Abstract
Background
SARS-CoV-2 infection in transplant patients has shown greater lethality and vaccination in this group of patients has shown less information. The objective of this study is to show the statistics in Mexico of lethality in kidney recipients infected with COVID-19 in relation to vaccination and variants of the coronavirus.
Methods
This is a bibliographic search of kidney transplant recipient patients since the start of the pandemic in Mexico to determine lethality after SARS-CoV-2 compared to the general population and in relation to patients, the 4 most important infectious peaks in the country due to identified variants, and also before and after vaccination.
Results
The global lethality is 26.91% from the beginning of the pandemic to April 9, 2022 in kidney recipients in Mexico (130 deaths of 483 infected kidney transplant recipients) compared to the national lethality of 5.60%. Variant B. 1.1.220 represented the highest lethality with 30.43% and the lowest lethality was Omicron with 16.41%. The lethality prior to vaccination was 30.94% and 23.46% after it.
Conclusion
Both some variants and vaccination have influenced a lower lethality due to COVID-19 in Mexico in kidney transplant patients; It is important to consider global recommendations, such as a third or fourth dose, a combination of mRNA vaccines and vectors in order to reduce lethality in this group of patients.
Due to the COVID-19 pandemic, it was expected that immunocompromised patients would have a higher number of complications and higher associated lethality [1], [2]. Within the first days of the pandemic, few data were available regarding renal recipients infected with SARS-CoV-2, where the most vigilant surveillance was based. narrow in the context of immunosuppression, although the symptoms were very similar to the non-transplanted population [3], [4]. Despite numerous studies, mortality can still be highly variable, some studies mention probabilities of death of 21.3%, assuming that the 28-day case - fatality rate is high in transplant patients, even newly transplanted patients may have a higher risk of death by COVID-19 compared to dialysis patients on the transplant waiting list [5]. Another study determines a mortality of 28% in renal transplant recipients, compared to 1% to 5% of the general population or even 8% to 15% of those >70 years of age in the United States [6]. And yet another study on mortality of 17.9% highlighted that age >60 years, cardiovascular disease, dyspnea, and fever maintained a risk association for death in a multivariate analysis [7]. It has also been determined that in addition to the higher mortality associated with SARS-CoV-2, kidney transplant recipients have a higher percentage of acute kidney injury [8].
With the knowledge of the high lethality and with the advent of vaccination, the first studies appear after the application of the first dose of the vaccine, regardless of which, documenting the low response of detectable antibodies, with only 17% of transplant recipients vaccinated [9] and considered a higher seroconversion after the second dose of the vaccine [10], [11]. Subsequently, studies with second doses of vaccination appear where the detection of antibodies increases considerably to 54% of transplanted people; however, these data demonstrate that a significant population of transplant recipients remain at risk of COVID-19 after the second dose of the vaccine, and interventions are proposed to improve this response to the vaccine such as additional doses (third dose) or modulation of immunosuppression [12].
Some explanations have been sought for this deficiency of antibody formation and a suboptimal effect of vaccination against SARS-CoV-2; a meta-analysis including data from 947 recovered transplant recipients from 15 clinical trials showed significantly lower rates of seroconversion among those who received mycophenolate mofetil, unlike other immunosuppressive agents [13], even with the measurement of antibodies of 37% against 63% of those who did not have antimetabolite against those who did, respectively [14]. With current knowledge, possible solutions lie in: 1. additional vaccination, 2. combination of mRNA and vector vaccines, 3. temporary interruption or reduction of the dose of mycophenolate, and 4. possibly increasing the dose of steroid; however, all of these should require additional focus [13]. Encouraging data suggest that age >68 years and longer time since transplantation were factors associated with antibody response [15]. In transplanted people, a deficient initial formation of antibodies has been observed, as well as low antibody production when the infection is acquired, the follow-up has resulted in a considerable decrease in a short time, 3 months, with a drop of up to 87% of the levels of anti-SARS-CoV-2 antibodies [16]. In addition, it was also documented that patients who received mRNA vaccines had significantly higher rates of seroconversion compared to vector-based vaccines [17].
Recent studies with a third dose of the vaccine showed that COVID-19 infection was observed in low responders and nonresponders, representing the 29% who did not show a humoral response after the third dose, and the humoral response to the vaccine was affected in patients receiving mycophenolate acid or belatacep; in addition, reduced kidney function and CD4 lymphopenia were also associated with a poor response to the vaccine [18,19]. Therefore, the objective of this study is to show the epidemiologic data of Mexico in relation to vaccination in our country and the influence on the lethality of kidney transplant patients due to SARS-CoV-2 in relation to the general population, as well as with variants of the same coronavirus.
Material and Methods
Design
This is a bibliographic search of patients infected with SARS-CoV-2 in Mexico that included the general population and kidney transplant patients.
Patients
All patients infected with SARS-CoV-2, both the general population and kidney transplant recipients, were considered eligible from February 28, 2020 in Mexico to April 9, 2022 of the official records in the country. The patients were classified in two ways: (1) by the peaks (waves ) of greater infection identified in Mexico and (2) based on data from the National Institute of Genomic Medicine (INMEGEN) where SARS-CoV-2 variants were identified where they were established four groups: (1) the first wave of infection, when the variant of the coronavirus B 1.1.220 predominated; (2) the second wave of infection, when the variant B 1.1.519 predominated; (3) the third wave of infection, when the Alpha and Gamma variants predominated at the beginning and later multiple Delta variants dominated; and (4) from the end of December 2021 to April 2022, when the Omicron variant predominated. A classification was also made in relation to vaccination: (1) patients infected before vaccination in Mexico, before January 7, 2021 (although vaccination was officially on December 25, 2020, protection by vaccination usually starts 15 days after application, which is why the date was considered in January); and (2) after vaccination. From these statistics, the number of infected people and those with a death outcome were sought in order to determine their lethality at the moments mentioned historically.
Data Collection
The data of the registered patients were obtained from the national statistics of the Secretary of Health of Mexico, as well as the official data of the National Transplant Center, from which the number of infected people per period and the corresponding lethality.
Statistics
The lethality data are presented in frequencies and percentages globally in the general population and transplant recipients, as well as the subdivision of lethality by variants in each wave of infection in Mexico and by the effect of vaccination.
Results
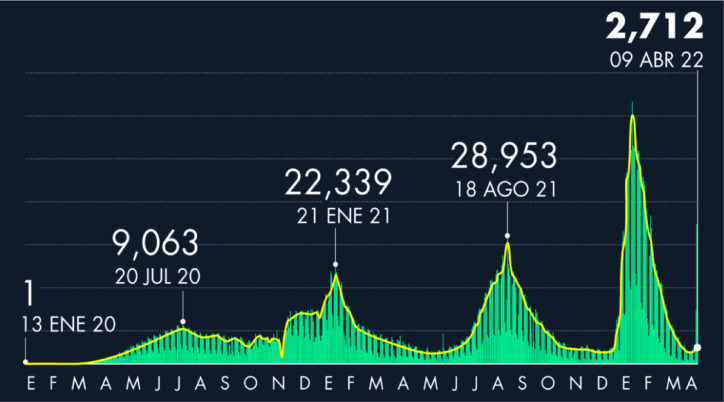
The bibliographic search is carried out starting with the National Institute of Genomic Medicine data, where it establishes the main variants during the time of the pandemic in Mexico; the typing of all the cases of the variants was not carried out, with initial percentages close to 10%, a gradual increase until the number of genomes was around 70% to 90% of the cases, and remaining consistent since then. The most predominant variants were identified in each of the peaks, with the highest incidence in Mexico, there have been 4 peaks of infection in the country: the first peak with its nadir on July 20, 2020; second peak with its nadir on January 21, 2021; third peak with its nadir on August 18, 2021; and fourth peak with its nadir on January 19, 2022. Currently in Mexico with a fourth peak due to the Omicron variant, of which the final lethality will not be reported, because it is active at this time with its highest moment of contagion in a single day for January 19, 2022 (60,552 people infected), from there with a continuous decrease until the end of the data analysis on April 9, 2022, where there are 5,722,541 accumulated cases of infected people with 323,729 deaths officially registered by the Mexican Secretary of Health (Fig 1 ).
Fig 1.
Number of cases per day of COVID-19 in Mexico. Cumulative cases as of April 9, 2022 of 5,722,541 deaths up to this same period of 323,729. Source: The Secretary of Health of Mexico, image taken from the newspaper El Economista [20].
The lethality in the general population is 5.60% compared to 26.91% for the transplanted population. Regarding the cases, an analysis is made first in relation to the moments of greatest infection by wave of infection in Mexico and later in relation to vaccination.
In Relation to the Variants
The first wave was dominated by the B 1.1.220 variant, with a lethality in the general population of 9.37% (109,456 deaths per 1,168,395 infected people) and 30.43% (63 deaths per 207 infected people) in the transplanted population in this same period. In the case of the second wave, with a predominance of variant B 1.1.519, the lethality in the general population was 9.15% (110,924 deaths out of 1,212,295 of the total number of people infected in the period), compared to the lethality of transplanted people of 23.02% (29 of 126 people). In the third wave there was no variant predominance and it was mainly distributed among the Alpha, Gamma, Delta, and other variants with a lethality of 4.99% in the general population (78,439 of 1,571,256 people for the period) against 29.67% in transplant recipients (27 of 91 people for the same period). Finally, the fourth wave, current in Mexico, with a predominance of the Omicron variant as of April 9, has a lethality of 1.40% (24,910 of 1,770,595 people) compared to 16.41% in renal recipients for this same period 11 of 67) (Table 1 ).
Table 1.
General and transplant population with COVID-19; as well as deaths associated with variants and vaccination
|
Infected |
Deaths |
Lethality | |||||
|---|---|---|---|---|---|---|---|
| Totals at the end of the period | During the period | Totals at the end of the period | During the period | % | |||
| IN RELATION TO THE VARIANTS | |||||||
| Total population in Mexico | 5,722,541 | 323,729 | 5.60 | ||||
| B 1.1.220/Others (28-02-2020 to 05-12-2020) | 1,168,395 | 1,168,395 | 109,456 | 109,456 | 9.37 | ||
| B 1.1.519/Others (06-12-2020 to 15-05-2021) | 2,380,690 | 1,212,295 | 220,380 | 110,924 | 9.15 | ||
| Alpha/Gamma/Delta/Others (16-05-2021 to 27-12-2021) | 3,951,946 | 1,571,256 | 298,819 | 78,439 | 4.99 | ||
| Omicron/Others (28-12-2022 to 09-04-2022) | 5,722,541 | 1,770,595 | 323,729 | 24,910 | 1.40 | ||
| Population with kidney transplant in Mexico | 483 | 130 | 26.91 | ||||
| B 1.1.220/Others (28-02-2020 to 05-12-2020) | 207 | 207 | 63 | 63 | 30.43 | ||
| B 1.1.519/Others (06-12-2020 to 15-05-2021) | 333 | 126 | 92 | 29 | 23.02 | ||
| Alpha/Gamma/Delta/Others (16-05-2021 to 27-12-2021) | 424 | 91 | 119 | 27 | 29.67 | ||
| Omicron/Others (28-12-2022 to 09-04-2022) | 483 | 67 | 130 | 11 | 16.41 | ||
| IN RELATION TO VACCINATION | |||||||
| Total population in Mexico | 5,722,541 | 323,729 | 5.60 | ||||
| Pre-vaccination (28-02-2020 to 07-01-2021) | 1,493,569 | 1,493,569 | 131,031 | 131,031 | 8.77 | ||
| Post-vaccination (08-01-2021 to 09-04-2022) | 5,722,541 | 4,228,972 | 323,729 | 192,698 | 4.55 | ||
| Population with kidney transplant in Mexico | 483 | 130 | 26.91 | ||||
| Pre-vaccination (28-02-2020 to 07-01-2021) | 223 | 223 | 69 | 69 | 30.94 | ||
| Post-vaccination (08-01-2021 to 09-04-2022) | 483 | 260 | 130 | 61 | 23.46 | ||
Regarding Vaccination
Before vaccination in Mexico, the lethality was 8.77% (131,031 of 1,493,569 of the total infected people) compared to 30.94% for the transplant population (69 of 223 for the period before vaccination). The figures after vaccination started was 4.55% lethality in the general population (192,698 of 4,228,972 of the population that contracted COVID-19) against 23.46% of renal recipients (61 of 260) (Table 1).
Discussion
The lethality in transplant patients in Mexico by SARS-CoV-2, according to official figures, is 4 times more than in the general population, 26.91% against 5.60%. In our country there were 4 “peaks” (also called “waves”) of contagion where a particular variant predominated, compared to others in smaller numbers, according to studies by the National Institute of Genomic Medicine. In the general population, these variants also had a specific lethality that decreased as each wave of contagion appeared; from the first to the second wave it was almost constant 9.37% against 9.15%, then in the third to 4.99% (almost half of lethality) and in the fourth wave 1.40% (7 times the lethality of the first wave). On the other hand, in people with kidney transplants, this lethality was initially 30.47% in the first wave and decreased to 16.41% for the current wave of contagion (half of the initial lethality), with the number of deaths still being extremely high among people who become infected.
An important point to clarify is that immunity conditions are decreased in patients with kidney disease mainly owing to uremia. In addition, community immunity is also interrupted in elderly people, people with chronic degenerative diseases, and in patients with chronic kidney disease or transplants, because the differentiation of B cells, as their activating factor, compromises the formation of antibodies and thus the effectiveness of vaccination [21], [22]. In renal transplant patients, both innate and adaptive immunity are impaired. Innate immunity with impairment of costimulatory molecules such as CD80 and CD86 for antigen-presenting cells and dendritic cells are common in patients with elevated uremic toxins, and Toll-like receptor expression is also modified, all of which decreases antibody production. In the case of adaptive immunity it is diminished, with deterioration in the ability to present antigens incapable of recognizing the pathogen and B-cell lymphopenia; They also mention that the neutralizing antibody titers for SARS-CoV-2 protein S are adequate after the third dose of the vaccine, especially in mRNA vaccines in solid organ transplant recipients in general [23]. In some way, this may explain why after vaccination in the general population, lethality is reduced by half (8.77%-4.55%), and in the case of people with kidney transplants, said lethality did not drop even a third of the stage before vaccination (30.94%-23.46%) in our country [24].
A study in Scotland [25] shows that 93% of its transplant population (5281 transplant recipients) had a schedule of 2 vaccines. Where the rate of infection and hospitalization was evaluated and where its efficacy was 33% and 38%, respectively, for each event, the outcome of death was 10% in kidney recipients and <0.1% in the vaccinated population. These figures contrast with those found in our population, with a lethality rate of 23.46% when vaccination has already started. Unfortunately, we also do not have the figures of the transplanted population that has already complied with the 2-dose scheme, much less a booster with a third, which is recommended in this vulnerable group in addition to other complementary strategies to reduce the risk of COVID-19 infection and its complications. Figures closer to our lethality are described in some meta-analyses [26], [27] where it ranged from 18.6% to 23%, respectively, and in studies in Europe and America, mortality ranges from 20% to 32% in kidney transplant recipient patients compared to the general population (between 1% to 14% after adjusting for age and comorbidities) [28]. However, within the guidelines to be followed is that transplant patients should receive vaccination schedules of 3 and ≤4 doses; reduction of immunosuppression is a consideration in the early stages of the infection, as well as considering the comorbidities that each patient presents in a particular way with the intention of making preventive maneuvers.
Finally, regarding the variants of SARS-CoV-2 that are appearing, they are known to have compromised the effect of the vaccines used, but despite this, there is considerable efficacy in reducing infection, serious events that require hospitalization and, above all, mortality [29].
The main limitation of the study is to base it solely on national statistics without being able to establish a cohort of patients infected by SARS-CoV-2 in renal recipients in order to determine all the variables to establish risk factors, knowledge of evolution, type of vaccine, measurement of antibodies, and so on.
Conclusions
There is a very high lethality in kidney transplant patients with SARS-CoV-2 infection owing to the their poor immune response. In Mexico, the lethality is 1 death for every 4 transplanted people, unlike the general population (1 death for every 20 people infected). We must reinforce the idea of 3 to 4 doses of the vaccine in this group of patients, the reduction of immunosuppression in the first phase of the infection, attention to the comorbidities present in each renal transplant recipient, and a combination of mRNA and vector vaccines in order to reduce lethality in this group of patients.
References
- 1.Wu C, Chen X, Cai Y, et al. Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 pneumonia in Wuhan, China. JAMA Intern Med. 2020;180:934–943. doi: 10.1001/jamainternmed.2020.0994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hernández-Rivera J, Silva-Rueda R, Mendoza Mariana M, et al. COVID-19 generalidades y enfermedad renal. Artículo de revisión. Gac Med Bilbao. 2021;118:143–159. [Google Scholar]
- 3.Nair V, Jandovitz N, Hirsch JS, et al. COVID-19 in kidney transplant recipients. Am J Transplant. 2020;20:1819–1825. doi: 10.1111/ajt.15967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pérez RE, Arce AMT, Meléndez AR, et al. Survival of transplanted patients infected with moderate and severe COVID-19 in Mexico. Trends Transplant. 2020;14:1–6. [Google Scholar]
- 5.Hilbrands LB, Duivenvoorden R, Vart P, et al. COVID-19-related mortality in kidney transplant and dialysis patients: results of the ERACODA collaboration. Nephrol Dial Transplant. 2020;35:1973–1983. doi: 10.1093/ndt/gfaa261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Akalin E, Azzi Y, Bartash R, et al. COVID-19 and kidney transplantation. N Engl J Med. 2020;382:2475–2477. doi: 10.1056/NEJMc2011117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Caillard S, Chavarot N, Francois H, et al. French SOT COVID Registry. Is COVID-19 infection more severe in kidney transplant recipients? Am J Transplant. 2021;21:1295–1303. doi: 10.1111/ajt.16424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cravedi P, Mothi SS, Yorg A, et al. COVID-19 and kidney transplantation: Results from the TANGO International Transplant Consortium. Am J Transplant. 2020;20:3140–3148. doi: 10.1111/ajt.16185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Boyarsky BJ, Werbel WA, Avery RK, et al. Immunogenicity of a single dose of SARS-CoV-2 messenger RNA vaccine in solid organ transplant recipients. JAMA. 2021;325:1784–1786. doi: 10.1001/jama.2021.4385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Middleton RJ, Gorton J, O'Riordan EO, et al. Impact of shielding and first dose of COVID-19 vaccination in kidney transplant recipients. Nephron. 2022;146:64–66. doi: 10.1159/000518631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Castelló IB, Maestre EM, Escorihuela DR, et al. SARS-CoV-2 infection after vaccination: kidney transplant recipient profile and disease evolution in a single center [e-pub ahead of print]. Transplant Proc doi: 10.1016/j.transproceed.2021.12.013, [accessed January 7, 2022]. [DOI] [PMC free article] [PubMed]
- 12.Boyarsky BJ, Werbel WA, Avery RK, et al. Antibody response to 2-dose SARS-CoV-2 mRNA vaccine series in solid organ transplant recipients. JAMA. 2021;325:2204–2206. doi: 10.1001/jama.2021.7489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Karbasi-Afshar R, Izadi M, Fazel M, Khedmat H. Response of transplant recipients to influenza vaccination based on type of immunosuppression: a meta-analysis. Saudi J Kidney Dis Transpl. 2015;26:877–883. doi: 10.4103/1319-2442.164556. [DOI] [PubMed] [Google Scholar]
- 14.Rozen-Zvi B, Yahav D, Agur T, Zingerman B, Ben-Zvi H, Atamna A. ntibody response to SARS-CoV-2 mRNA vaccine among kidney transplant recipients: prospective cohort study. Clin Microbiol Infect. 2021;S1198-743X:00216-0. doi: 10.1016/j.cmi.2021.04.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yi SG, Moore LW, Eager T, et al. Risk factors associated with an impaired antibody response in kidney transplant recipients following 2 doses of the SARS-CoV-2 mRNA vaccine. Transplant Direct. 2021;8:e1257. doi: 10.1097/TXD.0000000000001257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fernandes G, Devresse A, Scohy A, et al. Rapid cecline in vaccine-induced anti-SARS-CoV-2 antibody titers 3 months after kidney transplantation: a case series from Belgium. Transplantation. 2022;106:e98–e99. doi: 10.1097/TP.0000000000003963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Correia AL, Leal R, Pimenta AC, et al. The type of SARS-CoV-2 vaccine influences serological response in kidney transplant recipients. Clin Transplant. 2022;36:e14585. doi: 10.1111/ctr.14585. [DOI] [PubMed] [Google Scholar]
- 18.Ducloux D, Bamoulid J, Chabannes M, et al. Current vaccine strategies against SARS_CoV-2 only poorly protect kidney transplant recipients. J Infect. 2022;84:e34–e35. doi: 10.1016/j.jinf.2022.01.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Quiroga B, Soler MJ, Ortiz A, et al. Loss of humoral response 3 months after SARS-CoV-2 vaccination in the CKD spectrum: the multicentric SENCOVAC study. Nephrol Dial Transplant. 2022;37:994–999. doi: 10.1093/ndt/gfac007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.El Eleconomista. Número de casos de Covid-19 en México al 09 de abril de 2022, < https://www.eleconomista.com.mx/politica/Numero-de-casos-de-Covid-19-en-Mexico-al-09-de-abril-de-2022-20220410-0001.html >; 2022 [accessed 09.04.22].
- 21.Hou YC, Lu KC, Kuo KL. The efficacy of COVID-19 vaccines in chronic kidney disease and kidney transplantation patients: a narrative review. Vaccines (Basel) 2021;9:885. doi: 10.3390/vaccines9080885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pahl MV, Gollapudi S, Sepassi L, et al. Effect of end-stage renal disease on B-lymphocyte subpopulations, IL-7, BAFF and BAFF receptor expression. Nephrol Dial Transplant. 2010;25:205–212. doi: 10.1093/ndt/gfp397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ando M, Shibuya A, Tsuchiya K, Akiba T, Nitta K. Reduced expression of Toll-like receptor 4 contributes to impaired cytokine response of monocytes in uremic patients. Kidney Int. 2006;70:358–362. doi: 10.1038/sj.ki.5001548. [DOI] [PubMed] [Google Scholar]
- 24.Government of Mexico. Special newsletter on transplants and COVID 19, < https://www.gob.mx/cenatra/documentos/boletin-informativo-especial-trasplantes-y-covid-19 >; 2022 [accessed 09.04.22].
- 25.Thomson P, Methven S, Mark PB. The impact of vaccination on incidence and outcomes of SARS-CoV-2 infection in patients with kidney failure in Scotland. J Am Soc Nephrol. 2022;33:677–686. doi: 10.1681/ASN.2022010046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Raja MA, Mendoza MA, Villavicencio A, et al. COVID-19 in solid organ transplant recipients: a systematic review and meta-analysis of current literature. Transplant Rev (Orlando) 2021;35 doi: 10.1016/j.trre.2020.100588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kremer D, Pieters TT, Verhaar MC, et al. A systematic review and meta-analysis of COVID-19 in kidney transplant recipients: lessons to be learned. Am J Transplant. 2021;21:3936–3945. doi: 10.1111/ajt.16742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Devresse A, De Greef J, Yombi JC, et al. Immunosuppression and SARS-CoV-2 infection in kidney transplant recipients. Transplant Direct. 2022;8:e1292. doi: 10.1097/TXD.0000000000001292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wahid M, Jawed A, Mandal RK, et al. Variants of SARS-CoV-2, their effects on infection, transmission and neutralization by vaccine-induced antibodies. Eur Rev Med Pharmacol Sci. 2021;25:5857–5864. doi: 10.26355/eurrev_202109_26805. [DOI] [PubMed] [Google Scholar]