Abstract
Objective:
To determine whether pelvic floor physical therapy (PFPT) attendance differs based on referring provider specialty and identify factors related to PFPT initiation and completion.
Methods:
IRB-approved retrospective cohort study examining referrals from Female Pelvic Medicine and Reconstructive Surgery (FPMRS) and non-FPMRS providers at a single academic medical center to affiliated PFPT clinics over a 12-month period. Demographics, referring specialty and diagnoses, prior treatment, and details regarding PFPT attendance were collected. Characteristics between FPMRS and non-FPMRS referrals were compared and multivariate logistic regression analyses were performed to identify factors associated with PFPT initiation and completion.
Results:
A total of 497 referrals were placed for PFPT. Compared to non-FPMRS referrals, FPMRS referrals were older (54.7 vs 35.6 years), had higher parity, more were postmenopausal (56% vs 18%), and had Medicare insurance (22% vs 10%) (all p<0.001). Most FPMRS referrals were for urinary incontinence (69% vs 31%), while non-FPMRS referrals were for pelvic pain (70% vs 27%) (both p<0.0001). PFPT attendance was similar in both groups when comparing rates of initiation (47% vs 45%) and completion (13% vs 16%). In multivariate analysis, factors associated with initiation were age ≥ 65 years old, additional therapy provided at referring visit, private insurance, Asian race, pregnant or postpartum at time of referral, and >1 referring diagnosis (all p<0.05). No factors were associated with completion.
Conclusions:
Less than half of referrals to PFPT initiate therapy and only 15% complete PFPT. The populations referred by FPMRS and non-FPMRS providers are different, but ultimately PFPT utilization is similar.
Keywords: pelvic floor disorders, conservative therapy, pelvic floor physical therapy, treatment compliance
Introduction
Pelvic floor muscle exercises (PFME), including use of pelvic floor physical therapy (PFPT), is recommended conservative therapy by professional societies for many pelvic floor disorders (PFD), including urinary incontinence,1,2 fecal incontinence,3,4 pelvic pain,5 painful bladder syndrome,6 and pelvic organ prolapse.7,8 Despite PFME being recognized as first-line therapy for many PFD, there is limited literature on PFPT utilization outside regimented study protocols.
Prior studies demonstrate 65–78% of referred patients will initiate PFPT by attending at least one session, but less than half will ultimately complete their PFPT programs.9–12 Factors associated with lower compliance include greater distance between patients’ home and PFPT site and longer duration between referral and PFPT start date.9 Concurrent initial evaluation of PFD by a Female Pelvic Medicine and Reconstructive Surgery (FPMRS) provider and physical therapist leads to increased PFPT initiation but does not improve PFPT completion.11 Enhanced PFPT counseling does not increase initiation or completion rates.12
Referrals to PFPT may originate from all providers that evaluate and care for women with PFD. This includes providers in Obstetrics & Gynecology, Urology, and Medicine, particularly those with FPMRS training. The specialty of the referring provider may play a critical role in whether patients initiate and complete PFPT. Other factors such as referring diagnoses, insurance status, cost, and prior exposure to physical therapy may also be important in treatment adherence. Prior studies have not examined PFPT referrals from a broad and varied referral base and compared PFPT compliance based on referring provider specialty.
The objective of this study was to determine whether the specialty of the referring provider impacted PFPT initiation and completion for various PFD. We hypothesized that FPMRS referrals would have higher rates of PFPT initiation and completion compared to non-FPMRS referrals. We presumed patients may place more importance and value on PFPT once they have heard comprehensive treatment options from FPMRS providers who they specifically sought out for directive PFD evaluation and management.
Methods
This was an IRB-approved retrospective cohort study of all women referred from the departments of Obstetrics & Gynecology, Urology, and Medicine at an academic medical center to affiliated PFPT clinics over a 12-month period from January 1, 2018 through December 31, 2018. Patients were identified by reviewing all referrals made to our institutional Rehabilitation Services from those departments during the study period and screened for appropriate ICD-10 codes including, but not limited to, female stress urinary incontinence (N39.3), overactive bladder (N32.81), fecal incontinence (R15.9), pelvic pain (R10.2), and vaginal prolapse (N81.10). Two PFPT locations were available to patients: the main academic medical center and a satellite center 3.5 miles away. All physical therapists were female, and their primary focus was pelvic floor disorders. Inclusion criteria was female gender with PFPT referral. Pregnancy at time of referral was permitted and we identified referrals made in the postpartum period, within 6 weeks after delivery. Exclusion criteria included male gender and physical therapy referrals not related to PFD.
Demographics, referring provider specialty and diagnoses, prior treatment for PFD, additional treatment provided at referring visit, history of PFPT or physical therapy for any indication, PFPT attendance, and physical therapist documented symptom assessment and goal achievement were collected. Prior treatment and additional therapy provided at referring visit included appropriate medications, devices such as pessary or dilators, procedures, or surgery based on patient’s PFD. Charts were further reviewed for reasons for not initiating or completing PFPT. Severity of PFD was measured by the Pelvic Floor Distress Inventory-20 (PFDI-20) which was administered at the initial appointment for most patients seen by FPMRS or who attended PFPT. We calculated two time intervals: 1) days from referral to patient contacting PFPT and 2) days from patient contacting PFPT to attendance of first appointment. Out-of-pocket expense was measured as co-pay for each PFPT session. Study data were collected and managed using REDCap (Research Electronic Data Capture) hosted at University of California, Los Angeles.13,14 REDCap is a secure, web-based software platform designed to support data capture for research studies, providing 1) an intuitive interface for validated data capture; 2) audit trails for tracking data manipulation and export procedures; 3) automated export procedures for seamless data downloads to common statistical packages; and 4) procedures for data integration and interoperability with external sources.
We defined providers as either FPMRS or non-FPMRS. FPMRS had sub-specialty training and were in the departments of Obstetrics & Gynecology or Urology. Non-FPMRS were all providers in the departments of Obstetrics & Gynecology, Urology, and Medicine who did not have FPMRS training. We categorized patients into two groups: initiators and non-initiators. Initiators were those who attended at least one PFPT session, while non-initiators did not attend any PFPT. If a patient contacted PFPT to schedule an appointment but did not attend any sessions, she was categorized as a non-initiator. Initiators were further divided into two groups: completers and non-completers. Completers were defined as initiators who were discharged from PFPT, met PFPT goals, or noted sufficient improvement. Non-completers were initiators who did not meet these criteria. PFPT completion did not require attendance of a specific number of sessions.
Univariate comparisons of demographic and clinical characteristics by referring provider specialty and PFPT initiation and completion statuses were performed using Chi-square (or Fisher’s exact if necessary) and Wilcoxon rank-sum tests as appropriate. Multivariate logistic regression analyses were conducted to identify factors associated with a higher likelihood of PFPT initiation and completion. Covariates included in both logistic regression models were chosen a priori as well as variables with p<0.20 from the univariate analyses. For both models, the a priori variables were age, race, and referring provider specialty. All analyses were conducted in SAS 9.4 (Cary, NC).
Results
During the 12-month study period, we identified 497 referrals to PFPT, with 250 referrals from FPMRS and 247 referrals from non-FPMRS (Table 1). Of the referrals from FPMRS, 66% (n=165) were from Obstetrics & Gynecology and 34% (n=85) were from Urology. Non-FPMRS referrals consisted of 92% (n=227) from Obstetrics & Gynecology, 3% (n=8) from Urology, and 5% (n=12) from Medicine. Compared to non-FPMRS referrals, FPMRS referrals were older, had higher parity, were more likely to be postmenopausal, and more likely on Medicare (p<0.001 for all). Referring diagnoses also differed between groups; FPMRS referrals were more likely for urinary incontinence, while non-FPMRS referrals were more likely for pelvic pain (both p<0.0001). Significant differences were seen among other referring diagnoses. Referrals during pregnancy and the postpartum period were almost exclusively made by non-FPMRS (both p<0.001); FPMRS made one referral during pregnancy. FPMRS referrals were less likely to have a history of prior PFPT (p=0.02), but no differences were seen in prior PFD treatment or prior physical therapy for any indication. There was no difference in number of referring diagnoses between groups. FPMRS referrals had more severe PFD based on median PFDI-20 scores (p=0.01). PFDI-20 scores were available for 49% (n=122) of FPMRS and 23% (n=57) of non-FPMRS referrals.
Table 1:
Patient characteristics by FPMRS and Non-FPMRS pelvic floor physical therapy referrals
| Total N=497 | FPMRS n=250 | Non-FPMRS n=247 | p-value | |
|---|---|---|---|---|
| Age, years, median (IQR) | 41.4 (32.8, 60.5) | 54.7 (40.6, 68.3) | 35.6 (30.3, 44.1) | <0.0001 1 |
| Race, % (n) | 0.35 | |||
| Non-Hispanic White | 59% (291) | 58% (144) | 60% (147) | |
| Hispanic | 13% (64) | 12% (31) | 13% (33) | |
| Asian | 12% (62) | 16% (39) | 9% (23) | |
| Black | 5% (26) | 5% (12) | 6% (14) | |
| Other | 6% (30) | 5% (12) | 7% (18) | |
| Unknown | 5% (24) | 5% (12) | 5% (12) | |
| Parity | <0.0001 2 | |||
| 0 | 38% (191) | 29% (72) | 48% (119) | |
| 1 | 19% (96) | 18% (44) | 21% (52) | |
| 2 | 29% (145) | 35% (88) | 23% (57) | |
| 3 | 9% (45) | 13% (32) | 5% (13) | |
| ≥4 | 4% (20) | 6% (14) | 2% (6) | |
| Pregnant at time of referral, % (n) | 3% (16) | 0% (1) | 6% (15) | <0.01 2 |
| Postpartum at time of referral, % (n) | 7% (34) | 0% (0) | 14% (34) | <0.0001 2 |
| Menopausal status, % (n) | <0.0001 | |||
| Premenopausal | 63% (313) | 44% (110) | 82% (203) | |
| Postmenopausal | 37% (184) | 56% (140) | 18% (44) | |
| Insurance, % (n) | <0.001 2 | |||
| Commercial | 82% (409) | 76% (191) | 88% (218) | |
| Medicare | 16% (78) | 22% (54) | 10% (24) | |
| Medi-Cal | 2% (8) | 2% (4) | 2% (4) | |
| Uninsured | 0% (1) | 0% (0) | 0% (1) | |
| Other | 0% (1) | 0% (1) | 0% (1) | |
| Referring diagnosis, % (n) | ||||
| Urinary incontinence | 50% (249) | 69% (173) | 31% (76) | <0.0001 |
| Voiding dysfunction | 4% (21) | 8% (19) | 1% (2) | <0.001 2 |
| IC/PBS | 5% (26) | 6% (14) | 5% (12) | 0.71 |
| Pelvic pain | 48% (239) | 27% (67) | 70% (172) | <0.0001 |
| Pelvic organ prolapse | 8% (42) | 10% (24) | 7% (18) | 0.35 |
| Pelvic floor weakness | 2% (9) | 0% (1) | 3% (8) | 0.02 2 |
| Anal incontinence | 4% (20) | 7% (18) | 1% (2) | <0.001 2 |
| Defecatory dysfunction | 2% (10) | 4% (10) | 0% (0) | <0.01 2 |
| Other | 2% (12) | 2% (6) | 2% (6) | 0.98 |
| Number of referring diagnoses, % (n) | 0.162 | |||
| 1 | 61% (301) | 65% (163) | 56% (138) | |
| 2 | 30% (151) | 28% (69) | 33% (82) | |
| 3 | 7% (36) | 6% (14) | 9% (22) | |
| 4 | 2% (9) | 2% (4) | 2% (5) | |
| Prior PFD treatment, % (n) | 36% (181) | 38% (94) | 35% (87) | 0.58 |
| Prior physical therapy, % (n) | 37% (184) | 38% (96) | 36% (88) | 0.52 |
| Prior pelvic floor physical therapy, % (n) | 11% (56) | 8% (20) | 15% (36) | 0.02 |
| Pre-PFDI-20 score, median (IQR) 3 | 79.2 (47.9, 114.6) | 83.1 (58.3, 116.7) | 62.5 (33.3, 112.5) | 0.01 1 |
| Additional therapy provided at referring visit, % (n) | 46% (231) | 42% (106) | 51% (125) | 0.06 |
| Second referral for PFPT prior to initiating, % (n) | 0.392 | |||
| Yes, FPMRS | 1% (5) | 0% (1) | 2% (4) | |
| Yes, Non-FPMRS | 4% (19) | 4% (9) | 4% (10) |
Wilcoxon rank-sum
Fisher’s exact
More than 10% of sample size missing
Abbreviations: IC/PBS=interstitial cystitis/painful bladder syndrome; PFD=pelvic floor disorder; PFDI=Pelvic Floor Distress Inventory; PFPT=pelvic floor physical therapy; FPMRS=Female Pelvic Medicine and Reconstructive Surgery
There was no difference in rate of PFPT contact (50% vs 48%), initiation (47% vs 45%) or completion (13% vs 16%) between FPMRS and non-FPMRS (Figure 1). In terms of PFPT attendance, 35% of referrals attended ≥3 sessions and 5% attended ≥10 sessions, with no differences noted between referral groups. Median days from referral to contact was shorter for referrals from FPMRS than from non-FPMRS (8 vs 14, p<0.01), but longer from contact to initial appointment (31 vs 29, p=0.04).
Figure 1.
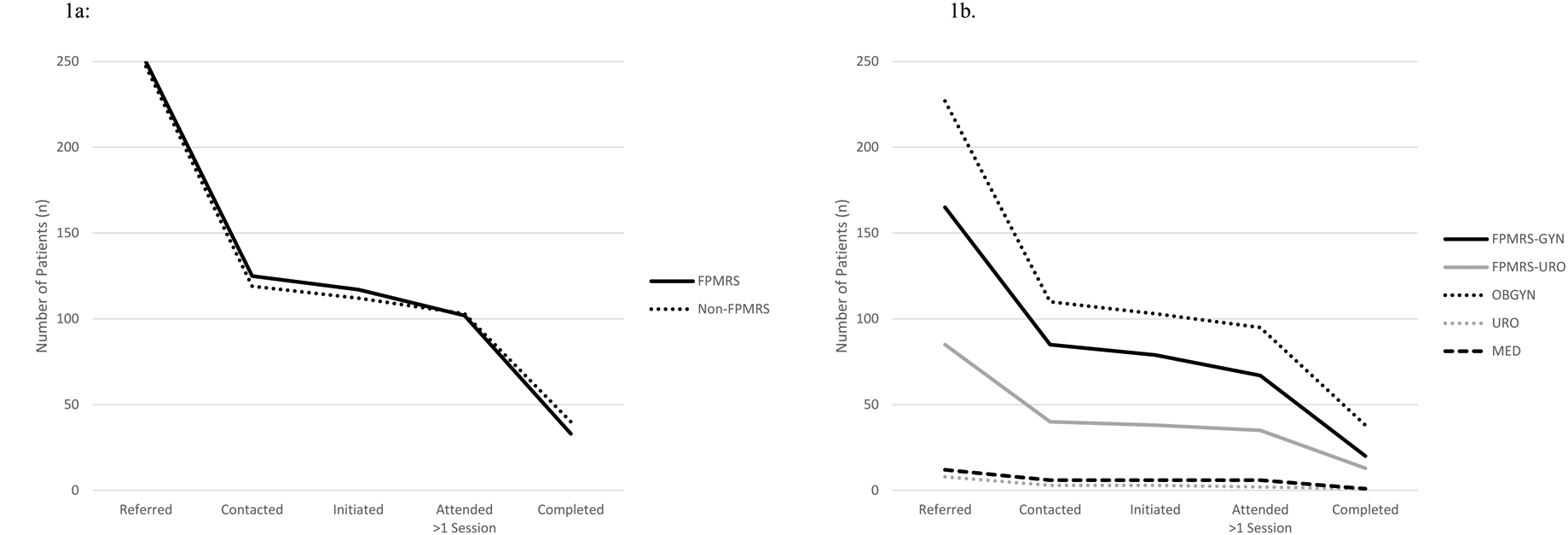
1a: Pelvic floor physical therapy attendance by FPMRS and non-FMPRS providers
1b. Pelvic floor physical therapy attendance for each provider specialty
Abbreviations: FPMRS=Female Pelvic Medicine and Reconstructive Surgery; FPMRS-GYN=Female Pelvic Medicine and Reconstructive Surgery in the department of Obstetrics & Gynecology; FPMRS-URO=Female Pelvic Medicine and Reconstructive Surgery in the department of Urology; OBGYN=Obstetrics & Gynecology; URO=Urology; MED=Medicine
Comparison of initiators and non-initiators showed differences in race (p<0.01) and number of referring diagnoses (p<0.001) (Table 2). Initiators were more likely to have prior PFPT experience (p=0.02) and have additional therapy provided at referring visit (p<0.01). When comparing types of additional therapy, there was no specific therapy associated with greater rates of PFPT initiation. Comparison of completers and non-completers demonstrated higher rates of completion in patients referred for pelvic pain and lower rates of completion in those referred for urinary incontinence (both p=0.02). There were no significant differences for any other univariate comparisons. Median number of sessions attended were different between completers and non-completers (6.0 (IQR 4, 9) vs 3.5 (IQR 2, 5), p<0.0001).
Table 2:
Patient characteristics by PFPT initiation and completion status
| n=268 | p-value | n=156 | p-value | |||
|---|---|---|---|---|---|---|
| Age, years, median (IQR) | 40.1 (32.2, 60.6) | 44.0 (33.6, 60.2) | 0.211 | 38.2 (32.1, 63.9) | 41.0 (32.4, 58.5) | 0.811 |
| Race, % (n) | <0.01 | 0.092 | ||||
| Non-Hispanic White | 55% (127) | 61% (164) | 63% (46) | 52% (81) | ||
| Hispanic | 11% (25) | 15% (39) | 5% (4) | 13% (21) | ||
| Asian | 19% (43) | 7% (19) | 20% (14) | 19% (29) | ||
| Black | 5% (12) | 5% (14) | 1% (1) | 7% (11) | ||
| Other | 5% (12) | 7% (18) | 8% (6) | 4% (6) | ||
| Unknown | 4% (10) | 5% (14) | 3% (2) | 5% (8) | ||
| Parity | 0.262 | 0.062 | ||||
| 0 | 42% (96) | 35% (95) | 55% (40) | 36% (56) | ||
| 1 | 19% (44) | 19% (52) | 19% (14) | 19% (30) | ||
| 2 | 28% (63) | 31% (82) | 18% (13) | 32% (50) | ||
| 3 | 9% (21) | 9% (24) | 7% (5) | 10% (16) | ||
| ≥4 | 2% (5) | 6% (15) | 1% (1) | 3% (4) | ||
| Pregnant at time of referral, % (n) | 5% (11) | 2% (5) | 0.082 | 8% (6) | 3% (5) | 0.112 |
| Postpartum at time of referral, % (n) | 9% (20) | 5% (14) | 0.12 | 5% (4) | 10% (16) | 0.322 |
| Menopausal status, % (n) | 0.48 | 0.73 | ||||
| Premenopausal | 65% (148) | 62% (165) | 63% (46) | 65% (102) | ||
| Postmenopausal | 35% (81) | 38% (103) | 37% (27) | 35% (54) | ||
| Insurance, % (n) | 0.142 | 0.342 | ||||
| Commercial | 86% (197) | 79% (212) | 90% (66) | 84% (131) | ||
| Medicare | 12% (28) | 19% (50) | 10% (7) | 13% (21) | ||
| Medi-Cal | 2% (4) | 1% (4) | 0% (0) | 3% (4) | ||
| Uninsured | 0% (0) | 0% (1) | -- | -- | ||
| Other | 0% (0) | 0% (1) | -- | -- | ||
| Referring diagnosis, % (n) | ||||||
| Urinary incontinence | 51% (116) | 50% (133) | 0.82 | 40% (29) | 56% (87) | 0.02 |
| Voiding dysfunction | 6% (13) | 3% (8) | 0.14 | 5% (4) | 6% (9) | 0.992 |
| IC/PBS | 5% (12) | 5% (14) | 0.99 | 4% (3) | 6% (9) | 0.772 |
| Pelvic pain | 52% (119) | 45% (120) | 0.11 | 63% (46) | 47% (73) | 0.02 |
| Pelvic organ prolapse | 8% (19) | 9% (23) | 0.91 | 7% (5) | 9% (14) | 0.802 |
| Pelvic floor weakness | 2% (4) | 2% (5) | 0.992 | 0% (0) | 2% (4) | 0.312 |
| Anal incontinence | 5% (12) | 3% (8) | 0.20 | 4% (3) | 6% (9) | 0.762 |
| Defecatory dysfunction | 2% (5) | 2% (5) | 0.992 | 5% (2) | 2% (3) | 0.662 |
| Other | 4% (9) | 1% (3) | 0.072 | 1% (1) | 5% (8) | 0.282 |
| Number of referring diagnoses, % (n) | <0.001 2 | 0.332 | ||||
| 1 | 50% (114) | 70% (187) | 49% (36) | 50% (78) | ||
| 2 | 38% (87) | 24% (64) | 38% (28) | 38% (59) | ||
| 3 | 10% (22) | 5% (14) | 13% (9) | 9% (13) | ||
| 4 | 3% (6) | 1% (3) | 0% (0) | 3% (6) | ||
| Prior PFD treatment, % (n) | 39% (90) | 34% (91) | 0.22 | 37% (27) | 40% (63) | 0.62 |
| Prior physical therapy, % (n) | 41% (95) | 33% (89) | 0.06 | 38% (28) | 43% (67) | 0.51 |
| Prior pelvic floor physical therapy, % (n) | 15% (34) | 8% (22) | 0.02 | 14% (10) | 15% (24) | 0.74 |
| Pre-PFDI-20 score, median (IQR)* | 77.6 (46.9, 114.6) | 79.2 (54.2, 112.5) | 0.741 | 66.7 (46.9, 113.6) | 80.2 (47.9, 114.6) | 0.361 |
| Additional therapy provided at referring visit, % (n) | 53% (121) | 41% (110) | <0.01 | 49% (36) | 54% (85) | 0.47 |
| Second referral for PFPT prior to initiating, % (n) | 0.352 | 0.442 | ||||
| Yes, FPMRS | 2% (4) | 0% (1) | 0% (0) | 3% (4) | ||
| Yes, Non-FPMRS | 4% (9) | 4% (10) | 3% (2) | 4% (7) | ||
| Co-pay per PFPT session, % (n) | 0.382 | |||||
| $0–25 | -- | -- | -- | 79% (58) | 86% (134) | |
| $26–50 | -- | -- | -- | 20% (14) | 13% (20) | |
| ≥$51 | -- | -- | -- | 1% (1) | 1% (2) |
Wilcoxon rank-sum
Fisher’s exact
Abbreviations: IC/PBS=interstitial cystitis/painful bladder syndrome; PFD=pelvic floor disorder; PFDI=Pelvic Floor Distress Inventory; PFPT=pelvic floor physical therapy; FPMRS=Female Pelvic Medicine and Reconstructive Surgery
From the logistic regression, factors significantly associated with PFPT initiation included age ≥65 years old, additional therapy provided at referring visit, private insurance, Asian race, referral during pregnancy or postpartum period, and having 2 or 3 referring diagnoses (all p <0.05). No factors were associated with PFPT completion on logistic regression (Table 3).
Table 3:
Odds ratios from multivariate logistic regression of PFPT initiation and completion.
| PFPT Initiation1 N=229 |
PFPT Completion2 N=73 |
|||
|---|---|---|---|---|
| OR (95% CI) | p-value | OR (95% CI) | p-value | |
| Age (<65 vs ≥65) | 1.98 (1.01–3.89) | <0.05 | 1.54 (0.72–3.32) | 0.27 |
| Referring provider specialty (FPMRS vs Non-FPMRS) | 1.35 (0.88–2.07) | 0.17 | 1.28 (0.64–2.56) | 0.49 |
| Prior PFPT (yes vs no) | 1.41 (0.75–2.62) | 0.28 | -- | |
| Additional therapy provided at referring visit (yes vs no) | 1.74 (1.16–2.61) | <0.01 | 0.68 (0.37–1.28) | 0.23 |
| Insurance (public vs private) 3 | 2.43 (1.19–4.98) | 0.01 | -- | |
| Race (White as referent) | 0.02 | |||
| Hispanic | 0.92 (0.52–1.65) | |||
| Asian4 | 2.89 (1.55–5.39) | |||
| Black | 1.41 (0.61–3.31) | |||
| Other | 0.86 (0.37–1.97) | |||
| Unknown | 0.72 (0.29–1.75) | |||
| Race (White vs non-white) | 0.67 (0.37–1.21) | 0.18 | ||
| Pregnant at time of referral (no vs yes) | 3.58 (1.11–11.61) | 0.03 | 1.90 (0.50–7.22) | 0.35 |
| Postpartum at time of referral (no vs yes) | 2.77 (1.22–6.31) | 0.02 | 0.46 (0.13–1.65) | 0.23 |
| Number of referring diagnoses (1 as referent) | <0.01 | -- | ||
| 2 | 2.02 (1.32–3.10) | |||
| 3 | 2.28 (1.06–4.90) | |||
| 4 | 3.96 (0.93–16.93) | |||
| Urinary Incontinence | -- | 1.43 (0.69–2.94) | 0.33 | |
| Pelvic pain | -- | 1.53 (0.70–3.32) | 0.28 | |
Among those contacted for PFPT
Among those who initiated PFPT
Public insurance includes Medi-Cal, Medicare, and other
Asians were more likely to be initiators compared to all other races
Abbreviations: PFPT= pelvic floor physical therapy; FPMRS=Female Pelvic Medicine and Reconstructive Surgery
Goal achievement was seen in 23% (n=52) of initiators and an additional 50% (n=114) were noted to have subjective symptom improvement. Symptoms were unchanged in 14% (n=32) and worse in 0.4% (n=1). Subjective symptom assessment was not documented in 3% (n=6), and 10% (n=24) of initiators attended only one session thereby preventing assessment of improvement.
Reasons for not initiating or completing PFPT were not documented for 85% and 82%, respectively. Of the identified reasons, distance (6% overall) was the most common reason for not initiating PFPT. Not having sufficient time to attend PFPT (8% overall) was the most common for not completing PFPT. There were no differences seen between FPMRS and non-FPMRS (Table 4).
Table 4:
Reasons for Not Attending and Completing Pelvic Floor Physical Therapy
| Total N=268 | FPMRS n=133 | Non-FPMRS n=135 | p-value | |
|---|---|---|---|---|
| % (n) | % (n) | % (n) | ||
| Reasons for Not Attending PFPT | ||||
| No time | 1% (4) | 2% (3) | 1% (1) | 0.371 |
| Too far | 6% (16) | 8% (11) | 4% (5) | 0.131 |
| Cost | 2% (5) | 0% (0) | 4% (5) | 0.061 |
| Not sufficiently bothersome | 3% (8) | 2% (3) | 4% (5) | 0.771 |
| Did home pelvic floor exercises | 1% (4) | 1% (3) | 0% (1) | 0.371 |
| Went to outside PFPT | 4% (12) | 6% (8) | 3% (4) | 0.251 |
| Other | 1% (3) | 2% (2) | 1% (1) | 0.621 |
| Unknown | 85% (228) | 83% (111) | 87% (117) | 0.46 |
| Reasons for Not Completing PFPT 2 | n=156 | n=84 | n=72 | |
| No time | 8% (12) | 7% (6) | 8% (6) | 0.78 |
| Too far | 3% (5) | 2% (2) | 4% (3) | 0.661 |
| Cost | 1% (2) | 1% (1) | 1% (1) | 0.991 |
| No improvement | 4% (8) | 4% (4) | 5% (4) | 0.991 |
| Other | 2% (3) | 2% (2) | 1% (1) | 0.991 |
| Unknown | 82% (128) | 82% (69) | 82% (59) | 0.97 |
Fisher’s exact
Patients could have ≥1 reason identified for not attending or completing pelvic floor physical therapy. Percentage represents of number patients with that identified reason over the number of patients in each group.
Discussion
Despite PFME, including PFPT, being recommended early conservative therapy for many PFD, our study demonstrates less than half of patients referred from a large academic medical center to affiliated PFPT initiate therapy and only 15% complete PFPT. Referring provider specialty did not impact rates of initiation or completion.
This is the first study we are aware of that specifically addresses the question of PFPT attendance based on referring provider specialty and that explores referrals spanning over multiple specialties and PFD. Our initial hypothesis was that referrals from FPMRS would have greater attendance as those patients sought out specialty care, received comprehensive counseling regarding management options, and mutually decided with their provider to pursue PFPT. Whereas with non-FPMRS referrals, PFPT may have been considered an early, benign intervention with plans to concomitantly or subsequently refer to FPMRS if PFPT was insufficient.
Our results demonstrated the populations referred by FPMRS and non-FPMRS are different. FPMRS referrals were older, more likely to be postmenopausal and have Medicare. Appropriately, FPMRS had more referrals for incontinence and bowel and bladder dysfunction, which makes up a significant portion of their practice. The majority of non-FPMRS referrals were from the department of Obstetrics & Gynecology and consisted of younger women with pelvic pain and pelvic floor weakness. These referrals also included women who were pregnant or postpartum. Despite referring different patient populations, PFPT attendance was similar and did not appear to be impacted by the referring provider. Additionally, while there were significant differences between FPMRS and non-FPMRS in time intervals from PFPT referral to attendance of first session, this was not associated with differences in PFPT attendance, and most patients initiated PFPT within 6 weeks from referral.
We identified other factors associated with PFPT initiation including Asian race, greater number of referring diagnoses, and prior PFPT. Additionally, women referred during pregnancy and postpartum were more likely to attend, though no differences were seen with completion.
Our study adds to the literature on PFPT attendance rates. Prior studies have demonstrated PFPT initiation rates between 65–78%9–12 compared to our 49%. Our initiation rates may be lower as we only included referrals to our affiliated PFPT clinics rather than referrals to any community PFPT office.10–12 By excluding referrals to outside PFPT we may be missing a subset of patients with higher attendance rates as they are able to identify and initiate PFPT more convenient to their home or work. Greater distance to PFPT is a barrier to initiating care, even in the setting of treatment without cost.9 This result is aligned with our finding that distance to PFPT was the most frequently identified reason for not initiating PFPT.
Our overall PFPT completion rate of 15% is lower than the reported 29–42%10–12 among PFPT referrals from FPMRS at academic medical centers in the United States. This difference may be in part due to various definitions of PFPT completion in the literature and, again, our limited examination inclusion of only institution affiliated PFPT referrals. Brown et al. reported the highest completion rate of 42%, with completion defined as attendance of ≥3 visits or discharge from PFPT. Under this alternative definition, our completion rate increases to 35%. However, completers in our study attended a median number of 6 sessions, which is double the number of sessions they acknowledged as completion. Shannon et al. defined completion as discharge from PFPT by the physical therapist when meeting goals, which is more aligned to our definition, yet they still had greater completion rates. In those studies, patients selected their PFPT allowing them to presumably choose locations more convenient or better covered by insurance thereby reducing barriers to PFPT access.
Race has been associated with compliance in prior studies, and our study highlights this aspect as well. Shannon et al. reported a trend towards lower compliance with Hispanic race and Brown et al. reported greater compliance with non-Hispanic white race. Our study demonstrated that Asian race was associated with greater rates of initiation, but that effect was not seen in rates of completion. These studies, including ours, were limited by a predominantly non-Hispanic white cohort, and therefore the impact of race on compliance is difficult to interpret or generalize to more diverse populations.
Strengths of this study were the large number of referrals to institution-affiliated PFPT clinics over a one-year time period and the equal distribution from both FPMRS and non-FPMRS. Data collection was comprehensive given the ability to access PFPT details since it was within the same electronic medical record. We were specifically able to look at whether patients contacted PFPT, cost of therapy, and patients’ stated goals and subjective improvement.
Limitations of this study include its retrospective nature and varied patient follow-up with referring providers. For many patients it was not documented why they did not attend PFPT, therefore we were unable to identify specific barriers patients may experience in accessing and attending PFPT. Also, because we chose to include only referrals to the institution affiliated PFPT, we are unable to describe a more global experience of PFPT utilization.
In summary, we found that PFPT initiation and especially completion rates were low despite guidelines and universal endorsement of early conservative therapy for the majority of PFD. The utilization of PFPT does not appear to be impacted by the referring provider. We therefore support that PFPT be widely promoted and recommended from all providers who evaluate PFD whether they are providing a broader scope of care or evaluating specifically for PFD. Further research needs to identify why patients may not initiate PFPT and determine which of these barriers to PFPT can be modified for improved compliance and successful use of conservative care. Additionally, examination of what further therapies patients elect for after referral to PPFT could provide better recognition of patient desires and motivations for management of PFD. Understanding patient experiences with PFPT may be better achieved in a prospective manner with standardized follow-up with routine phone calls or follow-up visits after referral to PFPT specifically addressing barriers and access to care.
Sources of support:
This research was supported by NIH National Center for Advancing Translational Science (NCATS) UCLA CTSI Grant Number UL1TR001881.
References
- 1.Dumoulin C, Hay-Smith J, Habée-Séguin GM, Mercier J. Pelvic floor muscle training versus no treatment, or inactive control treatments, for urinary incontinence in women: A short version Cochrane systematic review with meta-analysis. Neurourol Urodynam 2015;34:300–8. [DOI] [PubMed] [Google Scholar]
- 2.Urinary incontinence in women. Practice Bulletin No. 155. American College of Obstetricians and Gynecologists. Obstet Gynecol 2015;126:e66–e81. [DOI] [PubMed] [Google Scholar]
- 3.Fecal incontinence. Practice Bulletin No. 210. American College of Obstetricians and Gynecologists. Obstet Gynecol 2019;133:e260–e273. [DOI] [PubMed] [Google Scholar]
- 4.Wald A, Bharucha AE, Cosman BC, Whitehead WE. ACG clinical guideline: Management of benign anorectal disorders. Am J Gastroenterol 2014;109:1141–57. [DOI] [PubMed] [Google Scholar]
- 5.Fitz FF, Resende APM, Stupp L, Sartori MGF, Girawo MJBC, Castro RA. Biofeedback for the treatment of pelvic floor muscle dysfunction: a systematic review and meta-analysis. IUJ 2012;23:1495–1516. [DOI] [PubMed] [Google Scholar]
- 6.Hanno PM, Erickson D, Modwin R, Faraday MM. Diagnosis and treatment interstitial cystitis/bladder pain syndrome: AUA guideline amendment. J Urol 2015;4:1545–1553. [DOI] [PubMed] [Google Scholar]
- 7.Hagen S, Stark D. Conservative prevention and management of pelvic organ prolapse in women (Review). Cochrane Database Syst Rev 2011;12. [DOI] [PubMed] [Google Scholar]
- 8.Pelvic organ prolapse. Practice Bulletin No. 214. American College of Obstetricians and Gynecologists. Obstet Gynecol 2019;134:e126–e142. [DOI] [PubMed] [Google Scholar]
- 9.Tibaek S, Dehlendorff C. Do women with pelvic floor dysfunction referred by gynaecologists and urologists at hospitals complete a pelvic floor muscle training programme? A retrospective study, 1992–2008. IUJ 2013;24:1361–1369. [DOI] [PubMed] [Google Scholar]
- 10.Shannon MB, Genereuz M, Brincat C, Adams W, Brubaker L, Mueller ER, et al. Attendance at prescribed pelvic floor physical therapy in a diverse, urban urogynecology population. PM R 2018;10:601–606. [DOI] [PubMed] [Google Scholar]
- 11.Brown HW, Barnes HC, Lim A, Giles DL, McAchran SE. Better together: multidisciplinary approach improves adherence to pelvic floor physical therapy. IUJ 2020;31:887–893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Shannon MB, Adams W, Fitzgerald CM, Mueller ER, Brubaker L, Brincan C. Does patient education augment pelvic floor physical therapy preparedness and attendance? A randomized controlled trial. Female Pelvic Med Reconstr Surg 2018;24:155–160. [DOI] [PubMed] [Google Scholar]
- 13.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG, Research electronic data capture (REDCap) – A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009;42:377–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Harris PA, Taylor R, Minor BL, Elliott, Fernandez M, O’Neal L, McLeod L, Delacqua G, Delacqua, Kirby J, Duda SN, REDCap Consortium, The REDCap consortium: Building an international community of software partners. J Biomed Inform 2019. May 9 [doi: 10.1016/j.jbi.2019.103208] [DOI] [PMC free article] [PubMed] [Google Scholar]


