Abstract
Background and Objectives
Dementia awareness initiatives aim to promote helping behaviors toward people living with dementia. We applied the bystander intervention process model in the context of the general public’s helping behaviors toward people living with dementia, and we sought to identify the mechanisms underlying the association between dementia knowledge and helping behaviors.
Research Design and Methods
In a survey featuring vignettes for the general public in Japan (N = 904), we presented four situations in which people could exhibit helping behaviors toward a person with dementia. Guttman scale analysis was used to test this sequential ordering of the bystander intervention process model: (a) interpreting the need to help, (b) perceiving personal responsibility, and (c) intention to provide help. Mediation analysis was used to examine whether the effects of knowledge on helping behaviors were mediated by attitude toward people living with dementia and the bystander intervention process.
Results
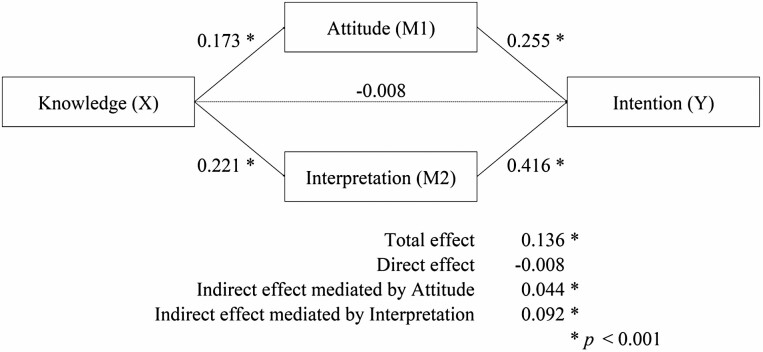
The results support the two-step model in which interpreting the situation as one where assistance is required is a prerequisite of helping behavior. Dementia knowledge had a significant total effect on intention to provide help (β = 0.136, p < .001). Interpretation (indirect effect: β = 0.092, p < .001), as well as attitude (indirect effect: β = 0.044, p < .001), was found to completely mediate the effect of dementia knowledge on intention to provide help.
Discussion and Implications
Dementia awareness initiatives designed to promote helping behaviors should focus on knowledge transfer, improving the general public’s attitudes toward people living with dementia, and their ability to interpret when such people need assistance.
Keywords: Behavioral and psychological symptoms of dementia (BPSD), Community care, Dementia, Education, Social support
Translational Significance: It remains unclear how helping behaviors toward people with dementia are triggered among the public. The process and mechanism were examined in this study. The results of this study suggest that knowledge of dementia promotes intention of helping behavior, mediated by interpretation of the need for help and positive attitudes toward people with dementia. It is recommended that dementia education programs focus on providing knowledge about the early symptoms of dementia and changing attitudes toward people with dementia.
It is estimated that there are over 43 million people living with dementia worldwide, and this figure is expected to increase in the future (GBD 2016 Disease and Injury Incidence and Prevalence Collaborators, 2019). As a result of the prevalence of this condition, many dementia-friendly initiatives are being pursued globally to promote the social inclusion of people living with dementia (Shannon & Bail, 2018). Challenging the stigma of negative societal perceptions of dementia is central to such dementia-friendly initiatives (Hebert & Scales, 2019), and creating dementia-friendly communities can help people living with dementia maximize the length of time they can live in their own communities and continue to engage in normal daily life (Alzheimer Disease International, 2016). Thus, dementia-friendly initiatives for the general public, as well as for health-care providers, are now widely encouraged (Alzheimer’s Disease Internatinal & World Health Organization, 2015).
The awareness-raising aspect of dementia-friendly initiatives is based on the premise that improving the public’s dementia literacy and reducing associated stigma will promote helping behaviors toward people living with dementia (Lane & Yu, 2020; Maki et al., 2020; Ministry of Health Labour and Welfare, 2015). In Japan, since 2005, over 12 million people, representing 10% of the country’s population, have participated in a standardized dementia-friendly initiative called “Dementia Supporters” (Community Care Policy Network, 2020). The initiative aims to increase public awareness and understanding of dementia, and to translate that understanding into “supportive social actions” (Hayashi, 2017; Maki et al., 2020). The videos that are frequently used in this initiative provide examples of some actions, such as neighbors helping a person living with dementia traveling in the wrong direction to get home and a convenience store clerk helping a person living with dementia calculate her payment (Community Care Policy Network, 2022). Similar efforts have been made in the United Kingdom and other countries through initiatives such as “Dementia Friends” (Alzheimer’s Society, 2020).
Previous research has shown that awareness-raising approaches such as Dementia Supporters and Dementia Friends improve not only the public’s knowledge of dementia but also the public’s attitudes toward people living with dementia (Cowan, 2021; Matsuda et al., 2018). As the educational interventions inherent in dementia-friendly initiatives further aim to promote helping behaviors toward people living with dementia, it is necessary to examine whether knowledge and attitudes lead to helping behavior. In this regard, previous studies have revealed that knowledge of dementia is associated with intentions and motivations to perform helping behaviors, and that this association is partially mediated by attitudes toward dementia. For example, based on the theory of planned behavior (Ajzen, 1991), Lane and Yu (2020) reported that dementia knowledge is significantly associated with intentions to perform helping behaviors, and that this association is partially mediated by person-centered attitudes. Additionally, Takao and Maki (2019) reported that self-assessed knowledge of dementia has both a direct and indirect effect on motivation to participate in dementia prevention and support activities, mediated by positive attitudes toward people living with dementia. In both studies, however, attitudes toward people living with dementia do not completely mediate the effects of knowledge on helping behavior, and the mediating factors, other than attitudes, remain unknown. Identifying other mediating mechanisms will help to justify and improve dementia education.
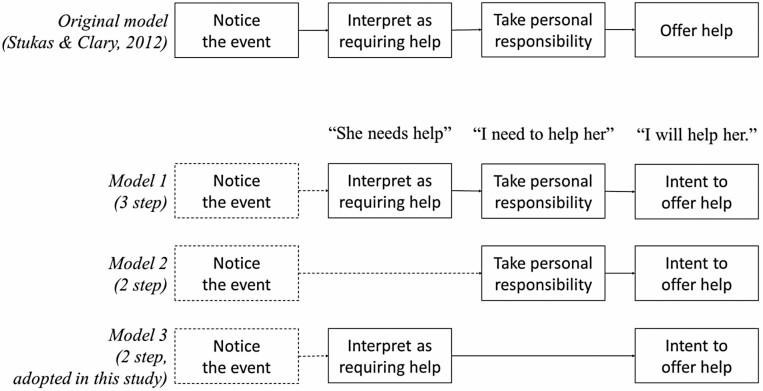
The bystander effect theory may represent another mediating mechanism underlying the effect of dementia knowledge on performance of helping behaviors. The bystander effect theory, first presented in Latané and Darley’s (1970) famous social psychology study, was used to develop a bystander intervention process model, concerning helping behaviors, to explain bystanders’ interventions during assault incidents. This bystander intervention process model has previously been applied in the contexts of financial elder abuse (Gilhooly et al., 2016), drunk-driving cessation (Rabow et al., 1990), organ donation, and green living (Anker & Feeley, 2011). Stukas and Clary (2012) proposed a three-step bystander intervention process model: (a) noticing the event, (b) interpreting the situation as one in which assistance is required, and (c) taking personal responsibility to help (Figure 1, top). This model affords a focus on “interpretation of need” (i.e., determining whether assistance is required), an element that cannot be fully considered through the theory of planned behavior. Greater knowledge of dementia helps people identify the early symptoms of dementia (interpreting the situation) and early help-seeking behaviors (Perry-Young et al., 2018; Rimmer et al., 2005; Werner, 2003) and knowledge about the situation were significantly associated with bystander interventions (Banyard, 2008); thus, it can be hypothesized that knowledge about dementia also helps people recognize the symptoms of those living with dementia (interpreting the situation) and intervene when such people require help.
Figure 1.
The bystander intervention process model in the context of helping behaviors.
According to previous literature, awareness-raising approaches, which educate people about dementia, can increase the likelihood that an individual will perform helping behaviors in two pathways: people would have more positive attitudes toward those living with dementia and a better ability to interpret signs that they may require help. However, to the best of our knowledge, no previous studies have applied the bystander intervention process model in the context of helping people living with dementia. Identifying the applicability of the model to helping behavior for people living with dementia will allow us to examine, in more detail, the mechanisms of dementia awareness programs’ impact on helping behavior.
The aim of this study is (a) to apply the three-step bystander intervention process model to helping behaviors for people living with dementia and (b) to identify mediating mechanisms in the effect of dementia knowledge on performing helping behaviors. The hypotheses of the present study were (a) the bystander intervention process model is a good fit in the context of helping behaviors toward people living with dementia and (b) knowledge of dementia increases the probability of performing helping behaviors via the dementia attitudes and bystander intervention processes (namely, “interpreting the needs to intervene” and “personal responsibility”), parallelly. This study provides an empirical basis for the awareness-raising approaches applied in dementia-friendly initiatives, and applications of the findings can contribute to improving the level of community engagement of people living with dementia.
Method
Sample
We examined our hypotheses using data obtained from an online survey that was conducted in July 2020. The survey participants were recruited from the registered members of an internet research company (Rakuten Research); all participants were aged 15–69 years, and were distributed across nine cities in the Tokyo metropolis. A quota-sampling method based on 11 participants for each stratum of city (nine cities), age (six age groups: 10–19, 20–29, 30–39, 40–49, 50–59, and 60–69 years old), and gender (two strata). If a stratum contained fewer than 11 participants, we supplemented this with participants from an adjacent age group; in particular, there was a limited number of registered members aged 15–19 years, meaning only 10 participants were recruited from this age group. Finally, 1,000 participants were recruited; of these, any health or social care workers were excluded. Survey responses were voluntary, and respondents were given rewards by the survey company. Participants under 18 years of age registered with their parents’ consent. All data were anonymous, and informed consent was obtained on the internet survey system. The present study was approved by the Research Ethics Committee of the Graduate School of Medicine, The University of Tokyo (#2019206NI).
Measurements
Helping behaviors
Because people rarely help those living with dementia, we measured the intention to perform helping behaviors, as in previous studies (Lane & Yu, 2020; Takao & Maki, 2019). Intention of helping behaviors was measured using the following four vignettes, which described situations in which people living with dementia may need help:
Vignette A
One day, in the middle of summer, you are walking in the neighborhood and see an older woman wearing a heavy coat. She does not appear to be feeling hot, and you do not know the woman. The streets are sparsely populated, but you do not see anyone who seems to be worried about the older woman. You are in no hurry.
Vignette B
You are a clerk in a supermarket. An older woman, a regular customer, arrived this morning to buy two bunches of bananas; however, it is now evening, and she has returned to buy two more bunches of bananas. She also visited the supermarket twice yesterday and bought bananas. She is appropriately dressed.
Vignette C
As you are walking in your neighborhood, you see an older woman wandering the area; she appears anxious and is looking around her. The woman’s face is not familiar, and she is appropriately dressed. You are in no hurry.
Vignette D
You are shopping at the grocery store when you notice an older woman put a large number of fried side dishes into her shopping basket. You have never spoken to the woman before, but you know that she lives alone in your neighborhood. She is appropriately dressed, and you are in no hurry.
These four vignettes were developed based on interviews with family caregivers of persons living with dementia, the simulation-training materials developed by Igarashi et al. (2020), and discussions with nursing/public health researchers. Participants read each vignette and, for each, responded either “agree” or “disagree” to the following questions: (a) “She needs help”; (b) “I need to help her”; and (c) “I will help her.” Questions (a) and (b), respectively, corresponded to the elements “interpreting the situation as one in which assistance is required” and “taking personal responsibility” of the three-step bystander intervention process model (Stukas & Clary, 2012). These items are equivalent to those in the existing literature, such as Rabow et al. (1990), which measured interpretation and personal responsibility regarding actual helping behavior. Because our survey cannot measure actual behavior, we added question (c) to measure helping behavior intention instead. The “noticing the event” element of the bystander intervention process model was excluded from this survey because the respondents had already noticed the situation when reading the vignette. The interpretability of the vignettes and questions were examined through a preliminary survey that was conducted using an internet crowdsourcing service (n = 50) and a convenience sample (n = 7), and modifications were made based on the results obtained. The major modifications were to change the question “I want to help her” to “I will help her” and the answer “yes/no” to “agree/disagree” to make it easier to understand.
Knowledge and attitude
Knowledge of dementia was measured using a scale developed and validated by Mikami et al. (2017).
This scale comprises 10 statements; for example: “dementia is mainly managed through inpatient treatment,” “some forms of dementia are associated with shivering and stiffness of the limbs,” and “appropriate interaction with people living with dementia can relieve the symptoms of dementia.” In our study, the participants responded to each question with “yes” or “no” and, for each participant, the number of correct answers was summed (range: 1–10). Higher scores indicated greater knowledge. The Cronbach’s α for our sample was .50.
Attitude toward dementia was measured using a scale developed and validated by Kim and Kuroda (2011). This scale includes 14 statements: “I would have no problem if a person living with dementia moved in next door to my house,” “I can talk to a person living with dementia without hesitation,” and “it would be difficult to socialize with my neighbors if one of my family members developed dementia.” Participants provided answers using a 4-point Likert scale (4 = agree; 1 = disagree; range: 14–56). Seven of the 14 items were reverse-scored, and higher scores indicated more positive attitudes. Cronbach’s α for our sample was .81.
Covariates
The following covariates were controlled in the mediation analysis: age (year), gender (male = 1; female = 0), education (graduation from junior high school = 1, graduation from high school = 2, graduation from junior or career college = 3, graduation from university = 4, graduation from graduate school = 5), family experience of dementia (yes = 1; no = 0), and experience of caring for a family member living with dementia (yes = 1; no = 0). Age and education were used as interval variables. A previous systematic review of the general public’s dementia knowledge found that age, gender, education, and ethnicity are common major correlates of dementia knowledge (Cahill et al., 2015). Of these, ethnicity was not included among the covariates in the present study because Japan has a relatively low degree of ethnic diversity (Ministry of Justice, 2019). In addition, Takao and Maki (2019) showed that nursing care experience and contact with a person living with dementia are significantly associated with both dementia knowledge and motivation to perform helping behaviors. Based on this, we included experience of having a family member living with dementia and of providing care for a family member living with dementia among our covariates.
Statistical Analysis
Analysis 1: Fitness of the bystander intervention process model
We tested the fitness of the bystander intervention process model using the same approach as that applied by Rabow et al. (1990). First, the rate of intention to perform helping behaviors (referred to as “intention” below) was calculated for all participants and for those who agreed to the former two decisions in the three-step process (i.e., “interpreting the situation as one in which assistance is required,” referred to as “interpretation” below, and “taking personal responsibility,” referred to as “responsibility” below). The relationship between these two elements of the bystander intervention process model and performance of helping behaviors was then tested using a chi-square test. Finally, Guttman scale analysis was used to test the ordering of the three steps (interpretation, responsibility, intention); as criteria, we set >0.9 for the coefficient of reproducibility and >0.65 for the coefficient of scalability (Menzel, 1953; Streiner et al., 2014). The Guttman analysis was performed on three models (see Figure 1). Model 1 included interpretation, responsibility, and intention (three-step), model 2 included responsibility and intention (two-step), and model 3 included interpretation and intention (two step). Because Models 1 and 2 were rejected in this analysis, subsequent analyses examined the model including only interpretation and intention.
Analysis 2: Mediation analysis
We built a parallel mediation model with two mediating variables (i.e., attitude and bystander intervention process; see Figure 2). For each participant, the number of vignettes for which he/she gave a positive response to the interpretation was summed to produce the interpretation score (range 1–4), and similarly, the number of vignettes for which he/she gave a positive response to the intention was produced as the intention score (range 1–4). This is because a mediation analysis is unable to process a binary variable as a mediating variable. Using a regression-based bootstrapping approach, we tested whether dementia attitudes (M1) and interpretation of a need for assistance (M2) mediate the effects of dementia knowledge (X) on intention to perform helping behaviors (Y). For the mediation analysis, PROCESS (Hayes, 2017), a macro program of SPSS (version 24), was used. Bootstrapped (5,000 random resamples) estimates of 95% confidence intervals (CIs) were used to determine significant mediation.
Figure 2.
Complete mediation model indicating beta coefficients for knowledge (X), attitude (M1), interpretation (M2), and intention (Y; n = 900).
Results
Participants’ Characteristics
One thousand participants were recruited, of whom 904 (health and social care workers were excluded; n = 96) were included in the analysis. Table 1 shows the characteristics of the total participant sample. The mean age was 45.0 (SD = 13.9) years; 467 (51.7%) were males; 184 (20.4%) from junior or career college, 481 (53.2%) from university, and 62 (6.9%) from graduate school; 251 (27.8%) had a family member living with dementia; and 93 (10.3%) had experience of providing nursing care for a family member living with dementia. Four cases provided missing data for education and were consequently excluded from the mediation analysis. The mean scores for dementia knowledge and attitudes toward people living with dementia were 8.3 (SD = 1.5), a high score indicating greater knowledge, and 36.6 (SD = 5.8), a high score indicating positive attitude, respectively.
Table 1.
Participants’ Characteristics (N = 904)
| Characteristic | Mean | SD | n | % |
|---|---|---|---|---|
| Knowledge | 8.3 | 1.5 | ||
| Attitude | 36.6 | 5.8 | ||
| Age | 45.0 | 13.9 | ||
| Gender (male) | 467 | 51.7 | ||
| Educationa | ||||
| Junior high school | 14 | 1.5 | ||
| High school | 159 | 17.6 | ||
| Junior or career college | 184 | 20.4 | ||
| University | 481 | 53.2 | ||
| Graduate school | 62 | 6.9 | ||
| Family experienceb (yes) | 251 | 27.8 | ||
| Care experiencec (yes) | 93 | 10.3 |
aFour respondents provided missing data for education.
bExperience of having a family member with dementia.
cExperience of caring for a family member with dementia.
Bystander Intervention Process Model
Table 2 shows, for each of the four vignettes, the response patterns for the bystander intervention process model. In terms of the total sample, the rates of intention to perform helping behaviors were 33.5%, 29.5%, 55.6%, and 17.6% for vignettes A–D, respectively. The chi-square test revealed that, for all vignettes, intention was significantly associated with both interpretation and responsibility (p < .001).
Table 2.
The Decision Process of Helping Behavior (N = 904)
| Variable | Intention | ||||
|---|---|---|---|---|---|
| Agree | Disagree | ||||
| n | % | n | % | ||
| Vignette A | |||||
| Responsibility | Agree | 222 | 85.1 | 39 | 14.9 |
| Disagree | 81 | 12.6 | 562 | 87.4 | |
| Interpretation | Agree | 276 | 55.8 | 219 | 44.2 |
| Disagree | 27 | 6.6 | 382 | 93.4 | |
| Total | 303 | 33.5 | 601 | 66.5 | |
| Vignette B | |||||
| Responsibility | Agree | 192 | 90.6 | 20 | 9.4 |
| Disagree | 75 | 10.8 | 617 | 89.2 | |
| Interpretation | Agree | 231 | 54.0 | 197 | 46.0 |
| Disagree | 36 | 7.6 | 440 | 92.4 | |
| Total | 267 | 29.5 | 637 | 70.5 | |
| Vignette C | |||||
| Responsibility | Agree | 365 | 90.6 | 38 | 9.4 |
| Disagree | 138 | 27.5 | 363 | 72.5 | |
| Interpretation | Agree | 497 | 67.4 | 240 | 32.6 |
| Disagree | 6 | 3.6 | 161 | 96.4 | |
| Total | 503 | 55.6 | 401 | 44.4 | |
| Vignette D | |||||
| Responsibility | Agree | 105 | 78.9 | 28 | 21.1 |
| Disagree | 54 | 7.0 | 717 | 93.0 | |
| Interpretation | Agree | 131 | 41.2 | 187 | 58.8 |
| Disagree | 28 | 4.8 | 558 | 95.2 | |
| Total | 159 | 17.6 | 745 | 82.4 |
Note: Values in italics indicate responses that are not consistent with the ordinality of the hypothesis.
Table 3 shows the coefficients of reproducibility and scalability determined through Guttman analysis of each model. The coefficient of reproducibility exceeded 0.9 for all pairs. Meanwhile, the coefficient of scalability for interpretation and intention exceeded 0.65 for model 3, indicating that interpretation was a prerequisite for intention. Some of the coefficients of scalability were below 0.65 in models 1 and 2; thus, these models were rejected because they did not fulfill the ordering criteria. Finally, we adopted model 3, a two-step bystander intervention process model that included interpretation and intention (Figure 1, bottom).
Table 3.
Guttman Scaling Analysis of Three Models (N = 904).
| Condition | Model 1 | Model 2 | Model 3 | |||
|---|---|---|---|---|---|---|
| CoR | CoS | CoR | CoS | CoR | CoS | |
| Vignette A | 0.959 | 0.653 | 0.955 | 0.325 | 0.985 | 0.890 |
| Vignette B | 0.958 | 0.599 | 0.959 | 0.211 | 0.980 | 0.845 |
| Vignette C | 0.945 | 0.615 | 0.924 | 0.216 | 0.997 | 0.976 |
| Vignette D | 0.968 | 0.657 | 0.970 | 0.341 | 0.985 | 0.870 |
Notes: CoR = coefficient of reproducibility, CoS = coefficient of scalability. Model 1: Interpretation, responsibility, and intention. Model 2: Responsibility and intention. Model 3: Interpretation and intention.
Mediation Analysis
The mean number of vignettes with positive responses to interpretation was 2.29 (SD = 1.26), and the mean number of vignettes with positive responses to intention was 1.36 (SD = 1.23). Table 4 and Figure 2 show the results of the mediation analysis (n = 900). Higher knowledge was significantly associated with positive attitude (β = 0.173, p < .001) and a greater likelihood of interpretation (β = 0.221, p < .001). Gender (β = −0.113, p = .001) and family experience living with dementia (β = 0.127, p = .001) were associated with positive attitude, whereas age (β = 0.150, p < .001) and gender (β = −0.128, p < .001) were associated with interpretation. Positive attitudes (β = 0.255, p < .001), interpretation (β = 0.416, p < .001), age (β = 0.064, p = .026), and gender (β = −0.066, p = .020) were associated with a greater likelihood of intention. The total effect (β = 0.136, p < .001) of knowledge on intention was significant, but the direct effect (β = −0.008, p = .792) was not significant. Both the indirect effect mediated by attitude (β = 0.044, p < .001) and the indirect effect mediated by interpretation (β = 0.092, p < .001) were significant.
Table 4.
Coefficients for the Mediation Model, With Intention (Y) as the Outcome (n = 900)
| Variable | Attitudea (M1) | Interpretationb (M2) | Intentionc (Y) | |||
|---|---|---|---|---|---|---|
| β | p | β | p | β | p | |
| Knowledged (X) | 0.173 | <.001 | 0.221 | <.001 | −0.008 | .792 |
| Attitudea (M1) | 0.255 | <.001 | ||||
| Interpretation (M2) | 0.416 | <.001 | ||||
| Age | 0.041 | .214 | 0.150 | <.001 | 0.064 | .026 |
| Gendere | −0.113 | .001 | −0.128 | <.001 | −0.066 | .020 |
| Educationf | 0.019 | .569 | 0.002 | .961 | −0.021 | .450 |
| Family experienceg | 0.127 | .001 | 0.035 | .353 | 0.003 | .918 |
| Care experienceh | 0.052 | .179 | 0.026 | .491 | 0.029 | .386 |
| R 2 = .0825 | R 2 = .1076 | R 2 = .3266 | ||||
| F(6, 893) = 13.39 | F(6, 893) = 17.945 | F(8, 891) = 54.011 | ||||
| p < .001 | p < .001 | p < .001 |
Notes: M = mediator variable; X = independent variable; Y = dependent variables.
aScore for attitude toward people with dementia.
bThe number of positive responses to interpreting the situation as one in which assistance is required (0–4).
c The number of positive responses to intending to perform helping behaviors (0–4);
dScore for dementia knowledge.
eMale = 1, female = 0.
fGraduation from junior high school = 1, graduation from high school = 2, graduation from junior or career college = 3, graduation from university = 4, graduation from graduate school = 5.
gExperience of having a family member with dementia (“yes” = 1, “no” = 0).
hExperience of providing nursing care for a family member with dementia (“yes” = 1, “no” = 0).
Discussion
This study applied the bystander intervention process model (Stukas & Clary, 2012) to the general public’s exhibition of helping behaviors toward people living with dementia. The results support the model in which interpreting the situation as one where assistance is required is a prerequisite of helping behavior. Moreover, the effect of knowledge on helping behavior intention is mediated by the interpretation in parallel with attitudes toward people living with dementia. This was the first study that applied the bystander intervention process model to helping behavior related to people living with dementia and identified the mediating mechanism on the model. This study helps to justify and improve dementia education programs.
The present sample’s mean score for attitude toward people living with dementia was 36.6 (SD = 5.8). This mean score and variance were slightly lower than those reported in other studies based on university students in 2010 (mean = 39.8, SD = 6.5; Kim & Kuroda, 2011) and convenience store clerks from 2016 to 2018 (mean = 39.4, SD = 7.5; Igarashi et al., 2020). The low variance may have led to an underestimation of the parameters.
The results showed that our first hypothesis (that the bystander intervention process model is a good fit for helping behaviors toward people living with dementia) was partially supported. Interpreting the situation as one in which assistance is required is a necessary prerequisite for exhibiting helping behaviors toward people living with dementia; however, taking personal responsibility is not. The two-step model adopted in the present study fit all four vignettes, despite the diversity of the presented situations; this suggests that the model has high reliability in the context of helping behaviors toward people living with dementia. One possible reason for this discrepancy is that the “diffusion of responsibility” (Darley & Latane, 1968) prevalent in group situations did not occur since the vignette did not indicate the situation of the surrounding bystanders. If individuals are aware of the situation, the decision to take personal responsibility may be an important prerequisite. Furthermore, it is also possible that in our study, the danger of helping a person with dementia was relatively small, compared with other situations like assault. Therefore, the participant may have casually attempted to do it although she/he did not feel responsible.
Furthermore, underlying methodological issues of measurement and statistical analysis may also have led to the discrepancy between the adopted models in our study and the previous studies (Rabow et al, 1990; Anker & Feeley, 2011). In the study of Rabow et al. (1990), where a three-step model for drunk-driving cessation was adopted, personal responsibility was measured using the item “How able were you to intervene?” As this question did not seem to relate to personal responsibility, we adopted a different question, “I need to help her.” However, it was not fully investigated whether both questions were able to measure personal responsibility. In the study of Anker and Feeley (2011), where a four-step model for organ donation and green living was adopted, structural equation modeling and model fit indicator were used to test the bystander intervention process model. Although this structural equation modeling tested the associations between processes, it did not test the sequential ordering as done in Guttman analysis.
After controlling for covariates, knowledge showed a significant total effect on intention to provide help and was completely mediated by attitude and interpretation of a need for assistance. These results replicate those of previous studies (Lane & Yu, 2020; Takao & Maki, 2019) and support our second hypothesis (knowledge of dementia increases the probability of performing helping behaviors via the dementia attitudes and bystander intervention process). Compared with the partial mediation models demonstrated in previous studies (Lane & Yu, 2020; Takao & Maki, 2019), where attitude was the sole mediator, in the present study, interpretation of a need for assistance was shown to be a residual mediator.
Our results provide an empirical basis for awareness-raising approaches which aim to encourage helping behaviors toward people living with dementia. Approaches to raise awareness have been prevalent without an explicit theoretical framework. Recently, the theory of planned behavior (Ajzen, 1991) was applied to propose the positioning of attitude change as the mechanism; however, it was insufficient to explain the mechanism. In the present study, the bystander intervention model was introduced, and the interpretation of the need for help was supported as another underlying mechanism. Dementia education programs that transfer knowledge are expected to promote helping behavior toward people with dementia based on these models.
Furthermore, we found that the above two mechanisms are complete mediation models. Accordingly, it is suggested that if an educational program improves only knowledge, and not the attitudes or the ability to interpret the need for help, it will not promote helping behavior. Interventions that directly improve attitudes and interpretive skills are expected to increase helping behavior. First, in addition to the transfer of knowledge, it is encouraged to couple interventions that will improve attitudes toward people living with dementia. Several dementia education programs blend lectures with sessions to directly affect attitude through facilitating interactions with people living with dementia (e.g., Di Bona et al., 2019; Lokon et al., 2017) or by having people living with dementia share their experiences (e.g., Phillipson et al., 2019; Sari et al., 2020). The implementation of these attitude-oriented programs can have stronger effects on helping behaviors. Second, it is encouraged to convey knowledge about the early symptoms of dementia, beyond knowledge about the prevention and treatment of dementia. Descriptions of the early signs of dementia and differences between the symptoms of dementia and normal aging are usually included in standardized programs such as Dementia Supporters and Dementia Friends (ACT on Alzheimer’s, 2015; Hayashi, 2017). Educating people about the early signs of dementia is supposed to increase their capability to interpret a need for assistance and promote the general public’s exhibition of helping behaviors in the situations in which people living with dementia require help.
This study has several limitations. First, the participants in this study had a high mean score, with a small variance, for dementia knowledge. Thus, there is a possibility that the effect of knowledge was underestimated as a result of the ceiling effect. Second, because it is difficult to measure real-life behaviors, the present study measured behavioral intentions using vignettes. There may be a gap between respondents’ intentions and the behaviors they would perform in real life. In particular, we could not examine the influence of factors that can inhibit helping behaviors, such as the diffusion of responsibility, which has previously been highlighted in relation to the bystander intervention process (Darley & Latane, 1968). Third, both interpretation and behavioral intentions were measured using single questions with binary responses, which raises the risk of measurement error. Future studies should consider using more detailed instruments that feature multiple items and Likert scales, as performed by Anker and Feeley (2011). Third, the present study used data only from Japan and did not examine differences by region or culture. There is little difference in the implementation of helping behavior toward strangers in urban cities in diverse countries (Levine et al., 2001). However, there are considerable differences in attitudes toward people with dementia and older adults across countries and regions (World Alzheimer Report, 2019). As the prevalence of positive attitudes toward people with dementia in Japan is about average, the generalizability of this study cannot be reduced. It will be beneficial to examine whether the bystander intervention model is applicable to other regions and cultures. In addition, as this study was a cross-sectional survey, it is necessary to adopt an experimental approach to further investigate the mediation effect, in the future.
Despite the above limitations, this study is the first to apply the bystander intervention process model in the context of helping behaviors toward people living with dementia. Using Guttman scale analysis, we found that the two-step model, in which the general public interprets the need for assistance and then provides help, is a good fit in this regard. Compared with previous studies, methodologically, we improved the validity of the vignette questions. The study assumed ordinality using Guttman scaling analysis rather than structural equation modeling. We also identified a new underlying mechanism whereby knowledge promotes helping behavior. We can now use this model to examine helping behaviors toward people living with dementia. Knowledge of dementia was identified as being associated with helping behaviors, and this association was found to be mediated by interpretation of a need for assistance and attitude toward people living with dementia. This study provides an empirical basis for the awareness-raising approaches applied in dementia-friendly initiatives.
Acknowledgment
We our appreciation for valuable comments and advice on our later drafts by Dr. Naoki Kondo at Kyoto University.
Contributor Information
Hiroshige Matsumoto, Department of Community Health Nursing, Graduate School of Medicine, The University of Tokyo, Tokyo, Japan.
Ayumi Igarashi, Department of Gerontological Home Care and Long-Term Care Nursing, Graduate School of Medicine, The University of Tokyo, Tokyo, Japan.
Mariko Sakka, Department of Gerontological Home Care and Long-Term Care Nursing, Graduate School of Medicine, The University of Tokyo, Tokyo, Japan.
Manami Takaoka, Department of Gerontological Home Care and Long-Term Care Nursing, Graduate School of Medicine, The University of Tokyo, Tokyo, Japan.
Haruna Kugai, Department of Gerontological Home Care and Long-Term Care Nursing, Graduate School of Medicine, The University of Tokyo, Tokyo, Japan.
Kenichiro Ito, Virtual Reality Educational Research Center, The University of Tokyo, Tokyo, Japan.
Noriko Yamamoto-Mitani, Department of Community Health Nursing, Graduate School of Medicine, The University of Tokyo, Tokyo, Japan; Department of Gerontological Home Care and Long-Term Care Nursing, Graduate School of Medicine, The University of Tokyo, Tokyo, Japan.
Funding
This study was supported by a grant from JSPS KAKENHI (19H03956).
Conflict of Interest
None declared.
References
- ACT on Alzheimer’s. (2015). Dementia friends session workbook. https://actonalz.org/session-materials-0
- Ajzen, I. (1991). The theory of planned behavior. Organizational Behavior and Human Decision Processes, 50(2), 179–211. doi: 10.1016/0749-5978(91)90020-t [DOI] [Google Scholar]
- Alzheimer Disease International. (2016). Dementia friendly communities key principles. https://www.alz.co.uk/adi/pdf/dfc-principles.pdf
- Alzheimer’s Disease International & World Health Organization. (2015). Dementia: A public health priority. https://www.who.int/publications/i/item/dementia-a-public-health-priority
- Alzheimer’s Society. (2020). Dementia Friends. https://www.dementiafriends.org.uk/
- Anker, A. E., & Feeley, T. H. (2011). Are nonparticipants in Prosocial behavior merely innocent bystanders? Health Communication, 26(1), 13–24. doi: 10.1080/10410236.2011.527618 [DOI] [PubMed] [Google Scholar]
- Banyard, V. L. (2008). Measurement and correlates of prosocial bystander behavior: The case of interpersonal violence. Violence and Victims, 23(1), 83–97. doi: 10.1891/0886-6708.23.1.83 [DOI] [PubMed] [Google Scholar]
- Cahill, S., Pierce, M., Werner, P., Darley, A., & Bobersky, A. (2015). A systematic review of the public’s knowledge and understanding of Alzheimer’s disease and dementia. Alzheimer Disease and Associated Disorders, 29(3), 255–75. doi: 10.1097/WAD.0000000000000102 [DOI] [PubMed] [Google Scholar]
- Community Care Policy Network. (2020). Number of dementia friends as at 30th June 2020. http://www.caravanmate.com/result/
- Community Care Policy Network. (2022). Dementia Supporter Caravan. https://www.caravanmate.com/
- Cowan, T. L. (2021). College students’ and community members’ attitudes toward dementia: The impact of dementia friends sessions. Gerontology and Geriatrics Education, 42(1), 140–149. doi: 10.1080/02701960.2019.1657859 [DOI] [PubMed] [Google Scholar]
- Darley, J. M., & Latane, B. (1968). Bystander intervention in emergencies: Diffusion of responsibility. Journal of Personality and Social Psychology, 8(4 Part 1), 377–83. doi: 10.1037/h0025589 [DOI] [PubMed] [Google Scholar]
- Di Bona, L., Kennedy, S., & Mountain, G. (2019). Adopt a care home: An intergenerational initiative bringing children into care homes. Dementia, 18(5), 1679–1694. doi: 10.1177/1471301217725420 [DOI] [PubMed] [Google Scholar]
- GBD 2016 Dementia Collaborators. (2019). Global, regional, and national burden of Alzheimer’s disease and other dementias, 1990–2016: A systematic analysis for the Global Burden of Disease Study 2016. The Lancet Neurology, 18(1), 88–106. doi: 10.1016/S1474-4422(18)30403-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilhooly, M. M., Dalley, G., Gilhooly, K. J., Sullivan, M. P., Harries, P., Levi, M., Kinnear, D. C., & Davies, M. S. (2016). Financial elder abuse through the lens of the bystander intervention model. Public Policy & Aging Report, 26(1), 5–11. doi: 10.1093/ppar/prv028 [DOI] [Google Scholar]
- Hayashi, M. (2017). The Dementia Friends initiative—Supporting people with dementia and their carers: Reflections from Japan. International Journal of Care and Caring, 1(2), 281–287. doi: 10.1332/239788217x14951898377524 [DOI] [Google Scholar]
- Hayes, A. F. (2017). Introduction to mediation, moderation, and conditional process analysis: A regression-based approach (2nd ed.). Guilford Press. [Google Scholar]
- Hebert, C. A., & Scales, K. (2019). Dementia friendly initiatives: A state of the science review. Dementia, 18(5), 1858–1895. doi: 10.1177/1471301217731433 [DOI] [PubMed] [Google Scholar]
- Igarashi, A., Matsumoto, H., Takaoka, M., Kugai, H., Suzuki, M., & Yamamoto-Mitani, N. (2020). Educational program for promoting collaboration between community care professionals and convenience stores. Journal of Applied Gerontology, 39(7), 760–769. 10.1177/0733464819871878 [DOI] [PubMed] [Google Scholar]
- Kim, K., & Kuroda, K. (2011). Factors related to attitudes toward people with dementia: Development attitude toward dementia scale and dementia knowledge scale. Bulletin of Social Medicine, 28(1), 43–56. [Google Scholar]
- Lane, A. P., & Yu, F. C. H. (2020). Person-centered attitudes mediate the association between dementia knowledge and help-giving intentions in Singapore. International Psychogeriatrics, 32(3), 413–414. doi: 10.1017/S1041610219000796 [DOI] [PubMed] [Google Scholar]
- Latané, B., & Darley, J. M. (1970). The unresponsive bystander: Why doesn’t he help? Appleton-Century-Crofts. [Google Scholar]
- Levine, R. V., Norenzayan, A., & Philbrick, K. (2001). Cross-cultural differences in helping strangers. Journal of Cross-Cultural Psychology, 32(5), 543–560. doi: 10.1177/0022022101032005002 [DOI] [Google Scholar]
- Lokon, E., Li, Y., & Parajuli, J. (2017). Using art in an intergenerational program to improve students’ attitudes toward people with dementia. Gerontology & Geriatrics Education, 38(4), 407–424. doi: 10.1080/02701960.2017.1281804 [DOI] [PubMed] [Google Scholar]
- Maki, Y., Takao, M., Hattori, H., & Suzuki, T. (2020). Promoting dementia-friendly communities to improve the well-being of individuals with and without dementia. Geriatrics and Gerontology International, 20(6), 511–519. doi: 10.1111/ggi.13896 [DOI] [PubMed] [Google Scholar]
- Matsuda, Y., Hashimoto, R., Takemoto, S., Yoshioka, Y., Uehara, T., & Kawasaki, Y. (2018). Educational benefits for nurses and nursing students of the dementia supporter training program in Japan. PLoS One, 13(7), e0200586. doi: 10.1371/journal.pone.0200586 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Menzel, H. (1953). A new coefficient for scalogram analysis. Public Opinion Quarterly, 17(2), 268. doi: 10.1086/266460 [DOI] [Google Scholar]
- Mikami, M., Nakao, R., Horikawa, R., Sugiyama, K., Sawada, Y., Kirino, M., & Takemoto, Y. (2017). Developing a scale to assess dementia-related knowledge among local residents. Bulletin of Social Medicine, 18(21) 30 [in Japanese]. [Google Scholar]
- Ministry of Health Labour and Welfare. (2015). The comprehensive strategy for promotion of policy measures against dementia (new orange plan) summary. https://www.mhlw.go.jp/stf/seisakunitsuite/bunya/nop_1.html [Google Scholar]
- Ministry of Justice. (2019). Statistics on foreign residents. http://www.moj.go.jp/housei/toukei/toukei_ichiran_touroku.html
- Perry-Young, L., Owen, G., Kelly, S., & Owens, C. (2018). How people come to recognise a problem and seek medical help for a person showing early signs of dementia: A systematic review and meta-ethnography. Dementia, 17(1), 34–60. doi: 10.1177/1471301215626889 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phillipson, L., Hall, D., Cridland, E., Fleming, R., Brennan-Horley, C., Guggisberg, N., Frost, D., & Hasan, H. (2019). Involvement of people with dementia in raising awareness and changing attitudes in a dementia friendly community pilot project. Dementia, 18(7–8), 2679–2694. doi: 10.1177/1471301218754455 [DOI] [PubMed] [Google Scholar]
- Rabow, J., Newcomb, M. D., Monto, M. A., & Anthony, C. R. (1990). Altruism in drunk driving situations: Personal and situational factors in intervention. Social Psychology Quarterly, 53(3), 199–213. doi: 10.2307/2786959 [DOI] [Google Scholar]
- Rimmer, E., Wojciechowska, M., Stave, C., Sganga, A., & O’Connell, B. (2005). Implications of the Facing Dementia Survey for the general population, patients and caregivers across Europe. International Journal of Clinical Practice, 59, 17–24. doi: 10.1111/j.1368-504x.2005.00482.x. [DOI] [PubMed] [Google Scholar]
- Sari, D. W., Igarashi, A., Takaoka, M., Yamahana, R., Noguchi-Watanabe, M., Teramoto, C., & Yamamoto-Mitani, N. (2020). Virtual reality program to develop dementia-friendly communities in Japan. Australasian Journal on Ageing. doi: 10.1111/ajag.12797 [DOI] [PubMed] [Google Scholar]
- Shannon, K., & Bail, K. (2018). Dementia-friendly community initiatives: An integrative review. Journal of Clinical Nursing. doi: 10.1111/jocn.14746 [DOI] [PubMed] [Google Scholar]
- Streiner, D. L., Norman, G. R., & Cairney, J. (2014). Health measurement scales: A practical guide to their development and use. Oxford University Press. [Google Scholar]
- Stukas, A. A., & Clary, E. G. (2012). Altruism and helping behavior. In V. S. Ramachandran (Ed.), Encyclopedia of human behavior (2nd ed., pp. 100–107). Academic Press. [Google Scholar]
- Takao, M., & Maki, Y. (2019). Effects of attachment to and participation in the community on motivation to participate in dementia prevention and support activities: Analysis of Web survey data. Psychogeriatrics, 19(3), 236–245. doi:` 10.1111/psyg.12388 [DOI] [PubMed] [Google Scholar]
- Werner, P. (2003). Knowledge about symptoms of Alzheimer’s disease: Correlates and relationship to help-seeking behavior. International Journal of Geriatric Psychiatry, 18(11), 1029–1036. doi: 10.1002/gps.1011 [DOI] [PubMed] [Google Scholar]
- World Alzheimer Report. (2019). World Alzheimer Report 2019, attitudes to dementia. Alzheimer’s Disease International, 1, 15. https://www.alz.co.uk/research/world-report-2019 [Google Scholar]