Abstract
Polycystic ovary syndrome (PCOS), a frequently occurring health issue, has a significant effect on the cosmetic, metabolic, psychosocial and fertility aspects of women. A multidisciplinary team approach based on the core pillars of screening, assessment and counselling to detect, prevent and treat physiological and psychological issues in PCOS is very essential. Women are treated medically, but the psychosocial part is often forsaken. Hence, counselling forms an integral part of PCOS management that enables enhanced clinical outcomes and patient satisfaction. Digital tools and PCOS support groups have built an opportunity for physicians to create awareness, help timely diagnosis and overcome PCOS symptoms. The absence of clear guidelines to tackle the often less discussed aspects of PCOS warrants the need for consensus on PCOS counselling. This review summarizes the biopsychosocial health, clinical assessment and treatment strategies of PCOS and associated co-morbidities. The review article will discuss the clinician’s role in patient education with the special focus on counselling of females with PCOS regardless of age group.
Keywords: Biopsychosocial health, counselling, patient education, polycystic ovary syndrome
INTRODUCTION
Polycystic ovary syndrome (PCOS) is described as a thief of womanhood.[1] It has implications on cosmetic, metabolic, psychosocial and fertility aspects, making the multidisciplinary treatment approach mandatory rather than simply using medications. Counselling and patient education about PCOS are inevitably essential to address the health and psychosocial problems associated with PCOS; however, multiple health care practitioners (HCPs) may struggle with counselling. Male HCP may not be comfortable dealing with gynaecological or dermatologic issues related to PCOS, especially in adolescent girls. There are no clear guidelines on how to approach distress in women living with PCOS. Hence, there is a need for guidance on PCOS counselling that could serve as a toolkit for all the HCPs involved in treating PCOS.
Section 1: Definition of PCOS and diagnostic criteria
Definition: Polycystic ovary syndrome (PCOS) is a common endocrine disorder presenting as hyperandrogenism and anovulation, occurring at any age from adolescence to womanhood causing physical and psychological co-morbidities.[2]
Diagnostic criteria for PCOS: The diagnosis of PCOS is critical for the precise and timely institution of treatment. The complexities attached to PCOS allowed the proposal of three diagnostic criteria in adult women—National Institutes of Health (NIH) in 1990, Rotterdam American Society for Reproductive Medicine and the European Society of Human Reproduction and Embryology (ASRM/ESHRE)-sponsored PCOS Consensus Workshop Group in 2004, and Androgen Excess and PCOS Society (AE-PCOS) in 2006 [Figure 1].[3] Lujan et al.[4] suggested conservative diagnosis due to its characteristics that included appropriate patient education, careful treatment and enduring follow-up of patients as the actual health risks of these distinct phenotypes are slowly revealed. The NIH Consensus further recommended broader Rotterdam/ESHRE/ASRM criteria with the inclusion of a comprehensive PCOS phenotype [Box 1].[5] More criteria met by the patient with PCOS would imply a more severe phenotype; however, they do not provide any treatment guidance. Diagnostic investigations must exclude other causes and include thyroid function tests, prolactin, serum testosterone, dehydroepiandrosterone sulphate and follicle-stimulating hormone (FSH) levels.[6,7,8,9] Thus, we rule out Cushing’s disease, non-classic congenital adrenal hyperplasia, hypothyroidism and acromegaly, depending on particular circumstances.
Figure 1.
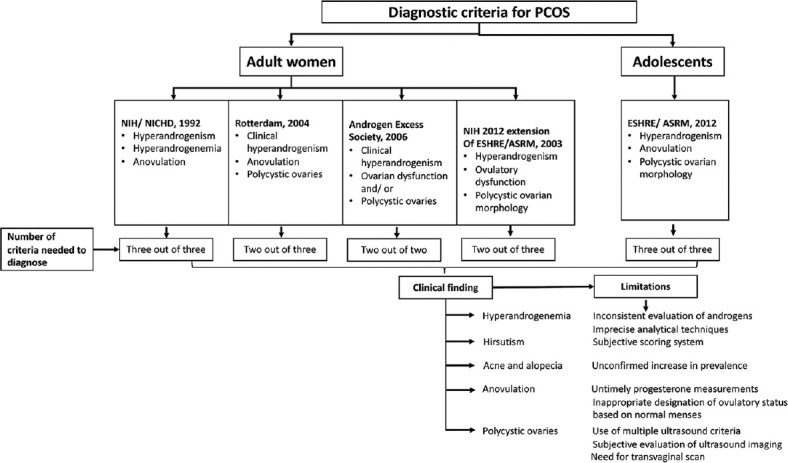
Diagnostic criteria for PCOS
Box 1.
PCOS phenotypes
| Phenotype A: hyperandrogenism + ovulatory dysfunction + PCOM |
| Phenotype B: hyperandrogenism + ovulatory dysfunction |
| Phenotype C: hyperandrogenism + PCOM |
| Phenotype D: ovulatory dysfunction + PCOM |
Challenges with PCOS:
Age: The spectrum of age groups affected by PCOS is extensive, including adolescent girls, women yet to marry, young women and preconception age. Thus, this greatly impacts the diagnostic tests, mode of treatment and expected outcomes.
Associated complications and co-morbid conditions: PCOS increases the prevalence of diverse complications and co-morbidities including metabolic disorders, psychological disorders, cardiac diseases and rarely endometrial cancer. Therefore, the clinical approach of diagnosis and treatment varies depending upon the current clinical condition of the patient.
Above all, counselling forms a pivotal part of the treatment regimen from commencing treatment till follow-up to achieve the maximum therapeutic benefits.
Section 2: Biopsychosocial prism of health
The biopsychosocial framework encompasses the three domains—biological, psychological and social factors—that govern the health status of the patient. It emphasizes the psychological and social causes of PCOS and its influence on the physical health of the patient [Box 2]. The negative biopsychosocial consequences warrant the need to create awareness and address these conditions promptly and correctly, and it is important to understand that only the biomedical approach may not show efficient results and needs psychosocial and social support. Indian women and adolescents too predominantly demonstrate PCOS with higher incidence and awareness in the urban population than rural.[10] Infertility, particularly in the Indian scenario, is imperilled with social pressure due to the importance given to begetting children by society [Figure 2].
Box 2.
Biopsychosocial prism of health
| Along with the biomedical approach, psychological support and social support are key facets of overall health. |
| The three biopsychosocial parameters determine the quality of life. |
| Psychological comorbidity, social comorbidity, sexual dysfunction, negative self-image, lowered self-esteem and eating disorders are common in patients with PCOS that impacts the physical health and psychological well-being of women. |
Figure 2.
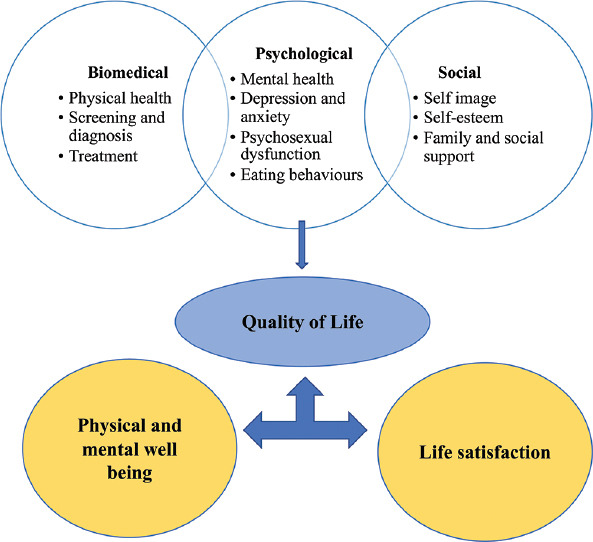
Biopsychosocial model of PCOS—a pragmatic approach to overall well-being
Psychological co-morbidity
A cross-sectional study in women with PCOS showed that 32% of the women were affected with anxiety and 5% were severely depressed, indicating the importance of assessment of mental health disorders in view of the factors influencing psychological well-being.[11] Studies show a curvilinear relationship between free testosterone and negative mood scale scores across the groups.[12] Recommendations suggest screening for depression and anxiety in adults and adolescents with PCOS using appropriate psychological instruments. In Indian women, a 54% prevalence of depression (GHQ-28 score ≥8) was reported, of whom 72% were obese, 70% had hirsutism, 61% had acne and 56% were infertile, indicating a considerable effect on the quality of life (QoL) of these women.[13] A Swedish registry of patients with PCOS (n = 24,385) and their full-siblings (n = 25,921) identified a range of psychiatric disorders in them. They analysed that the individuals with PCOS have 50% increased odds of psychiatric disorders, and their siblings too showed a higher risk of certain psychiatric comorbidities. The crude odds ratios for attempted suicide were 40% higher in patients with PCOS and 16% higher in their unaffected siblings.[14] In an Indian study from Kashmir, psychiatric morbidity was assessed using a structured interview by a psychiatrist. This study showed a high prevalence of almost all psychiatric disorders as compared to the control group. A higher prevalence of depression, anxiety disorders and suicidality was observed (depressive disorder 23.6%, generalized anxiety disorder 15.45% and suicidality 8.18%).[15] A meta-analysis by Brutocau et al.[16] has demonstrated that women with PCOS were at an increased risk of diagnosis of depression (odds ratio (OR), 2.79; 95% CI, 2.23–3.50), anxiety (OR, 2.75; 95% CI, 2.10–3.60), bipolar disorder (OR, 1.78; 95% CI, 1.43–2.23) and obsessive–compulsive disorder (OCD) (OR, 1.37; 95% CI 1.22–1.55); however, social phobia or panic disorder was not observed.
Social comorbidity
Physical manifestations of PCOS such as hirsutism, obesity, acne and infertility can have a negative effect on the patients’ social life. A cross-sectional study of 128 women with PCOS reported weight gain, infertility and hyperandrogenism as their greatest concerns and showed lower scores on the PCOS questionnaire (PCOSQ) subscale for weight and infertility, while hirsute women reported higher scores on the PCOSQ for emotions subscale, including mood disorders, anxiety, depression and low self-esteem.[17] Emotional and social functioning were the most affected domains rather than physical functioning.[18] Likewise, adolescents too were highly affected due to overweight and body perception, leading to bullying, social isolation and low health-related QoL. Another qualitative study conducted on Iranian adolescents suggested that attractiveness and threat to femininity were their main concerns and understanding these apprehensions can help HCPs in treating them.
A randomized controlled trial of 88 women demonstrated that 40% felt uncomfortable in social situations, 30% had high levels of depression, while 75% reported clinical levels of anxiety and 29% reported both.[19] A community-based cohort study conducted on 8,467 participants showed that women with PCOS had a higher prevalence of eating disorders (11.0% vs. 7.6%), low self-esteem (31.7% vs. 24.2%) and psychological distress (21.0% vs. 13.5%).[20] A population-based study conducted at ages 31 and 46 in women with PCOS showed a lowered health-related QoL with mental distress, low life satisfaction and poor health comparable to that of women with other chronic conditions, such as asthma, migraine, rheumatoid arthritis and depression.[21]
Sexual dysfunction, self-image and self-esteem
Pieces of evidence support that negative self-image and lowered self-esteem are common issues in patients with PCOS. Findings from a systematic review by Jones et al.[22] showed that the most adversely affected domain was weight and the least one was acne. A cross-sectional study in women with PCOS showed moderate sexual dysfunction, but feelings of insufficiency in social and sexual situations were distinctly raised and positively associated with hirsutism and depression.[23] An Iranian study of 400 women showed impaired self-confidence in PCOS groups in comparison with the non-PCOS group indicating imperative psychological attention and support.[24] Himelein et al.[25] suggests that women with PCOS may struggle with sexual discomfort or disinterest, perhaps as a result of concerns about sexual attractiveness. Cultural factors play an important role in the perception of self, thus affecting self-esteem. Among Brazilian women with PCOS, weight was not found to be as detrimental to self-esteem as in comparison with Austrian women. This finding attributed to the greater importance of thinness in Western countries than in developing countries.[26]
Eating disorders and disordered eating
Body dissatisfaction is widely accepted to play an important causal role in eating disorders. Eating disorders include anorexia nervosa, bulimia nervosa and binge eating, and disordered eating refers to symptoms influenced by behavioural, mental and emotional features. Although highly prevalent in patients with PCOS, inadequate screening methods make it vulnerable to remain under-diagnosed, thus affecting the physical health and psychological well-being of women. Thannickal et al.[27] analysed 36 studies involving 349,529 patients with PCOS reporting to have bulimia nervosa, binge eating or any other eating disorder, but not anorexia nervosa. Mixed results were observed across different eating disorders, but the overall occurrence is high in women with PCOS.[27]
Section 3: Clinical assessment and counselling
Screening, assessment and counselling are the core pillars that are pivotal to detect, prevent and treat physiological and psychological issues associated with PCOS. Patient counselling is a broad process, which comprises advising and educating the patients as well as their family about all the necessary medication-related information, lifestyle modifications and addressing psychological factors to enhance QoL. Effective counselling is important, since it improves patients’ understanding and knowledge about PCOS, resulting in improved medication adherence and better outcomes.
The strength-based counselling and motivational interviewing involve the recording of psychosocial history in adolescents and adult women, imperative to identify the concerned areas in them as well as to recognize the strengths and ambitions in adolescents.[6] An intervention initiated with counselling for psychological and socio-sexual issues will empower the release of emotional distress, develop positive relationship patterns with healthy behaviour and complement patient care.[28]
School sessions provide knowledge about PCOS, empowering girls to be assertive and protecting their self-esteem. The psychological factors may impede the application of lifestyle modification in situations such as asking a girl to exercise, without considering the embarrassments she might have to face in the gym. Hence, the biological, psychological, social and environmental factors need to be considered while counselling, focusing on the holistic approach. All the clinical symptoms do not have the same impact on the patients; thus, counselling depends on the symptoms presented, medications prescribed and age or both medications and age [Table 1]. The nutritional and genetic aspects (such as a family history of metabolic diseases, infertility or menstrual problems, etc.) need to be focused on along with the involvement of family and peer groups. Specific counselling may include fertility issues, risk of diabetes, risk of endometrial carcinoma and future risk of cardiovascular disease.
Table 1.
Counselling according to phase of life
| Phases of life | Hygiene and non-pharmacological therapy | Medication and interventional therapy | Counselling/other interventions |
|---|---|---|---|
| Adolescents | Skin hygiene to reduce acne; healthy lifestyle to maintain optimal weight; support to handle social challenges such as bullying and teasing | Contraindications, expected benefits, possible adverse effects, anticipated limitations and caveats related to laser treatment and medical therapy | Adolescent-centred interview; 360º assessment of significant symptoms, including family members and other caregivers; focus on self-esteem and self-image, assertiveness training and problem-solving skills |
|
| |||
| Reproductive age | |||
|
| |||
| No pregnancy | Skin hygiene; healthy lifestyle to maintain optimal weight; contraceptive counselling | Use of menstrual regulations for hirsutism as well as counselling | Focus on sexual health, self-esteem self-image and problem-solving skills if needed |
| Planning pregnancy | Skin hygiene; healthy lifestyle; pre-conception counselling | Avoidance of menstrual regulators, drugs with teratogenic potential, use of folic acid | Fertility-related counselling, e.g., explanation of fertile, period, rational use of pregnancy tests; psychosocial and family support |
| Menopause and post-menopause | Functional foods and non-pharmacological therapy for hot flashes; cosmetic therapy for hirsutism and alopecia; Screening for metabolic syndrome | Appropriate therapy for metabolic dysfunction, osteoporosis, estrogenic symptoms | Person-centred advice; family support |
A standardized pre-conceptional counselling regarding nutrition, vitamin supplementation and vaccinations play a key role in managing PCOS. The literature reports that adolescent girls and women with PCOS after nutritional counselling and complying with lifestyle interventions experienced improved clinical, metabolic and hormonal parameters.[29,30] Exercise in groups followed by counselling showed beneficial effects on waist circumference, weight and VO2 max in women with PCOS.[31] In this randomized study, 17 sedentary, overweight women with PCOS underwent 16 weeks of intervention and 8 weeks of high-intensity aerobic exercise followed by 8 weeks of group counselling. Rubella vaccination can be discussed if IgG is negative.
The questionnaire-based survey in women enabled early detection of PCOS, identification of phenotypes and referral to standard primary health care.[32] A systematic review suggested that PCOSQ and the SF-36 were used most frequently for the assessment of QoL in women with PCOS and were able to capture different aspects of QoL and identified the areas that can improve QoL in them.[33] Table 2 depicts some of the counselling techniques for adolescent and adult women affected with PCOS.
Table 2.
Counselling techniques for adolescent and adult women affected with PCOS
| CARES characteristics of a good health care provider | Water approach for motivational interviewing |
|---|---|
| C=Confident competence | W=Welcome warmly |
| A=Authentic accessibility | A=Ask and assess |
| R=Reciprocal respect | T=Tell truthfully |
| E=Expressive empathy | E=Explain with empathy |
| S=Straightforward simplicity | R=Reassure and return |
|
| |
| SMART technique for goal setting and self-monitoring | BATHE technique for clinical evaluation[34] |
|
| |
| S=Specific | B=Background (sociocultural) |
| M=Measurable | A=Affect (depressed/anxious mood) |
| A=Achievable | T=Trouble (predominant symptom causing problem) |
| R=Realistic | H=Handling (coping with problems) |
| T=Timely | E=Empathy (understanding and support) |
|
| |
| HEADSSS assessment for adolescents[35] | CRAFFT questions for obtaining drug history[36] |
|
| |
| H=Home and environment | C=Car (driving history using alcohol or drugs) |
| E=Education and employment | R=Relax (use of alcohol or drugs to relax) |
| E=Eating | A=Alone (use of alcohol or drugs when alone) |
| A=Activity or employment | F=Forget (forget things done while using alcohol or drugs) |
| D=Drugs | F=Friends/family (told by friends or family to cut down on drinking or drug use) |
| S=Suicidality | T=Trouble (getting into trouble while using alcohol or drugs) |
| S=Sex | |
| S=Safety | |
Physicians play a key role in creating awareness in adolescents and their parents about patterns of the menstrual cycle, since any menstrual abnormalities signal the need for medical testing and early treatment. However, several women complain about insufficient information obtained from the HCPs and negative experiences in relation to the diagnosis and management of PCOS reporting dissatisfaction with the provision of care and support.[18,37] A 2018 study revealed that women with PCOS had greater distrust and arguments in the opinions of their HCPs as compared to women without PCOS impacting the HCP’s efficiency of employing lifestyle interventions.[38]
Further research is essential to recognize and implement myriad ways to improve communication between adolescents and adult women with PCOS and their HCPs [Figure 3].[18] Even though clinicians have a major role in managing patients with PCOS, challenges do exist at patients’ and clinicians’ end [Boxs 3 and 4]. However, necessarily adopting a few strategies and principles would enable them to deal with PCOS satisfactorily and lessen the gaps existing in clinical practice [Box 5].
Figure 3.
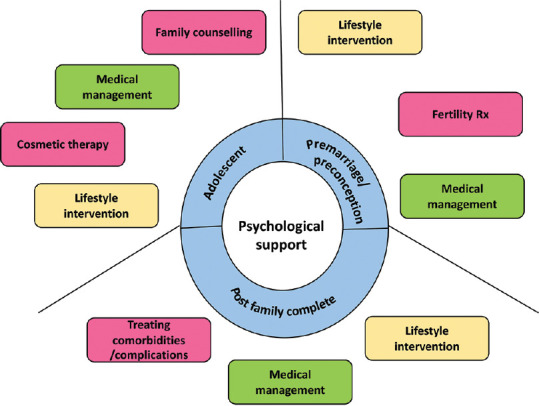
Psychosocial support and counselling
Box 3.
Barriers for PCOS treatment
| Insufficient knowledge and information provided to the patients |
| Lack of communication |
| Financial burden |
| Environmental and time barriers |
| Personal barriers including low self-confidence and shyness |
| Long waiting times for allied health care providers |
| Clinicians’ perception of patient access to and the availability of allied health professionals |
| Short consultations, non-standardized delivery of lifestyle management, lack of enforcement and follow-up of interventions |
Box 4.
Patient management strategies
| Identifying factors associated with psychological disorders and timely management |
| Recognize personal impediments |
| Observe and interpret non-verbal communications such as eye contact, facial expressions and body language |
| Motivate patient and restore self-esteem |
Box 5.
Clinician’s role
| Have clear communication with sufficient time |
| Avoid medical jargon |
| Tailor therapy as per patient’s symptoms |
| Explain treatment options |
| Engage patient in her treatment plan and ensure that it is understood properly |
| Provide age-appropriate educational materials |
| Be supportive, empathetic, do not shame or scare the patient |
| Consider cultural and linguistic aspects |
| Empower patient with positive attitude |
| Include caregiver or family member, parents or mother and peer group in conversation |
| Abide by ethical principles such as informed consent and confidentiality |
Section 4: Management of PCOS and associated co-morbidities [Figure 4, Box 6]
Figure 4.
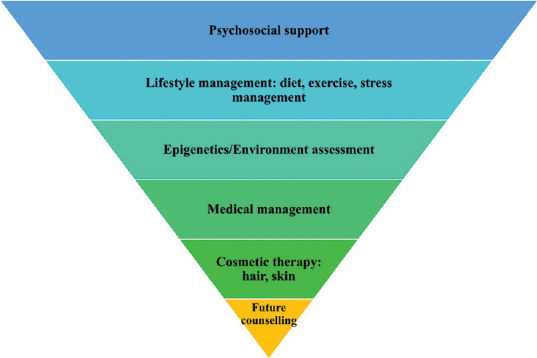
Treatment strategies used for PCOS
Box 6.
Management of PCOS
| A collaborative team approach comprising subspecialist physicians, gynaecologists, obstetricians, dermatologists and psychiatrists is needed for PCOS management. |
| Counselling is the centrepiece for dealing with patients of various age groups having PCOS. |
| Medicines, nutritional supplements, diet, exercise and other specific tools and techniques of counselling collectively form the basis of managing PCOS and related co-morbidities. |
A team comprising primary HCPs, subspecialist physicians, gynaecologists, obstetricians, dermatologists and psychiatrists is desirable to tailor the therapy as per the patient’s clinical presentations, complications and co-morbidities for managing PCOS. The therapeutic goals majorly involve treating the underlying symptoms such as cosmetic, infertility, physical and psychosocial issues. Several tools and interventions exist for the overall management of PCOS including non-pharmacological and pharmacological strategies; some of them are listed in Table 3.
Table 3.
Multiple co-morbidities associated with PCOS
| Co-morbidities | Tests/tools used for assessment | Treatment |
|---|---|---|
|
| ||
| Biomedical co-morbidities | ||
| Obesity | Body mass index, waist circumference, DEXA | Lifestyle modifications comprising a balanced diet, exercise and stress management, yoga and holistic approach, anti-obesity drugs, bariatric surgery[39] |
| Obstructive sleep apnoea | Polysomnography, Berlin tool, sleep questionnaire | Continuous positive airway pressure, oral appliances, surgical methods and weight loss[40] |
| Metabolic syndrome | Waistline, blood pressure, HDL cholesterol level, triglyceride level and fasting plasma glucose | Lifestyle modifications[41] |
| Insulin resistance | Glucose tolerance test | Thiazolidinediones, metformin and vitamin D[42] |
| Type 2 diabetes mellitus | Glycated haemoglobin (HbA1C) test | Lifestyle modifications, insulin and oral anti-hyperglycaemics[43] |
| Infertility | Full workup | In vitro fertilization lifestyle interventions, pharmacotherapy (metformin, clomiphene citrate, progestins) and surgical approach[44] |
| Dyslipidaemia | Lipid profile | Lifestyle modifications, lipid lowering agents such as statins, ω-3 polyunsaturated fatty acid and nicotinic acid[45] |
| Hypertension | Blood pressure | Lifestyle modifications |
| Cardiovascular disease | ECG, stress test | Lifestyle modifications[6] |
|
| ||
| Cosmetic co-morbidities | ||
|
| ||
| Hirsutism | Ferriman–Gallwey score | Oral contraceptives, eflornithine, cosmetic therapy, laser treatment[6] |
| Acne | Tutakne et al. (grades 1, 2, 3, 4)[46] | Oral contraceptives, anti-androgens, retinoids |
| Alopecia | Ludwig’s classification of hair loss[47] | Oral contraceptives, spironolactone, minoxidil |
|
| ||
| Psychiatric/psychosocial co-morbidities | ||
|
| ||
| Anxiety | The State-Trait Anxiety Inventory (STAI),[48] Hospital Anxiety and Depression Scale (HADS)[49] | Lifestyle modifications, counselling, cognitive–behavioural therapies, medications to treat physical, cosmetic health issues, psychological and psychiatric disorders, relaxation therapy (mindfulness, yoga), group therapy |
| Depression | Patient Health Questionnaire 2 (PHQ-2), Patient Health Questionnaire 9 (PHQ-9),[50,51] Hospital Anxiety and Depression Scale (HADS),[49] Beck’s Depression Inventory (BDI)[52] | |
| Psychosexual dysfunction | Female Sexual Function Index (FSFI)[53] | |
| Body image | Multidimensional Body-Self Relations Questionnaire (MBSRQ) | |
| Eating disorders | SCOFF tool (Sick, Control, One stone, Fat, Food)[54] | |
| Impaired quality of life | PCOS quality-of-life tool (PCOSQ), or the modified PCOSQ,[55] World Health Organization Quality of Life Instrument (WHOQOL-BREF)[56] | |
DEXA, dual-energy X-ray absorptiometry; ECG, electrocardiogram; HDL, high-density lipoprotein
More than 50% of the women with PCOS are insulin-resistant and have a higher risk of developing type 2 diabetes, abdominal obesity and dyslipidaemia. Medicines, nutritional supplements, diet, exercise and other specific tools and techniques of counselling collectively form the basis of managing PCOS and related co-morbidities. Studies have shown beneficial effects of vitamin or mineral supplements and vitamin-like nutrients such as bioflavonoids, alpha-lipoic acid, carnitine, omega-3 fatty acids, probiotics on PCOS-related symptoms and associated co-morbidities.[57] The behavioural and psychological interventions along with social support are able to bring out positive outcomes in controlling weight and managing obesity. Counselling women and adolescents belonging to various age groups about change in lifestyle is the foremost step in the management of obese PCOS, insulin resistance, infertility, psychological disorders and OSA. The literature shows that weight problems have the greatest negative impact on QoL of patients with PCOS, and studies have shown that patients with lower BMI have slightly lower anxiety and depression scores.[16] Lack of initiative, interest and perseverance will exist due to psychological problems. This may impact lifestyle management which is the cornerstone of PCOS therapy. Hence, to achieve optimal results, it is imperative to deal with psychological issues in PCOS.
Section 5: Role of media and digital technology in PCOS [Box 7]
Box 7.
Media and digital technology in PCOS
| Digital technology is a powerful support tool enabling remote patient monitoring, counselling and managing health status using telemedicine and wellness tools. |
| The digital versions of psychotherapy and robotic technology are gaining importance to address the psychosocial problems. |
| PCOS support groups provide socio-emotional support to women with PCOS to alleviate distress, empower and enhance self-management. |
Although PCOS is a highly prevalent disorder, it is characterized by a lack of awareness and knowledge about this syndrome. Easy access to the Internet and cell phones has given women and adolescents a platform to search for information about PCOS. Moreover, the Internet allows women to conveniently communicate and privately access and share experiences through emails, online support groups and social networking sites. However, the authenticity and accuracy of online information need to be validated by HCPs and scientific researchers so that patients of all age groups can use it relentlessly.
Internet and social media intensely impact the lives of adolescents depending on how they manage their health, and equating it with beauty might be problematic for them. For instance, teen magazines or blogs may illustrate hair removal methods, instant therapies for acne, ketogenic diet, or quick-fix diet and exercise, disregarding the importance of long-term lifestyle modifications, medical treatment and psychosocial support essential for managing PCOS symptoms and co-morbidities.[58] The ketogenic diet has been shown to reduce weight and improve insulin sensitivity; however, its long-term effects have not been studied.[59] Conversely, a ketogenic diet can worsen PCOS symptoms due to the physiological stress exerted on the body by low carbohydrate content. Hence, it is very important for adolescents and women to seek medical help and counselling rather than adopting several instant lifestyle alterations and therapies from online PCOS information without being aware of the downsides. Also, during counselling, the HCP should understand and identify whether the patient has used or misused social media and online information about PCOS that could be a guide to decide the appropriate therapeutic option for the patients.
Several digital tools have been introduced impacting the health care, much beyond just curtailing the consultation waiting time and expenses. Digital technology is a powerful support tool enabling remote patient monitoring, counselling and managing health status using telemedicine and wellness tools. Digital screening, assessment, psychotherapies and behavioural therapy are gaining wide acceptance among clinicians and patients.[60,61] Well-developed digital interventions do exist, particularly for cognitive and behavioural treatments,[62] and some clinical studies are underway involving the Internet and computer gameplay.[63] The digital versions of psychotherapy include acceptance and commitment therapy, behavioural activation, interpersonal psychotherapy, mindfulness interventions and problem-solving therapy. An Indian study reported the benefits of digital therapeutics in girls with PCOS using a wellness application, which improved patient engagement and treatment adherence in them.[64]
Recently, PCOS support groups have been established to provide emotional and social support to such women to alleviate distress, empower and enhance self-management. Studies show that numerous international, English-speaking PCOS support groups exist and have an online presence.[65] Currently, in India, PCOS support groups such as LOQUS,[66] Conquer PCOS,[67] PCOS support by geneOmbio Technologies,[68] HEAL PCOS,[69] etc., are known to provide informational and socio-emotional support to patients with PCOS. They are actively involved in PCOS awareness programs and help women to overcome PCOS symptoms. Such support groups in collaboration with HCPs and professional societies can improve the accessibility of evidence-based data. All HCPs should endorse PCOS support groups and refer patients to them.
CONCLUSION
Counselling is an integral part of PCOS management and every HCP should be aware of it. The optimum patient counselling would enable overall enhanced clinical outcomes and patient satisfaction. The application of patient-friendly clinical and psychological health and cosmetology counselling facilities by an interdisciplinary health care team will support adolescents, adult women and their families to live with and not suffer from PCOS. A positive association between psychological and health-related QoL brings forth that better psychiatric screening, diagnosis and access to treatment could improve QoL for women with PCOS. The need for research on the most effective treatment and longitudinal monitoring strategies for women with co-morbid PCOS is warranted.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERRENCES
- 1.Kitzinger C, Willmott J. 'The thief of womanhood':Women's experience of polycystic ovarian syndrome. Soc Sci Med. 2002;54:349–61. doi: 10.1016/s0277-9536(01)00034-x. [DOI] [PubMed] [Google Scholar]
- 2.Zawadzki J, Dunaif A. Diagnostic criteria for polycystic ovary syndrome:Towards a rational approach. In: Dunaif A, Givens HR, Haseltine FP, Merriam GR, editors. Polycystic Ovary Syndrome. Boston, MA: Blackwell Scientific; 1992. pp. 377–84. [Google Scholar]
- 3.Gainder S, Sharma B. Update on management of polycystic ovarian syndrome for dermatologists. Indian Dermatol Online J. 2019;10:97–105. doi: 10.4103/idoj.IDOJ_249_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lujan ME, Chizen DR, Pierson RA. Diagnostic criteria for polycystic ovary syndrome:Pitfalls and controversies. J Obstet Gynaecol Can. 2008;308:671–9. doi: 10.1016/S1701-2163(16)32915-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fauser BC, Tarlatzis BC, Rebar RW, Legro RS, Balen AH, Lobo R, et al. Consensus on women's health aspects of polycystic ovary syndrome (PCOS):The Amsterdam ESHRE/ASRM-Sponsored 3rd PCOS Consensus Workshop Group. Fertil Steril. 2012;97:28–38. e25. doi: 10.1016/j.fertnstert.2011.09.024. [DOI] [PubMed] [Google Scholar]
- 6.Teede H, Deeks A, Moran L. Polycystic ovary syndrome:A complex condition with psychological, reproductive and metabolic manifestations that impacts on health across the lifespan. BMC Med. 2010;8:41. doi: 10.1186/1741-7015-8-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Goodarzi MO, Carmina E, Azziz R. DHEA, DHEAS and PCOS. J Steroid Biochem Mol Biol. 2015;145:213–25. doi: 10.1016/j.jsbmb.2014.06.003. [DOI] [PubMed] [Google Scholar]
- 8.Moran C, Arriaga M, Arechavaleta-Velasco F, Moran S. Adrenal androgen excess and body mass index in polycystic ovary syndrome. J Clin Endocrinol Metab. 2015;100:942–50. doi: 10.1210/jc.2014-2569. [DOI] [PubMed] [Google Scholar]
- 9.Sheehan MT. Polycystic ovarian syndrome:Diagnosis and management. Clin Med Res. 2004;2:13–27. doi: 10.3121/cmr.2.1.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bharathi R, Swetha S, Neerajaa J, Madhavica J, Janani D, Rekha SN, et al. An epidemiological survey:Effect of predisposing factors for PCOS in Indian urban and rural population. Middle East Fertil Soc J. 2017;22:313–6. [Google Scholar]
- 11.Bazarganipour F, Ziaei S, Montazeri A, Foroozanfard F, Kazemnejad A, Faghihzadeh S. Psychological investigation in patients with polycystic ovary syndrome. Health Qual Life Outcomes. 2013;11:141. doi: 10.1186/1477-7525-11-141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Weiner CL, Primeau M, Ehrmann DA. Androgens and mood dysfunction in women:Comparison of women with polycystic ovarian syndrome to healthy controls. Psychosom Med. 2004;66:356–62. doi: 10.1097/01.psy.0000127871.46309.fe. [DOI] [PubMed] [Google Scholar]
- 13.Sundararaman PG, Shweta, Sridhar GR. Psychosocial aspects of women with polycystic ovary syndrome from south India. J Assoc Physicians India. 2008;56:945–8. [PubMed] [Google Scholar]
- 14.Cesta CE, Månsson M, Palm C, Lichtenstein P, Iliadou AN, Landén M. Polycystic ovary syndrome and psychiatric disorders:Co-morbidity and heritability in a nationwide Swedish cohort. Psychoneuroendocrinology. 2016;73:196–203. doi: 10.1016/j.psyneuen.2016.08.005. [DOI] [PubMed] [Google Scholar]
- 15.Hussain A, Chandel RK, Ganie MA, Dar MA, Rather YH, Wani ZA, et al. Prevalence of psychiatric disorders in patients with a diagnosis of polycystic ovary syndrome in Kashmir. Indian J Psychol Med. 2015;37:66–70. doi: 10.4103/0253-7176.150822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Brutocao C, Zaiem F, Alsawas M, Morrow AS, Murad MH, Javed A. Psychiatric disorders in women with polycystic ovary syndrome:A systematic review and meta-analysis. Endocrine. 2018;62:318–25. doi: 10.1007/s12020-018-1692-3. [DOI] [PubMed] [Google Scholar]
- 17.McCook JG, Reame NE, Thatcher SS. Health-related quality of life issues in women with polycystic ovary syndrome. J Obstet Gynecol Neonatal Nurs. 2005;34:12–20. doi: 10.1177/0884217504272945. [DOI] [PubMed] [Google Scholar]
- 18.Jones GL, Hall JM, Lashen HL, Balen AH, Ledger WL. Health-related quality of life among adolescents with polycystic ovary syndrome. J Obstet Gynecol Neonatal Nurs. 2011;40:577–88. doi: 10.1111/j.1552-6909.2011.01279.x. [DOI] [PubMed] [Google Scholar]
- 19.Lipton MG, Sherr L, Elford J, Rustin MH, Clayton WJ. Women living with facial hair:The psychological and behavioral burden. J Psychosom Res. 2006;61:161–8. doi: 10.1016/j.jpsychores.2006.01.016. [DOI] [PubMed] [Google Scholar]
- 20.Tay CT, Teede HJ, Hill B, Loxton D, Joham AE. Increased prevalence of eating disorders, low self-esteem, and psychological distress in women with polycystic ovary syndrome:A community-based cohort study. Fertil Steril. 2019;112:353–61. doi: 10.1016/j.fertnstert.2019.03.027. [DOI] [PubMed] [Google Scholar]
- 21.Karjula S, Morin-Papunen L, Franks S, Auvinen J, Järvelin MR, Tapanainen JS, et al. Population-based data at ages 31 and 46 show decreased HRQoL and life satisfaction in women with PCOS symptoms. J Clin Endocrinol Metab. 2020;105:1814–26. doi: 10.1210/clinem/dgz256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jones GL, Hall JM, Balen AH, Ledger WL. Health-related quality of life measurement in women with polycystic ovary syndrome:A systematic review. Hum Reprod Update. 2008;14:15–25. doi: 10.1093/humupd/dmm030. [DOI] [PubMed] [Google Scholar]
- 23.Fliegner M, Richter-Appelt H, Krupp K, Brunner F. Sexual function and socio-sexual difficulties in women with polycystic ovary syndrome (PCOS) Geburtshilfe Frauenheilkd. 2019;79:498–509. doi: 10.1055/a-0828-7901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Amini L, Valian K, Sdeghi Avvalshahr H, Montaeri A. Self-Confidence in women with and without polycystic ovary syndrome. J Family Reprod Health. 2014;8:113–6. [PMC free article] [PubMed] [Google Scholar]
- 25.Himelein MJ, Thatcher SS. Polycystic ovary syndrome and mental health:A review. Obstet Gynecol Surv. 2006;61:723–32. doi: 10.1097/01.ogx.0000243772.33357.84. [DOI] [PubMed] [Google Scholar]
- 26.Hashimoto DM, Schmid J, Martins FM, Fonseca AM, Andrade LH, Kirchengast S, et al. The impact of the weight status on subjective symptomatology of the polycystic ovary syndrome:A cross-cultural comparison between Brazilian and Austrian women. Anthropol Anz. 2003;61:297–310. [PubMed] [Google Scholar]
- 27.Thannickal A, Brutocao C, Alsawas M, Morrow A, Zaiem F, Murad MH, et al. Eating, sleeping and sexual function disorders in women with polycystic ovary syndrome (PCOS):A systematic review and meta-analysis. Clin Endocrinol (Oxf) 2020;92:338–49. doi: 10.1111/cen.14153. [DOI] [PubMed] [Google Scholar]
- 28.Nickel R, Ademmer K, Egle UT. Manualized psychodynamic interactional group therapy for the treatment of somatoform pain disorders. Bull Menninger Clin. 2010;74:219–37. doi: 10.1521/bumc.2010.74.3.219. [DOI] [PubMed] [Google Scholar]
- 29.Abdolahian S, Tehrani FR, Amiri M, Ghodsi D, Yarandi RB, Jafari M, et al. Effect of lifestyle modifications on anthropometric, clinical, and biochemical parameters in adolescent girls with polycystic ovary syndrome:A systematic review and meta-analysis. BMC Endocr Disord. 2020;20:71. doi: 10.1186/s12902-020-00552-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kim CH, Chon SJ, Lee SH. Effects of lifestyle modification in polycystic ovary syndrome compared to metformin only or metformin addition:A systematic review and meta-analysis. Sci Rep. 2020;10:7802. doi: 10.1038/s41598-020-64776-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Roessler KK, Birkebaek C, Ravn P, Andersen MS, Glintborg D. Effects of exercise and group counselling on body composition and VO2 max in overweight women with polycystic ovary syndrome. Acta Obstet Gynecol Scand. 2013;92:272–7. doi: 10.1111/aogs.12064. [DOI] [PubMed] [Google Scholar]
- 32.Kumarapeli V, Seneviratne Rde A, Wijeyaratne CN, Yapa RM, Dodampahala SH. A simple screening approach for assessing community prevalence and phenotype of polycystic ovary syndrome in a semi-urban population in Sri Lanka. Am J Epidemiol. 2008;168:321–8. doi: 10.1093/aje/kwn137. [DOI] [PubMed] [Google Scholar]
- 33.Behboodi Moghadam Z, Fereidooni B, Saffari M, Montazeri A. Measures of health-related quality of life in PCOS women:A systematic review. Int J Womens Health. 2018;10:397–408. doi: 10.2147/IJWH.S165794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Poon V. Short counseling techniques for busy family doctors. Can Fam Physician. 1997;43:705–13. [PMC free article] [PubMed] [Google Scholar]
- 35.Katzenellenbogen R. HEADSS:The “Review of Systems”for adolescents. Virtual Mentor. doi: 10.1001/virtualmentor.2005.7.3.cprl1-0503. 2005;7:Virtualmentor. 2005.7.3.cprl1-0503. doi:10.1001/virtualmentor.2005.7.3.cprl1-0503. [DOI] [PubMed] [Google Scholar]
- 36.Knight JR, Sherritt L, Shrier LA, Harris SK, Chang G. Validity of the CRAFFT substance abuse screening test among adolescent clinic patients. Arch Pediatr Adolesc Med. 2002;156:607–14. doi: 10.1001/archpedi.156.6.607. [DOI] [PubMed] [Google Scholar]
- 37.Tomlinson J, Pinkney J, Adams L, Stenhouse E, Bendall A, Corrigan O, et al. The diagnosis and lived experience of polycystic ovary syndrome:A qualitative study. J Adv Nurs. 2017;73:2318–26. doi: 10.1111/jan.13300. [DOI] [PubMed] [Google Scholar]
- 38.Lin AW, Bergomi EJ, Dollahite JS, Sobal J, Hoeger KM, Lujan ME. Trust in physicians and medical experience beliefs differ between women with and without polycystic ovary syndrome. J Endocr Soc. 2018;2:1001–9. doi: 10.1210/js.2018-00181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Legro RS. Obesity and PCOS:Implications for diagnosis and treatment. Semin Reprod Med. 2012;30:496–506. doi: 10.1055/s-0032-1328878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Pavwoski P, Shelgikar AV. Treatment options for obstructive sleep apnea. Neurol Clin Pract. 2017;7:77–85. doi: 10.1212/CPJ.0000000000000320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Mahalingaiah S, Diamanti-Kandarakis E. Targets to treat metabolic syndrome in polycystic ovary syndrome. Expert Opin Ther Targets. 2015;19:1561–74. doi: 10.1517/14728222.2015.1101067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Łagowska K, Bajerska J, Jamka M. The role of vitamin D oral supplementation in insulin resistance in women with polycystic ovary syndrome:A systematic review and meta-analysis of randomized controlled trials. Nutrients. 2018;10:1637. doi: 10.3390/nu10111637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Forslund M, Landin-Wilhelmsen K, Trimpou P, Schmidt J, Brännström M, Dahlgren E. Type 2 diabetes mellitus in women with polycystic ovary syndrome during a 24-year period:Importance of obesity and abdominal fat distribution. Hum Reprod Open. 2020;2020:hoz042. doi: 10.1093/hropen/hoz042. doi:10.1093/hropen/hoz042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Teede HJ, Misso ML, Deeks AA, Moran LJ, Stuckey BG, Wong JL, et al. Assessment and management of polycystic ovary syndrome:Summary of an evidence-based guideline. Med J Aust. 2011;195:S65–112. doi: 10.5694/mja11.10915. [DOI] [PubMed] [Google Scholar]
- 45.Liu Q, Xie YJ, Qu LH, Zhang MX, Mo ZC. Dyslipidemia involvement in the development of polycystic ovary syndrome. Taiwan J Obstet Gynecol. 2019;58:447–53. doi: 10.1016/j.tjog.2019.05.003. [DOI] [PubMed] [Google Scholar]
- 46.Tutakne MA, Chari KVR. Acne, rosacea and perioral dermatitis. In: Valia RG, Valia AR, editors. IADVL Textbook and Atlas of Dermatology. 2nd ed. Mumbai: Bhalani publishing House; 2003. pp. 689–710. [Google Scholar]
- 47.Ludwig E. Classification of the types of androgenetic alopecia (common baldness) occurring in the female sex. Br J Dermatol. 1977;97:247–54. doi: 10.1111/j.1365-2133.1977.tb15179.x. [DOI] [PubMed] [Google Scholar]
- 48.Spielberger CD, Vagg PR. Psychometric properties of the STAI:A reply to Ramanaiah, Franzen, and Schill. J Pers Assess. 1984;48:95–7. doi: 10.1207/s15327752jpa4801_16. [DOI] [PubMed] [Google Scholar]
- 49.Snaith RP. The hospital anxiety and depression scale. Health Qual Life Outcomes. 2003;1:29. doi: 10.1186/1477-7525-1-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Richardson LP, Rockhill C, Russo JE, Grossman DC, Richards J, McCarty C, et al. Evaluation of the PHQ-2 as a brief screen for detecting major depression among adolescents. Pediatrics. 2010;125:e1097–103. doi: 10.1542/peds.2009-2712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Kroenke K, Spitzer RL, Williams JB. The PHQ-9:Validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606–13. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.García-Batista ZE, Guerra-Peña K, Cano-Vindel A, Herrera-Martínez SX, Medrano LA. Validity and reliability of the Beck Depression Inventory (BDI-II) in general and hospital population of Dominican Republic. PLoS One. 2018;13:e0199750. doi: 10.1371/journal.pone.0199750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Rosen R, Brown C, Heiman J, Leiblum S, Meston C, Shabsigh R, et al. The Female Sexual Function Index (FSFI):A multidimensional self-report instrument for the assessment of female sexual function. J Sex Marital Ther. 2000;26:191–208. doi: 10.1080/009262300278597. [DOI] [PubMed] [Google Scholar]
- 54.Morgan JF, Reid F, Lacey JH. The SCOFF questionnaire:A new screening tool for eating disorders. West J Med. 2000;172:164–5. doi: 10.1136/ewjm.172.3.164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Holland JC, Kash KM, Passik S, Gronert MK, Sison A, Lederberg M, et al. A brief spiritual beliefs inventory for use in quality-of-life research in life-threatening illness. Psychooncology. 1998;7:460–9. doi: 10.1002/(SICI)1099-1611(199811/12)7:6<460::AID-PON328>3.0.CO;2-R. [DOI] [PubMed] [Google Scholar]
- 56.WHOQOL-BREF. [Last accessed on 2021 Jan 25]. Available from: https://www.who.int/mental_health/media/en/76.pdf .
- 57.Günalan E, Yaba A, Yılmaz B. The effect of nutrient supplementation in the management of polycystic ovary syndrome-associated metabolic dysfunctions:A critical review. J Turk Ger Gynecol Assoc. 2018;19:220–32. doi: 10.4274/jtgga.2018.0077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Sanchez N, Jones H. “Less than a wife”:A study of polycystic ovary syndrome content in teen and women's digital magazines. J Med Internet Res. 2016;18:e89. doi: 10.2196/jmir.5417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Mavropoulos JC, Yancy WS, Hepburn J, Westman EC. The effects of a low-carbohydrate, ketogenic diet on the polycystic ovary syndrome:A pilot study. Nutr Metab (Lond) 2005;2:35. doi: 10.1186/1743-7075-2-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Fairburn CG, Patel V. The impact of digital technology on psychological treatments and their dissemination. Behav Res Ther. 2017;88:19–25. doi: 10.1016/j.brat.2016.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.A Treatment Improvement protocol using technology-based therapeutic tools in behavioral health services. [Last accessed on 2020 Nov 12]. Available from: https://store.samhsa.gov/sites/default/files/d7/priv/sma15-4924.pdf .
- 62.Andersson G. The internet and CBT:A clinical guide. Boca Raton: CRC Press; 2014. [Google Scholar]
- 63.Iyadurai L, Blackwell SE, Meiser-Stedman R, Watson PC, Bonsall MB, Geddes JR, et al. Preventing intrusive memories after trauma via a brief intervention involving Tetris computer game play in the emergency department:A proof-of-concept randomized controlled trial. Mol Psychiatry. 2018;23:674–82. doi: 10.1038/mp.2017.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Mittal S, Lathia T, Kanade E, Jaykar A, Gulati N, Singal A. The benefits of digital therapeutics on patient reported outcomes in girls with PCOS. Presented at Endocrine Week 2020. Available from: https://www.ffly.in/research/details/the-benefit-of-digital-therapeutics-on-patient-reported-outcomes-in-girls-with-pcos .
- 65.Avery J, Ottey S, Morman R, Cree-Green M, Gibson-Helm M. Polycystic ovary syndrome support groups and their role in awareness, advocacy and peer support:A systematic search and narrative review. Curr Opin Endocr Metab Res. 2020;12:98–104. [Google Scholar]
- 66.PCOS LOQUS. [Last accessed on 2020 Nov 12]. Available from: https://pcosloqus.com/index.php .
- 67.Conquer PCOS. [Last accessed on 2020 Nov 12]. Available from: https://conquerpcos.org/
- 68.PCOS support. [Last accessed on 2020 Nov 12]. Available from: https://www.geneombiotechnologies.com/pcos-support/
- 69.HEAL PCOS. [Last accessed on 2021 Jan 11]. Available from: https://www.fitterfly.in/heal-pcos .


