Abstract
The current understanding of major depressive disorder (MDD) and bipolar disorder (BD) is plagued by a cacophony of controversies as evidenced by competing schools to understand MDD/BD. The DSM/ICD taxonomies have cemented their status as the gold standard for diagnosing MDD/BD. The aim of this review is to discuss the false dogmas that reign in current MDD/BD research with respect to the new, data-driven, machine learning method to model psychiatric illness, namely nomothetic network psychiatry (NNP). This review discusses many false dogmas including: MDD/BD are mind-brain disorders that are best conceptualized using a bio-psycho-social model or mind-brain interactions; mood disorders due to medical disease are attributable to psychosocial stress or chemical imbalances; DSM/ICD are the gold standards to make the MDD/BD diagnosis; severity of illness should be measured using rating scales; clinical remission should be defined using threshold values on rating scale scores; existing diagnostic BD boundaries are too restrictive; and mood disorder spectra are the rule. In contrast, our NNP models show that MDD/BD are not mind-brain or psycho-social but systemic medical disorders; the DSM/ICD taxonomies are counterproductive; a shared core, namely the reoccurrence of illness (ROI), underpins the intertwined recurrence of depressive and manic episodes and suicidal behaviors; mood disorders should be ROI-defined; ROI mediates the effects of nitro-oxidative stress pathways and early lifetime trauma on the phenome of mood disorders; severity of illness and treatment response should be delineated using the NNP-derived causome, pathway, ROI and integrated phenome scores; and MDD and BD are the same illness.
Keywords: Nomothetic network psychiatry, Depression, Mood disorders, Affective disorders, Inflammation, Oxidative and nitrosative stress, Neuro-immune
Core Tip: We review the merits of machine learning-derived nomothetic network psychiatry (NNP) models of mood disorders. The NNP models of mood disorders show that major depressive disorder/bipolar disorder are not mind-brain or psycho-social but systemic medical disorders. The DSM/ICD taxonomies are counterproductive. A shared core, namely the reoccurrence of illness (ROI), underpins the intertwined recurrence of depressive and manic episodes and suicidal behaviors. Mood disorders should be ROI-defined. ROI mediates the effects of nitro-oxidative stress pathways and early lifetime trauma on the phenome of mood disorders. Severity of illness and treatment response should be delineated using NNP-derived causome, adverse outcome pathways, ROI and phenome scores.
INTRODUCTION
The current status-quo view is that mood disorders are disorders of the brain associated with chemical imbalances and should be regarded as mental disorders with a multi-factorial etiology. The status-quo is that mood disorders should be diagnosed using DSM criteria[1] or ICD[2] criteria and that different subtypes of mood disorders exist including unipolar [major depressive disorder (MDD)] and bipolar disorder (BD), either manic or a major depressive episode (MDE). It is thought that MDD and BD-type 1 (BP1) are qualitatively distinct categories, although MDD and BD-type 2 (BP2) show quantitative differences. Furthermore, both MDD and BD show many comorbidities with neurological and medical disease and depression due to these conditions may be explained by psychosocial factors including loss of health or independence. Moreover, the status-quo dictates that severity of illness should be measured using the summed score of items of rating scale scores that assess depressive symptoms.
The conceptual MDD/BD frameworks are plagued with a cacophony of controversies, as evidenced by competing and even mutually antagonistic approaches to understanding these disorders including psychoanalysis (depression is a defense against loss and mourning), psychodynamic psychiatry (depression is the consequence of a pathological object relationship between parts of the self), commonsense or folk psychology (depression is a response to a psychological problem), self-system therapy (the primary factor in depression is problematic self-regulation), systemic therapy (systems e.g., the family create depression), biological psychiatry (depression is the consequence of chemical aberrations in the brain, e.g., a deficiency in serotonin), animal experiments (depression is sickness behavior or is the consequence of learned helplessness), the biopsychosocial model (biological as well as psychosocial factors are involved), cognitive-behavioral therapy (depression is the consequence of negative cognitions), cognitive neuropsychiatry (cognitive impairments in memory or attention are involved), the mind-brain dualism (mental and neural processes interact to cause depression), postpsychiatry (community development and engagements with communities are central and boredom and depression are the characteristic moods of our epoch), molecular psychiatry (genes and intracellular networks explain depression) and pan-omics and precision psychiatry (pan-omics data will reveal the true nature of depression phenotypes or transdiagnostic pathway-phenotypes). A latest new development, which indicates that contemporary psychiatry faces a profound crisis, is critical psychiatry with psychiatric survivor networks which question psychiatric practice, treatment, scientific methods, knowledge base, and the decontextualization of experience, and accuse status quo psychiatrists of harmful and unethical principles[3-5].
Another new direction in psychiatry is the research domain criteria (RDoC) developed by the National Institute of Mental Health (NIMH)[6]. Apart from criticizing and further undermining the credibility of the DSM categorizations, RDoC relies on dimensions as critical measures of psychopathology, which arises from aberrations in neural circuits in the brain, and should be examined by a matrix with 8 columns (genes, molecules, cells, circuits physiology, behavior, self-reports and paradigms) and a number of rows including memory, rewards, threat and perception. Nevertheless, there is no evidence base for the RDoC matrix approach which is developed in a top-down manner.
All medical disciplines, except psychiatry, are exclusively based on nomothetic network definitions of disease, as a default mode of clinical and research operations. The term “nomothetic” means the tendency to derive laws from indicator (independent) variables, which explains the variability in phenomena and allows us to generalize the model[7-9]. Nomothetic definitions include a variety of biological signatures which correspond to clinical measures and constitute drug targets for implementation of treatment. For example, the diagnosis of atherosclerosis, implies that the patient suffers from atherosclerotic plaques caused by a defined process which progressively worsen. In contrast, the diagnosis of MDD and BD according to DSM/ICD criteria are mere de-contextualized narratives devoid of any explanatory mechanisms.
The aim of this paper is to review the many false dogmas which determine current research in mood disorders; and to discuss these flaws with respect to the new, data-driven, machine learning method to model psychiatric illness, namely nomothetic network psychiatry (NNP)[10-13]. In line with a dichotomy[14], it could be considered that there is a co-existing of two major types of scientific psychiatric knowledge. The first is idiographic and is driven by “understanding” of subjective experiences and inter-subjective narratives, and the second is nomothetic and is governed by laws of natural and mathematical sciences representing explanatory models of disease[15,16]. With every respect and awareness of the values represented in subjective narrative and relevant cultural contexts[17], in this review we focus on the many caveats in scientific psychiatry which undermine the nomothetic approach. Moreover, we show that our novel nomothetic models also contain subjective experiences of the patient and that these idiographic experiences increase the richness and complexity of the nomothetic models. Finally, we will introduce a new mathematical index reflecting the reoccurrence of illness (ROI), which is a key factor in our nomothetic models[18,19].
NNP
NNP models
None of the previous psychiatric models tried to reunite the different buildings blocks of an illness into a data-driven model which includes causome and protectome features (or a deduced risk/resilience ratio), adverse-outcome pathways (AOPs), brainome features (the aggregate of aberration in brain regions), cognitome features (the aggregate of cognitive impairments), and ROI, symptomatome (the aggregate of different symptom domains or clinical phenotypes), and phenomenome (the self-description of the self-experience of the illness) features[10-13].
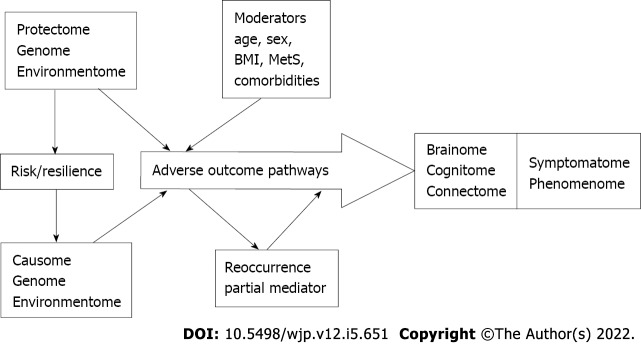
Figure 1 displays a theoretical framework of MDD/BD which is based on current state-of-the-art knowledge and causal reasoning and reunites the different building blocks into a causal model. It should be noted that this framework allows for the entry and analysis of a wide range of data into the model, including genome (genomics) and environmentome (psychosocial aspects, context-centered hermeneutic data), pan-omics data, functional brain imaging including connectome data, neurocognitive test results, descriptive psychopathological assessments including symptoms rated via interviews, and idiographic or phenomenological features as assessed with self-rating scales, including health-related quality of life (HR-QoL) data.
Figure 1.
Theoretical framework of mood disorders. Adapted from Maes et al[10]. BMI: Body mass index; Mets: Metabolic syndrome.
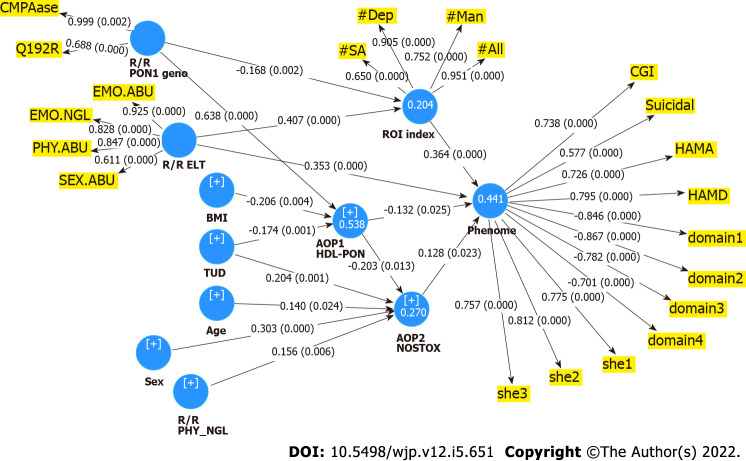
This theoretical causal framework can be tested and validated using partial least squares (PLS) pathway analysis[10-13]. Figure 2 shows the outcome of such a PLS model (NNP1) comprising causal links between three risk/resilience ratios, namely early lifetime trauma (ELT) indicators and paraoxonase (PON)1 genotype combined with PON1 enzymatic activity, two AOPs, namely an antioxidant and a neuro-oxidative toxicity indicator, one ROI-index, and the phenome of mood disorders[10]. In NNP1, the severity of ROI is represented as a reflective latent vector extracted from the number of lifetime depressive episodes in MDD, (hypo)manic and depressive episodes in BD and number of lifetime suicidal attempts in either MDD or BD[10]. The phenome of mood disorders is conceptualized as a factor (latent vector) extracted from symptomatome features (severity of depression, anxiety and global clinical impression and current suicidal ideation) and phenomenome features, including self-rated disabilities (scoring three subdomains, namely work/school, social and family) and self-rated HR-QoL (four subdomains, namely physical and psychological health, and social relationships and environment)[10].
Figure 2.
Results of partial least squares analysis. R/R: Risk/resilience; AOP: Adverse outcome pathways; PON1: Paraoxonase; ELT: Early lifetime trauma; EMO.ABU: Emotional abuse; EMO.NEGLECT: Emotional neglect; PHY.ABU: Physical abuse; PHY.NGL: Physical neglect; SEX.ABU: Sexual abuse; BMI: Body mass index; HDL: High density lipoprotein cholesterol; NOSTOX: Nitro-oxidative stress toxicity; ROI: Reoccurrence of illness; Dep: Depressive; Man: (Hypo)mania; SA: Suicide attempts; CGI: Clinical global impression; HAMD/HAMA: Hamilton Depression and Anxiety Rating Scale; Domains (1-4): Domains of the WHO-Quality of Life questionnaire; She (1-3): Sheehan Disability Scale (domains 1-3).
Simeonova et al[12] constructed another NNP model (NNP2) whereby indicants of increased bacterial translocation [increased immunoglobulin (Ig)A and IgM responses to lipopolysaccharides (LPS) of specific Gram-negative bacteria] were entered as causome factors leading to three AOPs, namely increased autoimmune responses to oxidized low-density lipoprotein, peroxide levels and IgM responses to a multitude of oxidative specific epitopes. These three AOPs and an ROI index significantly predict the phenome which was conceptualized as a factor extracted from the severity of illness score, the presence of mood disorders, MDD and BP1, treatment resistance and melancholia.
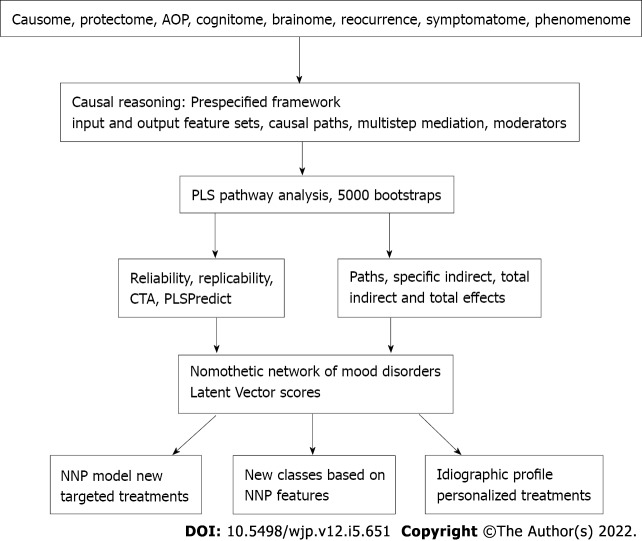
Figure 3 shows how PLS analysis was employed to construct and validate novel NNP models. As explained previously, different statistical tests should be used to validate the outer and inner models and the PLS models[11]. Goodness of fit should be checked with standardized root mean square residuals to avoid model misspecifications. The validity reliability of the latent factors should be checked using composite reliability, rho A, or Cronbach’s alpha and the average variance extracted. All indicators of the latent vectors should display loadings > 0.5 or by preference > 0.66[10-12] and Confirmatory Tetrad Analysis should be employed to check whether the latent factors are not mis-specified as reflective models. Other tests including blindfolding and PLS predict with 10-fold cross-validation and may be used to assess the predictive value of the model[10-13]. There are different methods to determine, a priori, the estimated number of cases including methods based on the psychometric properties and the strength of the intercorrelations among the factors and the factor loadings, the number of arrows pointing to a latent factor and its explained variance, and power analysis specific to multiple regression analysis[11]. An advantage is that these methods show that relatively small sample sizes of 70-127 cases may be sufficient to achieve a power of 0.8[11]. Most importantly, complete PLS analysis conducted on bootstrapped samples (e.g., 5.000) allows to compute the path coefficients with P values as well as the specific indirect, total indirect and total effects. This method allows to examine multi-step and multiple mediation paths as for example the links from PON1 genotype to ROI to phenome, and PON1 genotype to AOP1 and to AOP2 to phenome.
Figure 3.
How to construct nomothetic network psychiatry models and disclose new patient clusters. AOP: Adverse outcome pathways; PLS: Partial least squares; CTA: Confirmatory Tetrad Analysis; NNP: Nomothetic network psychiatry.
As such we were able to build reliable and replicable, bottom-up, data-driven nomothetic models of BD/MDD, which comprise key features of mood disorders assembled in a knowledge-based causal framework as indicated in Figures 1 and 2[10-13]. These NNP models integrate phenome with functional and molecular pathways and, therefore, “translate” those pathways into phenome features thereby objectivating the clinical phenome, a method named “reification of the clinical diagnosis”[10-13]. The NNP method also allows to construct pathway-phenotypes (biosignatures), for example, by constructing latent vectors which comprise pathway and phenome features[20] and pathway classes, as described in the next section.
Importantly, our NNP models may pass critical rationalism tests as proposed by Popper[21]. First of all, our NNP models can be refuted or corroborated and, thus, are falsifiable. Second, our NNP frameworks are based on state-of-the-art knowledge including on causome, protectome, AOP, and phenome data and, thus, are progressive. Third, new research should elaborate on our NNP models and enrich the indicators or feature sets with pan-omics and brainome data, delete less robust features and therefore, our models are changeable and provisional. Finally, through feature selection (only significant indicators are included in the model) and feature reduction (latent vectors are constructed based on strongly related indicators), our NNP models are parsimonious representations of the building blocks of the illness.
NNP networks reveal drug targets at the model and idiographic level
Once the nomothetic network is constructed, latent variable scores may be calculated which reflect the severity of causome factors, interactions between causome and protectome factors (for example, integrated in a risk/resilience ratio), different AOPs, the ROI-index and the phenome. These latent variable scores, therefore, reflect severity of the different building blocks of the illness. Our NNP models also contain idiographic features as for example self-rated severity of depression and anxiety, and self-rated HR-QoL and disabilities[10]. As a consequence, those latent variable scores not only define the nomothetic network model, but also an idiographic image or feature profile which is unique for every individual.
Consequently, our NNPs disclose new drug targets: (1) At the model level, namely causome factors such as PON1 activity, ELT, bacterial translocation; AOPs, including damage due to oxidative and nitrosative stress (O&NS) and lowered antioxidant defenses, and ROI, which is in part determined by causome features; and (2) In each individual because the idiomatic profile discloses specific aberrations.
New classifications based on NNP features
The NNP factor scores may be employed in consequent unsupervised machine learning techniques including clustering analysis methods to expose novel natural clusters of patients. Previously[10-12], we used K-median, Two-step, K-mean, Ward and Forgy’s clustering analysis to discover new categories based on the causome, AOPs, ROI and phenome latent vectors. Cluster analysis conducted on NNP1 models disclosed that 69.5% of mood disorder patients were allocated to a cluster with increased causome factors (interaction PON1 genotypes and PON1 enzymatic activity and ELT), O&NS-associated AOPs and increased ROI and phenome scores. Cluster analysis conducted on the NNP2 model showed that around 70% of the patients were allocated to a cluster with increased bacterial translocation, O&NS-associated AOPs and phenome severity[12]. Consequently, we have proposed to name the clusters with high causome, AOP, and ROI scores “Major DysMood Disorder due to neuro-affective toxicity” and the cluster with normal causome and AOP scores “DysMood Disorder”[10,12].
NNP-associated pathways
Nevertheless, both NNP1 and NNP2 are limited in that they focus on O&NS-related and bacterial-derived features and do not comprise other well-known causome/AOP factors of mood disorders, such as indicants of activated immune-inflammatory pathways[22]. The latter will be addressed in other NNP models as reviewed in false dogmas in mood disorders. Using (un)supervised learning techniques, we repeatedly showed that large subgroups of patients with mood disorders (MDD or MDE) show signs of immune activation including increased expression of T cell activation markers such as CD7+, CD25+ and CD2+, human leukocyte antigen (HLA)DR+ and cell surface antigens such as CD25+ [interleukin (IL)-2 receptor], class II Major Histocompatibility Complex HLA-DR, CD4+CD45RA, CD4+CD45RA+ and surface Ig[23,24]. These findings were further corroborated by data that mood disorders are accompanied by: (1) Increased levels of pro-inflammatory cytokines including IL-2, IL-1β, interferon (IFN)-γ and tumor necrosis factor (TNF)-α; (2) Increased expression of positive acute phase proteins such as haptoglobin and C-reactive protein (CRP); and (3) Lowered levels of negative acute phase proteins including albumin[22,25]. Based on these findings, there is now evidence that MDD/BD are immune-inflammatory and O&NS (IO&NS) disorders[22,25].
Enrichment and annotation analysis using the Gene Ontology knowledgebase pathways (Gene Ontology Resource) indicates that the protein-protein interactions in mood disorders are associated with peripheral IO&NS pathways which are highly significantly associated with a response to a bacterium, a response to LPS, or a cellular response to LPS, indicating that the increased bacterial translocation established in NNP2 is causally associated with IO&NS pathway activation (Maes et al, personal data). Moreover, the GO computational model of biological systems (Gene Ontology Resource) also shows that the IO&NS profile established in mood disorders is accompanied by different impairments in neuronal functions including microglial cell activation and neuroinflammation, positive regulation of gliogenesis, modulation of chemical synaptic transmission, synapse assembly, neurogenesis and neuroblast proliferation, axonogenesis, regulation of axon extension, retrograde axonal transport, synaptic pruning and more functional and molecular pathways (Maes et al, personal data). As explained previously, the pathway findings in mood disorders may be summarized as indicating increased neurotoxicity and reduced neuroprotection leading to IO&NS-induced neuro-affective toxicity[22,25].
Recently, dysfunctional and degenerative processes were established in the brain of mood disorder patients. For example, altered expressions of connectome circuits in the brain were established including downregulated anterior insula connectivity, and upregulated circuits from middle frontal gyrus and hippocampus to the frontal eye fields, the anterior insula to the amygdala and middle frontal gyrus to the amygdala (Kandilarova et al[26], to be submitted). Moreover, using a voxel-based morphometry method using a 3Т magnetic resonance imaging (MRI) system, Kandilarova et al[26] reported that MDD is characterized by significant reductions in grey matter volume in anterior cingulate cortex and medial frontal and regions on the left side, and inferior frontal gyrus, middle frontal gyrus, medial orbital gyrus and middle temporal gyrus on the right side. Such gray matter degeneration and dysfunctional brain connectome circuits may be predicted by increased neurotoxicity affecting brain functions and neuronal circuits[22,25]. It follows that our NNP1 and NNP2 models should be enriched with connectome (fMRI measurements) and brainome (e.g., MRI measurements) features, yielding causal pathways from peripheral or gene X environmental interactions to peripheral AOPs to central AOPs to connectome and brainome to ROI to phenome. We will now discuss false dogmas in mood disorders research with respect to the new knowledge obtained in our NNP models.
FALSE DOGMAS IN MOOD DISORDERS
False dogma 1: Mood disorders are mind-brain disorders that are best conceptualized using a bio-psycho-social model or mind-brain interactions
MDD/BD is most often conceptualized as a brain - mind illness as it is thought that the brain mediates the mind and that psychosocial factors may alter the brain - mind axis to cause mood disorders[27]. Another predominant view is that MDD/MDE are brain disorders which are caused by a faulty mood regulation as a consequence of interactions between a number of factors including biological features, genetic vulnerability, psychosocial stressors including losses and ELT, temperament and comorbidities[28]. Other theories posit that psychosocial stressors cause changes in chemicals (e.g., serotonin) especially in the brain regions which mediate mood, affection and reward including the thalamus, amygdala and hippocampus[28]. According to Kendler[29], the goal should be to understand how the psychosocial environment interacts with the networks within the mind-brain system that cause psychiatric illnesses. Accordingly, Kendler[29] proposed a philosophical structure for psychiatry with the acceptance of a bidirectional brain to mind and mind to brain causality. Nevertheless, the discussions as exemplified in Kendler[29]’s paper are reductionist. Why would psychosocial stressors be the sole stressors that induce MDD/MDE, while other environmentome variables such as viral and bacterial infections, environmental toxins and dietary factors are not taken into account?
Nevertheless, as described in NNP-associated pathways, we have shown that MDD/BD may have a peripheral origin and as a consequence should be regarded as a systemic disease. There is a growing realization that the AOPs of mood disorders are ‘holistic’ in nature comprising not only central but also peripheral processes. Thus, NNP2 showed that increased gut permeability and increased peripheral levels of neurotoxic substances (including LPS) are major causome factors in mood disorders which, in turn, may cause activated peripheral IO&NS pathways and neuroinflammation[22,25,30]. Our NNP models showed causal links from strictly peripheral factors (bacterial translocation) or gene X environmental interactions (PON1 gene x ELT) to AOPs (IO&NS pathways) and ROI to phenome. Enrichment and annotation analysis show how these peripheral pathways may cause neuro-affective toxicity which may explain fMRI and 3T MRI findings and the phenome of mood disorders (see NNP-associated pathways). Moreover, it should be added that a larger part of the variance in the severity of the phenome is explained by direct and indirect effects of causome, AOP and ROI features, namely around 57.7% and 44.2% in NNP2 and NNP1, respectively[10,12]. This evidence contrasts the view that mood disorders should be regarded as pure brain disorders or mind-brain disorders and that mind to brain causality and or psychosocial stress to brain dysfunctions are the main drivers of the illness.
False dogma 2: Mood disorders due to brain disease are attributable to psychosocial stress or chemical imbalances
A number on neurological brain disorders are associated with MDD/MDE (symptoms) including Parkinson’s and Alzheimer’s disease, multiple sclerosis, stroke and Huntington’s disease[31]. The widely held belief is that comorbid depression is caused by chemical imbalances in the brain (e.g., dopamine and serotonin), or that it is the result of negative thoughts following a diagnosis, helplessness, severe stress from living with a medical disorder, loss of independence or as a side effect of medication used to treat brain disorders[28]. Nonetheless, comorbid depression may worsen the morbidity and cause increased mortality of some brain disorders and the existence of depression may precede some neurological disorders, such as Alzheimer’s and Parkinson’s disease, implying that depression is a key component of these conditions[31].
In addition, in these neuro-immune and neurodegenerative brain disorders, depressive symptoms are associated with increased IO&NS pathways. For example, depression due to multiple sclerosis is associated with increased IL-6 and lowered albumin[32]. Depression due to stroke is largely predicted by hypertension and atherosclerosis as indicated by white matter hyperintensities (assessed with T2-weighted and fluid-attenuated inversion recovery MRI) and the volume of the acute stroke lesions (measured with diffusion-weighted MRI)[33]. White matter hyperintensities are a consequence of a chronic mild inflammatory process while the acute stroke lesions are accompanied by peripheral and central IO&NS responses[34-36]. The severity of the disabilities induced by stroke was not associated with the onset of depressive symptoms, indicating that the latter are a consequence of IO&NS pathways associated with the cause of stroke (atherosclerosis) as well as the systemic inflammation and neurodegeneration due to stroke[33]. In schizophrenia, another systemic neuro-immune disease[20], the severity of depression and manic symptoms is significantly associated with IO&NS indicants including increased levels of IL-6, high mobility group box1 and cytokine-induced activation of the tryptophan catabolite pathway[37,38]. In temporal lobe epilepsy (TLE), depression, anxiety and excitation aggregate with the clinical hallmarks of the illness (including seizure frequency, controlled vs uncontrolled TLE, presence of post-ictal confusion and aura) and a latent vector extracted from these clinical features is associated with PON-1 genotype-associated reductions in enzyme activity[39,40]. Furthermore, affective symptoms in TLE are strongly associated with protein oxidation and aldehyde formation and lowered-thiol groups indicating that damage to oxidative stress plays a key role in affective symptoms due to TLE[39,40]. In Parkinson’s disease, increased CRP, and chemokine (C-C motif) ligand 2 (a pro-inflammatory chemokine) are associated with the severity of depressive symptoms[41].
To sum it up, the current theory that depression in neuroinflammatory and neurodegenerative brain disorders is caused by psychological stress or chemical imbalances in neurotransmission is at best skewed toward reductionism and should be abandoned in favor of the novel findings that (neuro)inflammatory processes are to blame for these disorders’ associated mood symptoms.
False dogma 3: Mood disorders due to comorbid systemic illness are attributable to psychosocial stress
According to the ABC of psychiatric medicine, depression caused by medical diseases is explained by a variety of stressors linked to the illness, such as functional losses, the personal meaning ascribed to these stressors and attitudes about the illness itself[42]. Furthermore, personality traits, social support and stage of life, as well as earlier experiences, modify those personal meaning and beliefs[42]. Once sadness, anxiety and somatic distress appear, the risk to develop depressive disorders and persistent subthreshold symptoms is increased and modified by social support, medical complications, genetic loading and coping strategies.
It appears that these authors and the psycho-social school in general take for granted that a load on the mind-brain pathway causes depression, a folk psychology explanation. Folk or commonsense psychology explains the “mental state” of behaviors as the outcome of daily life experiences, as for example, “depression” is a response to a perception, pain, a belief, etc[11]. Based on these folk-like theories, treatment plans are then worked out to treat depression due to medical disease and these comprise advice, education and reassurance, specialized cognitive or dynamic behavioral psychotherapies, interpersonal therapy, problem solving and of course antidepressant treatment[41]. Some of these treatments may even be performed by non-specialists in primary and secondary care, including cognitive therapy to correct distorted thinking, encourage a sense of mastery and promote more accurate coping strategies.
Nevertheless, this psycho-social dogma fails to explain how or why the mind or mental pathways could lead to the behavioral and cognitive changes associated with MDD/MDE. In fact, depression due to a variety of medical illnesses may be attributed to the activated IO&NS pathways which characterize these disorders[31]. Thus, diabetes mellitus type 1 and 2, rheumatoid arthritis, inflammatory bowel disease, atherosclerosis, lupus erythematosus, chronic obstructive pulmonary disease, chronic kidney disease and psoriasis are all IO&NS disorders accompanied by a significantly higher prevalence of mood disorders[31]. The post-partum period, blood dialysis and IFN-α treatment are frequently accompanied by depression and also these conditions are characterized by activated IO&NS pathways[31].
New evidence shows that activated peripheral IO&NS pathways are directly associated with depressive symptoms in medical disorders. For example, depression is strongly comorbid with chronic apical periodontitis (CAP)[43]. Root canal LPS levels are increased in patients with CAP and are significantly associated with clinical depression due to CAP, as well as with severity of depression and HR-QoL[43]. Moreover, MDD due to CAP is characterized by increased indicants of O&NS including increased nitric oxide metabolites, lipid hydroperoxides and advanced oxidation protein products[43].
Moreover, previous NNP research examining depression associated with medical disease demonstrated that depressive and anxious symptoms are part of the same clinical core that encompasses the characteristics of those medical disorders. For example, in atherosclerosis and unstable angina, depression severity is substantially associated with the same core (latent vector), which also includes clinical characteristics such as atherosclerosis, unstable angina, class III/IV unstable angina and enhanced atherogenicity and insulin resistance[43]. The latter features are reflective manifestations of a common core, namely severe heart disease, which, therefore, is the cause of its manifestations. Moreover, a larger part of the variance (66.6%) in this common core was explained by peripheral IO&NS pathways[44].
A recent NNP constructed in children with depression due to transfusion-dependent thalassemia showed that depressive symptoms are strongly associated with indicants of peripheral iron-overload and immune-inflammatory responses caused by thalassemia and the repeated transfusions[45]. Moreover, the constructed NNP model showed that iron-overload indices (increased iron and ferritin) and immune-inflammatory biomarkers (increased IL-1β, TNF-α and IL-10) and key depressive subdomains such as sadness, physio-somatic symptoms (fatigue and pain), social isolation and irritability symptoms and lowered self-esteem belong to the same core. Furthermore, 73.0% of the variance in this common core was explained by number of transfusions and hospital admissions and use of Desferal[45].
We constructed another NNP in depression due to type 2 diabetes mellitus and established that 61.7% of the variance in depressive and anxiety symptoms could be explained by indicants of immune activation and the combined effects of insulin resistance and atherogenicity, which partially mediated the effects of immune activation on depressive symptoms[46]. In patients with depression and anxiety due to established coronavirus disease 2019 infection, we found that 70.0% of the variance in the severity of affective symptoms was explained by the combined effects of lung inflammation (as assessed with lung computed tomography scan) and reduced oxygen saturation and that these effects were partially mediated by IL-6, IL-10, CRP, soluble advanced glycation products and lowered albumin[47]. Overall, the current view that depression caused by medical disorders should be explained by losses or beliefs about the illness is at best reductionist and should be replaced by NNP models indicating that activated IO&NS pathways in medical disease are responsible for comorbid depression.
False dogma 4: DSM/ICD are the gold standards to make the MDD/BD diagnosis
MDD/MDE are commonly defined as a cluster of symptoms which are more severe than sadness and may be discriminated from the latter by the duration of symptoms (more than two weeks according to DSM) and the number of symptoms (more than 5 in DSM). However, the decision whether a patient suffers from MDD/MDE rather that a sadness reaction is made by the clinician (either psychiatrist or general practitioner) who will treat the patient with antidepressants depending on whether MDD is present or not. BD formerly known as manic-depressive psychosis is characterized by recurrent episodes of MDE and mania (BP type 1) or hypomania (BP type 2). ICD classifies “mood disorders” which is further subdivided into MDD and BD, whereas the DSM-5 classifies two separate categories, namely MDD and BD[1,2].
Nevertheless, there are several serious problems with the DSM/ICD case definitions of MDD, MDE and BD, BP1 and BP2. First, the case definitions are often unreliable with an intraclass kappa reliability of 0.28 indicating minimal agreement among psychiatrists[48,49]. Furthermore, the DSM case definitions of affective disorders are unreliable and invalid[49,50]. BD is often over diagnosed with studies showing that only 42.9% of patients diagnosed with the DSM criteria of BD meet the diagnostic criteria[50]. The misdiagnosis rate is associated with the low demarcation of BD from personality disorders including borderline personality disorder, polysubstance abuse and attention deficit disorder[50]. BD patients are often misclassified as suffering from MDD or other conditions with a rate as high as 60%[51]. Another major problem is that the diagnosis of BD is often underrated when the patient presents with a depressive index episode and an atypical course of manic or hypomanic symptoms[50].
A more fundamental flaw of the DSM/ICD case definitions of mood disorders is their top-down manner of generation[11]. Both taxonomies diagnose mood disorders prior to biomarker and neurocognitive investigation, treating these features as ancillary data that may or may not support the diagnosis[10-13]. Most current biological, neurocognitive and molecular research employs these top-down case definitions as independent variables, while the key features and even causome, protectome and cognitome features are employed as dependent variables in statistical analyses. Nevertheless, causal reasoning indicates that those features should be the explanatory variables, while the diagnosis of mood disorders is a higher-order concept constructed using these features[10-12]. Based on these inadequate model assumptions, researchers then use unreliable diagnostic classes, based on value laden and controversial criteria, as explanatory variables in analysis of variance to analyze biomarker levels, brainome data, and neurocognitive test scores and sometimes even causome/protectome data. As such, current biomarker research continues to employ unreliable diagnostic classes applied in inadequate model assumptions further confounded by the use of inappropriate statistical analysis[10,11]. Overall, no falsification of the dogma-like, top-down DSM/ICD classes or criteria is possible using data from sources other than the DSM/ICD, precluding a deductive approach[11].
False dogma 5: Severity of illness should be measured using rating scales
Another gold-standard dogma is that the severity of mood disorders should be assessed using rating scales such as the Hamilton Depression Rating Scale (HDRS)[52]. Instruments which aim to assess severity of depression encompass a number of observable or self-rated symptoms including loss of interest, sadness, fatigue, concentration problems, insomnia, lowered self-esteem, feelings of worthlessness or suicidal ideation. Because psychiatrists consider such symptoms to be reflective measurements of an underlying phenomenon, they typically add the scores on the separate items and construct an unweighted sum-score, which is thought to reflect severity of illness. However, to compute such sum scores, rating scales should be unidimensional, i.e., all items should load heavily on one primary factor that has additional adequate psychometric properties[53,54]. We discussed before[54] that the indicators of latent vectors should have loadings > 0.5 with Cronbach alpha > 0.7, composite reliability > 0.8, and average explained variance > 0.5 while Confirmatory Tetrad Analysis should show that the model is not mis-specified as a reflective model. Our analyses showed that the HDRS (and other scales as well) do not comply with these criteria and that the total unweighted sum of the items may not be used as a severity index. Fried et al[53] reported that the HDRS and other commonly used rating scales of depression do not comply with the unidimensionality criterion. Moreover, these rating scales cannot be used as outcome variables in randomized controlled studies because in order to interpret repeated measurements, rating scales must be unidimensional and show measurement invariance[53].
There are more serious issues with the rating scales currently in use. Numerous items on these rating scales are based on descriptions from folk psychology, such as “I feel down”, “I feel depressed”, “I cry easily”, “I feel sad” and “I feel disappointed”. To obtain meaningful data for psychiatric inventories, folk psychology-like terminology is translated into Likert scale items and useful statistical entities are created after some window dressing[11]. As such, commonsense psychology terms are used as proxies for severe symptoms such as anhedonia and feelings of guilt and incorporated as criteria to make the diagnosis of mood disorders without reference to any independent validator, including causome, AOP or brainome markers.
Of course, psychological concepts such as mood cannot be directly assessed, but the best approach is to assess multiple observable manifestations of the underlying construct, which is the cause of the covariation among its indicators. In fact, our NNP models consist of unidimensional, reliable, validated and replicable latent vectors, including a phenome latent vector[10]. In fact, the severity of illness should not be assessed using one folk-psychology-derived rating scale, but by the causome, AOP, ROI and phenome latent vector scores. The latter should be based on various assessments including interview-based measurements of illness severity and suicidal ideation, and self-rated scores, including HR-QoL and disabilities[10]. We are aware that the final reflective latent vector (based on feature selection and reduction), will almost certainly contain folk psychology-like expressions, but this is less significant in the context of a NNP model, as the clinical phenome latent vector is reified as a concrete construct.
False dogma 6: Clinical remission should be defined using threshold values on rating scale scores
It is common practice to employ rating scale scores to define remission and partial remission. For example, influential psychiatrists, including Eugene Paykel, David Kupfer, Michael Thase and Roger McIntyre developed criteria to delineate remission and partial remission based on a single depression rating scale score, often the HDRS. However, such methods are not accurate. Firstly, as described above, the HDRS cannot be employed as a measure of change during treatment[54]. Secondly, and more importantly, remission, partial remission and relapse should be defined using the modifiable building blocks of the illness (thus excluding genotypes and the ROI-index), namely causome, AOP, cognitome, brainome and phenome features as computed in our NNPs.
Furthermore, remission of a psychiatric disorder should be delineated using Soft Independent Modelling of Class Analogy (SIMCA) and not by a threshold value applied to an unreliable scale[20]. Thus, a principal component model should be built around the healthy control class using causome, AOP and phenome features (excluding the unmodifiable features) and the apparent remitters should be projected into this SIMCA model and be authenticated as controls (that is, being allocated to the healthy class) or rejected as belonging to the control class[55]. Cases that cannot be authenticated as normal controls are non-remitters and, in the latter, the “relative improvement” should be assessed as an improvement in the modifiable AOPs, brainome, cognitome and phenome latent vector scores.
False dogmas 7: Existing diagnostic boundaries are too restrictive and spectra are the rule
The diagnosis of BD should be inclusive: Another problem is that the diagnosis of BD became more and more inclusive and that the diagnosis of MDD became more restricted[50]. As such, the classical prevalence rate of BD, which is around 0.5% to 1.5%, has increased and may even reach a rate as high as 10%[56]. It is debated whether a lack of well-defined MDD and BD case definitions leads to an overdiagnosis of MDD or BD to the detriment of BD or MDD[50]. The downside of over diagnosing BD is that patients with other conditions will be treated with mood stabilizers some of which have detrimental side effects on HR-QoL[57]. The downside of over diagnosing MDD to the detriment of BD is that those patients will be devoid of more targeted treatments with mood stabilizers. In fact, another pointless debate is that BD is frequently undiagnosed[57] or over diagnosed[59].
An even greater problem is the status of BP2. Some studies suggest that BP2 is a distinct category which should be separated from recurrent MDD and BP1 and this is based on proband studies[60]. Nevertheless, some studies suggest that the reliability coefficient of BP2 is not greater than that of chance, whereas other authors claim that a good interrater reliability may be obtained when BP2 is diagnosed by experienced psychiatrists[60]. Consequently, some authors have relaxed the case definitions of BP2 for example using new hypomania checklists which include subsyndromal hypomania or subthreshold bipolarity, which is considered to belong to the soft BP spectrum[61,62]. Consequently, these authors use this checklist, which shows a sensitivity of 80% to detect true bipolar patients and a specificity of 51% (computed vs MDD) to diagnose BD. Consequently, up to 79% of fibromyalgia patients suddenly belong to the bipolar spectrum using a diagnostic algorithm which is grossly inadequate[63].
BD subtypes shape a continuum: Some authors proposed the “bipolar spectrum” concept which considers that bipolarity occurs along a continuum from soft to clear forms of BD, thus contrasting the categorical view of the DSM[64]. As a result, the increased prevalence of BD may be explained by the detection of softer BD phenotypes such as BP-2, BP-3, rapid cyclers and cyclothymia[56]. The BP spectrum may also comprise MDD with hyperthymic traits, depressive mixed states with hypomanic symptoms including sexual arousal, ultrarapid-cycling forms, patients with lifelong temperamental dysregulation, and cyclic irritable-dysphoric, intermittently explosive or impulse-ridden clinical expression[56]. Even the status of agitated depression appears to have remained elusive, with some suggesting that this type of depression is a mixed state or, more accurately, “pseudo-unipolar”, and should be renamed “excited mixed depression”[65]. One can only speculate on the number of additional surreal labels that will be coined in the near future.
Mood disorders subtypes are part of a continuum: Another heavily debated issue is whether MDD and BP belong to a continuum (continuous theory) or whether they constitute distinct categories (discontinuous theory)[66,67]. Some authors claim that research consolidated the existence of a broad bipolar spectrum between the extremes of unipolar MDD and psychotic manic-depressive illness[68]. It is thought that the continuity spectrum between MDD and BD is supported by a number of findings including the presence of mixed states (both mania and depressive symptoms co-occur), no real separation between MDD and MDE in BD, and that many MDD patients may shift into BD. On the other hand, some findings would support the discontinuous theory, namely BP occurs more frequently in BP probands’ relatives and BD shows an equal sex distribution whereas MDD shows a higher frequency in females; and BP shows a more recurrent course than MDD[66,67]. Nevertheless, some results support the dimensional and categorical approach with the mood disorders extremes (severe MDD and BP1) showing a categorical distinction, and the moderate mood disorders (BP2 and MDD) showing continuous differences[67]. Nevertheless, these studies have no merit because the accurate machine learning tests were not used to examine the continuum vs discontinuum theories.
There are different depressive subtypes: Modern psychiatry generally considers that there are different MDD/MDE subtypes including atypical depression, melancholia, recurrent depressive disorder, dysthymia, bipolar depression, double depression, psychotic depression, seasonal affective disorder, depression with postpartum onset, perinatal depression, postpartum depression, prenatal depression, depression with catatonic features, chronic depression, persistent depressive disorder, geriatric depression, premenstrual dysphoric disorder and treatment resistant depression[1,69]. Some of these subtypes came and went including reactive depression, situational depression, vital depression, endogenous depression, endogenomorph depression, hidden depression, concealed depression, anxious depression and a mixed episode in BDs.
Nevertheless, because the reliability of their parent classes (MDD and MDE) is very low, we may speculate that those different classes have zero reliability. In addition, virtually none of these classes, except melancholia, has been validated using unsupervised and supervised machine learning techniques[70]. Using both supervised (SIMCA) and unsupervised (clustering and factor analysis) methods we were able to show that melancholia is at the same time a continuous and a discrete class[70]. Thus, along the continuum of severity of illness, some symptoms (namely the melancholic symptoms) become more severe and more prevalent and as, a consequence, may shape a distinct symptom profile, i.e., major depression with melancholic features. As such, qualitative distinctions may be the result of quantitative distinctions, implying that all debates over continuum or discontinuum theories are pointless.
There are differences between unipolar MDD vs bipolar MDE: Another pointless discussion is whether there are differences between unipolar MDD and bipolar MDE, and whether they are the same or different diseases[71]. As a result, “depression with and without mania might be understood as the same condition”, while “BD disorder” could be thought of as mania, with or without depression. Another point of view is that unipolar MDD and BD depression are separate illnesses that can coexist[71]. Biological dysregulation is a risk factor for both MDD and BD, although it appears to be more strongly linked to BD than unipolar MDD, implying that BD is linked to more excessive responses to psychosocial stresses than MDD[71]. From a biological standpoint, the IO&NS pathways in MDD, BP1 and BP2 differ significantly, with those pathways being more expressed in MDD and BP1 than in BP2 and more in MDD than in BP1[72]. In depression, cell-mediated immunity is activated as well, but not in mania or hypomania[73]. All the changes, however, are quantitative rather than qualitative and some studies found immune-inflammatory pathway differences between unipolar and bipolar depression[74], while others found no IO&NS differences between MDE in MDD and BD[75].
It is better to abolish all psychiatric diagnostic systems: Overall, the dimensional approach to the mood disorders spectrum idea, as well as the over diagnosing of BD with more inclusive diagnostic criteria, have blurred the lines between distinct diagnostic categories, lowering the diagnostic reliability of these mood disorders[75]. Given the above it is not surprising that the DSM and ICD taxonomies lack reliability, validity and therefore, are counterproductive for research purposes[6,77-79]. As a result, it is not unexpected that some authors came to the conclusion that all psychiatric diagnostic systems should be abolished[80].
Based on the NNP models we developed in our research, we believe it is best to eliminate all the above-mentioned mood disorders diagnostic classes and labels. To begin with, none of these classes has been designated as a separate category. Second, our NNP models show that none of the major classes MDD, BD, BP1, or BP2 are significant. For example, supervised methods like SIMCA were unable to validate these classes as distinct entities when applied to clinical and biomarker data in our data set (personal data). More importantly, two-step cluster analyses using all features of NNP1 and NNP2 as categorical variables revealed new trans-diagnostic clusters (see new classifications based on NNP features), which are more influential than the classification into MDD, BD, BP1 and BP2[10,12]. These negative findings on the MDD and BD classifications may be explained by the fact that: (1) They are binary concepts (present or not present); (2) They are top-down taxonomies based on unreliable clinical criteria and without external validation; and (3) The latent vector scores of causome, AOP, cognitome, ROI and phenome contain more accurate information on mood disorders than the binary diagnosis into MDD and BD.
Dogma 8: No need to ROI-define mood disorders: The DSM and ICD categorization systems have never placed a high value on course trajectory specifiers. Symptoms, symptom clusters and BD polarity, as well as a few course specifiers like rapid cycling, chronic depression and seasonal patterns, are used to classify DSM/ICD disorders. Interestingly, a recent project proposed to make a clinical course-graphing scale for DSM-5 disorders, namely the Timeline Course Graphing Scale for the DSM-5 Mood Disorders (TCGS)[81]. This new method takes a more systematic approach to graphing the course of mood disorders, allowing researchers to estimate the onset of mood disorders (early vs late onset) as well as the severity of the illness (chronicity, subthreshold syndrome, and so on). The TCGS’ major goal is to distinguish MDD from the new DSM-5 class Persistent Depression, because it was anticipated that failing to distinguish the two diseases could cause treatment efforts to fail[81]. Another way to prospectively study the alternating symptoms in BD is the NIMH Life Chart Method[82].
Nevertheless, the DSM/ICD categorization systems and the TCGS/NIMH proposals do not take into account the disease’s recurrence pattern, severity of recurrence, recurrence of suicidal behaviors, and recurrence-related worsening in cognitive functioning, HR-QoL life, and increased impairments[18]. Previously, some authors proposed staging models which included criteria considering functional and cognitive impairments[83-86]. However, these were theoretical models, whereas the ROI-index produced from the NNP model is calculated using predictive mathematical algorithms and real patient data. Furthermore, earlier theoretical models provided phase-related classifications of unipolar and bipolar patients, but we computed continuous ROI scores in the combined MDD and BD group and derived externally validated ROI phases by binning the ROI into three ROI groups[18]. This ROI, as discussed in NNP models, includes information on episode and suicide recurrence, as well as the binary classification of BD and MDD/MDE.
The ROI is a crucial component of the NNP models because it predicts the phenome of mood disorders and mediates the effects of the causome (interactions between the PON1 gene and ELT) on the phenome, as detailed in NNP models. Furthermore, ROI was found to be associated with not only the phenome[10], but also the severity of depressive and manic symptoms, current suicidal ideation, and cognitive impairments in semantic memory and executive functions, as well as socioeconomic status, treatment, and biomarkers such as lowered antioxidant defenses, increased nitro-oxidative stressors, insulin resistance, CRP and a variety of other biomarkers[19]. More crucially, the ROI index is influenced by the interactions between ELTs and PON1 enzymatic activity[10].
Most importantly, our ROI latent vector is unidimensional and fits a reflective model with adequate reliability validity and replicability and, therefore, the ROI (i.e., its organic substrate) is the cause of the reoccurrence of depressive episodes in MDD and depressive and manic episodes in BD and suicidal attempts in both MDD/BD as well. By inference, the reoccurrence of these phenomena is determined by a same underlying phenomenon which is partly determined by PON1 genotype and ELT interactions, and IO&NS pathways[10]. The ROI-index is not only strongly associated with PON1 gene x ELT interactions, but also with O&NS pathways indicating lipid and protein oxidation[18]. Moreover, a recent meta-analysis showed that there are strong associations between suicide attempts and ideation and IO&NS pathways with a high effect size[87]. There is also some evidence that sensitization of IO&NS pathways may underpin this reoccurrence[73].
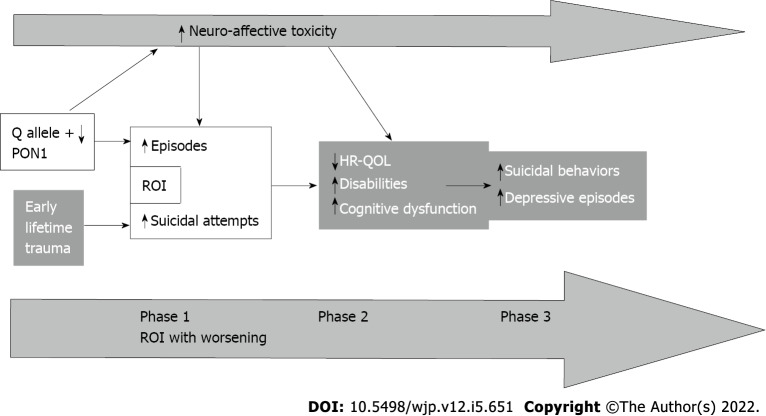
Through binning, we constructed three patient groups that reflect relevant phases of mood disorders, namely: “(1) An early phase; (2) A relapse-retrogression phase; and (3) A suicidal-retrogression phase”[18]. Table 1 shows that these phases are externally validated by clinical features. Figure 4 shows that the causal links from ELTs and PON1 genotype to ROI to phenome capture the lifetime trajectory of MDD/BD patients from childhood to an increasing number of episodes and suicidal behaviors to the progressive worsening of disease in terms of cognitive deficits, HR-QoL, and disabilities[18].
Table 1.
Characteristics of the three stages of affective disorders[18]
|
Stages
|
Phase 1: Early phase
|
Phase 2: Relapse-regression
|
Phase 3: Suicidal regression
|
| Early lifetime trauma | - | + | ++ |
| Number of depressive episodes | + | ++ | +++ |
| Number of (hypo)manic episodes | + | ++ | ++ |
| Number of suicidal attempts | + | + | +++ |
| A lifetime history suicidal ideation | + | + | ++ |
| Current suicidal ideation | + | + | +++ |
| Lower income | + | ++ | +++ |
| Disabilities | + | ++ | ++ |
| Reduced health-related quality of life | + | ++ | ++ |
| Reduced cognitive processing speed | + | ++ | ++ |
| Deficits in executive functioning | - | - | + |
Figure 4.
Causal links from early lifetime trauma and paraoxonase 1 genotype and enzymatic activity to reoccurrence of illness to phenome including health-related quality of life. ROI: Reoccurrence of illness; HR-QOL: Health-related quality of life; PON1: Paraoxonase 1.
Such findings indicate that MDD, BD, and recurrent episodes and suicidal attempts share a common substrate and that MDD and BD should be regarded as the same disorder, namely “DysMood disorder” whereby the causome, AOPs, and ROI shape a distinct class namely “Major DysMood Disorder due to neuro-affective toxicity”.
CONCLUSION
Psychosocial or mind-brain models have traditionally been used to explain mood disorders, but these models are inadequate because such models are not even falsifiable. The DSM/ICD criteria for mood disorders are narratives that have been stripped of their context and are therefore without any mechanistic explanation. The DSM/ICD classifications of mood disorders are not only unreliable but their dogma-like nature prevents inductive (as top-down) and deductive (as incontrovertible) remodeling of the case-definitions.
We built new bottom-up, data-driven, machine learning NNP models of mood disorders that reify all the components of mood disorders, as is the case in all medical disciplines where diagnosis offers a pathophysiological explanation. Neuro-affective toxicity causes functional and structural impairments in the brain, as shown by these NNP models and enrichment/annotation analysis. In mood disorders, the ROI index plays a critical role in mediating the effects of causome pathways on the phenome. The ROI index is also significantly linked to a progressive worsening of cognitive impairments, phenome severity, disabilities and HR-QoL. As a result, MDD and BD should be treated as if they were one and the same illness.
Our findings show that the causome, AOP and ROI features identified in our NNPs should be new drug targets for treating “Major DysMood Disorder”, rather than the binary diagnosis of BD or MDD. The new drug targets include: Reduced PON1 enzyme activity and its consequences, increased Gram-negative bacteria or LPS translocation, increased ELTs and their consequences, lowered levels of antioxidants and elevated reactive oxygen and nitrogen species, lipid peroxidation with higher levels of aldehydes, protein oxidation and formation of oxidative-specific epitopes, nitrosative stress and increased autoimmune responses to oxidative-specific epitopes. As discussed in NNP-associated pathways, these O&NS disorders are strongly linked to activated immune-inflammatory pathways and together they may cause functional and structural changes in the brain indicative of neuro-affective toxicity. It is important to note, as well, that PON1 activity and ELT-associated sensitization of IO&NS pathways are new drug targets, and that targeted treatments may help prevent further episodes and worsening of the disease, including progression into later phases with increased cognitive and functional deterioration, as well as suicide risk.
Footnotes
Conflict-of-interest statement: The authors have no conflict of interest with any commercial or other association in connection with the submitted article.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Peer-review started: July 11, 2021
First decision: October 4, 2021
Article in press: April 25, 2022
Specialty type: Psychiatry
Country/Territory of origin: Australia
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Kaur M, United States S-Editor: Wang JJ L-Editor: Filipodia P-Editor: Wang JJ
Contributor Information
Michael HJ Maes, Department of Psychiatry, Chulalongkorn University, Bangkok 10330, Thailand. dr.michaelmaes@hotmail.com.
Drozdstoy Stoyanov, Department of Psychiatry, Medical University Plovdiv, Plovdiv 4000, Bulgaria.
References
- 1.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (Fifth ed). Arlington, VA: American Psychiatric Publishing, 2013: 5-25. [Google Scholar]
- 2.World Health Organization. ICD-10: international statistical classification of diseases and related health problems: tenth revision, 2nd ed, 2004. [cited 11 June 2021]. Available from: https://apps.who.int/iris/handle/10665/42980 .
- 3.Crawford MJ, Hopkins W, Thomas P, Moncreiff J, Bindman J, Gray AJ. Most psychiatrists oppose plans for new mental health act. BMJ. 2001;322:866. [PMC free article] [PubMed] [Google Scholar]
- 4.Szasz TS. The Myth of Mental Illness: Foundations of a Theory of Personal Conduct. British: Secker & Warburg, 1961. [Google Scholar]
- 5.Benning TB. No such thing as mental illness? BJPsych Bull. 2016;40:292–295. doi: 10.1192/pb.bp.115.053249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Insel T, Cuthbert B, Garvey M, Heinssen R, Pine DS, Quinn K, Sanislow C, Wang P. Research domain criteria (RDoC): toward a new classification framework for research on mental disorders. Am J Psychiatry. 2010;167:748–751. doi: 10.1176/appi.ajp.2010.09091379. [DOI] [PubMed] [Google Scholar]
- 7.Cone JD. Idiographic, nomothetic, and related perspectives in behavioral assessment. In: Nelson RO, Hayes SC. Conceptual Foundations of Behavioral Assessment. New York: Guilford Press, 1986: 111-128. [Google Scholar]
- 8.Hurlburt RT, Knapp TJ. Münsterberg in 1898, Not Allport in 1937, Introduced the Terms ‘Iidiographic’ and ‘Nomothetic’ to American Psychology. Theory Psychol. 2006;16:287–293. [Google Scholar]
- 9.Haynes SN, O’Brien WH. Principles and Practice of Behavioral Assessment. In: Idiographic and Nomothetic Assessment. Boston: Springer, 2000: 109-126. [Google Scholar]
- 10.Maes M, Moraes JB, Bonifacio KL, Barbosa DS, Vargas HO, Michelin AP, Nunes SOV. Towards a new model and classification of mood disorders based on risk resilience, neuro-affective toxicity, staging, and phenome features using the nomothetic network psychiatry approach. Metab Brain Dis. 2021;36:509–521. doi: 10.1007/s11011-020-00656-6. [DOI] [PubMed] [Google Scholar]
- 11.Stoyanov D, Maes MH. How to construct neuroscience-informed psychiatric classification? World J Psychiatry. 2021;11:1–12. doi: 10.5498/wjp.v11.i1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Simeonova D, Stoyanov D, Leunis JC, Murdjeva M, Maes M. Construction of a nitro-oxidative stress-driven, mechanistic model of mood disorders: A nomothetic network approach. Nitric Oxide. 2021;106:45–54. doi: 10.1016/j.niox.2020.11.001. [DOI] [PubMed] [Google Scholar]
- 13.Maes M, Vojdani A, Galecki P, Kanchanatawan B. How to Construct a Bottom-Up Nomothetic Network Model and Disclose Novel Nosological Classes by Integrating Risk Resilience and Adverse Outcome Pathways with the Phenome of Schizophrenia. Brain Sci. 2020;10 doi: 10.3390/brainsci10090645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Wilhelm Windelband Präludien. Meiner: Philosophische BibliothekAs, 2021 . [Google Scholar]
- 15.Di Nicola V, Stoyanov D. Psychiatry in Crisis. In: Psychiatric Nosology Revisited: At the Crossroads of Psychology and Medicine. Cham: Springer, 2021: 31-41. [Google Scholar]
- 16.Stoyanov DS. The endophenotype project and the validation theory: integration of neurobiology and psychiatry. Folia Med (Plovdiv) 2010;52:18–25. [PubMed] [Google Scholar]
- 17.Stoyanov D, Fulford B, Stanghellini G, Van Staden W, Wong MT. International perspectives in values-based mental health practice: Case studies and commentaries. Switzerland: Springer Nature, 2021. [Google Scholar]
- 18.Maes M, Moraes JB, Congio A, Bonifacio KL, Barbosa DS, Vargas HO, Michelin AP, Carvalho AF, Nunes SOV. Development of a Novel Staging Model for Affective Disorders Using Partial Least Squares Bootstrapping: Effects of Lipid-Associated Antioxidant Defenses and Neuro-Oxidative Stress. Mol Neurobiol. 2019;56:6626–6644. doi: 10.1007/s12035-019-1552-z. [DOI] [PubMed] [Google Scholar]
- 19.Maes M, Congio A, Moraes JB, Bonifacio KL, Barbosa DS, Vargas HO, Morris G, Puri BK, Michelin AP, Nunes SOV. Early Life Trauma Predicts Affective Phenomenology and the Effects are Partly Mediated by Staging Coupled with Lowered Lipid-Associated Antioxidant Defences. Biomol Concepts. 2018;9:115–130. doi: 10.1515/bmc-2018-0010. [DOI] [PubMed] [Google Scholar]
- 20.Maes M, Anderson G. False Dogmas in Schizophrenia Research: Toward the Reification of Pathway Phenotypes and Pathway Classes. Front Psychiatry. 2021;12:663985. doi: 10.3389/fpsyt.2021.663985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Popper K. On the Structure of Scientific Revolution. Chicago: Chicago University Press, 1962. [Google Scholar]
- 22.Maes M, Carvalho AF. The Compensatory Immune-Regulatory Reflex System (CIRS) in Depression and Bipolar Disorder. Mol Neurobiol. 2018;55:8885–8903. doi: 10.1007/s12035-018-1016-x. [DOI] [PubMed] [Google Scholar]
- 23.Maes M, Lambrechts J, Bosmans E, Jacobs J, Suy E, Vandervorst C, de Jonckheere C, Minner B, Raus J. Evidence for a systemic immune activation during depression: results of leukocyte enumeration by flow cytometry in conjunction with monoclonal antibody staining. Psychol Med. 1992;22:45–53. doi: 10.1017/s0033291700032712. [DOI] [PubMed] [Google Scholar]
- 24.Maes M, Bosmans E, Suy E, Vandervorst C, De Jonckheere C, Raus J. Immune disturbances during major depression: upregulated expression of interleukin-2 receptors. Neuropsychobiology. 24:115–120. doi: 10.1159/000119472. [DOI] [PubMed] [Google Scholar]
- 25.Leonard B, Maes M. Mechanistic explanations how cell-mediated immune activation, inflammation and oxidative and nitrosative stress pathways and their sequels and concomitants play a role in the pathophysiology of unipolar depression. Neurosci Biobehav Rev. 2012;36:764–785. doi: 10.1016/j.neubiorev.2011.12.005. [DOI] [PubMed] [Google Scholar]
- 26.Kandilarova S, Stoyanov D, Sirakov N, Maes M, Specht K. Reduced grey matter volume in frontal and temporal areas in depression: contributions from voxel-based morphometry study. Acta Neuropsychiatr. 2019;31:252–257. doi: 10.1017/neu.2019.20. [DOI] [PubMed] [Google Scholar]
- 27.Helen I. Is depression a brain disorder? Neuroscience in mental health care. In: Pickersgill M, van Keulen I. Sociological Reflections on the Neurosciences (Advances in Medical Sociology, Vol 13). Bingley: Emerald Group Publishing Limited, 2011: 123-152. [Google Scholar]
- 28.Harvard Health Publishing. What causes depression? [cited 10 January 2022]. Available from: https://www.health.harvard.edu/mind-and-mood/what-causes-depression .
- 29.Kendler KS. Toward a philosophical structure for psychiatry. Am J Psychiatry. 2005;162:433–440. doi: 10.1176/appi.ajp.162.3.433. [DOI] [PubMed] [Google Scholar]
- 30.Rudzki L, Maes M. From "Leaky Gut" to Impaired Glia-Neuron Communication in Depression. Adv Exp Med Biol. 2021;1305:129–155. doi: 10.1007/978-981-33-6044-0_9. [DOI] [PubMed] [Google Scholar]
- 31.Maes M, Kubera M, Obuchowiczwa E, Goehler L, Brzeszcz J. Depression's multiple comorbidities explained by (neuro)inflammatory and oxidative & nitrosative stress pathways. Neuro Endocrinol Lett. 2011;32:7–24. [PubMed] [Google Scholar]
- 32.Kallaur AP, Lopes J, Oliveira SR, Simão AN, Reiche EM, de Almeida ER, Morimoto HK, de Pereira WL, Alfieri DF, Borelli SD, Kaimen-Maciel DR, Maes M. Immune-Inflammatory and Oxidative and Nitrosative Stress Biomarkers of Depression Symptoms in Subjects with Multiple Sclerosis: Increased Peripheral Inflammation but Less Acute Neuroinflammation. Mol Neurobiol. 2016;53:5191–5202. doi: 10.1007/s12035-015-9443-4. [DOI] [PubMed] [Google Scholar]
- 33.Jaroonpipatkul C, Onwanna J, Tunvirachaisakul C, Jittapiromsak N, Rakvongthai Y, Chutinet A, Maes M. Depressive symptoms due to stroke are strongly predicted by the volume and location of the cerebral infarction, white matter hyperintensities, hypertension, and age: a precision nomothetic psychiatry analysis. 2021. [DOI] [PubMed] [Google Scholar]
- 34.Lehmann ALCF, Alfieri DF, de Araújo MCM, Trevisani ER, Nagao MR, Pesente FS, Gelinski JR, de Freitas LB, Flauzino T, Lehmann MF, Lozovoy MAB, Breganó JW, Simão ANC, Maes M, Reiche EMV. Immune-inflammatory, coagulation, adhesion, and imaging biomarkers combined in machine learning models improve the prediction of death 1 year after ischemic stroke. Clin Exp Med. 2022;22:111–123. doi: 10.1007/s10238-021-00732-w. [DOI] [PubMed] [Google Scholar]
- 35.Wardlaw JM, Chappell FM, Valdés Hernández MDC, Makin SDJ, Staals J, Shuler K, Thrippleton MJ, Armitage PA, Muñoz-Maniega S, Heye AK, Sakka E, Dennis MS. White matter hyperintensity reduction and outcomes after minor stroke. Neurology. 2017;89:1003–1010. doi: 10.1212/WNL.0000000000004328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Jin R, Yang G, Li G. Inflammatory mechanisms in ischemic stroke: role of inflammatory cells. J Leukoc Biol. 2010;87:779–789. doi: 10.1189/jlb.1109766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Almulla AF, Al-Rawi KF, Maes M, Al-Hakeim HK. In schizophrenia, immune-inflammatory pathways are strongly associated with depressive and anxiety symptoms, which are part of a latent trait which comprises neurocognitive impairments and schizophrenia symptoms. J Affect Disord. 2021;287:316–326. doi: 10.1016/j.jad.2021.03.062. [DOI] [PubMed] [Google Scholar]
- 38.Kanchanatawan B, Thika S, Sirivichayakul S, Carvalho AF, Geffard M, Maes M. In Schizophrenia, Depression, Anxiety, and Physiosomatic Symptoms Are Strongly Related to Psychotic Symptoms and Excitation, Impairments in Episodic Memory, and Increased Production of Neurotoxic Tryptophan Catabolites: a Multivariate and Machine Learning Study. Neurotox Res. 2018;33:641–655. doi: 10.1007/s12640-018-9868-4. [DOI] [PubMed] [Google Scholar]
- 39.de Araújo Filho GM, Martins DP, Lopes AM, de Jesus Brait B, Furlan AER, Oliveira CIF, Marques LHN, Souza DRS, de Almeida EA. Oxidative stress in patients with refractory temporal lobe epilepsy and mesial temporal sclerosis: Possible association with major depressive disorder? Epilepsy Behav. 2018;80:191–196. doi: 10.1016/j.yebeh.2017.12.025. [DOI] [PubMed] [Google Scholar]
- 40.Michelin AP, Maes MHJ, Supasitthumrong T, Limotai C, Matsumoto AK, de Oliveira Semeão L, de Lima Pedrão JV, Moreira EG, Kanchanatawan B, Barbosa DS. Reduced paraoxonase 1 activities may explain the comorbidities between temporal lobe epilepsy and depression, anxiety and psychosis. World J Psychiatry. 2022;12:308–322. doi: 10.5498/wjp.v12.i2.308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lindqvist D, Hall S, Surova Y, Nielsen HM, Janelidze S, Brundin L, Hansson O. Cerebrospinal fluid inflammatory markers in Parkinson's disease--associations with depression, fatigue, and cognitive impairment. Brain Behav Immun. 2013;33:183–189. doi: 10.1016/j.bbi.2013.07.007. [DOI] [PubMed] [Google Scholar]
- 42.Peveler R, Carson A, Rodin G. Depression in medical patients. BMJ. 2002;325:149–152. doi: 10.1136/bmj.325.7356.149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hashioka S, Inoue K, Miyaoka T, Hayashida M, Wake R, Oh-Nishi A, Inagaki M. The Possible Causal Link of Periodontitis to Neuropsychiatric Disorders: More Than Psychosocial Mechanisms. Int J Mol Sci. 2019;20 doi: 10.3390/ijms20153723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Mousa RF, Smesam HN, Qazmooz HA, Al-Hakeim HK, Maes M. A pathway phenotype linking metabolic, immune, oxidative, and opioid pathways with comorbid depression, atherosclerosis, and unstable angina. CNS Spectr. 2021:1–15. doi: 10.1017/S1092852921000432. [DOI] [PubMed] [Google Scholar]
- 45.Al-Hakeim HK, Najm AH, Moustafa SR, Maes M. Construction of an exposure-pathway-phenotype in children with depression due to transfusion-dependent thalassemia: Results of (un)supervised machine learning. J Affect Disord. 2021;282:644–655. doi: 10.1016/j.jad.2020.12.089. [DOI] [PubMed] [Google Scholar]
- 46.Al-Hakeim HK, Hadi HH, Jawad GA, Maes M. Intersections between Copper, β-Arrestin-1, Calcium, FBXW7, CD17, Insulin Resistance and Atherogenicity Mediate Depression and Anxiety Due to Type 2 Diabetes Mellitus: A Nomothetic Network Approach. J Pers Med. 2022;12 doi: 10.3390/jpm12010023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Al-Jassas HK, Al-Hakeim HK, Maes M. Intersections between pneumonia, lowered oxygen saturation percentage and immune activation mediate depression, anxiety, and chronic fatigue syndrome-like symptoms due to COVID-19: A nomothetic network approach. J Affect Disord. 2022;297:233–245. doi: 10.1016/j.jad.2021.10.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Regier DA, Kuhl EA, Kupfer DJ. The DSM-5: Classification and criteria changes. World Psychiatry. 2013;12:92–98. doi: 10.1002/wps.20050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Lieblich SM, Castle DJ, Pantelis C, Hopwood M, Young AH, Everall IP. High heterogeneity and low reliability in the diagnosis of major depression will impair the development of new drugs. BJPsych Open. 2015;1:e5–e7. doi: 10.1192/bjpo.bp.115.000786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Ghouse AA, Sanches M, Zunta-Soares G, Swann AC, Soares JC. Overdiagnosis of bipolar disorder: a critical analysis of the literature. ScientificWorldJournal. 2013;2013:297087. doi: 10.1155/2013/297087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.National Depressive and Manic-depressive Association. Living with bipolar Disorder: how far have we really come? [cited 6 January 2022]. Available from: https://secure2.convio.net/dabsa/pdfs/bphowfar1.pdf .
- 52.HAMILTON M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Fried EI, van Borkulo CD, Epskamp S, Schoevers RA, Tuerlinckx F, Borsboom D. Measuring depression over time . . . Or not? Psychol Assess. 2016;28:1354–1367. doi: 10.1037/pas0000275. [DOI] [PubMed] [Google Scholar]
- 54.Almulla AF, Al-Hakeim HK, Maes M. Schizophrenia phenomenology revisited: positive and negative symptoms are strongly related reflective manifestations of an underlying single trait indicating overall severity of schizophrenia. CNS Spectr. 2021;26:368–377. doi: 10.1017/S1092852920001182. [DOI] [PubMed] [Google Scholar]
- 55.Al-Hakeim HK, Mousa RF, Al-Dujaili AH, Maes M. In schizophrenia, non-remitters and partial remitters to treatment with antipsychotics are qualitatively distinct classes with respect to neurocognitive deficits and neuro-immune biomarkers: results of soft independent modeling of class analogy. Metab Brain Dis. 2021;36:939–955. doi: 10.1007/s11011-021-00685-9. [DOI] [PubMed] [Google Scholar]
- 56.Merikangas KR, Akiskal HS, Angst J, Greenberg PE, Hirschfeld RM, Petukhova M, Kessler RC. Lifetime and 12-month prevalence of bipolar spectrum disorder in the National Comorbidity Survey replication. Arch Gen Psychiatry. 2007;64:543–552. doi: 10.1001/archpsyc.64.5.543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Nunes CS, Maes M, Roomruangwong C, Moraes JB, Bonifacio KL, Vargas HO, Barbosa DS, Anderson G, de Melo LGP, Drozdstoj S, Moreira E, Carvalho AF, Nunes SOV. Lowered quality of life in mood disorders is associated with increased neuro-oxidative stress and basal thyroid-stimulating hormone levels and use of anticonvulsant mood stabilizers. J Eval Clin Pract. 2018;24:869–878. doi: 10.1111/jep.12918. [DOI] [PubMed] [Google Scholar]
- 58.Smith DJ, Ghaemi N. Is underdiagnosis the main pitfall when diagnosing bipolar disorder? BMJ. 2010;340:c854. doi: 10.1136/bmj.c854. [DOI] [PubMed] [Google Scholar]
- 59.Zimmerman M. Would broadening the diagnostic criteria for bipolar disorder do more harm than good? J Clin Psychiatry. 2012;73:437–443. doi: 10.4088/JCP.11com07288. [DOI] [PubMed] [Google Scholar]
- 60.Simpson SG, McMahon FJ, McInnis MG, MacKinnon DF, Edwin D, Folstein SE, DePaulo JR. Diagnostic reliability of bipolar II disorder. Arch Gen Psychiatry. 2002;59:736–740. doi: 10.1001/archpsyc.59.8.736. [DOI] [PubMed] [Google Scholar]
- 61.Angst J. ["Up and down". Bipolar illnesses--underestimated prevalence and complexity] Krankenpfl J. 2003;41:224. [PubMed] [Google Scholar]
- 62.Rybakowski JK, Angst J, Dudek D, Pawlowski T, Lojko D, Siwek M, Kiejna A. Polish version of the Hypomania Checklist (HCL-32) scale: the results in treatment-resistant depression. Eur Arch Psychiatry Clin Neurosci. 2010;260:139–144. doi: 10.1007/s00406-009-0030-4. [DOI] [PubMed] [Google Scholar]
- 63.Alciati A, Sarzi-Puttini P, Batticciotto A, Torta R, Gesuele F, Atzeni F, Angst J. Overactive lifestyle in patients with fibromyalgia as a core feature of bipolar spectrum disorder. Clin Exp Rheumatol. 2012;30:122–128. [PubMed] [Google Scholar]
- 64.Berk M, Berk L, Moss K, Dodd S, Malhi GS. Diagnosing bipolar disorder: how can we do it better? Med J Aust. 2006;184:459–462. doi: 10.5694/j.1326-5377.2006.tb00319.x. [DOI] [PubMed] [Google Scholar]
- 65.Kim W, Kim H, Citrome L, Akiskal HS, Goffin KC, Miller S, Holtzman JN, Hooshmand F, Wang PW, Hill SJ, Ketter TA. More inclusive bipolar mixed depression definitions by requiring fewer non-overlapping mood elevation symptoms. Acta Psychiatr Scand. 2016;134:189–198. doi: 10.1111/acps.12563. [DOI] [PubMed] [Google Scholar]
- 66.Benazzi F. The relationship of major depressive disorder to bipolar disorder: continuous or discontinuous? Curr Psychiatry Rep. 2005;7:462–470. doi: 10.1007/s11920-005-0068-6. [DOI] [PubMed] [Google Scholar]
- 67.Benazzi F. Is there a continuity between bipolar and depressive disorders? Psychother Psychosom. 2007;76:70–76. doi: 10.1159/000097965. [DOI] [PubMed] [Google Scholar]
- 68.Akiskal HS. The prevalent clinical spectrum of bipolar disorders: beyond DSM-IV. J Clin Psychopharmacol. 1996;16:4S–14S. doi: 10.1097/00004714-199604001-00002. [DOI] [PubMed] [Google Scholar]
- 69.Hegerl U, Wittmann M, Pfeiffer-Gerschel T. “European Alliance against Depression (EAAD)” - Europaweites Interventionsprogramm gegen Depression und Suizidalität. Psychoneuro. 2004;30:677–679. [Google Scholar]
- 70.Maes M, Schotte C, Maes L, Cosyns P. Clinical subtypes of unipolar depression: Part II. Quantitative and qualitative clinical differences between the vital and nonvital depression groups. Psychiatry Res. 1990;34:43–57. doi: 10.1016/0165-1781(90)90057-c. [DOI] [PubMed] [Google Scholar]
- 71.Cuellar AK, Johnson SL, Winters R. Distinctions between bipolar and unipolar depression. Clin Psychol Rev. 2005;25:307–339. doi: 10.1016/j.cpr.2004.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Katrenčíková B, Vaváková M, Paduchová Z, Nagyová Z, Garaiova I, Muchová J, Ďuračková Z, Trebatická J. Oxidative Stress Markers and Antioxidant Enzymes in Children and Adolescents with Depressive Disorder and Impact of Omega-3 Fatty Acids in Randomised Clinical Trial. Antioxidants (Basel) 2021;10 doi: 10.3390/antiox10081256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Nobis A, Zalewski D, Waszkiewicz N. Peripheral Markers of Depression. J Clin Med. 2020;9 doi: 10.3390/jcm9123793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Martinuzzi E, Barbosa S, Courtet P, Olié E, Guillaume S, Ibrahim EC, Daoudlarian D, Davidovic L, Glaichenhaus N, Belzeaux R. Blood cytokines differentiate bipolar disorder and major depressive disorder during a major depressive episode: Initial discovery and independent sample replication. Brain Behav Immun Health. 2021;13:100232. doi: 10.1016/j.bbih.2021.100232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Sowa-Kućma M, Styczeń K, Siwek M, Misztak P, Nowak RJ, Dudek D, Rybakowski JK, Nowak G, Maes M. Are there differences in lipid peroxidation and immune biomarkers between major depression and bipolar disorder: Effects of melancholia, atypical depression, severity of illness, episode number, suicidal ideation and prior suicide attempts. Prog Neuropsychopharmacol Biol Psychiatry. 2018;81:372–383. doi: 10.1016/j.pnpbp.2017.08.024. [DOI] [PubMed] [Google Scholar]
- 76.Phelps J, Angst J, Katzow J, Sadler J. Validity and utility of bipolar spectrum models. Bipolar Disord. 2008;10:179–193. doi: 10.1111/j.1399-5618.2007.00562.x. [DOI] [PubMed] [Google Scholar]
- 77.Stoyanov D. The Reification of Diagnosis in Psychiatry. Neurotox Res. 2020;37:772–774. doi: 10.1007/s12640-019-00139-2. [DOI] [PubMed] [Google Scholar]
- 78.Hyman SE. The diagnosis of mental disorders: the problem of reification. Annu Rev Clin Psychol. 2010;6:155–179. doi: 10.1146/annurev.clinpsy.3.022806.091532. [DOI] [PubMed] [Google Scholar]
- 79.Hyman SE. Diagnosing the DSM: Diagnostic Classification Needs Fundamental Reform. Cerebrum. 2011;2011:6. [PMC free article] [PubMed] [Google Scholar]
- 80.Timimi A. No more psychiatric labels: Why formal psychiatric diagnostic systems should be abolished. Int J Clin Health Psychol. 2014;14:208–215. [Google Scholar]
- 81.Mccullough JP Jr, Clark SW, Klein DN, First MB. Introducing a Clinical Course-Graphing Scale for DSM-5 Mood Disorders. Am J Psychother. 2016;70:383–392. doi: 10.1176/appi.psychotherapy.2016.70.4.383. [DOI] [PubMed] [Google Scholar]
- 82.Denicoff KD, Ali SO, Sollinger AB, Smith-Jackson EE, Leverich GS, Post RM. Utility of the daily prospective National Institute of Mental Health Life-Chart Method (NIMH-LCM-p) ratings in clinical trials of bipolar disorder. Depress Anxiety. 2002;15:1–9. doi: 10.1002/da.1078. [DOI] [PubMed] [Google Scholar]
- 83.Berk M, Brnabic A, Dodd S, Kelin K, Tohen M, Malhi GS, Berk L, Conus P, McGorry PD. Does stage of illness impact treatment response in bipolar disorder? Bipolar Disord. 2011;13:87–98. doi: 10.1111/j.1399-5618.2011.00889.x. [DOI] [PubMed] [Google Scholar]
- 84.Scott J, Leboyer M, Hickie I, Berk M, Kapczinski F, Frank E, Kupfer D, McGorry P. Clinical staging in psychiatry: a cross-cutting model of diagnosis with heuristic and practical value. Br J Psychiatry. 2013;202:243–245. doi: 10.1192/bjp.bp.112.110858. [DOI] [PubMed] [Google Scholar]
- 85.Kapczinski F, Dias VV, Kauer-Sant'Anna M, Brietzke E, Vázquez GH, Vieta E, Berk M. The potential use of biomarkers as an adjunctive tool for staging bipolar disorder. Prog Neuropsychopharmacol Biol Psychiatry. 2009;33:1366–1371. doi: 10.1016/j.pnpbp.2009.07.027. [DOI] [PubMed] [Google Scholar]
- 86.Ferensztajn E, Remlinger-Molenda A, Rybakowski J. [Staging of unipolar affective illness] Psychiatr Pol. 2014;48:1127–1141. doi: 10.12740/PP/24239. [DOI] [PubMed] [Google Scholar]
- 87.Vasupanrajit A, Jirakran K, Tunvirachaisakul C, Solmi M, Maes M. Inflammation and nitro-oxidative stress in current suicidal attempts and current suicidal ideation: a systematic review and meta-analysis. Mol Psychiatry. 2022 doi: 10.1038/s41380-021-01407-4. [DOI] [PubMed] [Google Scholar]