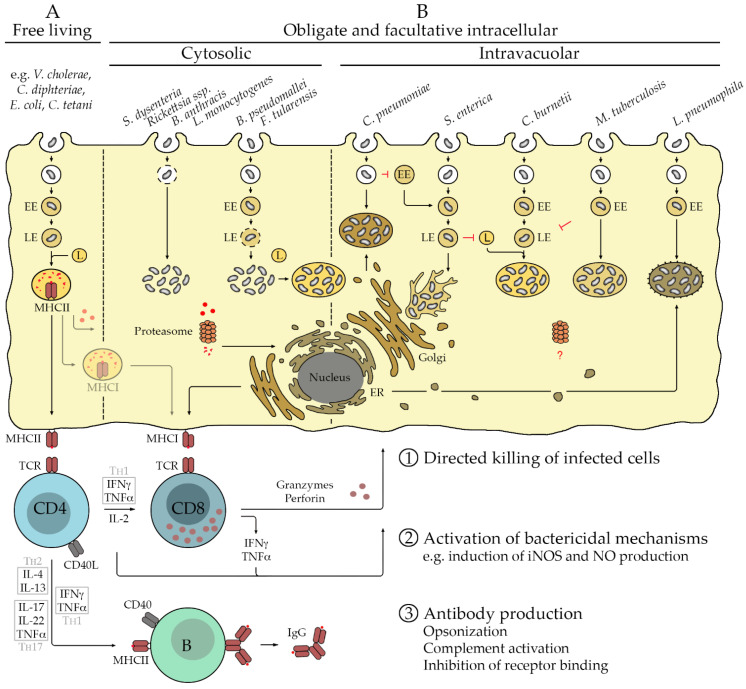
Figure 1.
Extra- and intracellular bacteria and immune response. Free-living bacteria are taken up by phagocytes such as MØ and DCs as well as B cells that serve as professional antigen-presenting cells (APCs). Phagosomes develop into early endosomes (EE) and further to late endosomes (LE) that finally fuse with lysosomes (L). The activity of proteases and acidic environments of the Ls results in the degradation of the pathogen and its proteins, fragments of which are bound by MHCII molecules in the lysosomal membrane. MHCII/peptide complexes are presented on the cell surface to CD4+ T cells. The protective immune response is dominated by activated CD4+ T cells as well as B cells that produce antibodies against surface molecules of the pathogen. Depending on the cytokine environment provided by the APC, CD4+ T cells develop to T helper (TH) cells, either to TH2 cells producing IL-4 and IL-13, TH1 cells that secrete IFNγ and TNFα, or TH17 cells releasing IL-17, TNFα, and IL-22 that acts on non-immune cells. All TH cells also release IL-2, which promotes T cell proliferation and survival. Activated TH cells interact with activated B cells via the binding of CD40L to CD40 on the B cell surface, initiating the germinal center reaction where immunoglobulin class switch and affinity maturation occurs, so that high-affinity IgG instead of the initial IgM is produced. In addition, memory B cells develop. The cytokines that are produced by different TH cells promote the generation of certain IgG isotypes in this process. Antibodies can act against extracellular bacteria by opsonization for the uptake by phagocytes or direct destruction of the pathogen by complement activation. (A). Only a few bacteria replicate exclusively within target cells. These include members of the family of Rickettsiacea, Chlamydia (C.) pneumoniae, and Coxiella (C.) burnetii. Rickettsiae escape from the phagosome via the release of phospholipases that dissolve the phagosomal membrane and replicate free in the cytosol [6]. C. pneumoniae, instead, leaves the endocytic route and recruits Golgi-derived vesicles to form a unique compartment for replication that is associated with the microtubule organizing center (MTOC) [7]. Phagosomes containing C. burnetii, in turn, fuse with Ls to build a phagolysosomal-like vacuole for bacterial replication. Several other bacteria are facultative intracellular pathogens. Examples are B. anthracis, L. monocytogenes, B. pseudomallei, F. tularensis, S. enterica, M. tuberculosis, and L. pneumophila. Similar to rickettsiae, B. anthracis infects macrophages (MØ) and escapes from the phagosome to replicate free in the cytosol. L. monocytogenes, B. pseudomalleii, and F. tularensis deliberate from LEs and then also replicate free in the cytosol of infected cells. Cytosolic F. tularensis may also retranslocate into autolysosome-like vacuoles. In contrast, S. enterica inhibits fusion of LEs with Ls and replicates in LE-like compartments that are associated with the MTOC and form filaments [8]. M. tuberculosis inhibits maturation of EEs and replicates in LE-like vacuoles, while EEs containing L. pneumophila fuse with vesicles derived from the ER to form ribosome-coated compartments for bacterial replication [9]. (B). Efficient defense against intracellular pathogens usually requires the activation of cytotoxic CD8+ T cells that are capable of the direct killing of infected cells. CD8+ T cells are activated by antigenic peptides that derive from cytosolic proteins that are degraded by the proteasome. Peptides are transferred to the ER to be loaded onto MHCI molecules that are presented on the cell surface of all nucleated cells to be recognized by CD8+ T cells. Bacterial antigens that are recognized by CD8+ T cells may derive predominantly from secreted proteins or surface proteins that are accessible for proteasomal degradation in the cytosol ①. Initial activation of CD8+ T cells and defense against intracellular bacteria further require the activation of CD4+ T cells, predominantly of the TH1 type. These cells support CD8+ T cell responses. In addition, CD4+ TH1 cells (as well as TH17 cells and IFNγ-releasing CD8+ T cells) induce bactericidal mechanisms such as the induction of nitric oxide synthase (iNOS) and NO production in infected cells via the release of IFNγ and TNFα. In this way, CD4+ TH1 cells contribute to bacterial elimination ②. Antibodies produced by B cells may play a minor role in the defense against primary infection with intracellular bacteria but can contribute to protection in secondary infection. In addition to the aforementioned mechanisms, antibodies can here participate in defense by the inhibition of the binding of the bacteria to receptors that mediate bacterial uptake into target cells ③. For those bacteria that replicate within cellular compartments and thus are hidden from the cytosol and the proteasome, the activation of CD8+ T cell responses during the infection may not be efficient.