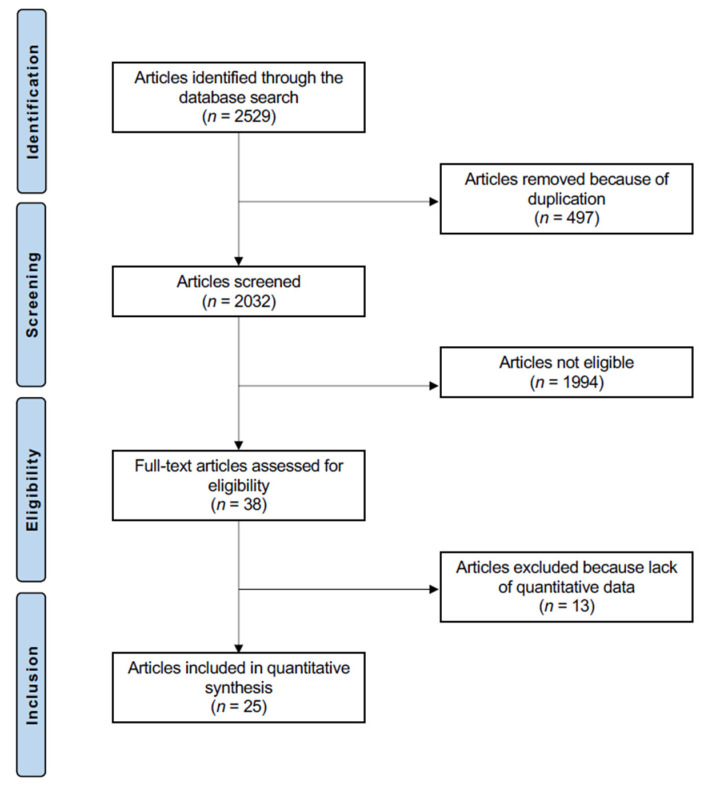
A total of 2529 papers were found in the initial literature search. Of them, 497 were excluded because of redundancy. A further 1994 articles were not eligible: not comparing mobile versus fixed bearing for UKA in a clinical setting (n = 1059), study type and design (n = 825), poor level of evidence (n = 31), experimental implants/protocols (n = 7), combining arthroplasty with other interventions (n = 11), combining unicompartmental and total knee arthroplasty (n = 4), other body regions (n = 37), missing information on sample size and follow-up (n = 8), language limitation (n = 9), and uncertain results (n = 3). Thirteen studies did not report any quantitative data under the outcome of interest and were excluded from the present investigation. Finally, 25 articles were included for analysis (Figure 1).
Figure 1.
Flow chart of the literature search.
3.2. Methodological Quality Assessment
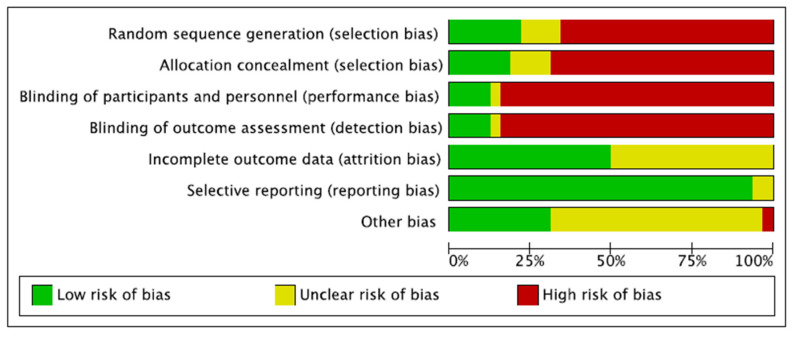
As only 20% (5 of 25) of the included studies performed a random allocation, the risk of selection bias was moderate to high. Performance and detection biases were also high, as assessors and patient blinding were seldom performed. Attrition and reporting biases were both low. The risk of other potential biases was moderate. Overall, the overall risk of bias was moderate (Figure 2).
Figure 2.
Risk of bias assessment. The risk of bias tool assessed the risk of bias (low, unclear, or high) per each risk of bias item presented as percentages across all included studies. The risk of selection bias evaluated the random sequence generation and the allocation concealment. The risk of detection bias assessed the blinding procedure during the outcome assessment. The risk of attrition bias refers to incomplete outcome data during study enrollment or analysis. The risk of reporting bias analyses the selective publication of results based on their statistical or clinical relevance. If the authors identified additional risks of bias, these were considered as “other bias”.
3.3. Risk of Publication Bias
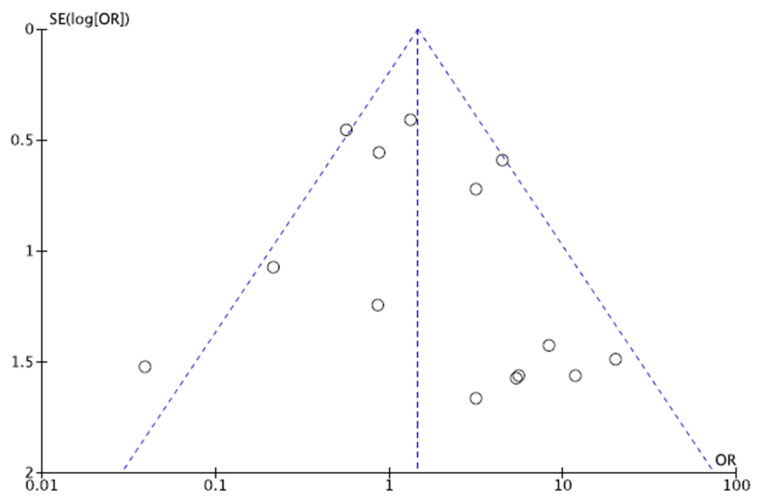
To assess the risk of publication bias, the funnel plot of the most commonly reported outcome (rate of revision) was performed. The plot evidenced adequate symmetry of the referral points. Egger’s test resulted in p = 0.3, attesting to this publication a low risk of publication bias. The funnel plot is shown in Figure 3.
Figure 3.
Funnel plot. The funnel plot charted the standard error (SE) of the log odds ratio (Log OR) versus its odd ratio. The degree of asymmetry of the plot is directly proportional to the degree of bias.
3.4. Study Characteristics and Results of Individual Studies
Data from 4696 patients were collected; 58% (2724 of 4696 patients) were women. The mean length of follow-up was 45.8 ± 43.2 months. The mean age of the patients was 65.0 ± 5.6 years. At baseline, comparability between the MB and FB groups was found in terms of mean age and BMI, sex, mean KSS, and ROM (p > 0.1). Study generalities and patient demographic at baseline are shown in greater detail in Table 1.
Table 1.
Generalities and patient baseline of the included studies (MB: mobile bearing; FB: fixed bearing).
| Author, Year | Journal | Design | Follow-Up (Months) | Bearing | Procedures (n) | Mean Age | Women (%) |
|---|---|---|---|---|---|---|---|
| Artz et al., 2015 [31] | J. Arthroplasty | Randomised | 24 | MB | 205 | 62.0 | 50% |
| FB | 284 | 71.4 | 44% | ||||
| Bhattacharya et al., 2012 [32] | Knee | Retrospective | 44.7 | FB | 91 | 67.7 | 58% |
| MB | 49 | 68.8 | 47% | ||||
| Biau et al., 2013 [33] | J. Arthroplasty | Retrospective | 24 | MB | 33 | 67.7 | 59% |
| FB | 57 | 68.8 | 51% | ||||
| Catani et al., 2011 [34] | Knee Surg Sports Traumatol Arthrosc | Retrospective | 12 | MB | 10 | 70.3 | 80% |
| FB | 10 | 70.3 | 60% | ||||
| Confalonieri et al., 2004 [13] | Knee | Randomised | 68.4 | MB | 20 | 71.0 | 45% |
| FB | 20 | 69.5 | 60% | ||||
| Emerson et al., 2002 [35] | Clin. Orthop. Relat. Res. | Prospective | 81.6 | MB | 50 | 63.0 | 56% |
| FB | 51 | 63.0 | 66% | ||||
| Forster et al., 2007 [36] | Knee Surg. Sports Traumatol. Arthrosc. | Prospective | 24 | FB | 17 | 75.0 | 69% |
| MB | 13 | 55.0 | 42% | ||||
| Gilmour et al., 2018 [23] | J. Arthroplasty | Prospective | 24 | FB | 58 | 61.8 | 45% |
| MB | 54 | 62.6 | 45% | ||||
| Gleeson et al., 2004 [37] | Knee | Randomised | 24 | FB | 57 | 66.7 | 41% |
| MB | 47 | 64.7 | 60% | ||||
| Inoue et al., 2016 [38] | J. Arthroplasty | Retrospective | 27.3 | FB | 24 | 75.0 | 76% |
| MB | 28 | 73.3 | 76% | ||||
| Kayani et al., 2019 [24] | Bone Joint J. | Prospective | 3 | MB | 73 | 66.1 | 53% |
| FB | 73 | 65.3 | 56% | ||||
| Kazarian et al., 2020 [25] | J. Bone Joint Surg. | Retrospective | 44.4 | FB | 162 | 63.2 | 59% |
| MB | 91 | 62.2 | 52% | ||||
| Kim et al., 2016 [39] | Knee Surg. Sports Traumatol. Arthrosc. | Retrospective | 94 | MB | 1441 | 62.0 62.0 | 91% 91% |
| FB | 135 | ||||||
| Kim et al., 2020 [26] | Int. Orthop. | Retrospective | 60 | FB | 58 | 61.3 | 93% |
| MB | 57 | 60.7 | 84% | ||||
| Koppens et al., 2019 [15] | Acta Orthop. | Randomised | 24 | MB | 33 | 64.0 | 52% |
| FB | 32 | 61.0 | 47% | ||||
| Li et al., 2006 [40] | Knee | Randomised | 24 | FB | 28 | 70.0 | 32% |
| MB | 28 | 74.0 | 29% | ||||
| Neufeld et al., 2018 [18] | J Arthroplasty | Retrospective | 120 | MB | 38 | 60.3 | 58% |
| FB | 68 | 64.6 | 50% | ||||
| Ozcan et al., 2018 [41] | Arch. Orthop. Trauma Surg. | Retrospective | 28.8 | FB | 153 | ||
| MB | 171 | ||||||
| Paratte et al., 2011 [42] | Clin. Orthop. Relat. Res. | Retrospective | 180 | FB | 79 | 62.8 | 63% |
| MB | 77 | 63.4 | 68% | ||||
| Patrick et al., 2020 [14] | J. Orthop. Surg. Res. | Retrospective | 14.4 | MB | 150 | 68.6 | 53% |
| FB | 44 | 67.7 | 86% | ||||
| Pronk et al., 2020 [43] | Knee Surg. Sports Traumatol. Arthrosc. | Retrospective | 12 | MB | 66 | 61.4 | 47% |
| FB | 97 | 61.2 | 44% | ||||
| Seo et al., 2019 [44] | Arch. Ortho.p Trauma Surg. | Retrospective | 120 | MB | 36 | 64.5 | 97% |
| FB | 60 | 61.8 | 95% | ||||
| Tecame et al., 2018 [45] | Int. Orthop. | Retrospective | 42 | MB | 9 | 47.8 | 17% |
| FB | 15 | 48.4 | |||||
| Verdini et al., 2017 [46] | Muscles Ligaments Tendons J. | Prospective | 20 | MB | 7 | 68.0 | 60% |
| FB | 8 | 67.0 | 40% | ||||
| Whittaker et al., 2010 [16] | Clin. Orthop. Relat. Res. | Retrospective | 3.6 | FB | 150 | 68.0 | 53% |
| MB | 79 | 63.0 | 48% |
3.5. Results of Syntheses
No difference was found in ROM (p = 0.05), KSS (p = 0.9), KSFS (p = 0.2), and OKS (p = 0.4). No difference was found in the rate of revision (p = 0.2), aseptic loosening (p = 0.9), deep infections (p = 0.99), fractures (p = 0.6), and further extension of OA to the contralateral joint compartment (p = 0.2). These results are shown in greater detail in Table 2.
Table 2.
Main results of the meta-analyses. The final effect was evaluated as odds ratio for binary data and as mean difference for continuous data (MB: mobile bearing; FB: fixed bearing; CI: confidence interval).
| Endpoint | MB | FB | Model | 95% CI | Final Effect | p | I2 (%) |
|---|---|---|---|---|---|---|---|
| ROM | 243 | 249 | Fixed | −4.37, −0.04 | −2.21 | 0.05 | 0 |
| KSS | 487 | 548 | Random | −6.38, 5.64 | −0.37 | 0.9 | 99 |
| KSFS | 176 | 241 | Fixed | −1.92, 0.31 | −0.81 | 0.2 | 0 |
| OKS | 97 | 95 | Random | −11.56, 4.44 | −3.56 | 0.4 | 95 |
| Revision | 2353 | 1148 | Random | 0.82, 3.20 | 1.62 | 0.2 | 52 |
| Aseptic Loosening | 1810 | 658 | Random | 0.16, 7.96 | 1.12 | 0.9 | 89 |
| Deep Infections | 1781 | 404 | Fixed | 0.28, 3.47 | 0.99 | 0.99 | 0 |
| Fractures | 1679 | 277 | Random | 0.08, 4.85 | 0.61 | 0.6 | 62 |
| OA Progression | 1752 | 602 | Fixed | 0.81, 2.60 | 1.45 | 0.2 | 3 |
4. Discussion
According to the main findings of the present study, MB implants performed in a similar fashion to FB implants for UKA. No difference was found in KSS, KSFS, OKS, ROM, and rate of complication.
Previous systematic reviews and meta-analyses that compared the two implants were not exhaustive, finding no clinically relevant differences in patient-reported outcome measures (PROMs), ROM, and rate of complication [8,9,16,17,18,19,20,21]. The present study updated current evidence, including recently published clinical investigations [22,23,24,25,26], investigating also additional endpoints that were not investigated by previous meta-analyses (ROM, KSFS, KOS). Ko et al. [19] included in a systematic review 1019 procedures (10 studies), finding a similar rate of complication between the two implants. Similar results were evidenced by Peersman et al. [8] in a systematic review of 9463 knees (44 studies). Cheng et al. [20] performed a meta-analysis involving 915 knees (nine studies). The authors found no difference in clinical outcomes and complication rates. Zhang et al. [9], in a recent meta-analysis involving 2612 procedures (14 studies), reported no difference in KSS, OKS, ROM, and complications. On the contrary, Burger et al. [21], in a systematic review including 2265 procedures (28 studies), concluded that MB reported a greater rate of revision compared to FB implants and similar clinical outcomes. The present study evidenced no difference between the two implant designs in the rate of revision, aseptic loosening, and OA progression. These results were confirmed by previous similar meta-analyses [16,17,18]. The most common reasons for revision following UKA implantation are aseptic loosening, progression of arthritis, and wear of the polyethylene insert [7,16,17,19]. Given their more congruent bearing surfaces with a larger contact area, MB implants have been introduced to reproduce better anatomic knee motion, minimise constraints, contact stress, and, thus, polyethylene wear [35,47,48,49]. These features should reduce implant loosening and polyethylene wear and favour longer MB implant survivorship [50,51]. However, suboptimal implant alignment and soft-tissue balancing can lead to bearing dislocation or impingement [37]. Indeed, MB implants are very sensitive to soft-tissue balancing [19]. Any undercorrection of the articular compartment promotes higher component stress contributing to polyethylene dislocation. On the other hand, any overcorrection promotes greater contact stress in the contralateral compartment, accelerating OA progression [4]. Given its flat tibial articular surface, FB implants are easier to implant, and the risk of bearing dislocation is minimal [35,49,52]. In this respect, FB implants could offload the contralateral compartment, slowing or preventing osteoarthritis progression [19]. The flat tibial component of FB implants, given their fatigue and shear-stress-related mechanism, are less compliant during flexion and can lead to point loading; hence, they are more prone to inlay surface deformation and delamination [53,54]. However, the results from the present study did not evidence any difference in the rate of OA progression between the two implants.
The present study certainly has limitations. The retrospective design of most of the included studies is an important limitation. Indeed, only 5 of 25 included studies performed randomised allocation, which represents an important source of selection bias. The limited length of the follow-up in many included studies represents another important limitation, which limits the reliability of the present investigation and jeopardises the ability to identify possible longer-term complications. The current literature lacks long-term randomised controlled trials, and future high-quality investigations are required. The postoperative rehabilitation protocol was seldom described, and the general health information of the included patients is often missing. Although the description of the surgical technique was adequately reported in most studies, the surgeon’s experience was barely stated. The latter may influence the clinical outcome, especially in MB implants, which require a longer learning curve and accurate soft-tissue balancing [55,56,57]; however, given the limited available data for inclusion, it was not possible to consider this endpoint for analysis. Given the lack of quantitative data, the analyses were conducted regardless of the type of the implant. Heterogeneities were found with regard to the implant manufacturers. Other studies did not specify which implant they used or combined two or more implants. Given these heterogeneities, no further analyses were possible to conduct. Given these limitations, results from the present study should be considered cautiously.
5. Conclusions
The present meta-analysis failed to identify the possible superiority of the MB implants over the FB for UKA in patients with monocompartmental knee osteoarthritis. Long observational investigations are required to evaluate possible long-term complications and implant survivorship. These results should be interpreted within the limitations of the present study.
Author Contributions
Conceptualization, F.M.; methodology, F.C., K.E. and F.M.; software, F.M.; validation, N.M., F.H. and J.E.; formal analysis, F.M.; data curation, F.M.; writing—original draft preparation, F.M., A.D.; writing—review and editing, F.M. and N.M.; supervision, J.E.; project administration, F.M.; All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
The datasets generated during and/or analysed during the current study are available throughout the manuscript.
Conflicts of Interest
The authors declare no conflict of interest.
Ethical Approval
This study complies with ethical standards.
Funding Statement
This research received no external funding.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Oliveria S.A., Felson D.T., Reed J.I., Cirillo P.A., Walker A.M. Incidence of symptomatic hand, hip and knee osteoarthritis among patients in a health maintenance organisation. Arthritis Rheum. 1995;38:1134–1144. doi: 10.1002/art.1780380817. [DOI] [PubMed] [Google Scholar]
- 2.Tille E., Beyer F., Auerbach K., Tinius M., Lutzner J. Better short-term function after unicompartmental compared to total knee arthroplasty. BMC Musculoskelet. Disord. 2021;22:326. doi: 10.1186/s12891-021-04185-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Panzram B., Bertlich I., Reiner T., Walker T., Hagmann S., Gotterbarm T. Cementless unicompartmental knee replacement allows early return to normal activity. BMC Musculoskelet. Disord. 2018;19:18. doi: 10.1186/s12891-017-1883-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kozinn S.C., Scott R. Unicondylar knee arthroplasty. J. Bone Jt. Surg. Am. 1989;71:145–150. doi: 10.2106/00004623-198971010-00023. [DOI] [PubMed] [Google Scholar]
- 5.Leiss F., Gotz J.S., Maderbacher G., Zeman F., Meissner W., Grifka J., Benditz A., Greimel F. Pain management of unicompartmental (UKA) vs. total knee arthroplasty (TKA) based on a matched pair analysis of 4144 cases. Sci. Rep. 2020;10:17660. doi: 10.1038/s41598-020-74986-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Argenson J.N. Unicompartmental knee arthroplasty versus total knee arthroplasty. Knee Surg. Sports Traumatol. Arthrosc. 2017;25:681–686. doi: 10.1007/s00167-015-3868-1. [DOI] [PubMed] [Google Scholar]
- 7.Migliorini F., Tingart M., Niewiera M., Rath B., Eschweiler J. Unicompartmental versus total knee arthroplasty for knee osteoarthritis. Eur. J. Orthop. Surg. Traumatol. 2019;29:947–955. doi: 10.1007/s00590-018-2358-9. [DOI] [PubMed] [Google Scholar]
- 8.Peersman G., Stuyts B., Vandenlangenbergh T., Cartier P., Fennema P. Fixed-versus mobile-bearing UKA: A systematic review and meta-analysis. Knee Surg. Sports Traumatol. Arthrosc. 2015;23:3296–3305. doi: 10.1007/s00167-014-3131-1. [DOI] [PubMed] [Google Scholar]
- 9.Zhang W., Wang J., Li H., Wang W., George D.M., Huang T. Fixed- versus mobile-bearing unicompartmental knee arthroplasty: A meta-analysis. Sci. Rep. 2020;10:19075. doi: 10.1038/s41598-020-76124-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Capella M., Dolfin M., Saccia F. Mobile bearing and fixed bearing total knee arthroplasty. Ann. Transl. Med. 2016;4:127. doi: 10.21037/atm.2015.12.64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Schneider D.T., Ostermeier P.S., Rinio D.M., Marquaß P.D.B. Fixed vs Mobile Bearing Prothesis. [(accessed on 1 January 2022)]. Available online: https://www.joint-surgeon.com/orthopedic-services/knee/total-replacement-knee-types-of-procedures.
- 12.Huang F., Wu D., Chang J., Zhang C., Qin K., Liao F., Yin Z. A Comparison of Mobile- and Fixed-Bearing Unicompartmental Knee Arthroplasties in the Treatment of Medial Knee Osteoarthritis: A Systematic Review and Meta-analysis of 1861 Patients. J. Knee Surg. 2021;34:434–443. doi: 10.1055/s-0039-1697901. [DOI] [PubMed] [Google Scholar]
- 13.Confalonieri N., Manzotti A., Pullen C. Comparison of a mobile with a fixed tibial bearing unicompartimental knee prosthesis: A prospective randomized trial using a dedicated outcome score. Knee. 2004;11:357–362. doi: 10.1016/j.knee.2004.01.003. [DOI] [PubMed] [Google Scholar]
- 14.Ng J.P., Fan J.C.H., Lau L.C.M., Tse T.T.S., Wan S.Y.C., Hung Y.W. Can accuracy of component alignment be improved with Oxford UKA Microplasty(R) instrumentation? J. Orthop. Surg. Res. 2020;15:354. doi: 10.1186/s13018-020-01868-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Koppens D., Rytter S., Munk S., Dalsgaard J., Sorensen O.G., Hansen T.B., Stilling M. Equal tibial component fixation of a mobile-bearing and fixed-bearing medial unicompartmental knee arthroplasty: A randomized controlled RSA study with 2-year follow-up. Acta Orthop. 2019;90:575–581. doi: 10.1080/17453674.2019.1639965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Whittaker J.P., Naudie D.D., McAuley J.P., McCalden R.W., MacDonald S.J., Bourne R.B. Does bearing design influence midterm survivorship of unicompartmental arthroplasty? Clin. Orthop. Relat. Res. 2010;468:73–81. doi: 10.1007/s11999-009-0975-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bruce D.J., Hassaballa M., Robinson J.R., Porteous A.J., Murray J.R., Newman J.H. Minimum 10-year outcomes of a fixed bearing all-polyethylene unicompartmental knee arthroplasty used to treat medial osteoarthritis. Knee. 2020;27:1018–1027. doi: 10.1016/j.knee.2020.02.018. [DOI] [PubMed] [Google Scholar]
- 18.Neufeld M.E., Albers A., Greidanus N.V., Garbuz D.S., Masri B.A. A Comparison of Mobile and Fixed-Bearing Unicompartmental Knee Arthroplasty at a Minimum 10-Year Follow-up. J. Arthroplast. 2018;33:1713–1718. doi: 10.1016/j.arth.2018.01.001. [DOI] [PubMed] [Google Scholar]
- 19.Ko Y.B., Gujarathi M.R., Oh K.J. Outcome of Unicompartmental Knee Arthroplasty: A Systematic Review of Comparative Studies between Fixed and Mobile Bearings Focusing on Complications. Knee Surg. Relat. Res. 2015;27:141–148. doi: 10.5792/ksrr.2015.27.3.141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cheng T., Chen D., Zhu C., Pan X., Mao X., Guo Y., Zhang X. Fixed- versus mobile-bearing unicondylar knee arthroplasty: Are failure modes different? Knee Surg. Sports Traumatol. Arthrosc. 2013;21:2433–2441. doi: 10.1007/s00167-012-2208-y. [DOI] [PubMed] [Google Scholar]
- 21.Burger J.A., Kleeblad L.J., Sierevelt I.N., Horstmann W.G., Nolte P.A. Bearing design influences short- to mid-term survivorship, but not functional outcomes following lateral unicompartmental knee arthroplasty: A systematic review. Knee Surg. Sports Traumatol. Arthrosc. 2019;27:2276–2288. doi: 10.1007/s00167-019-05357-x. [DOI] [PubMed] [Google Scholar]
- 22.Deckard E.R., Jansen K., Ziemba-Davis M., Sonn K.A., Meneghini R.M. Does Patellofemoral Disease Affect Outcomes in Contemporary Medial Fixed-Bearing Unicompartmental Knee Arthroplasty? J. Arthroplast. 2020;35:2009–2015. doi: 10.1016/j.arth.2020.03.007. [DOI] [PubMed] [Google Scholar]
- 23.Gilmour A., MacLean A., Rowe P., Banger M., Donnelly I., Jones B., Blyth M. Robotic-Arm Assisted Versus Conventional Unicompartmental Knee Arthroplasty. The 2 year Results of a Randomised Controlled Trial. J. Arthroplast. 2018;33:S109–S115. doi: 10.1016/j.arth.2018.02.050. [DOI] [PubMed] [Google Scholar]
- 24.Kayani B., Konan S., Tahmassebi J., Rowan F.E., Haddad F.S. An assessment of early functional rehabilitation and hospital discharge in conventional versus robotic-arm assisted unicompartmental knee arthroplasty: A prospective cohort study. Bone Jt. J. 2019;101:24–33. doi: 10.1302/0301-620X.101B1.BJJ-2018-0564.R2. [DOI] [PubMed] [Google Scholar]
- 25.Kazarian G.S., Barrack T.N., Okafor L., Barrack R.L., Nunley R.M., Lawrie C.M. High Prevalence of Radiographic Outliers and Revisions with Unicompartmental Knee Arthroplasty. J. Bone Jt. Surg. Am. 2020;102:1151–1159. doi: 10.2106/JBJS.19.01277. [DOI] [PubMed] [Google Scholar]
- 26.Kim M.S., Koh I.J., Kim C.K., Choi K.Y., Baek J.W., In Y. Comparison of implant position and joint awareness between fixed- and mobile-bearing unicompartmental knee arthroplasty: A minimum of five year follow-up study. Int. Orthop. 2020;44:2329–2336. doi: 10.1007/s00264-020-04662-2. [DOI] [PubMed] [Google Scholar]
- 27.Howick J.C.I., Glasziou P., Greenhalgh T., Carl Heneghan Liberati A., Moschetti I., Phillips B., Thornton H., Goddard O., Hodgkinson M. The 2011 Oxford CEBM Levels of Evidence. Oxford Centre for Evidence-Based Medicine. 2011. [(accessed on 1 January 2022)]. Available online: https://www.cebm.net/index.aspx?o=5653.
- 28.Page M.J., McKenzie J.E., Bossuyt P.M., Boutron I., Hoffmann T.C., Mulrow C.D., Shamseer L., Tetzlaff J.M., Akl E.A., Brennan S.E., et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. doi: 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Insall J.N., Dorr L.D., Scott R.D., Scott W.N. Rationale of the Knee Society clinical rating system. Clin. Orthop. Relat. Res. 1989;248:13–14. doi: 10.1097/00003086-198911000-00004. [DOI] [PubMed] [Google Scholar]
- 30.Murray D.W., Fitzpatrick R., Rogers K., Pandit H., Beard D.J., Carr A.J., Dawson J. The use of the Oxford hip and knee scores. J. Bone Jt. Surg. Br. 2007;89:1010–1014. doi: 10.1302/0301-620X.89B8.19424. [DOI] [PubMed] [Google Scholar]
- 31.Artz N.J., Hassaballa M.A., Robinson J.R., Newman J.H., Porteous A.J., Murray J.R. Patient Reported Kneeling Ability in Fixed and Mobile Bearing Knee Arthroplasty. J. Arthroplast. 2015;30:2159–2163. doi: 10.1016/j.arth.2015.06.063. [DOI] [PubMed] [Google Scholar]
- 32.Bhattacharya R., Scott C.E., Morris H.E., Wade F., Nutton R.W. Survivorship and patient satisfaction of a fixed bearing unicompartmental knee arthroplasty incorporating an all-polyethylene tibial component. Knee. 2012;19:348–351. doi: 10.1016/j.knee.2011.04.009. [DOI] [PubMed] [Google Scholar]
- 33.Biau D.J., Greidanus N.V., Garbuz D.S., Masri B.A. No difference in quality-of-life outcomes after mobile and fixed-bearing medial unicompartmental knee replacement. J. Arthroplast. 2013;28:220–226.e221. doi: 10.1016/j.arth.2012.05.017. [DOI] [PubMed] [Google Scholar]
- 34.Catani F., Benedetti M.G., Bianchi L., Marchionni V., Giannini S., Leardini A. Muscle activity around the knee and gait performance in unicompartmental knee arthroplasty patients: A comparative study on fixed- and mobile-bearing designs. Knee Surg. Sports Traumatol. Arthrosc. 2012;20:1042–1048. doi: 10.1007/s00167-011-1620-z. [DOI] [PubMed] [Google Scholar]
- 35.Emerson R.H., Jr., Hansborough T., Reitman R.D., Rosenfeldt W., Higgins L.L. Comparison of a mobile with a fixed-bearing unicompartmental knee implant. Clin. Orthop. Relat. Res. 2002;404:62–70. doi: 10.1097/00003086-200211000-00011. [DOI] [PubMed] [Google Scholar]
- 36.Forster M.C., Bauze A.J., Keene G.C. Lateral unicompartmental knee replacement: Fixed or mobile bearing? Knee Surg. Sports Traumatol. Arthrosc. 2007;15:1107–1111. doi: 10.1007/s00167-007-0345-5. [DOI] [PubMed] [Google Scholar]
- 37.Gleeson R.E., Evans R., Ackroyd C.E., Webb J., Newman J.H. Fixed or mobile bearing unicompartmental knee replacement? A comparative cohort study. Knee. 2004;11:379–384. doi: 10.1016/j.knee.2004.06.006. [DOI] [PubMed] [Google Scholar]
- 38.Inoue A., Arai Y., Nakagawa S., Inoue H., Yamazoe S., Kubo T. Comparison of Alignment Correction Angles Between Fixed-Bearing and Mobile-Bearing UKA. J. Arthroplast. 2016;31:142–145. doi: 10.1016/j.arth.2015.07.024. [DOI] [PubMed] [Google Scholar]
- 39.Kim K.T., Lee S., Lee J.I., Kim J.W. Analysis and Treatment of Complications after Unicompartmental Knee Arthroplasty. Knee Surg. Relat. Res. 2016;28:46–54. doi: 10.5792/ksrr.2016.28.1.46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Li M.G., Yao F., Joss B., Ioppolo J., Nivbrant B., Wood D. Mobile vs. fixed bearing unicondylar knee arthroplasty: A randomized study on short term clinical outcomes and knee kinematics. Knee. 2006;13:365–370. doi: 10.1016/j.knee.2006.05.003. [DOI] [PubMed] [Google Scholar]
- 41.Ozcan C., Simsek M.E., Tahta M., Akkaya M., Gursoy S., Bozkurt M. Fixed-bearing unicompartmental knee arthroplasty tolerates higher variance in tibial implant rotation than mobile-bearing designs. Arch. Orthop. Trauma Surg. 2018;138:1463–1469. doi: 10.1007/s00402-018-3005-y. [DOI] [PubMed] [Google Scholar]
- 42.Parratte S., Pauly V., Aubaniac J.M., Argenson J.N. No long-term difference between fixed and mobile medial unicompartmental arthroplasty. Clin. Orthop. Relat. Res. 2012;470:61–68. doi: 10.1007/s11999-011-1961-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Pronk Y., Paters A.A.M., Brinkman J.M. No difference in patient satisfaction after mobile bearing or fixed bearing medial unicompartmental knee arthroplasty. Knee Surg. Sports Traumatol. Arthrosc. 2021;29:947–954. doi: 10.1007/s00167-020-06053-x. [DOI] [PubMed] [Google Scholar]
- 44.Seo S.S., Kim C.W., Lee C.R., Kwon Y.U., Oh M., Kim O.G., Kim C.K. Long-term outcomes of unicompartmental knee arthroplasty in patients requiring high flexion: An average 10-year follow-up study. Arch. Orthop. Trauma Surg. 2019;139:1633–1639. doi: 10.1007/s00402-019-03268-7. [DOI] [PubMed] [Google Scholar]
- 45.Tecame A., Savica R., Rosa M.A., Adravanti P. Anterior cruciate ligament reconstruction in association with medial unicompartmental knee replacement: A retrospective study comparing clinical and radiological outcomes of two different implant design. Int. Orthop. 2019;43:2731–2737. doi: 10.1007/s00264-019-04341-x. [DOI] [PubMed] [Google Scholar]
- 46.Verdini F., Zara C., Leo T., Mengarelli A., Cardarelli S., Innocenti B. Assessment of patient functional performance in different knee arthroplasty designs during unconstrained squat. Muscle Ligaments Tendons J. 2017;7:514–523. doi: 10.11138/mltj/2017.7.3.514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Smith T.O., Hing C.B., Davies L., Donell S.T. Fixed versus mobile bearing unicompartmental knee replacement: A meta-analysis. Orthop. Traumatol. Surg. Res. 2009;95:599–605. doi: 10.1016/j.otsr.2009.10.006. [DOI] [PubMed] [Google Scholar]
- 48.Ammarullah M.I., Afif I.Y., Maula M.I., Winarni T.I., Tauviqirrahman M., Akbar I., Basri H., van der Heide E., Jamari J. Tresca Stress Simulation of Metal-on-Metal Total Hip Arthroplasty during Normal Walking Activity. Materials. 2021;14:7554. doi: 10.3390/ma14247554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Jamari J., Ammarullah M.I., Saad A.P.M., Syahrom A., Uddin M., van der Heide E., Basri H. The Effect of Bottom Profile Dimples on the Femoral Head on Wear in Metal-on-Metal Total Hip Arthroplasty. J. Funct. Biomater. 2021;12:38. doi: 10.3390/jfb12020038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.O’Connor J.J., Goodfellow J.W. Theory and practice of meniscal knee replacement: Designing against wear. Proc. Inst. Mech. Eng. Part H. 1996;210:217–222. doi: 10.1243/PIME_PROC_1996_210_415_02. [DOI] [PubMed] [Google Scholar]
- 51.Kendrick B.J., Longino D., Pandit H., Svard U., Gill H.S., Dodd C.A., Murray D.W., Price A.J. Polyethylene wear in Oxford unicompartmental knee replacement: A retrieval study of 47 bearings. J. Bone Jt. Surg. Br. 2010;92:367–373. doi: 10.1302/0301-620X.92B3.22491. [DOI] [PubMed] [Google Scholar]
- 52.Brockett C.L., Jennings L.M., Fisher J. The wear of fixed and mobile bearing unicompartmental knee replacements. Proc. Inst. Mech. Eng. Part H. 2011;225:511–519. doi: 10.1177/2041303310393824. [DOI] [PubMed] [Google Scholar]
- 53.Argenson J.N., Parratte S. The unicompartmental knee: Design and technical considerations in minimizing wear. Clin. Orthop. Relat. Res. 2006;452:137–142. doi: 10.1097/01.blo.0000229358.19867.60. [DOI] [PubMed] [Google Scholar]
- 54.Manson T.T., Kelly N.H., Lipman J.D., Wright T.M., Westrich G.H. Unicondylar knee retrieval analysis. J. Arthroplast. 2010;25:108–111. doi: 10.1016/j.arth.2010.05.004. [DOI] [PubMed] [Google Scholar]
- 55.Zambianchi F., Digennaro V., Giorgini A., Grandi G., Fiacchi F., Mugnai R., Catani F. Surgeon’s experience influences UKA survivorship: A comparative study between all-poly and metal back designs. Knee Surg. Sports Traumatol. Arthrosc. 2015;23:2074–2080. doi: 10.1007/s00167-014-2958-9. [DOI] [PubMed] [Google Scholar]
- 56.Ridgeway S.R., McAuley J.P., Ammeen D.J., Engh G.A. The effect of alignment of the knee on the outcome of unicompartmental knee replacement. J. Bone Jt. Surg. Br. 2002;84:351–355. doi: 10.1302/0301-620X.84B3.0840351. [DOI] [PubMed] [Google Scholar]
- 57.Robertsson O., Knutson K., Lewold S., Lidgren L. The routine of surgical management reduces failure after unicompartmental knee arthroplasty. J. Bone Jt. Surg. Br. 2001;83:45–49. doi: 10.1302/0301-620X.83B1.0830045. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated during and/or analysed during the current study are available throughout the manuscript.