Abstract
Rationale
A large body of work demonstrates the impact of housing instability on health by exploring the effects of evictions and homelessness on psychological wellbeing of young adults and children. However, limited research leverages national longitudinal data to examine whether and how experiences of a range of housing insecurity events, rather than just eviction or homelessness, affect physical health among midlife and older adults.
Objective
The current study examines (1) prevalence of housing insecurity among midlife and older adults by age and race, (2) linkages between housing insecurity experiences and facets of physical health, and (3) age and race moderations on these effects.
Method
This study employs regression models to examine whether experiences of housing insecurity affect self-rated physical health and chronic physical conditions among midlife and older adults (N = 2598) leveraging two waves of the National Study of Midlife in the United States (MIDUS).
Results
Models revealed that housing insecurity experiences predicted poorer self-rated physical health and additional chronic conditions, even when controlling for previous physical health. Moderation analyses indicated that housing insecurity has a stronger relationship with chronic conditions among midlife adults as compared to older adults, and among Black adults as compared to white adults. These results suggest that experiences of housing insecurity leave adults vulnerable to compromised physical health, and that housing insecurity experiences may be particularly detrimental to the health of midlife Black adults.
Conclusions
This research adds to the extant literature by introducing a comprehensive measure of housing insecurity experiences, and contributes to a life course perspective regarding how housing insecurity can affect physical health. This research has implications for policy that addresses housing insecurity as a public health concern, especially in the aftermath of the 2008 recession and the economic and housing crisis caused by the COVID-19 pandemic.
Keywords: United States, Housing insecurity, Physical health problems, Self-rated health, Chronic conditions, Midlife and aging, Racial disparities, Longitudinal
Highlights
-
•
Housing insecurity should be measured as a comprehensive range of experiences.
-
•
Housing insecurity experiences are more prevalent among Blacks and midlife adults.
-
•
Housing insecurity is associated with poorer physical health.
-
•
This work has implications for targeting housing policy to improve public health.
1. Introduction
In the United States (U.S.), housing insecurity is an issue many experience on a daily basis. Such experiences, including increased rates of homelessness, eviction, and housing insecurity, tend to surge in the aftermath of economic, public health, and political events, bringing housing insecurity considerations to the forefront of national attention. The Great Recession of 2008 was one such event that contributed to increases in housing issues. In the aftermath of the recession, it was estimated that 900,000 to 1.1 million families with children in the U.S. could be categorized as being in deep poverty, and therefore at risk of experiencing housing uncertainty and homelessness (Sard, 2009). As a result of rising unemployment and general economic instability, homeless shelters saw increases of up to 40 percent in certain parts of the country immediately after the 2008 recession (Sard, 2009).
In addition to economic challenges of the recession, increasing housing and rent prices have compounded the issues of housing insecurity in the U.S. The housing sector in the United States is experiencing unprecedented levels of unaffordability, with median rent prices and home values increasing by 61% and 112%, respectively, between 1960 and 2016 (Swope & Hernández, 2019). On the other hand, purchasing power has not changed (DeSilver, 2020). Housing instability is exacerbated by external, structural, and environmental factors, including historical redlining practices, neighborhood gentrification, and climate disasters (McClure et al., 2019). The COVID-19 pandemic has compounded these issues of housing affordability and stability due to economic uncertainty and housing market dynamics; and these impacts exacerbated the vulnerabilities faced by low-income and minoritized populations concerning housing (Jones & Grigsby-Toussaint, 2020; Rogers & Power, 2020). Previous literature indicates the stress associated with increased housing unaffordability can impact various facets of physical and psychological wellbeing (Stahre et al., 2015).
Interest in better defining and researching housing insecurity and its health impacts was spurred by the prevalence of homelessness and other living insecurities after the Great Recession. While extant literature has contributed to establishing the linkage between housing and health, it has focused primarily on single item extreme measures of housing insecurity (particularly eviction and homelessness) in younger children and adolescents (Cutts et al., 2011; Leifheit et al., 2020). In contrast, this study aims to provide an assessment of the associations of a range of housing insecurity experiences on the health of midlife and aging adults, a group whose proportion in the U.S. population is rapidly growing, making the need for understanding the factors that influence their health imperative (Case et al., 2020). By doing so, this study contributes to a life course understanding of how housing insecurity experiences can shape health across age groups.
Additionally, this study will consider disparities in physical health. The use of various markers of physical health can provide a more comprehensive understanding of how housing insecurity is associated with various facets of wellbeing. Finally, a particularly salient feature of this study is the use of national longitudinal data, which will help to better estimate the effects of housing insecurity experiences after the 2008 recession on physical health, while controlling for baseline risk. This study also considers which groups are likely to experience housing insecurity events, and how age and race may moderate the relationship between housing insecurity and physical health; this will provide a greater understanding of the differential toll housing insecurity may play on the health of midlife and aging adults (Belsky & Pluess, 2009).
1.1. Defining housing insecurity
Cox et al. (2019) define housing insecurity as “limited or uncertain availability, access, or inability to acquire stable, safe, adequate, and affordable housing and neighborhoods in socially acceptable ways”. Routhier (2019) similarly advocates for “measuring housing insecurity as an index of multiple variables within four identified dimensions: unaffordability, poor conditions, overcrowding, and forced moves”. In contrast to this broad view of housing insecurity, many earlier studies focus only on specific markers of housing uncertainty (typically recent eviction and current homelessness; Vásquez-Vera et al., 2017; Gromis, 2019; Hoke & Boen, 2021). However, housing insecurity should not merely measure whether an individual currently has access to housing/shelter, but also whether they are vulnerable (i.e., for financial reasons, missed mortgage/rent payment, etc.) to disruptions in their current housing situation. This study offers an assessment that captures the multitude of housing insecurity experiences people might face. In doing so, the study contributes to the literature by creating a multidimensional measure of housing insecurity and studying the association with health outcomes.
1.2. Housing insecurity as a determinant of physical health
For mental and physical health, the effects of housing insecurity can operate through various pathways, including affordability, context (i.e., neighborhood quality), conditions (i.e., the quality of housing itself), and stability, the latter of which is the main housing aspect this paper will address (Rolfe et al., 2020; Swope & Hernández, 2019). In terms of physical health, the focus of this study, Desmond and Kimbro (2015) found that mothers who had previously been evicted reported poorer health for themselves as well as their children than those who had not. Pollack et al. (2010) found that unaffordable housing was associated with increased odds of poor self-rated health and conditions such as hypertension and arthritis. Stahre et al. (2015) found that housing insecure participants were two times more likely to self-report poor physical health than housing secure participants. Novick et al. (2020) found that housing insecurity, defined as not being able to afford a suitable home for oneself and one's family, was associated with increased risk for adverse kidney outcomes, which gives insights into the process of health deterioration that occurs to individuals who experience housing uncertainty at a physiological level. Thus, it is clear that housing insecurity can have immediate and long-lasting negative implications for various facets of physical health.
According to the stress process framework (Pearlin et al., 1981), disruptive life events, such as housing insecurity, can impact health not only in the immediate aftermath, but also over the longer term because chronic and acute stress can lead to wear and tear on the body, elevate allostatic load, contribute to dysregulation of the hypothalamic-pituitary-adrenal (HPA) axis, and lead to long lasting health effects through inflammatory pathways (Logan & Barksdale, 2008; Piazza et al., 2010; Ong et al., 2017). Additionally, housing insecurity can also contribute to poorer health through material pathways. Those who are housing insecure are also likely to experience food insecurity (Njai et al., 2017), and may have fewer resources available for other needs such as healthcare (Ma et al., 2008).
1.3. Age and race differences in housing insecurity and physical health vulnerabilities
The stress and consequent physical health repercussions associated with housing insecurity affects individuals differently depending on age and race. While older adults may be more vulnerable overall to chronic health conditions, midlife may be a time when the impact of housing insecurity on physical health is particularly acute. Midlife often brings with it responsibility on both sides of the generational divide in addition to work/career demands (Igarashi et al., 2013; Lachman et al., 2015). Additionally, older adults past retirement age may be eligible for affordable housing programs and government benefits such as Medicare, which may shield them from housing insecurity and the negative health effects associated with it. Since the 1949 National Housing Act, various programs and policies have been implemented to improve and subsidize housing costs for low-income elderly people (Pynoos, 2018).
Racially and ethnically minoritized populations are particularly affected by housing insecurity. Earlier research has found that non-Hispanic Black participants and Hispanics were at lower odds of reporting housing security compared to non-Hispanic whites (Njai et al., 2017). Furthermore, minoritized groups are more likely to experience housing discrimination. Feagin et al. (2006) found that institutions are more than twice as likely to reject Black applicants than white applicants for a mortgage, and while 76 percent of white families owned a home, only 48 percent of Black families owned one. In addition to housing discrimination, gaps in homeownership also likely exist due to lower income whites still having family support to afford housing because their families directly benefited from historical government programs supporting homeownership in the suburbs (Auspurg et al., 2019; Sharp et al., 2020). Racially minoritized groups are also more vulnerable in terms of the physical health and wellbeing impacts of housing insecurity events such as eviction, even after controlling for socioeconomic status (Hepburn et al., 2020; Williams & Mohammed, 2009). This has been attributed to the compounding effects of everyday discrimination or unfair treatment that can contribute to multisystem biological dysregulation and thus various physiological and emotional health consequences. In this study, we examine racial disparities in housing insecurity and physical health within the context of a more nuanced and comprehensive definition of housing insecurity.
1.4. The current study
The current study uses data from a national sample of midlife-to-older adults who responded to questions about the effect of the economic recession of 2008–09. The study explores the association between housing insecurity and two physical health outcomes: (1) self-rated physical health, and (2) number of chronic physical health conditions; hereafter, the terms “health outcomes” and “self-rated health” will refer specifically to “physical health outcomes”, unless indicated. Based on the theoretical propositions outlined above, our hypotheses are:
-
1.
Housing insecurity experiences, even on our more comprehensive characterization of housing insecurity, will be more prevalent among Black adults as compared to white adults and among midlife adults (<65) as compared to older adults (65+).
-
2.
Experiences of housing insecurity will be associated with higher levels of adverse reported health and chronic health conditions, even when controlling for prior health and individual demographic and socioeconomic characteristics, compared to those who did not experience housing insecurity.
-
3.
Having experienced housing insecurity will be associated with higher levels of adverse self-rated health and chronic conditions for midlife adults as compared to older adults.
-
4.
Having experienced housing insecurity will be associated with higher levels of adverse self-rated health and chronic conditions for Black adults than for whites.
2. Methods
2.1. Participants
This study uses data from Midlife in the United States (MIDUS), a national longitudinal study of health and wellbeing, to assess the effects of housing insecurity on health outcomes and health disparities. The MIDUS study began in 1995, and recruited U.S. adults between ages 25 to 75 (Radler, 2014).1 Specifically, the analysis uses data from the second and third waves of MIDUS, collected in 2004–2006 (MIDUS 2) and 2013–2015 (MIDUS 3), respectively (n = 2598; 15.24% Black). The sample includes health measures from the original MIDUS sample, as well as the Milwaukee African American (AA) oversample. MIDUS 2 Milwaukee was collected between 2005 and 2006; MIDUS 3 Milwaukee was collected between 2016 and 2017. The original MIDUS sample and the Milwaukee datasets were combined for the analysis.1
Several criteria were specified for selection into the final sample. Only participants with complete and valid data on sociodemographic characteristics, housing insecurity experiences, and health outcomes were included. In addition, the sample only included participants who identified their race as white or Black. The effects of these exclusions on our analytical sample size are indicated in Supplemental Tables 2 and 3 The final sample comprised 2598 individuals.
Housing insecurity will be used as the main predictor/independent variable for health outcomes in this study. As already indicated, two health outcomes are considered: self-rated physical health and number of chronic physical conditions (i.e., cardiovascular disease, cancer, and diabetes). Age and race will be investigated as potential moderators in the housing insecurity-health relationship. These measures are described in further detail below.
2.2. Measures
Descriptive statistics are presented in Table 1, Table 2. Housing insecurity, age, race, gender, educational level, income, and marital status were predictor variables; self-rated health and number of chronic health conditions were outcomes of interest.
Table 1.
Descriptive statistics for Housing Insecurity Experiences for the overall sample and by age and race.
| Housing Insecurity Experiences | Overall |
Age |
Race |
||||
|---|---|---|---|---|---|---|---|
| (%) | <65 (%) | 65+ (%) | UOR1 (95% C.I.) | White (%) | Black (%) | UOR2 (95% C.I.) | |
| Moved in with friends or family to save money | 5.62 | 7.2 | 3.6 | 0.48 (0.33–0.69) | 3.9 | 15.2 | 4.39 (3.09–6.22) |
| Missed a rent or mortgage payment | 8.20 | 11.8 | 3.7 | 0.29 (0.20–0.40) | 5.4 | 23.7 | 5.45 (4.05–7.32) |
| Were threatened with eviction or foreclosure | 6.31 | 9.3 | 2.6 | 0.26 (0.17–0.38) | 4.0 | 19.2 | 5.71 (4.10–7.92) |
| Lost home to foreclosure, or other | 4.93 | 6.7 | 2.8 | 0.40 (0.26–0.59) | 3.8 | 11.1 | 3.15 (2.14–4.59) |
| Experienced homelessness | 0.96 | 1.5 | 0.3 | 0.23 (0.07–0.62) | 0.6 | 2.8 | 4.47 (1.97–9.89) |
| Any Housing Insecurity | 14.28 | 18.7 | 8.8 | 0.42 (0.33–0.53) | 10.2 | 36.9 | 5.13 (4.01–6.56) |
UOR = Unadjusted Odds Ratios.
Reference group: < 65 years.
Reference group: Whites.
Table 2.
Descriptive statistics for health Status, chronic Conditions, demographic, and socioeconomic characteristics for the analytical sample (N = 2598). MIDUS Wave 2 and 3.
| Variable | Overall Sample (n = 2598) |
Housing Insecurity (n = 371) |
No Housing Insecurity (n = 2227) |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| % | mean | sd | range | % | mean | sd | range | % | mean | sd | range | |
| Health variables | ||||||||||||
| Self-rated physical health | ||||||||||||
| (W2) | ||||||||||||
| Poor/fair | 12.01 | 21.83 | 10.37 | |||||||||
| Good+ | 87.99 | 78.17 | 89.63 | |||||||||
| Self-rated physical health | ||||||||||||
| (W3) | ||||||||||||
| Poor/fair | 18.24 | 35.31 | 15.40 | |||||||||
| Good+ | 81.76 | 64.69 | 84.60 | |||||||||
| Chronic conditions (W2) | 1.93 | 1.69 | 0–14 | 2.20 | 1.82 | 0–11 | 1.89 | 1.66 | 0–14 | |||
| Chronic conditions (W3) | 2.45 | 1.90 | 0–15 | 2.91 | 2.14 | 0–15 | 2.37 | 1.85 | 0–10 | |||
| Sociodemographic variables | ||||||||||||
| Age (W3) | 63.51 | 11.08 | 39–94 | 59.08 | 9.90 | 42–90 | 64.25 | 11.10 | 39–94 | |||
| <65 | 55.35 | 72.51 | 52.49 | |||||||||
| 65+ | 44.65 | 27.49 | 47.51 | |||||||||
| Race (W3) | ||||||||||||
| White | 84.76 | 60.65 | 88.77 | |||||||||
| Black | 15.24 | 39.35 | 11.23 | |||||||||
| Gender (W3) | ||||||||||||
| Male | 42.96 | 38.27 | 43.74 | |||||||||
| Female | 57.04 | 61.73 | 56.26 | |||||||||
| Highest educational level (W3) | ||||||||||||
| High school or less | 30.48 | 38.81 | 29.10 | |||||||||
| Some college or more | 69.52 | 61.19 | 70.90 | |||||||||
| Household income (W3) | 82022 | 72157 | 0–3x105 | 50639 | 48848 | 0–3x105 | 87250 | 74069 | 0–3x105 | |||
| Marital status (W3) | ||||||||||||
| Married | 61.74 | 64.15 | 66.05 | |||||||||
| Not married | 38.26 | 35.85 | 33.95 | |||||||||
2.2.1. Housing insecurity
During MIDUS 3, respondents were asked whether or not they had experienced the following in the aftermath of the 2008 recession: (1) moved in with family/friends to save money; (2) missed a mortgage or rent payment; (3) threatened with foreclosure/eviction; (4) lost home to foreclosure; (5) lost home to something other than foreclosure; and (6) experienced homelessness since last interview. For the analysis, the study developed a comprehensive measure of housing insecurity by adding up the number of “yes” responses to the aforementioned questions. For this scale, “lost home to foreclosure” and “lost home to something other than foreclosure” were collapsed into the single category “lost home”. In the resulting housing insecurity index (HII), zero represents experiencing no housing insecurity, and five represents experiencing all dimensions of housing insecurity. A description of the components of the HII and item-associations with race and age are included in Table 1.
2.2.2. Self-rated health
In MIDUS 3, participants rated their physical health as 1 (excellent), 2 (very good), 3 (good), 4 (fair), or 5 (poor). This measure was dichotomized, such that participants who reported poor/fair health were denoted a score of “1”, while participants who reported good, very good, and excellent health were denoted as “0” (Manor et al., 2000). This measure is the first outcome of interest, and the analysis accounts for self-rated health in MIDUS 2.
While self-rated health measures can be influenced by individuals tending to rate themselves based on the context of the community around them or cultural expectations of health (Burgard & Chen, 2014), studies have found that self-rated health is a reasonably accurate predictor of actual health. Bunda and Busseri (2019) found that actual declines in physical health over time was predicted by subjective perceptions of declining self-rated health.
2.2.3. Number of chronic conditions
We also explore the association between housing insecurity and chronic conditions. Examples of chronic conditions include “asthma, bronchitis or emphysema, diabetes or high blood sugar, ulcer, migraine headaches, and thyroid disease” (Piazza et al., 2013). Participants are given a list of chronic conditions to indicate whether each condition was experienced in the past 12 months (either a yes or no response). In addition, participants also indicate whether they have ever experienced cancer or heart disease, and these chronic conditions were also added to the summative score. Our analysis included 15 overarching chronic physical condition categories following the operationalization used by Piazza et al. (2013), and is similar to measurement of chronic conditions used by Weston et al. (2020), and Woo et al. (2020). Number of chronic conditions from MIDUS 2 was included as a covariate in our models (mean = 1.93, sd = 1.69, range = 0–14). Number of chronic conditions collected in MIDUS 3 was our second outcome (mean = 2.45, sd = 1.90, range = 0–15).
2.2.4. Sociodemographic characteristics
Responses from MIDUS 3 were used to measure all sociodemographic variables. Age, race, gender, education, income, and marital status were collected through self-report, and included as predictors in the study.
2.2.4.1. Age
This study used age reported in MIDUS 3, and dichotomized the variable into two groups: adults less than 65 (reference group), and 65 and older. The average retirement age for U.S. adults born between 1943 and 1954 is 66 years of age, and for adults born before 1943, the age is 65 (much of the MIDUS sample is likely born within these years; Munnell, 2011). When adults reach retirement, they become eligible for a variety of governmental programs and Social Security benefits (Martin & Weaver, 2005). Additionally, Medicare health insurance becomes available at age 65 (Card et al., 2009). Thus, the sample was split into age groups according to adults 65 and older being eligible for several health and governmental benefits as opposed to midlife adults.
2.2.4.2. Race
Participants indicated their racial background in MIDUS 3 as White, Black/African American, Native American or Alaska Native Aleutian Islander/Eskimo, Asian, Native Hawaiian or Pacific Islander, or other. Participants were categorized by white (reference group) and Black for the regression analysis. Participants who did not indicate their racial origins as white or Black were excluded from the sample (n = 279). Many MIDUS papers have only examined Black and white participants when looking at racial differences in health, given the relatively limited sample size of other racial groups in the dataset (see Assari et al., 2019; Lankarani & Assari, 2017; Surachman et al., 2021), as we do in the current study.
2.2.4.3. Other covariates
Participants indicated gender in MIDUS 3 telephone as male or female (reference). Education was coded as high school or less (reference), some college or more. The income measure was taken from information on total pretax household income from wages, pensions, social security, and government assistance in MIDUS 3, and the natural logarithm of household income was used as a continuous variable in the analyses following standard approaches (Neman, 2020). Marital status was coded as married and unmarried (reference).
2.3. Analytic strategy
To address between-group differences in housing insecurity by race and age (Hypothesis 1), we produced descriptive statistics for the overall sample and by group (Table 1). Differences in the prevalence of housing insecurity items were assessed using univariate logistic regression models for both age and race (Table 1). Results are presented as univariate odds ratios (OR) and incidence rate ratios (IRR) for both of these analyses, indicating whether: (1) older respondents (65 +) differed from midlife participants (<65, reference group) and (2) Black participants differed from white participants (reference group). Our subsequent analyses focused on housing insecurity as a determinant of health. To study the association between housing insecurity and self-rated physical heath and chronic health conditions, we used logistic regression and Poisson regression, respectively. Housing insecurity was included as a predictor of these two outcomes and the models control for age, race, gender, education, income, marital status, and, at the previous wave, health status (Hypothesis 2). To study the moderating effect of age and race in the association between housing insecurity and the outcomes, an interaction term between each variable and housing insecurity was included in the final regression models (Hypotheses 3 and 4). The analysis used a threshold of alpha = .05 to determine significance.
3. Results
3.1. Housing insecurity index
The most common manifestation of housing insecurity was missing a rent or mortgage payment, with 8.20% of participants indicating that they had experienced this in the aftermath of the 2008 recession. The least common form of housing insecurity was homelessness, with only 0.96% of participants reporting this. A specific breakdown of each housing insecurity construct by age and race can be found in Table 1. There are variations by age and race in the five dimensions of housing insecurity, with those below 65 years of age and Black adults particularly experiencing “missed a rent or mortgage payment” and “threatened with eviction or foreclosure” more so than their peers. A Cronbach's alpha test of the housing insecurity index indicated a reliability score of 0.69 (95% CI = 0.67, 0.71). Section 3.2 provides the results of additional statistical tests.
3.2. Group comparisons
The first set of analyses describes the items and sum of the housing insecurity scale. This study examined whether the prevalence of housing insecurity differed by age and race. Participants within the sample were subset into two age categories: less than 65 years, and 65+ years. Participants aged less than 65 years had a mean of 0.37 housing insecurity experiences (sd = 0.88, range = 0–5), and participants aged 65+ years had a mean of 0.13 housing insecurity experiences (sd = 0.48, range = 0–4). A t-test illustrated that these mean differences were significant between the <65 and 65+ age groups, with <65 significantly more likely to experience higher housing insecurity than the 65+ group (t = 8.64, df = 2303.3, p < 0.001).
In our analyses, we also examined whether housing insecurity differed across racial groups. To do so, all participants within the sample were subset into Black and white. Whites had a mean of 0.18 housing insecurity experiences (sd = 0.60, range = 0–5), whereas Black participants had a mean of 0.72 housing insecurity experiences (sd = 1.15, range = 0–5). A t-test illustrated that these mean differences were significant between the white and Black groups, with Black participants experiencing higher housing insecurity than whites (t = 9.18, df = 434.99, p < 0.001).
3.3. Association of housing insecurity on physical health
The regression results can be found in Table 3, Table 4. Binary logistic regression was used to estimate the relationship between housing insecurity and self-rated physical health. Poisson regression was used to estimate the association between housing insecurity and the number of chronic conditions (a count variable). Model 1 in the tables examines the association between housing insecurity and demographic characteristics in predicting health outcomes. Model 2 adds MIDUS 2 health as an additional predictor in the model, to account for pre-existing risk. Model 3 examines the interaction between age and housing insecurity on health outcomes. Finally, Model 4 examines the interaction of race and housing insecurity on health outcomes.
Table 3.
Logistic regression models of housing insecurity and self-rated physical health, Midlife in the United States (n = 2598).
| Model 1 |
Model 2 |
Model 3 |
Model 4 |
|||||
|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| Housing Insecurity (HI) | 1.45*** | 1.28–1.63 | 1.46*** | 1.28–1.67 | 1.51*** | 1.31–1.75 | 1.52*** | 1.28–1.79 |
| Age * HI | 0.84 | 0.60–1.16 | ||||||
| Race * HI | 0.92 | 0.71–1.19 | ||||||
| Age (Ref=<65) | ||||||||
| 65+ | 0.92 | 0.74–1.15 | 0.94 | 0.75–1.19 | 0.94 | 0.75–1.20 | 0.94 | 0.75–1.20 |
| Race (Ref = White) | ||||||||
| Black | 1.90*** | 1.45–2.48 | 1.39* | 1.03–1.88 | 1.40* | 1.03–1.88 | 1.44* | 1.05–1.96 |
| Sex (Ref = Female) | ||||||||
| Male | 0.93 | 0.75–1.17 | 0.95 | 0.75–1.20 | 0.94 | 0.74–1.19 | 0.95 | 0.75–1.21 |
| Education (Ref = HS or less) | ||||||||
| Some college or more | 0.46*** | 0.37–0.57 | 0.52*** | 0.41–0.66 | 0.52*** | 0.41–0.66 | 0.52*** | 0.41–0.66 |
| Household Income | 0.89*** | 0.86–0.93 | 0.90*** | 0.87–0.94 | 0.90*** | 0.87–0.94 | 0.90*** | 0.87–0.94 |
| Marital Status (Ref = Not married) | ||||||||
| Married | 0.85 | 0.68–1.07 | 0.90 | 0.70–1.15 | 0.89 | 0.70–1.15 | 0.90 | 0.70–1.15 |
| MIDUS 2 Health | ||||||||
| Self-reported physical health | 8.82*** | 6.72–11.62 | 8.85*** | 6.74–11.66 | 8.82*** | 6.72–11.62 | ||
Significance level: †p ≤ 0.10, *p ≤ 0.05, **p ≤ 0.01, ***p ≤ 0.001.
Model 1 R2 = 0.092; Model 2 R2 = 0.192; Model 3 R2 = 0.193; Model 4 R2 = 0.192.
Table 4.
Poisson regression models of housing insecurity and chronic physical health conditions, Midlife in the United States (n = 2598).
| Model 1 |
Model 2 |
Model 3 |
Model 4 |
|||||
|---|---|---|---|---|---|---|---|---|
| IRR | 95% CI | IRR | 95% CI | IRR | 95% CI | IRR | 95% CI | |
| Housing Insecurity (HI) | 1.12*** | 1.08–1.15 | 1.07*** | 1.04–1.10 | 1.10*** | 1.06–1.14 | 1.00 | 0.96–1.05 |
| Age * HI | 0.89** | 0.83–0.96 | ||||||
| Race * HI | 1.15*** | 1.08–1.22 | ||||||
| Age (Ref=<65) | ||||||||
| 65+ | 1.46*** | 1.39–1.54 | 1.24*** | 1.17–1.30 | 1.23*** | 1.17–1.30 | 1.23*** | 1.17–1.30 |
| Race (Ref = White) | ||||||||
| Black | 1.17*** | 1.09–1.25 | 1.12** | 1.04–1.20 | 1.12** | 1.04–1.20 | 1.07† | 0.99–1.15 |
| Sex (Ref = Female) | ||||||||
| Male | 0.82*** | 0.78–0.86 | 0.92** | 0.87–0.97 | 0.91*** | 0.86–0.96 | 0.91*** | 0.86–0.96 |
| Education (Ref = HS or less) | ||||||||
| Some college or more | 0.87*** | 0.82–0.92 | 0.93** | 0.88–0.98 | 0.93** | 0.88–0.98 | 0.93** | 0.88–0.98 |
| Household Income | 0.98*** | 0.97–0.99 | 0.98** | 0.97–0.99 | 0.98** | 0.97–0.99 | 0.98*** | 0.97–0.99 |
| Marital Status (Ref = Not married) | ||||||||
| Married | 1.02 | 0.96–1.07 | 1.03 | 0.97–1.09 | 1.03 | 0.97–1.08 | 1.02 | 0.97–1.08 |
| MIDUS 2 Health | ||||||||
| Chronic conditions last 12 months | 1.21*** | 1.20–1.22 | 1.21*** | 1.20–1.23 | 1.21*** | 1.20–1.23 | ||
Significance level: †p ≤ 0.10, *p ≤ 0.05, **p ≤ 0.01, ***p ≤ 0.001.
Model 1 R2 = 0.113; Model 2 R2 = 0.312; Model 3 R2 = 0.315; Model 4 R2 = 0.317.
For self-rated physical health (Table 3) and number of chronic conditions (Table 4), a higher housing insecurity index was associated with poorer health outcomes. The association between housing insecurity and each outcome remained strong even when controlling for pre-existing health conditions in MIDUS 2 (see Model 2 in Table 3, Table 4).
For self-rated physical health, each one-unit increase in the housing insecurity index was associated with a 46 percent higher chance/risk of experiencing the outcome of poor/fair rated health (Table 3, Model 2). For number of chronic conditions, each one-unit increase in housing insecurity experiences was associated with a 7% increase in chronic conditions (Table 4, Model 2).
3.4. Age and race differences in the association between housing insecurity and physical health
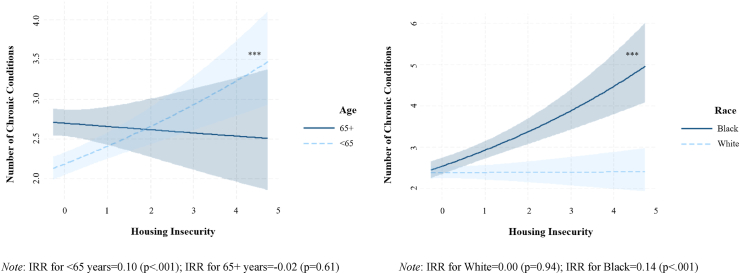
In Models 3 and 4 of the regression analyses, interaction terms between age and race and housing insecurity were added, respectively. For self-reported health, there was no interaction between housing insecurity and age. For chronic physical conditions, the interaction between housing insecurity and age indicates that the relationship between housing insecurity and chronic conditions is stronger for midlife participants than for older participants (Table 4, Model 3; Fig. 1, left panel).
Fig. 1.
The association between housing insecurity and number of chronic physical conditions: Moderation by age and race with confidence intervals.
Note: IRR for <65 years = 0.10 (p < 0.001); IRR for 65+ years = −0.02 (p = 0.61) Note: IRR for White = 0.00 (p = 0.94); IRR for Black = 0.14 (p < 0.001).
For self-rated health, the interaction between race and housing insecurity was non-significant (Table 3, Model 4). However, for chronic conditions, there was a significant interaction between race and housing insecurity (Table 4, Model 4). This indicates that as housing insecurity experiences increase, Black adults will be more susceptible to additional chronic conditions compared to whites (Fig. 1, right panel).
4. Discussion
The results indicate that housing insecurity was associated with higher odds of experiencing each health outcome of interest. This highlights the contribution of housing insecurity on physical health evaluations and chronic conditions in midlife and older adulthood. In terms of age, the regression results indicated that older adults had a significantly higher risk of additional chronic conditions, but no difference in odds of reporting poor health. When age was interacted with housing insecurity, no difference was found in the effect of housing insecurity on the self-rated health outcome by age. However, for chronic conditions, when age was interacted with housing insecurity, the pattern showed that midlife adults exhibited an increased risk of chronic health conditions, a pattern not found for older adults. This indicates that, as individuals face increasing housing insecurity experiences, older age is actually protective against adverse physical health as measured by the number of chronic conditions, whereas midlife adults are more susceptible to the negative health implications of housing insecurity experiences. It is possible older adults (particularly age 65+) may have access to retirement or social security benefits or programs, or more established family networks, that buffer the negative effects of housing insecurity on chronic health conditions. On the other hand, midlife adults may not have access to these services or social supports, which could explain the health deterioration effects observed in our models. It may also be the case that housing insecurity experiences for older adults may be more brief because they have Medicare and Social Security to protect them and get them back on their feet, while for midlife adults the experiences may be more protracted and thus have more time to accumulate in terms of health problems.
As posited, housing insecurity experiences varied significantly by race, similar to the findings of Lee and Evans (2020). Black adults had higher odds of self-reporting poorer physical health and more chronic conditions than white adults. These results are consistent with previous scholarship that has established that Black populations tend to experience worse health overall than whites (Kiang et al., 2019). It is also possible that Black adults are being diagnosed and treated with chronic conditions at lower rates than whites due to less accessible care or more bias in treatment (Kim et al., 2018). Thus, the effects in the analysis may be underestimating the association between chronic health and housing insecurity. When race was interacted with housing insecurity experiences, no difference was found between Black and white participants in the effect of housing insecurity on self-rated health. However, for chronic conditions, Black adults were found to have a significantly higher likelihood of experiencing additional chronic conditions as housing insecurity experiences increased, something not observed among whites. This indicates that the physical health burdens of housing insecurity, at least in terms of the number of chronic health conditions, may disproportionately impact Black communities. It was rather surprising to note that there was a null association between housing insecurity and chronic conditions for white adults. However, we propose potential explanations for this result. White adults may have more access to intergenerational wealth and other resources and supports, which may limit the negative impacts of housing insecurity on health (Avery & Rendall, 2002; Kuebler, 2013; Meschede et al., 2017, pp. 121–137). Additionally, research has found that Black households benefitted less from the post-Great Recession economic recovery compared to white working class households, and that Black households saw a much greater fraction of their wealth eliminated due to the Recession than did white households (Addo & Darity, 2021). Since housing insecurity is worse for the health of Black adults, policies that improved housing security would disproportionately benefit Black adults and could reduce disparities in health.
The results of the study indicate that housing insecurity is an important factor to consider when trying to address and understand the factors that shape individual health outcomes. It also implies that community or governmental action taken to support individuals and families at risk of housing insecurity experiences, such as eviction or foreclosure, may actually result in improved health for beneficiaries of these programs.
4.1. Strengths and limitations
A strength of the MIDUS dataset is the ability to control for various demographic and health behavior factors, including age, race, gender, education, income, and marital status. In addition, the longitudinal nature of the study allowed the assessment of the contributions of housing insecurity on MIDUS 3 health while controlling for corresponding MIDUS 2 health as a covariate/predictor. Despite the methodological strengths of this study, the results need to be interpreted with caution. The use of self-reported health measures may raise issues in terms of the accuracy and reliability of these reports. Minority or low SES populations may have less access to healthcare and thus conditions may not be accurately diagnosed (i.e., underreported). Another major issue with this sample is that it does not provide time-sensitive information on when housing insecurity was experienced, or how many times different housing insecurity items might have been experienced, which limits the ability to capture the full scope of the issue. Finally, there may be selection bias in the sample, such that older adults with housing insecurity may be more likely to have missing data or to have passed away between waves; thus older adults with housing insecurity captured by MIDUS may be disproportionately composed of healthy individuals. However, our analysis of attrition from MIDUS 2 to MIDUS 3 indicates that respondents kept in the analytical sample did not differ in terms of self-rated health, chronic conditions, age, or race (see Supplemental Table 1).
4.2. Future directions
This study opens the door to further research examining the potential effects of a variety of housing insecurity experiences on health (using a variety of measures such as biomarkers; Clair & Hughes, 2019) across the life course. Future work should examine housing insecurity experiences in conjunction with factors like neighborhood quality, and explore whether social support may buffer the negative impacts of housing insecurity on midlife and older adults. Furthermore, it is possible that the effect of housing insecurity on health becomes mediated through other downstream repercussions, such as job loss, pay cut, etc. Therefore, it would be useful in future research to untangle the direct and mediated effects of housing insecurity on health outcomes. Additionally, future studies should further examine disparities in prevalence and impacts of housing insecurity among various racial/ethnic/cultural communities in the U.S. (Chinchilla et al., 2021), not just based on a Black/white binary divide or a simple gender-based binary divide, while also considering disaggregation by other variables such as housing tenure type (that is, differentiating between homeowners and renters).
In the face of the COVID-19 pandemic and associated economic repercussions, it is likely that Americans will continue to face housing insecurity at increasing rates as more people become unemployed, a problem exacerbated by the continuing rise in rent costs (Egede & Walker, 2020; Benfer et al., 2021). Further research into the health impacts and racial/ethnic disparities of COVID-19-related housing insecurity and the formulation of effective interventions and countermeasures to reduce housing insecurity effects on health outcomes, therefore, becomes critical. Research by Fenelon et al. (2017) and Keene et al. (2020) has indicated housing assistance is associated with improved reported health among low-income adults (Lawler, 2001); and eviction moratoriums instated during the COVID-19 pandemic were also associated with better health among U.S. adults (Leifheit et al., 2021). However, our research signals that, in the aftermath of acute economic events such as the current pandemic or economic recessions, these housing supports and benefits (i.e., more affordable housing, preventing insecurity in the first place) should be extended to midlife adults, particularly in Black communities, rather than only the elderly population to protect/preserve population health.
5. Conclusions
Overall, this study supports that experiences of housing insecurity are more prevalent among the midlife adult age group and Black participants, and that housing insecurity is a determinant of physical health issues. However, the associations between housing insecurity and physical health are nuanced with regard to chronic conditions, such that experiencing housing insecurity was more detrimental for Black and midlife adults than for white and older participants. This provides support for increasing accessibility and affordability of housing in minoritized communities and for midlife adults. This research has far-reaching policy implications for policy makers, activists, and the population at large, and can be leveraged by stakeholders to address housing insecurity as a public health issue. Future work should examine how experiences of housing insecurity can be buffered by social supports, housing programs, and local, state, and national policies in order to mitigate the adverse health implications of housing insecurity.
Ethical statement
MIDUS data collection is reviewed and approved by the Education and Social/Behavioral Sciences and the Health Sciences IRBs at the University of Wisconsin-Madison.
Author contributions
Aarti C. Bhat, Conceptualization, Formal analysis, Methodology, Visualization, Writing - original draft; David M. Almeida, Conceptualization, Funding acquisition, Project administration, Supervision; Andrew Fenelon, Conceptualization, Investigation, Validation; Alexis R. Santos-Lozada, Investigation, Project administration, Funding acquisition, Data curation, Validation, Supervision.
Declaration of competing interest
The authors have no conflicts of interest to declare.
Acknowledgement
The MIDUS project has been funded by the John D. and Catherine T. MacArthur Foundation Research Network, as well as National Institute on Aging (NIA) grants P01AG020166, R24AG054159, and U19AG051426. This work was supported by the Penn State Population Research Institute, which is supported by an infrastructure grant by the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD, P2CHD041025) and the Penn State Social Science Research Institute (SSRI). This project was also funded by the NICHD Social Environments and Population Health Training Program (T32HD007514).
Footnotes
For a detailed timeline of the study and recruitment please refer to http://www.midus.wisc.edu/data/timeline.php.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ssmph.2022.101128.
Contributor Information
Aarti C. Bhat, Email: acb6009@psu.edu.
David M. Almeida, Email: dalmeida@psu.edu.
Andrew Fenelon, Email: afenelon@psu.edu.
Alexis R. Santos-Lozada, Email: ars39@psu.edu.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- Addo F.R., Darity W.A., Jr. Disparate recoveries: Wealth, race, and the working class after the Great Recession. The Annals of the American Academy of Political and Social Science. 2021;695(1):173–192. [Google Scholar]
- Assari S., Helmi H., Bazargan M. Vol. 7. Multidisciplinary Digital Publishing Institute; 2019. Health insurance coverage better protects blacks than whites against incident chronic disease; p. 40. (Healthcare). No. 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Auspurg K., Schneck A., Hinz T. Closed doors everywhere? A meta-analysis of field experiments on ethnic discrimination in rental housing markets. Journal of Ethnic and Migration Studies. 2019;45(1):95–114. [Google Scholar]
- Avery R.B., Rendall M.S. Lifetime inheritances of three generations of whites and blacks. American Journal of Sociology. 2002;107(5):1300–1346. [Google Scholar]
- Belsky J., Pluess M. Beyond diathesis stress: Differential susceptibility to environmental influences. Psychological Bulletin. 2009;135(6):885–908. doi: 10.1037/a0017376. [DOI] [PubMed] [Google Scholar]
- Benfer E.A., Vlahov D., Long M.Y., Walker-Wells E., Pottenger J.L., Gonsalves G., Keene D.E. Eviction, health inequity, and the spread of COVID-19: Housing policy as a primary pandemic mitigation strategy. Journal of Urban Health. 2021;98(1):1–12. doi: 10.1007/s11524-020-00502-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bunda K., Busseri M.A. Subjective trajectories for self-rated health as a predictor of change in physical health over time: Results from an 18-year longitudinal study. Social Cognition. 2019;37(3):206–228. [Google Scholar]
- Burgard S.A., Chen P.V. Challenges of health measurement in studies of health disparities. Social Science & Medicine. 2014;106:143–150. doi: 10.1016/j.socscimed.2014.01.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Card D., Dobkin C., Maestas N. Does Medicare save lives? Quarterly Journal of Economics. 2009;124(2):597–636. doi: 10.1162/qjec.2009.124.2.597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Case A., Deaton A., Stone A.A. Decoding the mystery of American pain reveals a warning for the future. Proceedings of the National Academy of Sciences. 2020;117(40):24785–24789. doi: 10.1073/pnas.2012350117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chinchilla M., Yue D., Ponce N.A. Housing insecurity among latinxs. Journal of Immigrant and Minority Health. 2021:1–10. doi: 10.1007/s10903-021-01258-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clair A., Hughes A. Housing and health: New evidence using biomarker data. Journal of Epidemiology & Community Health. 2019;73(3):256–262. doi: 10.1136/jech-2018-211431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cox R., Henwood B., Rodnyansky S., Rice E., Wenzel S. Road map to a unified measure of housing insecurity. Cityscape. 2019;21(2):93–128. [Google Scholar]
- Cutts D.B., Meyers A.F., Black M.M., Casey P.H., Chilton M., Cook J.T., Geppert J., de Cuba S.E., Heeren T., Coleman S., Rose-Jacobs R., Frank D.A. US housing insecurity and the health of very young children. American Journal of Public Health. 2011;101(8):1508–1514. doi: 10.2105/AJPH.2011.300139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeSilver D. Pew Research Center; 2020, May 30. For most U.S. workers, real wages have barely budged in decades.https://www.pewresearch.org/fact-tank/2018/08/07/for-most-us-workers-real-wages-have-barely-budged-for-decades/ Retrieved April 4, 2022, from. [Google Scholar]
- Desmond M., Kimbro R.T. Eviction's fallout: Housing, hardship, and health. Social Forces. 2015;94(1):295–324. [Google Scholar]
- Egede L.E., Walker R.J. Structural racism, social risk factors, and covid-19 — a dangerous convergence for black Americans. New England Journal of Medicine. 2020;383(12):e77. doi: 10.1056/NEJMp2023616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feagin J.R., Feagin C.B., Baker D.V. 6th ed. Pearson College Division; 2006. Social problems: A critical power-conflict perspective. [Google Scholar]
- Fenelon A., Mayne P., Simon A.E., Rossen L.M., Helms V., Lloyd P., Sperling J., Steffen B.L. Housing assistance programs and adult health in the United States. Public Health. 2017;107:571–578. doi: 10.2105/AJPH.2016.303649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gromis A. Princeton University, Eviction Lab; Princeton, NJ: 2019. Eviction: Intersection of poverty, inequality, and housing. [Google Scholar]
- Hepburn P., Louis R., Desmond M. Racial and gender disparities among evicted Americans. Sociological Science. 2020;7:649–662. [Google Scholar]
- Hoke M.K., Boen C.E. The health impacts of eviction: Evidence from the national longitudinal study of adolescent to adult health. Social Science & Medicine. 2021;273 doi: 10.1016/j.socscimed.2021.113742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Igarashi H., Hooker K., Coehlo D.P., Manoogian M.M. My nest is full:” Intergenerational relationships at midlife. Journal of Aging Studies. 2013;27(2):102–112. doi: 10.1016/j.jaging.2012.12.004. [DOI] [PubMed] [Google Scholar]
- Jones A., Grigsby-Toussaint D.S. Housing stability and the residential context of the COVID-19 pandemic. Cities & health. 2020:1–3. [Google Scholar]
- Keene D.E., Niccolai L., Rosenberg A., Schlesinger P., Blankenship K.M. Rental assistance and adult self-rated health. Journal of Health Care for the Poor and Underserved. 2020;31(1):325–339. doi: 10.1353/hpu.2020.0025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kiang M.V., Krieger N., Buckee C.O., Onnela J.P., Chen J.T. Decomposition of the US black/white inequality in premature mortality, 2010–2015: An observational study. BMJ Open. 2019;9(11) doi: 10.1136/bmjopen-2019-029373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim E.J., Kim T., Conigliaro J., Liebschutz J.M., Paasche-Orlow M.K., Hanchate A.D. Racial and ethnic disparities in diagnosis of chronic medical conditions in the USA. Journal of General Internal Medicine. 2018;33(7):1116–1123. doi: 10.1007/s11606-018-4471-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuebler M. Closing the wealth gap: A review of racial and ethnic inequalities in homeownership. Sociology Compass. 2013;7(8):670–685. [Google Scholar]
- Lachman M.E., Teshale S., Agrigoroaei S. Midlife as a pivotal period in the life course: Balancing growth and decline at the crossroads of youth and old age. International Journal of Behavioral Development. 2015;39(1):20–31. doi: 10.1177/0165025414533223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lankarani M.M., Assari S. Positive and negative affect more concurrent among Blacks than Whites. Behavioral Sciences. 2017;7(3):48. doi: 10.3390/bs7030048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lawler K. 2001. Coordinating housing and health care provision for America's growing elderly population. [Google Scholar]
- Lee B.A., Evans M. Forced to move: Patterns and predictors of residential displacement during an era of housing insecurity. Social Science Research. 2020;87 doi: 10.1016/j.ssresearch.2020.102415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leifheit K.M., Pollack C.E., Raifman J., Schwartz G.L., Koehler R.D., Bronico J.V.R.…Linton S.L. Variation in state-level eviction moratorium protections and mental health among US adults during the COVID-19 pandemic. JAMA Network Open. 2021;4(12) doi: 10.1001/jamanetworkopen.2021.39585. e2139585-e2139585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leifheit K.M., Schwartz G.L., Pollack C.E., Black M.M., Edin K.J., Althoff K.N., Jennings J.M. Eviction in early childhood and neighborhood poverty, food security, and obesity in later childhood and adolescence: Evidence from a longitudinal birth cohort. SSM-population health. 2020;11 doi: 10.1016/j.ssmph.2020.100575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Logan J.G., Barksdale D.J. Allostasis and allostatic load: Expanding the discourse on stress and cardiovascular disease. Journal of Clinical Nursing. 2008;17(7B):201–208. doi: 10.1111/j.1365-2702.2008.02347.x. [DOI] [PubMed] [Google Scholar]
- Ma C.T., Gee L., Kushel M.B. Associations between housing instability and food insecurity with health care access in low-income children. Ambulatory Pediatrics. 2008;8(1):50–57. doi: 10.1016/j.ambp.2007.08.004. [DOI] [PubMed] [Google Scholar]
- Manor O., Matthews S., Power C. Dichotomous or categorical response? Analysing self-rated health and lifetime social class. International Journal of Epidemiology. 2000;29(1):149–157. doi: 10.1093/ije/29.1.149. [DOI] [PubMed] [Google Scholar]
- Martin P.P., Weaver D.A. Social security: A program and policy history. Social Security Bulletin. 2005;66:1. [PubMed] [Google Scholar]
- McClure E., Feinstein L., Cordoba E., Douglas C., Emch M., Robinson W., Galea S., Aiello A.E. The legacy of redlining in the effect of foreclosures on Detroit residents' self-rated health. Health & Place. 2019;55:9–19. doi: 10.1016/j.healthplace.2018.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meschede T., Taylor J., Mann A., Shapiro T.M. Social Science Research Network; 2017. Family achievements?”: How a college degree accumulates wealth for whites and not for Blacks. [Google Scholar]
- Munnell A.H. What is the average retirement age. Center for Retirement Research. 2011;11(11):1–7. [Google Scholar]
- Neman T.S. Does your neighborhood's income distribution matter? A multi-scale study of financial well-being in the U.S. Social Indicators Research. 2020;152(3):951–970. [Google Scholar]
- Njai R., Siegel P., Yin S., Liao Y. Prevalence of perceived food and housing security—15 states, 2013. MMWR. Morbidity and Mortality Weekly Report. 2017;66(1):12. doi: 10.15585/mmwr.mm6601a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Novick T.K., Omenyi C., Han D., Zonderman A.B., Evans M.K., Crews D.C. Housing insecurity and risk of adverse kidney outcomes. The Kidney. 2020;1(4):241–247. doi: 10.34067/KID.0000032019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ong A.D., Williams D.R., Nwizu U., Gruenewald T.L. Everyday unfair treatment and multisystem biological dysregulation in African American adults. Cultural Diversity and Ethnic Minority Psychology. 2017;23(1):27–35. doi: 10.1037/cdp0000087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearlin L.I., Menaghan E.G., Lieberman M.A., Mullan J.T. Vol. 22. 1981. The stress process. (Source: Journal of health and social behavior). Issue 4. [PubMed] [Google Scholar]
- Piazza J.R., Almeida D.M., Dmitrieva N.O., Klein L.C. Frontiers in the use of biomarkers of health in research on stress and aging. Journals of Gerontology Series B: Psychological Sciences and Social Sciences. 2010;65(5):513–525. doi: 10.1093/geronb/gbq049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piazza J.R., Charles S.T., Sliwinski M.J., Mogle J., Almeida D.M. Affective reactivity to daily stressors and long-term risk of reporting a chronic physical health condition. Annals of Behavioral Medicine. 2013;45(1):110–120. doi: 10.1007/s12160-012-9423-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pollack C.E., Griffin B.A., Lynch J. Housing affordability and health among homeowners and renters. American Journal of Preventive Medicine. 2010;39(6):515–521. doi: 10.1016/j.amepre.2010.08.002. [DOI] [PubMed] [Google Scholar]
- Pynoos J. The future of housing for the elderly: Four strategies that can make a difference. Public Policy & Aging Report. 2018;28(1):35–38. [Google Scholar]
- Radler B.T. The midlife in the United States (MIDUS) series: A national longitudinal study of health and well-being. Open Health Data. 2014;2(1) doi: 10.5334/ohd.ai. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogers D., Power E. Housing policy and the COVID-19 pandemic: The importance of housing research during this health emergency. International Journal of Housing Policy. 2020;20(2):177–183. [Google Scholar]
- Rolfe S., Garnham L., Godwin J., Anderson I., Seaman P., Donaldson C. Housing as a social determinant of health and wellbeing: Developing an empirically-informed realist theoretical framework. BMC Public Health. 2020;20(1):1–19. doi: 10.1186/s12889-020-09224-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Routhier G. Beyond worst case needs: Measuring the breadth and severity of housing insecurity among urban renters. Housing Policy Debate. 2019;29(2):235–249. [Google Scholar]
- Sard B. Vol. 8. Center on Budget and Policy Priorities; 2009. (Number of homeless families climbing due to recession). [Google Scholar]
- Sharp G., Whitehead E., Hall M. Tapped out? Racial disparities in extrahousehold kin resources and the loss of homeownership. Demography. 2020;57(5):1903–1928. doi: 10.1007/s13524-020-00913-4. [DOI] [PubMed] [Google Scholar]
- Stahre M., VanEenwyk J., Siegel P., Njai R. Housing insecurity and the association with health outcomes and unhealthy behaviors, Washington State, 2011. Preventing Chronic Disease. 2015;12(7) doi: 10.5888/pcd12.140511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Surachman A., Jenkins A.I., Santos A.R., Almeida D.M. Socioeconomic status trajectories across the life course, daily discrimination, and inflammation among Black and white adults. Psychoneuroendocrinology. 2021;127 doi: 10.1016/j.psyneuen.2021.105193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swope C.B., Hernández D. Housing as a determinant of health equity: A conceptual model. Social Science & Medicine. 2019;243 doi: 10.1016/j.socscimed.2019.112571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vásquez-Vera H., Palència L., Magna I., Mena C., Neira J., Borrell C. The threat of home eviction and its effects on health through the equity lens: A systematic review. Social Science & Medicine. 2017;175:199–208. doi: 10.1016/j.socscimed.2017.01.010. [DOI] [PubMed] [Google Scholar]
- Weston S.J., Graham E.K., Turiano N.A., Aschwanden D., Booth T., Harrison F.…Donnellan M.B. Is healthy neuroticism associated with chronic conditions? A coordinated integrative data analysis. Collabra: Psychology. 2020;6(1) doi: 10.1525/collabra.267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams D.R., Mohammed S.A. Discrimination and racial disparities in health: Evidence and needed research. Journal of Behavioral Medicine. 2009;32(1):20–47. doi: 10.1007/s10865-008-9185-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woo J., Lehrer H.M., Whyne E., Steinhardt M. The longitudinal association of psychological resources with chronic conditions and the mediating roles of health behaviours and allostatic load. Psychology and Health. 2020;35(5):629–643. doi: 10.1080/08870446.2019.1656205. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.