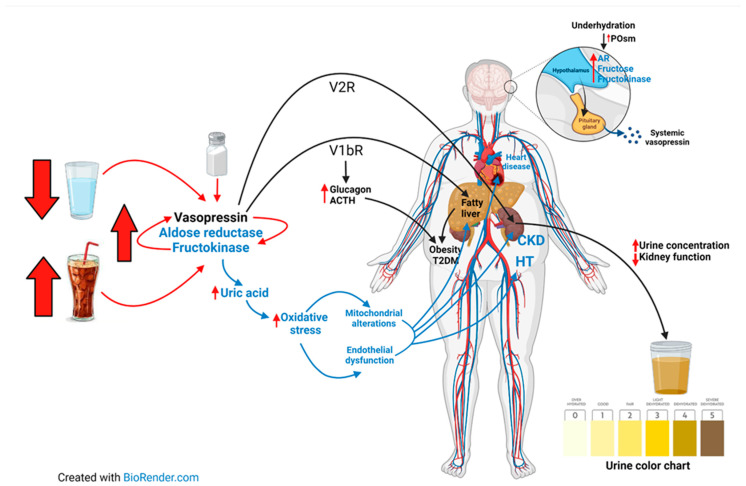
Figure 1.
Low water intake coupled with sugar-sweetened beverage (SSB) intake activate both vasopressin and the aldose reductase-fructokinase pathways, which also can synergize with each other, aggravating target organ damage. In the brain, milder increases in systemic osmolality due to dehydration induce the expression of the aldose reductase pathway in the supraoptic nuclei of the hypothalamus, followed by the production of fructose. In turn, the fructose is metabolized locally by fructokinase, driving the synthesis of vasopressin. The increased vasopressin activity stimulates V2R in the kidney, inducing urine concentration and chronically renal alterations. Stimulation of the V1b receptor occurs in the pancreatic islets as well as in the liver and the anterior pituitary, thereby stimulating the secretion of glucagon and the adrenocorticotropic hormone. V1bR stimulation also mediates fat production and other features of metabolic syndrome, such as fatty liver, obesity, and eventually, type 2 diabetes. Aldose reductase-fructokinase pathway activation induces an increase in uric acid synthesis which induces intracellular oxidative stress, mitochondrial alterations, and endothelial dysfunction. This eventually results in target organ damage, the organs that are more affected being the liver (fatty liver), heart (heart failure), kidney (chronic kidney disease) and the vessels (hypertension). High salt intake may lead to an increase in serum osmolality, thereby inducing chronic underhydration, activating both the polyol-fructose and vasopressin pathways. (Abbreviations: ACTH, adrenocorticotropic hormone; AR, aldose reductase; CKD, chronic kidney disease; HT, hypertension; POsm, Plasma osmolality; T2DM, type 2 diabetes mellitus).