Abstract
Invasive aspergillosis (IA) is a life-threatening fungal disease that causes high morbidity and mortality in immunosuppressed patients. Early and accurate diagnosis and treatment of IA remain challenging. Given the broad range of non-specific clinical symptoms and the shortcomings of current diagnostic techniques, most patients are either diagnosed as “possible” or “probable” cases but not “proven”. Moreover, because of the lack of sensitive and specific tests, many high-risk patients receive an empirical therapy or a prolonged treatment of high-priced antifungal agents, leading to unnecessary adverse effects and a high risk of drug resistance. More precise diagnostic techniques alongside a targeted antifungal treatment are fundamental requirements for reducing the morbidity and mortality of IA. Monoclonal antibodies (mAbs) with high specificity in targeting the corresponding antigen(s) may have the potential to improve diagnostic tests and form the basis for novel IA treatments. This review summarizes the up-to-date application of mAb-based approaches in assisting IA diagnosis and therapy.
Keywords: monoclonal antibody, invasive aspergillosis, Aspergillus infection, diagnosis, therapy
1. Introduction
Invasive aspergillosis (IA), the most devastating form of Aspergillus infection, refers to an opportunistic, life-threatening, acute and rapidly progressing infectious disease [1]. IA is predominately caused by Aspergillus fumigatus, which is ubiquitous within our environment. Other Aspergillus species such as Aspergillus flavus, Aspergillus niger, Aspergillus terreus and Aspergillus nidulans can also cause IA [2]. IA usually occurs in immunosuppressed patients, including neutropenic hosts, patients undergoing prolonged treatment with corticosteroids, and allogeneic hematopoietic stem cell transplant (HSCT) and solid organ transplant (SOT) recipients [3,4]. With delayed diagnosis, the mortality of IA in immunodeficient hosts can be high as 90%.
The increasing number of immunodeficient patients due to immune suppressive therapy accounts for the growth in IA numbers. Globally, IA causes in excess of 200,000 mortal infections every year [5,6]. Additionally, patients suffering from IA have an increased risk of complications from viral infections such as influenza and COVID-19 [7,8]. IA cases secondary to viral infections have complex clinical presentations leading to further difficulty and delays in diagnosis and therapy [9,10]. Accurate diagnosis and a targeted antifungal treatment are the fundamental requirements for reducing both the morbidity and mortality of IA.
Monoclonal antibodies (mAbs), produced by a single B-lymphocyte clone, have high specificity in targeting the corresponding antigen(s) and have the potential to improve diagnostic tests, forming the basis for novel IA treatments. MAbs have been developed for diagnosis and therapy of cancers [11,12], autoimmune disease [13], asthma [14] and infectious diseases [15,16] including COVID-19 [17,18] but have yet to reach their full potential for improving the outcomes of IA. This review examines the potential usefulness of mAbs in diagnosing and treating IA from different perspectives.
2. Pathogenesis of Invasive Aspergillosis
The conidia of the Aspergillus species that causes IA are small (approximately 2.5–3.5 μm in diameter), and covered in a hydrophobic layer. They are very robust under normal atmospheric conditions, and can remain airborne, dispersing widely on air currents after release [19], and can be inhaled unless removed by physical filtration [20,21]. Healthy hosts clear inhaled conidia that become trapped in the mucociliary escalator effectively, and the immunological cellular defences clear those that penetrate as far as the alveoli [21,22,23]. In contrast, the conidia can escape clearance from the respiratory tract in immunodeficient patients.
After inhalation, the hydrophobic exterior protein cover and melanin protect the conidia from being recognized and attacked by the host by masking of the pathogen-associated molecular patterns (PAMPs) [21,24,25,26]. Conidial constituents that mediate the adherence and colonization to the host epithelial cells include conidial sialic acid residues [27,28] and fucose-specific lectin A [29]. Subsequently, surviving conidia start to swell and release surface hydrophobin and melanin, exposing PAMPs that interact with pattern recognition receptors (PRRs) on pulmonary epithelial cells. Conidial wall β (1-3)-glucan is recognized by dectin-1 and initiates engulfment by epithelia [30]. This internalization process is promoted by the interaction of conidial calcineurin A (Cal A) and integrin α5β1 [31] and the activation of cellular molecules [32,33,34]. Engulfment of conidia induces the inflammatory response in the epithelia. Most conidia are killed during this offensive response; however, the conidia that escape phagocytosis continue to swell and germinate into filamentous hyphae. Galactosaminogalactan (GAG), a soluble molecule secreted by the hyphae, mediates the fungal attachment to the host pulmonary epithelial cells [35,36]. In addition, GAG production around the hyphae leads to the reduction of β (1-3)-glucan exposure. This blocks the interaction between the β (1-3)-glucan and the dectin-1, which attenuates the inflammatory responses and fungal death [35]. GAG also has been shown to induce neutrophil apoptosis, inhibit the formation of neutrophil extracellular traps (NETs) termed NETosis and pre-inflammation, so as to protect the Aspergillus from killing [23,37,38].
Hyphae invading host tissues grow quickly with an extension rate of 20.2 to 25.4 μm/h [39], and release proteases such as cysteine and serine protease, metalloproteinase, and elastase that degrade the host epithelial tissue and generate nutrients that support further fungal growth [40,41]. Aspergillus hyphae express and secrete multiple mycotoxins that aggravate the damage to host pulmonary cells and basement membrane [42] or affect the host immunity [43]. Of these, gliotoxin facilitates the internalization of Aspergillus conidia by type II human pneumocyte cells [33] and prohibits the host’s immune response by inducing apoptosis in macrophages and monocytes [43,44,45]. Fumagillin is cytotoxic to lymphocytes, leading to cellular immune suppression [46,47]. It also causes destruction of the pulmonary tissue and promotes fungal growth [48]. These virulence factors have the dual properties of disrupting the host’s immune system and facilitating fungal growth, leading to hyphae crossing endothelial barriers and invading blood vessels. This process may lead to rapid dissemination and colonization of remote tissues and organs, resulting in the histologically typical features of IA lesions that are characterised by tissue injury, necrosis and hypoxia [22].
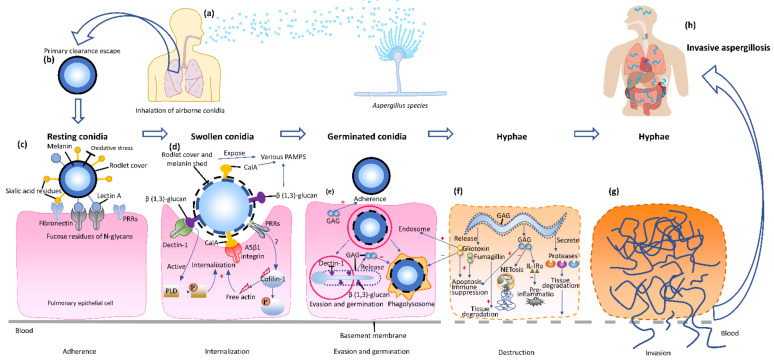
In summary, airborne Aspergillus conidia reach the airways by inhalation, but hyphae are the invasive fungal form in human infections. Aspergillus cell wall components facilitate the adherence and induce endocytosis by host cells. The proteases released by Aspergillus hyphae promote the remote invasion of the parenchyma and blood vessels. Various toxins co-impede the immune system function of the individuals and aggravate the severity of IA (Figure 1).
Figure 1.
The pathogenesis of invasive aspergillosis. (a) Inhalation. Airborne conidia are inhaled into the respiratory system of the immunosuppressed host. (b) Clearance escape. The resting conidia escape primary clearance and immune attack. (c) Adherence. The rodlet protein cover and melanin of the resting conidia mask the pathogen-associated molecular patterns (PAMPs) and protect the conidia from oxidative stress and the environment (UV) and host (reactive oxygen species, ROS), and from being recognized and attacked by the host. Lectin A and sialic acid residues mediate the adherence and colonization onto the fucose residues of N-glycans and fibronectin of the pulmonary epithelial cells. (d) Internalization. The swollen conidia release the surface hydrophobic layer and melanin, exposing more PAMPs, such as β (1-3)-glucan and calcineurin A (Cal A), to be recognized by dectin-1 and integrin α5β1, respectively, on the epithelial cell wall, inducing the internalization. In addition, the formation of actin polymerization and activation of phospholipase D (PLD) both boost the internalization. (e) Evasion and germination. The swollen conidia in the endosome evade the phagolysosome killing and germinate into tubes and hyphae. Galactosaminogalactan (GAG) on the hyphae wall can be released as a soluble molecule, mediating adhesion, inhibiting phagocytosis and suppressing the host inflammatory responses by masking of β (1,3)-glucan on the hyphal wall. (f) Destruction. GAG released by mature hyphae facilitates the induction of neutrophil apoptosis and prohibits formation of neutrophil extracellular traps (NETosis), and pre-inflammation by induction of IL-IRa. The secreted gliotoxin and fumagillin are involved in pathogen internalization, cell apoptosis, host immune inhibition and tissue degradation. (g) Invasive aspergillosis. The tissue-invasive hyphae penetrate the alveolar epithelia and basement membrane into the blood vessel, disseminating to the whole body and causing IA (h). +: promote; −: inhibit.
3. Monoclonal Antibodies and Diagnosis of Invasive Aspergillosis
3.1. Challenges of Invasive Aspergillosis Diagnosis
The early and accurate diagnosis of IA is a major challenge because there are a broad range of non-specific clinical symptoms, such as cough, fever, chills, dyspnea, hemoptysis, chest pains, headaches, and weight loss associated with IA [21,49]. A full range of diagnostic methods have been evaluated for IA (Table 1). The current consensus, from the European Organization for Research and Treatment of Cancer and the Mycoses Study Group Education and Research Consortium (EORTC/MSGERC) [50], establishes the identification of Aspergillus in biopsy tissue samples, or a positive culture of pathogens from a specimen taken from a normally sterile site as the gold standard for diagnosis of IA. In immunosuppressed patients, particularly those with neutropenia and thrombocytopenia, the invasive procedures needed to obtain tissue samples are hazardous, thereby limiting their availability [21,51]. Consequently, most patients are either diagnosed as “possible” or “probable” cases but not “proven” because of the shortcomings of the diagnostic techniques currently available [50,52,53]. The criteria for a “probable” IA diagnosis require the presence of a host factor, which is usually immune suppression, clinical features such as fever unresponsive to antibacterial treatment, and mycologic detection. Those who meet the criteria for a host factor and a clinical characteristic but without mycological evidence should be considered as “possible” IA cases.
Table 1.
Advantages and disadvantages of classical diagnostic methods for IA.
| Diagnostic Methods | Advantages | Disadvantages |
|---|---|---|
| Histopathology and microbiology | Gold standard Pathologic changes of the tissue Morphology of the Aspergillus |
Invasive operation High requirements for specimen quality Technology dependent on the technician Time-consuming False-negative |
| Fungal biomarker assay | Early detection Non-invasive Various sample resources Platform widely available Rapid turnaround time |
False-positive False-negative Unknown pathogen species Unknown infection site |
| Aspergillus polymerase chain reaction (PCR) test | Specific species Various sample resources Rapid turnaround time |
Lack of standardization Contamination can be problematic |
| CT scanning | Fast and non-invasive Location of infection site Lesion size and number |
Non-specific Pathogen not identified Viability of pathogen not indicated |
| Serological antibody test | Easily performed on readily accessible samples | False-negative in immunocompromised host |
3.2. Monoclonal Antibody-Based Diagnostic Approaches for Invasive Aspergillosis
The difficulty in diagnosing IA has spurred many investigators to explore the value of both in vitro and in vivo approaches using mAbs. In recent decades, these methods have gradually been adopted clinically. The Aspergillus cell wall components, such as polysaccharides and glycoproteins, and secreted functional molecules could all be potential targets for assays using platforms based on mAbs to indicate infection with Aspergillus species. All of these techniques take advantage of the highly specific interaction with the target antigen and mAb.
3.2.1. The Detection of Aspergillus Antigens in Blood and Urine Using Monoclonal Antibodies
Soluble molecules released or metabolized by Aspergillus, such as galactomannan (GM) and other galactomannoprotein [54,55,56] in the blood and bronchoalveolar lavage fluid (BALF), are promising biomarkers for Aspergillus infection. These soluble antigens in various specimens can be detected by the mAb in vitro and some of the assays, such as lateral flow device (LFD) analysis, have been designed as a “point-of-care (POC)” diagnostic method [57,58,59]. The detection of these circulating or break down antigens provides evidence of Aspergillus infection in the early infection period and may prompt the initiation of antifungal treatment but does not identify the infecting species.
The most common in vitro diagnostic approach is the mAb-based antigen detection sandwich ELISA that is used to detect the Aspergillus antigens in blood samples. The mAb EB-A2 against GM binds to an epitope of β-(1-5)-connected galactofuranose residues, and is the first antibody to have been widely investigated in an ELISA [54]. The Platelia™ Aspergillus EIA, an mAb EB-A2-based GM detection sandwich microplate assay, is a well-established commercial test that may detect GM at an early stage of infection [60,61], supporting a diagnosis of IA. The sensitivity of this GM assay in serum ranges from 41% to 78%, which is lower than that of BALF, which varies from 60% to 100%. The specificity of this assay in serum is 60% to 95%, which is again lower than the 85% to 98% tested in BALF [62,63,64]. The sensitivity of this GM assay is further reduced by earlier treatment with antifungal agents [50,65].
In an effort to improve the performance of a biomarker assay for Aspergillus antigens, a variety of other assays based on novel mAbs have been investigated. Hao et al. [66] produced 17 candidate antibodies and developed an assay using two of these in sandwich ELISA to detect Aspergillus antigens in a rabbit model of IA. Wang et al. [67] have developed a sandwich ELISA using mAb against recombinant Afmp1p and Afmp4p that detects the antigen in culture filtrate and serum from Aspergillus infected rabbit. Ansari and colleagues recently reported two mAbs that recognised recombinant A. flavus mannoprotein 1 (Aflmp1), that were both highly specific to A. flavus and A. parasiticus cell wall fragments [68]. Our team has produced two mAbs including 1D2 and 4E4 against Aspergillus cell wall glycoproteins, which are capable of testing the secreted antigens in culture media and plasma antigens in A. fumigatus infected IA mice [69]. These studies display promise in detecting various circulating antigens in pre-clinical research, supporting development for clinical application later.
An LFD has been developed that detects antigens in plasma and BALF samples. This is a non-culture mAb-based immunoassay that can be used at the POC to detect Aspergillus antigens of human IA [58,70]. The primary LFD test is a JF-5 based assay, which can detect (galacto)mannoprotein antigens in different samples [71]. In BALF specimens, the sensitivity of LFD testing varies from 58% to 89%, and the specificity ranges between 68% and 100% [58,72,73,74,75] but is less sensitive on plasma. Further studies are needed to determine the clinical utility of this test.
There has been interest in using urine as a diagnostic sample in LFD, as it can be readily obtained and may be useful for monitoring patients at home. Marr and colleagues reported that an mAb476-based LFD test using urine can be beneficial in IA diagnosis in high-risk hosts [76]. MAbs, such as EB-A2 and WF-AF-1, have been well standardised using the LFD technique and are now available commercially [58,77]. This test has been reported to be of value in the diagnosis of COVID-19-associated pulmonary aspergillosis [8]. Given that the LFD urine test is a rapid, non-invasive, economic, convenient, and easy to perform by untrained personnel, it may be used as a “home-testing” technique to monitor the disease progress and treatment efficacy [57,78]. The combination of LFD with other methods such as PCR may increase the diagnostic accuracy significantly [73,79].
3.2.2. The Use of Aspergillus Monoclonal Antibodies for Microscopy and Imaging
Microscopy
MAbs have also been used as probes to detect Aspergillus in formalin-fixed and paraffin-embedded tissue specimens using immunohistochemistry (IHC) or immunofluorescence (IF) to identify the bound complexes [69,80].
An early study indicated that an mAb-based IHC procedure was able to differentiate Aspergillus species from other filamentous fungi and assisted the clinical diagnosis and treatment of IA [81]. In human formalin-fixed and paraffin-embedded lung, liver and skin tissues, mAb EB-A2 was able to identify Aspergillus hyphae and fungal fragments within phagocytic cells [82,83]. Another commercial mAb, WF-AF-1, has been employed to detect Aspergillus antigens in specimens embedded in paraffin blocks from pediatric patients [80]. Tests on specimens offer a rapid identification of Aspergillus elements, particularly in those patients whose microbiological cultures are negative. Other non-commercial mAbs specific to Aspergillus have been used for detecting Aspergillus species in infected animal tissue samples and may have future clinical applications [66,69].
This technique may identify Aspergillus species more rapidly than traditional culture techniques and does not rely on the viability of the organism in samples from patients who have been heavily treated with antifungal agents. The antigens released or metabolised into the parenchymal tissue can also be detected by mAb-probed IHC/IF. This technique can also be used to identify pathogens in stored tissues to aid retrospective studies of fungal infection.
Recently, Amich et al. reported that three-dimensional light sheet fluorescence microscopy (3D-LSFM) could be used to visualize and quantify the location of fungal infection lesions ex vivo, as well as the immune reaction at the cellular level in whole extracted lungs from a mouse model [84]. The fluorescence labelled mAb JF5 (JF5-DyLight 655) was used to locate the A. fumigatus infection lesions. Henneberg et al. confirmed this result using DyLight-650-conjugated JF5 [85]. This novel ex vivo diagnostic tool adds an alternative mAb-based approach for IA diagnosis.
Imaging
MAb-directed in vivo molecular imaging is a novel technique designed to identify specific Aspergillus species causing infective lesions in living animals. Aspergillus cell wall components identified by the tracer conjugated to mAb detected by PET/MR has been reported to be sufficiently sensitive to determine the infection site at a very early stage in IA animal models during life [49,86].
Molecular imaging is defined as an optical method that is able to qualitatively and quantitatively display specific biological profiles at the tissue, cellular or molecular level via signals released by reporters or tracers (such as radionuclides, metal nanoparticles) conjugated with highly specific binding agents (such as mAb). Changes identified at the cellular and molecular level in early stage disease may become apparent before anatomical changes can be seen. To date, two key non-invasive molecular imaging modalities have been reported in animal models [87]. The first one is an optical imaging technique that relies on the photon production by either bioluminescent [88,89] or fluorescent [89,90] reporters of gene-modified pathogens [90,91]. The second is based on the mAb-conjugated radionuclide release of either positrons (e.g., positron emission tomography, PET) [92,93] or γ-rays (e.g., single-photon emission computed tomography, SPECT) [92]. The combination of these functional imaging modalities with conventional imaging (such as CT and MRI) produce high-contrast images of tissue structures capable of showing the specific site of lesions [49,86]. Molecular imaging is showing promise as a non-invasive, precise method for the early diagnosis of IA in vivo, facilitating a personalized therapeutic regimen and treatment follow-up [94] as well as reducing the unnecessary drug application and hospital expenditures.
Bioluminescence Imaging
Bioluminescence imaging (BLI) relies on the detection of photons emitted during the biochemical generation of light by the luciferase enzyme catalyzing the luciferin oxidation [95]. The firefly luciferase gene regulated by the gpdA promoter has been successfully inserted into the genome of A. fumigatus [96] to locate the infection pathogens in BLI. In addition, BLI is capable of screening the infection progress over time in the same animal to define the time course of an infection, reducing the need for sacrificing multiple animals at various time points [96,97]. BLI can only detect the gene-modified Aspergillus strains and has limited depth penetration, but is sufficiently sensitive and specific to monitor the pathogenesis and treatment of IA both in vitro and in vivo in small animals [91,96,97,98,99]. Nevertheless, BLI is not applicable to studies in humans [96,97].
Immune PET/MRI
Positron emission tomography (PET) scan is an imaging test that can help reveal both normal and abnormal metabolic activity or biochemical functions in the tissues and organs by radioactivity. Given that PET has limited accuracy in pinpointing the precise location of the disease, it is usually combined with CT or MRI and referred to as PET/CT or PET/MRI scanning. Radiolabelled mAb-mediated PET combined with MRI, termed immunoPET/MRI [100], is a comparatively new field in cancer diagnosis [101], but has not been fully explored as a tool in clinical IA diagnosis. The mouse mAb JF5 (mJF5) [102], which binds to antigens common to A. fumigatus, A. flavus, A. niger and A. terreus, binds to invasive hyphae rather than the resting conidia [87]. Rolle et al. [86] first reported a [64Cu] DOTA (1,4,7,10-tetraazacyclododecane-1,4,7,10-tetraacetic acid)-labelled mJF5-directed in vivo PET/MRI to determine the location of A. fumigatus in IPA mice, thereby diagnosing IPA specifically and non-invasively. This study indicated that radionuclide labelled-mJF5-mediated in vivo molecular imaging is capable of detecting A. fumigatus hyphae in mice and distinguishing Aspergillus infection from bacterial infection or sterile inflammation in lungs, emphasizing the promising nature of this technique for diagnosing IA.
As a first step toward translating this diagnostic approach for possible clinical application, Davies and colleagues produced a novel humanized mAb JF5 (hJF5) specific for A. fumigatus antigens and conjugated it to [64Cu] DOTAGA (1,4,7,10-tetraazacyclododececane,1-(glutaric acid)-4,7,10-triacetic acid) or [64Cu] NODAGA (1,4,7-triazacyclononane,1-glutaric acid-4,7-acetic acid) [49]. This group found that the uptake of [64Cu] NODAGA-hJF5 in the lungs of A. fumigatus infected animals was significantly improved when compared to that in mice receiving [64Cu] DOTAGA-hJF5 and mJF5 tracers, demonstrating that the conjugation of 64Cu and the chelator NODAGA to hJF5 enhanced the performance of immunoPET/MRI in vivo for lung lesions. Furthermore, this radiolabelled antibody tracer can be used to monitor the treatment responsiveness of new antifungal regimens [49]. In addition to this, hJF5 mAb has been double-conjugated with both [64Cu] DOTAGA and DyLight650 and visualized by PET/MRI and 3D light sheet fluorescence microscopy (LSFM). This study gives evidence of the multiple applications of dual-labelled hJF5 for imaging, as it can be used to localize and quantify the A. fumigatus infection in vivo and ex vivo, as well as monitoring the responsiveness of antifungal azole treatment [85].
At present, all of these mAb-guided molecular imaging modalities have been applied only in pre-clinical IA studies, though they show promise in the diagnosis of IPA. Moreover, a multimodal imaging method is beneficial for in vivo evaluation of antifungal drugs in animal models [103]. Future work needs to be conducted to evaluate this innovative imaging method in IA animal models involving other organ infections, such as those of the brain, kidney and spleen, and to facilitate its translation to the clinical setting.
4. Monoclonal Antibodies and Invasive Aspergillosis Therapy
4.1. Challenges of Invasive Aspergillosis Therapy
Effective anti-Aspergillus treatment closely depends on the initial treatment in the early course of the Aspergillus infection, recovery from neutropenia and, if possible, reversal of immune suppressive therapy. Because of the lack of sensitive and specific tests, many high-risk patients receive an empirical therapy regimen of high-priced antifungal agents before they are accurately diagnosed, or a prolonged treatment after proven diagnosis, posing a heavy economic burden on society and the patients’ families [104]. In addition, anti-fungal prophylaxis or improper drug usage may lead to antibiotic overuse, unnecessary adverse effects on the patient and resistance to Aspergillus species such as A. fumigatus [6].
As present, there are three main drug classes of antifungal agents: triazoles, amphotericin B and echinocandins [105,106,107,108]. All agents require long therapeutic cycles and have varying degrees of toxicity and various adverse effects. These include hepatotoxicity, neurotoxicity, impairment of renal function, nausea, vomiting, hypertriglyceridemia, and complex drug interactions with other treatment regimens. Furthermore, the mortality rate of IA in immunosuppressed individuals still ranges from 30% to 90% in spite of anti-Aspergillus therapy [5]. Surgery is another alternative for those patients who have limited lung lesions or for infections that do not respond to antifungal drugs. This has very limited application in those who are critically immunocompromised due to the high risk of fatal haemorrhage, death or other complications after surgery [21]. Because of these limitations, the development of new, rapid acting, effective and specific anti-mold therapeutic options is needed to manage the increasing population of immunosuppressed patients. MAb-based immunotherapeutic strategies may offer an avenue to develop such novel treatments because of the high specificity of mAb binding to the corresponding antigen.
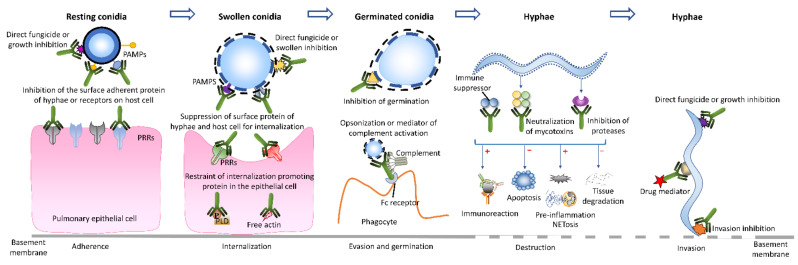
4.2. Anti Aspergillus Activity of Monoclonal Antibodies
Invasive aspergillosis is associated with a complex process of adherence, internalization, and invasion of Aspergillus and the involvement of various proteases and toxins. Thus, mAbs specific to those molecules protect the host and aid removal of Aspergillus pathogens by suppression of adherence [109,110,111], opsonization [112], neutralization of toxins or enzymes [113], complement activation and directing fungicidal activity [110,114,115] (Figure 2). For example, the mAbs binding to sialic acid [27] and galactosaminogalactan [35] on Aspergillus or to epithelia receptors, such as fibronectin [27,35] or E-cadherin [116,117], may interfere with Aspergillus adhesion, endocytosis and agglutination and downregulate the pathogenicity of the fungi. Aspergillus toxin neutralization restricts epithelial internalization and promotes the immune response to the pathogens, thus reducing invasion and dissemination of Aspergillus [33,43]. All of these approaches have promise in protecting the host from fungal attack. Moreover, some mAbs have catalytic ability that can hydrolyse the target antigens and directly destroy the pathogens, independently from the individual’s immune system [118]. Additionally, the mAb can be used as a mediator to direct the anti-fungal drug to the infection site, enhancing the anti-fungal activity.
Figure 2.
Monoclonal antibody-based modes to suppress or eliminate Aspergillus.
4.3. Monoclonal Antibody-Based Immunotherapeutic Modes for Invasive Aspergillosis
The number of mAb-related therapeutic strategies investigated for IA is steadily expanding and includes both in vitro and in vivo studies, although the immune treatment of IA is still in its infancy. The mAb-guided therapeutic regimens have gained widespread interest in IA treatment because mAbs bind to the specific antigens and can target the Aspergillus infection quickly and accurately. In 1993, Frosco et al. generated five mAbs (BB11, MB8, KD5, GD11, and CCIII 19) against elastase that effectively inhibited the enzymatic activity of elastase in vivo, but found that these mAbs did not protect immunocompromised mice from fatal A. fumigatus infection. This suggested elastase may not be the principal virulence factor included in IPA mice [119]. Since then, further mAbs directed against a large variety of cell wall antigens of A fumigatus have been reported, and antifungal activity tested both in vitro and in vivo. All of the mAbs related to the treatment of Aspergillus infection are listed in Table 2, including the therapeutic effects, antibody subclass and references.
Table 2.
Monoclonal antibody-mediated therapeutic effects in Aspergillus infection.
| Therapeutic Effects | MAb | Subclass | References |
|---|---|---|---|
| Fungal growth inhibition/fungicidal activity (in vitro) | C7, K10, A9, Mab-7, SMB19, R-5, MS112-IIB1, YW327.6S2, 3G11 and 5H5 | IgM, IgG, IgG1, IgG3 | [110,112,113,115,120,121,122,123,124] |
| Fungal growth inhibition/fungicidal activity (in vivo) | K10, A9, 2G8, R-5, 3G11 and 5H5 | IgM, IgG1, IgG2b, IgG3 | [112,115,118,123,125,126] |
| Germination suppression (in vitro) | K10, A9, 2G8, R-5, 3G11 and 5H5 | IgM, IgG1, IgG2b, IgG3 | [112,115,118,123,125,126] |
| Attachment inhibition (in vitro) | 2G8, Mab-7, AK-14 | IgG2b, IgM | [109,110,111,125] |
| Protease inhibition (in vivo) | BB11, MB8, KD5, GD11, and CCIII 19 | IgG1 and IgG2a | [119] |
| Immunological enhancement (in vitro and in vivo) | A9, SMB19, MS112-IIB1, 3G11, 5H5, YW327.6S2 | IgG1, IgM, IgG1, IgG3, IgG | [112,113,122,123,124] |
| Drug mediator (in vitro and in vivo) | MPS5.44 | IgM | [127] |
As shown in Table 2, various mAbs can act as an anti-fungal agents and protect the hosts directly in different ways based on the binding between the antibody and the antigen. In addition, those mAbs specific to receptors such as Axl that have inhibitory effects on specific parts of the immune response may improve the outcome of IA in a mouse model [124]. MAbs can also be used as a carrier to direct antifungal drugs to the diseased region, resulting in precise treatment with fewer side effects. For instance, alliinase conjugated mAb produces cytotoxic allicin molecules in the presence of alliin and effectively killed the fungi in vitro [127]. This study opens a new door to treat serious Aspergillus infection using antibody-directed enzyme prodrug technology (ADEPT) [128], which can guide the enzyme to activate a prodrug at a specific infection site, thus diminishing the adverse effect to other parts of the body.
Additionally, some mAbs that do not have fungicidal properties could have antifungal effects by conjugating with a radiation emitter. Known as radioimmunotherapy [126], this has been widely utilized in anti-cancer treatment and shows very promising results [129]. Although it has yet to be explored with IA, radioimmunotherapy showed fungicidal activity against Cryptococcus neoformans in vitro by significantly decreasing the tissue burdens of cryptococcosis in a mouse model, as well as extending the survival time with minimal toxicity [130].
Taken together, the mAb-mediated immune therapy strategies are currently associated with the direct interference of pathogen attachment, inhibition of conidia germination, restraint of hyphal growth, fungal growth inhibition or fungicidal activity, fungal protease inhibition to prevent the tissue digression, immune activity enhancement of the host and drug mediation (Figure 2). Thereby, this new immune treatment avenue hinders the fungal growth and exerts a protective effect to the animal in vivo. In addition, mAbs can take part in the drug transportation, leading to specific and precise mAb-mediated treatments with less side effects. These pre-clinical studies demonstrate an extremely promising future in immune treatment of IA. However, most studies focus on the final therapeutic effects in the in vitro or in vivo experiments, but rarely explore the detailed fungicidal mechanisms of mAbs in IA treatment. Further studies are required to illustrate these specific mechanisms.
5. Perspectives and Conclusions
Mab-mediated immuno-diagnostic and -therapeutic approaches have potential to improve the outcome of IA. However, further studies are needed to realise this promise in a clinical setting where there is high IA morbidity and morbidity. Novel immune-molecular imaging modalities offer the promise of a rapid test that can identify Aspergillus species in vivo, offsetting the need for invasive and potentially harmful tests, such as biopsies or BALF, in severely neutropenic or thrombocytopenic patients. Linking mAbs to differing contrast agents may allow their use with several imaging platforms such as PET/MRI. Secondly, given that IA patients have high mortality, other novel strategies for preventing Aspergillus infection are needed. Passive immunisation with mAbs against Aspergillus species appears to improve survival in mouse models of IA, but there are no reports of humanising mAbs or the potential for use as prophylaxis in humans or as treatment to augment the activity of antifungal pharmaceutical agents.
The clinical diagnosis and management of IA remains challenging, because of the non-specific symptoms coupled with the lack of precise and non-invasive diagnostic methods. The delayed diagnosis leads to delayed antifungal treatment, aggravating the disease progression. The mAb-mediated diagnostic methods with high sensitivity and specificity, including molecular imaging, offer the promise of accurate diagnostic modalities that limit this vicious cycle of progressive infection by early detection of the fungal wall antigens or secreted molecules. In addition, the pathogen-specific mAb-directed antifungal regimens show therapeutic promise in IA by inhibiting important steps in the pathogenesis of IA, enhancing the host response and directing fungicidal activity. In conclusion, the mAb-based diagnostic and therapeutic strategies have been widely applied in modern medicine, and further innovation can be expected to improve the diagnosis and treatment of IA. However, as there are many challenges in designing, powering and conducting clinical trials with relevant endpoints, progress has been slow. All-cause mortality at day 42 is useful for acute pulmonary IA but does not work well for slowly progressive infection. The EORTC-MSG defined an overall response endpoint that requires improvement in all three sub-elements (clinical, radiological and mycological) so that if lesions are stable, the response is defined as failure [131]. Despite these difficulties, there is recognition of an unmet need [132]. At present, most of these antibody-guided diagnostic and therapeutic investigations are at the pre-clinical stage, and multi-centre collaboration offers the opportunity to translate these promising agents into clinical practice [133].
Abbreviations
| IA | invasive aspergillosis |
| mAbs | monoclonal antibodies |
| mAb | monoclonal antibody |
| HSCT | allogeneic hematopoietic stem cell transplant |
| SOT | solid organ transplant |
| PAMPs | pathogen-associated molecular patterns |
| PRRs | pattern recognition receptors |
| Cal A | calcineurin A |
| GAG | galactosaminogalactan |
| NETs | neutrophil extracellular traps |
| ROS | reactive oxygen species |
| PLD | phospholipase D |
| EORTC/MSGERC | European Organization for Research and Treatment of Cancer and the Mycoses Study Group Education and Research Consortium |
| PCR | polymerase chain reaction |
| GM | galactomannan |
| BALF | bronchoalveolar lavage fluid |
| LFD | lateral flow device |
| IHC | immunohistochemistry |
| IF | immunofluorescence |
| PET | positron emission tomography |
| SPECT | single-photon emission computed tomography |
| BLI | bioluminescence imaging |
| LSFM | light sheet fluorescence microscopy |
| ADEPT | antibody-directed enzyme prodrug technology |
| FDA | Food and Drug Administration. |
Author Contributions
Conceptualization, X.L., A.S.-T., J.G.L., M.B. and S.T.C.; supervision, A.S.-T., J.G.L., M.B. and S.T.C.; writing—original draft preparation, X.L. and A.S.-T.; writing—review and editing, X.L., A.S.-T., J.G.L., M.B., S.A.M., Y.Z. and S.T.C.; project administration, A.S.-T., J.G.L., M.B. and S.T.C.; funding acquisition, X.L., A.S.-T., J.G.L., M.B. and S.T.C. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
Funding Statement
This research was funded by support from the University of Otago Vice-Chancellor’s Strategic Development Fund, Maurice and Phyllis Paykel Trust grant, the Sandy Smith Scholarship/Grants-in-Aid and University of Otago Doctoral Scholarship.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Imbert S., Cassaing S., Bonnal C., Normand A.C., Gabriel F., Costa D., Blaize M., Lachaud L., Hasseine L., Kristensen L., et al. Invasive aspergillosis due to Aspergillus cryptic species: A prospective multicentre study. Mycoses. 2021;64:1346–1353. doi: 10.1111/myc.13348. [DOI] [PubMed] [Google Scholar]
- 2.Alastruey-Izquierdo A., Alcazar-Fuoli L., Cuenca-Estrella M. Antifungal susceptibility profile of cryptic species of Aspergillus. Mycopathologia. 2014;178:427–433. doi: 10.1007/s11046-014-9775-z. [DOI] [PubMed] [Google Scholar]
- 3.Azoulay E., Russell L., Van De Louw A., Metaxa V., Bauer P., Povoa P., Montero J.G., Loeches I.M., Mehta S., Puxty K., et al. Diagnosis of severe respiratory infections in immunocompromised patients. Intensive Care Med. 2020;46:298–314. doi: 10.1007/s00134-019-05906-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jenks J.D., Gangneux J.P., Schwartz I.S., Alastruey-Izquierdo A., Lagrou K., Thompson Iii G.R., Lass-Florl C., Hoenigl M., European Confederation of Medical Mycology Council Investigators Diagnosis of breakthrough fungal infections in the clinical mycology laboratory: An ECMM consensus statement. J. Fungi. 2020;6:216. doi: 10.3390/jof6040216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Brown G.D., Denning D.W., Gow N.A., Levitz S.M., Netea M.G., White T.C. Hidden killers: Human fungal infections. Sci. Transl. Med. 2012;4:165rv13. doi: 10.1126/scitranslmed.3004404. [DOI] [PubMed] [Google Scholar]
- 6.Rybak J.M., Fortwendel J.R., Rogers P.D. Emerging threat of triazole-resistant Aspergillus fumigatus. J. Antimicrob. Chemother. 2019;74:835–842. doi: 10.1093/jac/dky517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Segrelles-Calvo G., Araujo G.R.S., Llopis-Pastor E., Carrillo J., Hernandez-Hernandez M., Rey L., Rodriguez Melean N., Escribano I., Anton E., Zamarro C., et al. Prevalence of opportunistic invasive aspergillosis in COVID-19 patients with severe pneumonia. Mycoses. 2021;64:144–151. doi: 10.1111/myc.13219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Autier B., Prattes J., White P.L., Valerio M., Machado M., Price J., Egger M., Gangneux J.P., Hoenigl M. Aspergillus lateral flow assay with digital reader for the diagnosis of COVID-19-associated pulmonary aspergillosis (CAPA): A multicenter study. J. Clin. Microbiol. 2022;60:e0168921. doi: 10.1128/JCM.01689-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Marr K.A., Platt A., Tornheim J.A., Zhang S.X., Datta K., Cardozo C., Garcia-Vidal C. Aspergillosis complicating severe coronavirus disease. Emerg. Infect. Dis. 2021;27:18–25. doi: 10.3201/eid2701.202896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sharma A., Mishra T., Kumar N., Soubani A.O. Influenza-associated aspergillosis: Nationwide trends, predictors and outcomes from 2005 to 2014. Chest. 2020;158:1857–1866. doi: 10.1016/j.chest.2020.06.010. [DOI] [PubMed] [Google Scholar]
- 11.Chen W., Li M., Younis M.H., Barnhart T.E., Jiang D., Sun T., Lang J.M., Engle J.W., Zhou M., Cai W. ImmunoPET of trophoblast cell-surface antigen 2 (Trop-2) expression in pancreatic cancer. Eur. J. Nucl. Med. Mol. Imaging. 2022;49:861–870. doi: 10.1007/s00259-021-05563-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bagati A., Kumar S., Jiang P., Pyrdol J., Zou A.E., Godicelj A., Mathewson N.D., Cartwright A.N.R., Cejas P., Brown M., et al. Integrin alphavbeta6-TGFbeta-SOX4 pathway drives immune evasion in triple-negative breast cancer. Cancer Cell. 2021;39:54–67. doi: 10.1016/j.ccell.2020.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Carnasciali A., Amoriello R., Bonechi E., Mazzoni A., Ravagli C., Doumett S., Cappiello L., D’Elios M.M., Baldi G., Ballerini C. T cell delivery of nanoparticles-bound anti-CD20 monoclonal antibody: Successful B cell depletion in the spinal cord during experimental autoimmune encephalomyelitis. J. Neuroimmune Pharmacol. 2021;16:376–389. doi: 10.1007/s11481-020-09931-w. [DOI] [PubMed] [Google Scholar]
- 14.Menzies-Gow A., Corren J., Bourdin A., Chupp G., Israel E., Wechsler M.E., Brightling C.E., Griffiths J.M., Hellqvist A., Bowen K., et al. Tezepelumab in adults and adolescents with severe, uncontrolled asthma. N. Engl. J. Med. 2021;384:1800–1809. doi: 10.1056/NEJMoa2034975. [DOI] [PubMed] [Google Scholar]
- 15.Sirivichayakul C., Limkittikul K., Chanthavanich P., Yoksan S., Ratchatatat A., Lim J.K., Arunsodsai W., Sabchareon A. Monoclonal antibody-based capture ELISA in the diagnosis of previous dengue infection. Virol. J. 2019;16:125. doi: 10.1186/s12985-019-1222-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Weber-Lima M.M., Prado-Costa B., Becker-Finco A., Costa A.O., Billilad P., Furst C., De Moura J.F., Alvarenga L.M. Acanthamoeba spp. monoclonal antibody against a CPA2 transporter: A promising molecular tool for acanthamoebiasis diagnosis and encystment study. Parasitology. 2020;147:1678–1688. doi: 10.1017/S0031182020001778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wang C., Li W., Drabek D., Okba N.M.A., Van Haperen R., Osterhaus A., Van Kuppeveld F.J.M., Haagmans B.L., Grosveld F., Bosch B.J. A human monoclonal antibody blocking SARS-CoV-2 infection. Nat. Commun. 2020;11:2251. doi: 10.1038/s41467-020-16256-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kreye J., Reincke S.M., Kornau H.C., Sanchez-Sendin E., Corman V.M., Liu H., Yuan M., Wu N.C., Zhu X., Lee C.D., et al. A therapeutic non-self-reactive SARS-CoV-2 antibody protects from lung pathology in a COVID-19 hamster model. Cell. 2020;183:1058–1069. doi: 10.1016/j.cell.2020.09.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Park S.J., Mehrad B. Innate immunity to Aspergillus species. Clin. Microbiol. Rev. 2009;22:535–551. doi: 10.1128/CMR.00014-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kuek L.E., Lee R.J. First contact: The role of respiratory cilia in host-pathogen interactions in the airways. Am. J. Physiol. Lung Cell Mol. Physiol. 2020;319:L603–L619. doi: 10.1152/ajplung.00283.2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Latgé J.-P., Chamilos G. Aspergillus fumigatus and Aspergillosis in 2019. Clin. Microbiol. Rev. 2019;33:e00140-18. doi: 10.1128/CMR.00140-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Strickland A.B., Shi M. Mechanisms of fungal dissemination. Cell Mol. Life Sci. 2021;78:3219–3238. doi: 10.1007/s00018-020-03736-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Van De Veerdonk F.L., Gresnigt M.S., Romani L., Netea M.G., Latge J.P. Aspergillus fumigatus morphology and dynamic host interactions. Nat. Rev. Microbiol. 2017;15:661–674. doi: 10.1038/nrmicro.2017.90. [DOI] [PubMed] [Google Scholar]
- 24.Aimanianda V., Bayry J., Bozza S., Kniemeyer O., Perruccio K., Elluru S.R., Clavaud C., Paris S., Brakhage A.A., Kaveri S.V., et al. Surface hydrophobin prevents immune recognition of airborne fungal spores. Nature. 2009;460:1117–1121. doi: 10.1038/nature08264. [DOI] [PubMed] [Google Scholar]
- 25.Chai L.Y., Netea M.G., Sugui J., Vonk A.G., Van De Sande W.W., Warris A., Kwon-Chung K.J., Kullberg B.J. Aspergillus fumigatus conidial melanin modulates host cytokine response. Immunobiology. 2010;215:915–920. doi: 10.1016/j.imbio.2009.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Valsecchi I., Dupres V., Stephen-Victor E., Guijarro J.I., Gibbons J., Beau R., Bayry J., Coppee J.Y., Lafont F., Latge J.P., et al. Role of hydrophobins in Aspergillus fumigatus. J. Fungi. 2017;4:2. doi: 10.3390/jof4010002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Warwas M.L., Watson J.N., Bennet A.J., Moore M.M. Structure and role of sialic acids on the surface of Aspergillus fumigatus conidiospores. Glycobiology. 2007;17:401–410. doi: 10.1093/glycob/cwl085. [DOI] [PubMed] [Google Scholar]
- 28.Sheppard D.C. Molecular mechanism of Aspergillus fumigatus adherence to host constituents. Curr. Opin. Microbiol. 2011;14:375–379. doi: 10.1016/j.mib.2011.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Houser J., Komarek J., Kostlanova N., Cioci G., Varrot A., Kerr S.C., Lahmann M., Balloy V., Fahy J.V., Chignard M., et al. A soluble fucose-specific lectin from Aspergillus fumigatus conidia--structure, specificity and possible role in fungal pathogenicity. PLoS ONE. 2013;8:e83077. doi: 10.1371/journal.pone.0083077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rodriguez-De La Noval C., Ruiz Mendoza S., De Souza Goncalves D., Da Silva Ferreira M., Honorato L., Peralta J.M., Nimrichter L., Guimaraes A.J. Protective efficacy of lectin-Fc (IgG) fusion proteins in vitro and in a pulmonary aspergillosis in vivo model. J. Fungi. 2020;6:250. doi: 10.3390/jof6040250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Liu H., Lee M.J., Solis N.V., Phan Q.T., Swidergall M., Ralph B., Ibrahim A.S., Sheppard D.C., Filler S.G. Aspergillus fumigatus CalA binds to integrin alpha5beta1 and mediates host cell invasion. Nat. Microbiol. 2016;2:16211. doi: 10.1038/nmicrobiol.2016.211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Arunachalam D., Namperumalsamy V.P., Prajna L., Kuppamuthu D. Human corneal epithelial cells internalize Aspergillus flavus spores by actin-mediated endocytosis. Infect. Immun. 2021;89:e00794-20. doi: 10.1128/IAI.00794-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Zhang C.J., Chen F.Y., Liu X.Y., Han X.L., Hui Y.S., Su X.T., Chen Y., Sun Y.S., Han L. Gliotoxin induces cofilin phosphorylation to promote actin cytoskeleton dynamics and internalization of Aspergillus fumigatus into type II human pneumocyte cells. Front. Microbiol. 2019;10:1345. doi: 10.3389/fmicb.2019.01345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Jia X.D., Chen F.Y., Pan W.H., Yu R.T., Tian S.G., Han G.G., Fang H.Q., Wang S., Zhao J.Y., Li X.P., et al. Gliotoxin promotes Aspergillus fumigatus internalization into type II human pneumocyte A549 cells by inducing host phospholipase D activation. Microb. Infect. 2014;16:491–501. doi: 10.1016/j.micinf.2014.03.001. [DOI] [PubMed] [Google Scholar]
- 35.Gravelat F.N., Beauvais A., Liu H., Lee M.J., Snarr B.D., Chen D., Xu W., Kravtsov I., Hoareau C.M., Vanier G., et al. Aspergillus galactosaminogalactan mediates adherence to host constituents and conceals hyphal beta-glucan from the immune system. PLoS Pathog. 2013;9:e1003575. doi: 10.1371/journal.ppat.1003575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lee M.J., Geller A.M., Bamford N.C., Liu H., Gravelat F.N., Snarr B.D., Le Mauff F., Chabot J., Ralph B., Ostapska H., et al. Deacetylation of fungal exopolysaccharide mediates adhesion and biofilm formation. Mbio. 2016;7:e00252-16. doi: 10.1128/mBio.00252-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lee M.J., Liu H., Barker B.M., Snarr B.D., Gravelat F.N., Al Abdallah Q., Gavino C., Baistrocchi S.R., Ostapska H., Xiao T.L., et al. The fungal exopolysaccharide galactosaminogalactan mediates virulence by enhancing resistance to neutrophil extracellular traps. PLoS Pathog. 2015;11:e1005187. doi: 10.1371/journal.ppat.1005187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Gresnigt M.S., Bozza S., Becker K.L., Joosten L.A.B., Abdollahi-Roodsaz S., Van Der Berg W.B., Dinarello C.A., Netea M.G., Fontaine T., De Luca A., et al. A polysaccharide virulence factor from Aspergillus fumigatus elicits anti-inflammatory effects through induction of interleukin-1 receptor antagonist. PLoS Pathog. 2014;10:e1003936. doi: 10.1371/journal.ppat.1003936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Meletiadis J., Meis J.F., Mouton J.W., Verweij P.E. Analysis of growth characteristics of filamentous fungi in different nutrient media. J. Clin. Microbiol. 2001;39:478–484. doi: 10.1128/JCM.39.2.478-484.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Silva R.L.H., Rosa-Milani E., Brunaldi M.O., Maffei C.M.L. Murine model of invasive pulmonary Aspergillosis: Follow-up of tissue injury, fungal burden and mortality with distinct elastase production strains. J. Mycol. Med. 2019;29:112–119. doi: 10.1016/j.mycmed.2018.10.003. [DOI] [PubMed] [Google Scholar]
- 41.Rowley J., Namvar S., Gago S., Labram B., Bowyer P., Richardson M.D., Herrick S.E. Differential proinflammatory responses to Aspergillus fumigatus by airway epithelial cells in vitro are protease dependent. J. Fungi. 2021;7:468. doi: 10.3390/jof7060468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Gayathri L., Akbarsha M.A., Ruckmani K. In vitro study on aspects of molecular mechanisms underlying invasive aspergillosis caused by gliotoxin and fumagillin, alone and in combination. Sci. Rep. 2020;10:14473. doi: 10.1038/s41598-020-71367-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Arias M., Santiago L., Vidal-Garcia M., Redrado S., Lanuza P., Comas L., Domingo M.P., Rezusta A., Galvez E.M. Preparations for invasion: Modulation of host lung immunity during pulmonary aspergillosis by gliotoxin and other fungal secondary metabolites. Front. Immunol. 2018;9:2549. doi: 10.3389/fimmu.2018.02549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Stanzani M., Orciuolo E., Lewis R., Kontoyiannis D.P., Martins S.L., St John L.S., Komanduri K.V. Aspergillus fumigatus suppresses the human cellular immune response via gliotoxin-mediated apoptosis of monocytes. Blood. 2005;105:2258–2265. doi: 10.1182/blood-2004-09-3421. [DOI] [PubMed] [Google Scholar]
- 45.Waring P., Eichner R.D., Mullbacher A., Sjaarda A. Gliotoxin induces apoptosis in macrophages unrelated to its antiphagocytic properties. J. Biol. Chem. 1988;263:18493–18499. doi: 10.1016/S0021-9258(19)81385-6. [DOI] [PubMed] [Google Scholar]
- 46.Stevanovic J., Stanimirovic Z., Radakovic M., Stojic V. In vitro evaluation of the clastogenicity of fumagillin. Environ. Mol. Mutagen. 2008;49:594–601. doi: 10.1002/em.20409. [DOI] [PubMed] [Google Scholar]
- 47.Fallon J.P., Reeves E.P., Kavanagh K. The Aspergillus fumigatus toxin fumagillin suppresses the immune response of Galleria mellonella larvae by inhibiting the action of haemocytes. Microbiology. 2011;157:1481–1488. doi: 10.1099/mic.0.043786-0. [DOI] [PubMed] [Google Scholar]
- 48.Guruceaga X., Ezpeleta G., Mayayo E., Sueiro-Olivares M., Abad-Diaz-De-Cerio A., Aguirre Urizar J.M., Liu H.G., Wiemann P., Bok J.W., Filler S.G., et al. A possible role for fumagillin in cellular damage during host infection by Aspergillus fumigatus. Virulence. 2018;9:1548–1561. doi: 10.1080/21505594.2018.1526528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Davies G., Rolle A.M., Maurer A., Spycher P.R., Schillinger C., Solouk-Saran D., Hasenberg M., Weski J., Fonslet J., Dubois A., et al. Towards translational immunoPET/MR imaging of invasive pulmonary Aspergillosis: The humanised monoclonal antibody JF5 detects Aspergillus lung infections in vivo. Theranostics. 2017;7:3398–3414. doi: 10.7150/thno.20919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Donnelly J.P., Chen S.C., Kauffman C.A., Steinbach W.J., Baddley J.W., Verweij P.E., Clancy C.J., Wingard J.R., Lockhart S.R., Groll A.H., et al. Revision and update of the consensus definitions of invasive fungal disease from the European organization for research and treatment of cancer and the mycoses study group education and research consortium. Clin. Infect. Dis. 2020;71:1367–1376. doi: 10.1093/cid/ciz1008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Ullmann A.J., Aguado J.M., Arikan-Akdagli S., Denning D.W., Groll A.H., Lagrou K., Lass-Florl C., Lewis R.E., Munoz P., Verweij P.E., et al. Diagnosis and management of Aspergillus diseases: Executive summary of the 2017 ESCMID-ECMM-ERS guideline. Clin. Microbiol. Infect. 2018;24((Suppl. 1)):e1–e38. doi: 10.1016/j.cmi.2018.01.002. [DOI] [PubMed] [Google Scholar]
- 52.Thornton C.R. Breaking the mould—Novel diagnostic and therapeutic strategies for invasive pulmonary aspergillosis in the immune deficient patient. Expert Rev. Clin. Immunol. 2014;10:771–780. doi: 10.1586/1744666X.2014.904747. [DOI] [PubMed] [Google Scholar]
- 53.Steinbach W.J., Marr K.A., Anaissie E.J., Azie N., Quan S.P., Meier-Kriesche H.U., Apewokin S., Horn D.L. Clinical epidemiology of 960 patients with invasive aspergillosis from the PATH Alliance registry. J. Infect. 2012;65:453–464. doi: 10.1016/j.jinf.2012.08.003. [DOI] [PubMed] [Google Scholar]
- 54.Sarwar M., Gardezi S.A.H., Zaman G., Ikram A., Satti L., Khadim M.T. Evaluation of galactomannan and beta-d-glucan assays for the diagnosis of invasive aspergillosis in clinically suspected cases. J. Pak. Med. Assoc. 2020;70:442–446. doi: 10.5455/JPMA.1476. [DOI] [PubMed] [Google Scholar]
- 55.Dichtl K., Seybold U., Ormanns S., Horns H., Wagener J. Evaluation of a novel Aspergillus antigen enzyme-linked immunosorbent assay. J. Clin. Microbiol. 2019;57:e00136-19. doi: 10.1128/JCM.00136-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Egger M., Penziner S., Dichtl K., Gornicec M., Kriegl L., Krause R., Khong E., Mehta S., Vargas M., Gianella S., et al. Performance of the euroimmun Aspergillus antigen ELISA for the diagnosis of invasive pulmonary Aspergillosis in bronchoalveolar lavage fluid. J. Clin. Microbiol. 2022;60:e00215-22. doi: 10.1128/jcm.00215-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Davies G., Singh O., Prattes J., Hoenigl M., Sheppard P.W., Thornton C.R. asp f I: Old enemies but new opportunities for urine-based detection of invasive pulmonary Aspergillosis using lateral-flow technology. J. Fungi. 2020;7:19. doi: 10.3390/jof7010019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Jenks J.D., Mehta S.R., Taplitz R., Aslam S., Reed S.L., Hoenigl M. Point-of-care diagnosis of invasive aspergillosis in non-neutropenic patients: Aspergillus galactomannan lateral flow assay versus Aspergillus-specific lateral flow device test in bronchoalveolar lavage. Mycoses. 2019;62:230–236. doi: 10.1111/myc.12881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Jenks J.D., Hoenigl M. Point-of-care diagnostics for invasive aspergillosis: Nearing the finish line. Expert Rev. Mol. Diagn. 2020;20:1009–1017. doi: 10.1080/14737159.2020.1820864. [DOI] [PubMed] [Google Scholar]
- 60.Fisher B.T., Westling T., Boge C.L.K., Zaoutis T.E., Dvorak C.C., Nieder M., Zerr D.M., Wingard J.R., Villaluna D., Esbenshade A.J., et al. Prospective evaluation of galactomannan and (1-->3) beta-d-glucan assays as diagnostic tools for invasive fungal disease in children, adolescents, and young adults with acute myeloid leukemia receiving fungal prophylaxis. J. Pediatric Infect. Dis Soc. 2021;10:864–871. doi: 10.1093/jpids/piab036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Calero A.L., Alonso R., Gadea I., Vega M.D.M., Garcia M.M., Munoz P., Machado M., Bouza E., Garcia-Rodriguez J. Comparison of the performance of two galactomannan detection tests: Platelia Aspergillus Ag and Aspergillus galactomannan ag virclia monotest. Microbiol. Spectr. 2022;10:e02626-21. doi: 10.1128/spectrum.02626-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Herrera S., Husain S. Current state of the diagnosis of invasive pulmonary Aspergillosis in lung transplantation. Front. Microbiol. 2018;9:3273. doi: 10.3389/fmicb.2018.03273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Zhou W., Li H., Zhang Y., Huang M., He Q., Li P., Zhang F., Shi Y., Su X. Diagnostic value of galactomannan antigen test in serum and bronchoalveolar lavage fluid samples from patients with nonneutropenic invasive pulmonary Aspergillosis. J. Clin. Microbiol. 2017;55:2153–2161. doi: 10.1128/JCM.00345-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Lamoth F. Galactomannan and 1,3-beta-d-glucan testing for the diagnosis of invasive Aspergillosis. J. Fungi. 2016;2:22. doi: 10.3390/jof2030022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Leeflang M.M., Debets-Ossenkopp Y.J., Wang J., Visser C.E., Scholten R.J., Hooft L., Bijlmer H.A., Reitsma J.B., Zhang M., Bossuyt P.M., et al. Galactomannan detection for invasive aspergillosis in immunocompromised patients. Cochrane Database Syst. Rev. 2015;2015:CD007394. doi: 10.1002/14651858.CD007394.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Hao W., Pan Y.X., Ding Y.Q., Xiao S., Yin K., Wang Y.D., Qiu L.W., Zhang Q.L., Woo P.C., Lau S.K., et al. Well-characterized monoclonal antibodies against cell wall antigen of Aspergillus species improve immunoassay specificity and sensitivity. Clin. Vaccine Immunol. 2008;15:194–202. doi: 10.1128/CVI.00362-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Wang Z.Y., Cai J.P., Qiu L.W., Hao W., Pan Y.X., Tung E.T., Lau C.C., Woo P.C., Lau S.K., Yuen K.Y., et al. Development of monoclonal antibody-based galactomannoprotein antigen-capture ELISAs to detect Aspergillus fumigatus infection in the invasive aspergillosis rabbit models. Eur. J. Clin. Microbiol. Infect. Dis. 2012;31:2943–2950. doi: 10.1007/s10096-012-1645-3. [DOI] [PubMed] [Google Scholar]
- 68.Ansari S., Mousavi A., Safarnejad M.R., Farrokhi N., Alavi S.M., Schillberg S., Nolke G. Selection and characterization of two monoclonal antibodies specific for the Aspergillus flavus major antigenic cell wall protein Aflmp1. Fungal Biol. 2021;125:621–629. doi: 10.1016/j.funbio.2021.03.004. [DOI] [PubMed] [Google Scholar]
- 69.Lian X., Chambers S., Lewis J.G., Scott-Thomas A., Bhatia M. Two Monoclonal antibodies that specifically recognize Aspergillus cell wall antigens and can detect circulating antigens in infected mice. Int. J. Mol. Sci. 2022;23:252. doi: 10.3390/ijms23010252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Prattes J., Flick H., Pruller F., Koidl C., Raggam R.B., Palfner M., Eigl S., Buzina W., Zollner-Schwetz I., Thornton C.R., et al. Novel tests for diagnosis of invasive aspergillosis in patients with underlying respiratory diseases. Am. J. Respir. Crit. Care Med. 2014;190:922–929. doi: 10.1164/rccm.201407-1275OC. [DOI] [PubMed] [Google Scholar]
- 71.Thornton C., Johnson G., Agrawal S. Detection of invasive pulmonary aspergillosis in haematological malignancy patients by using lateral-flow technology. J. Vis. Exp. 2012;61:e3721. doi: 10.3791/3721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Jenks J.D., Mehta S.R., Taplitz R., Law N., Reed S.L., Hoenigl M. Bronchoalveolar lavage Aspergillus Galactomannan lateral flow assay versus Aspergillus-specific lateral flow device test for diagnosis of invasive pulmonary Aspergillosis in patients with hematological malignancies. J. Infect. 2019;78:249–259. doi: 10.1016/j.jinf.2018.10.014. [DOI] [PubMed] [Google Scholar]
- 73.Heldta S., Prattes J., Eigl S., Spiess B., Flick H., Rabensteiner J., Johnson G., Pruller F., Wolfler A., Niedrist T., et al. Diagnosis of invasive aspergillosis in hematological malignancy patients: Performance of cytokines, Asp LFD, and Aspergillus PCR in same day blood and bronchoalveolar lavage samples. J. Infect. 2018;77:235–241. doi: 10.1016/j.jinf.2018.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Mercier T., Schauwvlieghe A., De Kort E., Dunbar A., Reynders M., Guldentops E., Rijnders B., Verweij P.E., Lagrou K., Maertens J. Diagnosing invasive pulmonary aspergillosis in hematology patients: A retrospective multicenter evaluation of a novel lateral flow device. J. Clin. Microbiol. 2019;57:e01913-18. doi: 10.1128/JCM.01913-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Linder K.A., Kauffman C.A., Zhou S., Miceli M.H. Clinical application of Aspergillus lateral flow device in bronchoalveolar lavage fluid of patients with classic risk factors for invasive pulmonary aspergillosis. Mycoses. 2019;62:1189–1193. doi: 10.1111/myc.13012. [DOI] [PubMed] [Google Scholar]
- 76.Marr K.A., Datta K., Mehta S., Ostrander D.B., Rock M., Francis J., Feldmesser M. Urine antigen detection as an aid to diagnose invasive Aspergillosis. Clin. Infect. Dis. Off. Publ. Infect. Dis. Soc. Am. 2018;67:1705–1711. doi: 10.1093/cid/ciy326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Hoenigl M., Eigl S., Heldt S., Duettmann W., Thornton C., Prattes J. Clinical evaluation of the newly formatted lateral-flow device for invasive pulmonary aspergillosis. Mycoses. 2018;61:40–43. doi: 10.1111/myc.12704. [DOI] [PubMed] [Google Scholar]
- 78.Held J., Schmidt T., Thornton C.R., Kotter E., Bertz H. Comparison of a novel Aspergillus lateral-flow device and the Platelia (R) galactomannan assay for the diagnosis of invasive aspergillosis following haematopoietic stem cell transplantation. Infection. 2013;41:1163–1169. doi: 10.1007/s15010-013-0472-5. [DOI] [PubMed] [Google Scholar]
- 79.White P.L., Parr C., Thornton C., Barnes R.A. Evaluation of real-time PCR, galactomannan enzyme-linked immunosorbent assay (ELISA), and a novel lateral-flow device for diagnosis of invasive aspergillosis. J. Clin. Microbiol. 2013;51:1510–1516. doi: 10.1128/JCM.03189-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Choi J.K., Mauger J., McGowan K.L. Immunohistochemical detection of Aspergillus species in pediatric tissue samples. Am. J. Clin. Pathol. 2004;121:18–25. doi: 10.1309/DK1CG9MATKYYBFMQ. [DOI] [PubMed] [Google Scholar]
- 81.Phillips P., Weiner M.H. Invasive aspergillosis diagnosed by immunohistochemistry with monoclonal and polyclonal reagents. Hum. Pathol. 1987;18:1015–1024. doi: 10.1016/S0046-8177(87)80218-6. [DOI] [PubMed] [Google Scholar]
- 82.Pierard G.E., Arrese Estrada J., Pierard-Franchimont C., Thiry A., Stynen D. Immunohistochemical expression of galactomannan in the cytoplasm of phagocytic cells during invasive aspergillosis. Am. J. Clin. Pathol. 1991;96:373–376. doi: 10.1093/ajcp/96.3.373. [DOI] [PubMed] [Google Scholar]
- 83.Verweij P.E., Smedts F., Poot T., Bult P., Hoogkamp-Korstanje J.A., Meis J.F. Immunoperoxidase staining for identification of Aspergillus species in routinely processed tissue sections. J. Clin. Pathol. 1996;49:798–801. doi: 10.1136/jcp.49.10.798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Amich J., Mokhtari Z., Strobel M., Vialetto E., Sheta D., Yu Y., Hartweg J., Kalleda N., Jarick K.J., Brede C., et al. Three-dimensional light sheet fluorescence microscopy of lungs to dissect local host immune-Aspergillus fumigatus interactions. mBio. 2020;11:e02752-19. doi: 10.1128/mBio.02752-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Henneberg S., Hasenberg A., Maurer A., Neumann F., Bornemann L., Gonzalez-Menendez I., Kraus A., Hasenberg M., Thornton C.R., Pichler B.J., et al. Antibody-guided in vivo imaging of Aspergillus fumigatus lung infections during antifungal azole treatment. Nat. Commun. 2021;12:1707. doi: 10.1038/s41467-021-21965-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Rolle A.M., Hasenberg M., Thornton C.R., Solouk-Saran D., Mann L., Weski J., Maurer A., Fischer E., Spycher P.R., Schibli R., et al. ImmunoPET/MR imaging allows specific detection of Aspergillus fumigatus lung infection in vivo. Proc. Natl. Acad. Sci. USA. 2016;113:E1026–E1033. doi: 10.1073/pnas.1518836113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Gunzer M., Thornton C.R., Beziere N. Advances in the in vivo molecular imaging of invasive Aspergillosis. J. Fungi. 2020;6:338. doi: 10.3390/jof6040338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Gammon S.T., Foje N., Brewer E.M., Owers E., Downs C.A., Budde M.D., Leevy W.M., Helms M.N. Preclinical anatomical, molecular, and functional imaging of the lung with multiple modalities. Am. J. Physiol. Lung Cell Mol. Physiol. 2014;306:L897–L914. doi: 10.1152/ajplung.00007.2014. [DOI] [PubMed] [Google Scholar]
- 89.Andreu N., Zelmer A., Wiles S. Noninvasive biophotonic imaging for studies of infectious disease. FEMS Microbiol. Rev. 2011;35:360–394. doi: 10.1111/j.1574-6976.2010.00252.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Calvo-Álvarez E., Stamatakis K., Punzón C., Álvarez-Velilla R., Tejería A., Escudero-Martínez J.M., Pérez-Pertejo Y., Fresno M., Balaña-Fouce R., Reguera R.M. Infrared fluorescent imaging as a potent tool for in vitro, ex vivo and in vivo models of visceral leishmaniasis. PLoS Negl. Trop. Dis. 2015;9:e0003666. doi: 10.1371/journal.pntd.0003666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Zeng Q., Zhang Z., Chen P., Long N., Lu L., Sang H. In vitro and in vivo efficacy of a synergistic combination of itraconazole and verapamil against Aspergillus fumigatus. Front. Microbiol. 2019;10:1266. doi: 10.3389/fmicb.2019.01266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Boros E., Packard A.B. Radioactive transition metals for imaging and therapy. Chem. Rev. 2019;119:870–901. doi: 10.1021/acs.chemrev.8b00281. [DOI] [PubMed] [Google Scholar]
- 93.Brandt M., Cardinale J., Aulsebrook M.L., Gasser G., Mindt T.L. An overview of PET radiochemistry, part 2: Radiometals. J. Nucl. Med. 2018;59:1500–1506. doi: 10.2967/jnumed.117.190801. [DOI] [PubMed] [Google Scholar]
- 94.Anderson C.J., Lewis J.S. Current status and future challenges for molecular imaging. Philos. Trans. A Math. Phys. Eng. Sci. 2017;375:20170023. doi: 10.1098/rsta.2017.0023. [DOI] [PubMed] [Google Scholar]
- 95.Badr C.E., Tannous B.A. Bioluminescence imaging: Progress and applications. Trends Biotechnol. 2011;29:624–633. doi: 10.1016/j.tibtech.2011.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Brock M., Jouvion G., Droin-Bergere S., Dussurget O., Nicola M.A., Ibrahim-Granet O. Bioluminescent Aspergillus fumigatus, a new tool for drug efficiency testing and in vivo monitoring of invasive aspergillosis. Appl. Environ. Microbiol. 2008;74:7023–7035. doi: 10.1128/AEM.01288-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Velde G.V., Wiehr S. Fungal imaging. In: Jain S.K., editor. Imaging Infections. Springer International Publishing; Baltimore, MD, USA: 2017. pp. 173–183. [Google Scholar]
- 98.Ibrahim-Granet O., Jouvion G., Hohl T.M., Droin-Bergere S., Philippart F., Kim O.Y., Adib-Conquy M., Schwendener R., Cavaillon J.M., Brock M. In vivo bioluminescence imaging and histopathopathologic analysis reveal distinct roles for resident and recruited immune effector cells in defense against invasive aspergillosis. BMC Microbiol. 2010;10:105. doi: 10.1186/1471-2180-10-105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Galiger C., Brock M., Jouvion G., Savers A., Parlato M., Ibrahim-Granet O. Assessment of efficacy of antifungals against Aspergillus fumigatus: Value of real-time bioluminescence imaging. Antimicrob. Agents Chemother. 2013;57:3046–3059. doi: 10.1128/AAC.01660-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Wei W., Rosenkrans Z.T., Liu J., Huang G., Luo Q.Y., Cai W. ImmunoPET: Concept, design, and applications. Chem. Rev. 2020;120:3787–3851. doi: 10.1021/acs.chemrev.9b00738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Lechermann L.M., Lau D., Attili B., Aloj L., Gallagher F.A. In vivo cell tracking using PET: Opportunities and challenges for clinical translation in oncology. Cancers. 2021;13:4042. doi: 10.3390/cancers13164042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Thornton C.R. Development of an immunochromatographic lateral-flow device for rapid serodiagnosis of invasive aspergillosis. Clin. Vaccine Immunol. 2008;15:1095–1105. doi: 10.1128/CVI.00068-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Poelman J., Himmelreich U., Vanherp L., Zhai L.C., Hillen A., Holvoet B., Belderbos S., Brock M., Maertens J., Vande Velde G., et al. A multimodal imaging approach enables in vivo assessment of antifungal treatment in a mouse model of invasive pulmonary Aspergillosis. Antimicrob. Agents Chemother. 2018;62:e00240-18. doi: 10.1128/AAC.00240-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Leroux S., Ullmann A.J. Management and diagnostic guidelines for fungal diseases in infectious diseases and clinical microbiology: Critical appraisal. Clin. Microbiol. Infect. 2013;19:1115–1121. doi: 10.1111/1469-0691.12426. [DOI] [PubMed] [Google Scholar]
- 105.Shi N., Zheng Q., Zhang H. Molecular dynamics investigations of binding mechanism for triazoles inhibitors to CYP51. Front. Mol. Biosci. 2020;7:586540. doi: 10.3389/fmolb.2020.586540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Zhang M., Lu J., Duan X., Chen J., Jin X., Lin Z., Pang Y., Wang X., Lou H., Chang W. Rimonabant potentiates the antifungal activity of amphotericin B by increasing cellular oxidative stress and cell membrane permeability. FEMS Yeast Res. 2021;21:foab016. doi: 10.1093/femsyr/foab016. [DOI] [PubMed] [Google Scholar]
- 107.Aruanno M., Glampedakis E., Lamoth F. Echinocandins for the Treatment of Invasive Aspergillosis: From Laboratory to Bedside. Antimicrob. Agents Chemother. 2019;63:e00399-19. doi: 10.1128/AAC.00399-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Lamaris G.A., Lewis R.E., Chamilos G., May G.S., Safdar A., Walsh T.J., Raad I.I., Kontoyiannis D.P. Caspofungin-mediated beta-glucan unmasking and enhancement of human polymorphonuclear neutrophil activity against Aspergillus and non-Aspergillus hyphae. J. Infect. Dis. 2008;198:186–192. doi: 10.1086/589305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Torosantucci A., Chiani P., Bromuro C., De Bernardis F., Palma A.S., Liu Y., Mignogna G., Maras B., Colone M., Stringaro A., et al. Protection by anti-beta-glucan antibodies is associated with restricted beta-1,3 glucan binding specificity and inhibition of fungal growth and adherence. PLoS ONE. 2009;4:e5392. doi: 10.1371/journal.pone.0005392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Chaturvedi A.K., Kumar R., Kumar A., Shukla P.K. A monoclonal IgM directed against immunodominant catalase B of cell wall of Aspergillus fumigatus exerts anti-A. fumigatus activities. Mycoses. 2009;52:524–533. doi: 10.1111/j.1439-0507.2008.01635.x. [DOI] [PubMed] [Google Scholar]
- 111.Kumar A., Shukla P.K. A monoclonal antibody against glycoproteins of Aspergillus fumigatus shows anti-adhesive potential. Microb. Pathog. 2015;79:24–30. doi: 10.1016/j.micpath.2015.01.003. [DOI] [PubMed] [Google Scholar]
- 112.Matveev A.L., Krylov V.B., Khlusevich Y.A., Baykov I.K., Yashunsky D.V., Emelyanova L.A., Tsvetkov Y.E., Karelin A.A., Bardashova A.V., Wong S.S.W., et al. Novel mouse monoclonal antibodies specifically recognizing β-1,3-D-glucann antigen. PLoS ONE. 2019;14:e0215535. doi: 10.1371/journal.pone.0215535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Chauvin D., Hust M., Schutte M., Chesnay A., Parent C., Moreira G., Arroyo J., Sanz A.B., Pugniere M., Martineau P., et al. Targeting Aspergillus fumigatus crf transglycosylases with neutralizing antibody is relevant but not sufficient to erase fungal burden in a neutropenic rat model. Front. Microbiol. 2019;10:600. doi: 10.3389/fmicb.2019.00600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Ulrich S., Ebel F. Monoclonal antibodies as tools to combat fungal infections. J. Fungi. 2020;6:22. doi: 10.3390/jof6010022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Yadav R.K., Shukla P.K. A novel monoclonal antibody against enolase antigen of Aspergillus fumigatus protects experimental aspergillosis in mice. FEMS Microbiol. Lett. 2019;366:fnz015. doi: 10.1093/femsle/fnz015. [DOI] [PubMed] [Google Scholar]
- 116.Xu X.Y., Chen F., Sun H., Chen C., Zhao B.L. Important factors mediates the adhesion of Aspergillus fumigatus to alveolar epithelial cells with E-cadherin. Am. J. Transl. Res. 2016;8:2419–2425. [PMC free article] [PubMed] [Google Scholar]
- 117.Xu X.Y., Shi Y., Zhang P.P., Zhang F., Shen Y.Y., Su X., Zhao B.L. E-cadherin mediates adhesion and endocytosis of Aspergillus fumigatus blastospores in human epithelial cells. Chin. Med. J. 2012;125:617–621. [PubMed] [Google Scholar]
- 118.Bowen A., Wear M.P., Cordero R.J., Oscarson S., Casadevall A. A monoclonal antibody to cryptococcus neoformans glucuronoxylomannan manifests hydrolytic activity for both peptides and polysaccharides. J. Biol. Chem. 2017;292:417–434. doi: 10.1074/jbc.M116.767582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Frosco M.B., Chase T., Jr., Macmillan J.D. The effect of elastase-specific monoclonal and polyclonal antibodies on the virulence of Aspergillus fumigatus in immunocompromised mice. Mycopathologia. 1994;125:65–76. doi: 10.1007/BF01371095. [DOI] [PubMed] [Google Scholar]
- 120.Cenci E., Mencacci A., Spreca A., Montagnoli C., Bacci A., Perruccio K., Velardi A., Magliani W., Conti S., Polonelli L., et al. Protection of killer antiidiotypic antibodies against early invasive aspergillosis in a murine model of allogeneic T-cell-depleted bone marrow transplantation. Infect. Immun. 2002;70:2375–2382. doi: 10.1128/IAI.70.5.2375-2382.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Moragues M.D., Omaetxebarria M.J., Elguezabal N., Sevilla M.J., Conti S., Polonelli L., Ponton J. A monoclonal antibody directed against a Candida albicans cell wall mannoprotein exerts three anti-C. albicans activities. Infect. Immun. 2003;71:5273–5279. doi: 10.1128/IAI.71.9.5273-5279.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Chaturvedi A.K., Kavishwar A., Shiva Keshava G.B., Shukla P.K. Monoclonal immunoglobulin G1 directed against Aspergillus fumigatus cell wall glycoprotein protects against experimental murine aspergillosis. Clin. Diagn. Lab. Immunol. 2005;12:1063–1068. doi: 10.1128/CDLI.12.9.1063-1068.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Wharton R.E., Stefanov E.K., King R.G., Kearney J.F. Antibodies generated against Streptococci protect in a mouse model of disseminated aspergillosis. J. Immunol. 2015;194:4387–4396. doi: 10.4049/jimmunol.1401940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Shibata T., Habiel D.M., Coelho A.L., Hogaboam C.M. Axl receptor blockade protects from invasive pulmonary aspergillosis in mice. J. Immunol. 2014;193:3559–3565. doi: 10.4049/jimmunol.1401258. [DOI] [PubMed] [Google Scholar]
- 125.Torosantucci A., Bromuro C., Chiani P., De Bernardis F., Berti F., Galli C., Norelli F., Bellucci C., Polonelli L., Costantino P., et al. A novel glyco-conjugate vaccine against fungal pathogens. J. Exp. Med. 2005;202:597–606. doi: 10.1084/jem.20050749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Nosanchuk J.D., Dadachova E. Radioimmunotherapy of fungal diseases: The therapeutic potential of cytocidal radiation delivered by antibody targeting fungal cell surface antigens. Front. Microbiol. 2011;2:283. doi: 10.3389/fmicb.2011.00283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Appel E., Vallon-Eberhard A., Rabinkov A., Brenner O., Shin I., Sasson K., Shadkchan Y., Osherov N., Jung S., Mirelman D. Therapy of murine pulmonary aspergillosis with antibody-alliinase conjugates and alliin. Antimicrob. Agents Chemother. 2010;54:898–906. doi: 10.1128/AAC.01267-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Bagshawe K.D., Sharma S.K., Springer C.J., Rogers G.T. Antibody directed enzyme prodrug therapy (ADEPT). A review of some theoretical, experimental and clinical aspects. Ann. Oncol. Off. J. Eur. Soc. Med. Oncol. 1994;5:879–891. doi: 10.1093/oxfordjournals.annonc.a058725. [DOI] [PubMed] [Google Scholar]
- 129.Karam S.D., Raben D. Radioimmunotherapy for the treatment of head and neck cancer. Lancet Oncol. 2019;20:E404–E416. doi: 10.1016/S1470-2045(19)30306-7. [DOI] [PubMed] [Google Scholar]
- 130.Dadachova E., Nakouzi A., Bryan R.A., Casadevall A. Ionizing radiation delivered by specific antibody is therapeutic against a fungal infection. Proc. Natl. Acad. Sci. USA. 2003;100:10942–10947. doi: 10.1073/pnas.1731272100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Segal B.H., Herbrecht R., Stevens D.A., Ostrosky-Zeichner L., Sobel J., Viscoli C., Walsh T.J., Maertens J., Patterson T.F., Perfect J.R., et al. Defining responses to therapy and study outcomes in clinical trials of invasive fungal diseases: Mycoses Study Group and European Organization for Research and Treatment of Cancer consensus criteria. Clin. Infect. Dis. 2008;47:674–683. doi: 10.1086/590566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Food and Drug Administration Development Considerations of Antifungal Drugs to Address Unmet Medical Need. [(accessed on 11 May 2022)]; Available online: https://www.fda.gov/media/141400/download.
- 133.Rex J.H. Antifungal Drugs to Address Unmet Medical Need. [(accessed on 11 May 2022)]; Available online: https://www.fda.gov/media/141074/download.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.