Abstract
Bangladesh’s forest-dependent people rely on medicinal plants for traditional healthcare practices, as plant-based medicines are easily available and cost-effective. This study evaluated and documented ethnomedicinal practices for, and traditional knowledge of, utilising plants to cure ailments. Ethnobotanical indices quantified the use value (UV), frequency of citation, relative frequency of citation (RFC) and the informant consensus factor. Using a semi-structured questionnaire, the study interviewed 231 respondents from 18 villages in and around Chunati Wildlife Sanctuary (CWS). The study documented 134 medicinal plant species from 60 families; tree species were dominant (37.31%). Malvaceae (seven species), Rutaceae and Lamiaceae (six species each) families covered more species. Nearly half of the species (46.02%) were collected from CWS. Both above-ground and below-ground plant parts treated 71 types of ailments under 21 categories, with leaves (66 species) being the most widely used plant part. In total 33 species were used to treat dysentery, 25 species each for fever and jaundice, and 24 species for cuts and wounds. The average UV value was 0.24 and RFC value was 0.47%. Communities were found to utilise medicinal plants more at home than to sell at markets, substantially relying on medicinal plants to meet their domestic needs. Plants used for healthcare and cultural and religious beliefs have a strong connection that plays a vital role in plant conservation. This study identified 42 medicinal plant species that could be considered to treat COVID-19 patients in Bangladesh. The findings suggest that community awareness of sustainable harvesting and commercial cultivation could lead to conservation and use of these invaluable plant species for healthcare, new drugs discovery and sustainable forest management.
Supplementary Information
The online version contains supplementary material available at 10.1007/s42398-022-00230-z.
Keywords: Medicinal plants, Traditional knowledge, Ailments, Medicine preparation, Cultural and traditional beliefs, COVID-19
Introduction
Billions of people worldwide depend partly or entirely on more than 70,000 medicinal plants (Alamgir 2017), with this as a provisioning ecosystem service as mentioned in the United Nations (UN) Millennium Ecosystem Assessment (WHO 2005). Medicinal plants used in popular and traditional medicine and developing pharmaceuticals also provide cultural and economic value to local people (Kaky and Gilbert 2016; Jamshidi-Kia et al. 2018). Growing scientific and commercial interest is evident for medicinal plants as raw materials for herbal pharmaceutical companies growing in importance and increasing greatly due to global demand (Bieski et al. 2015). According to the World Health Organization (WHO), 70–95% people in developing countries still largely rely on medicinal plants for their primary healthcare purposes. The worldwide market value for medicinal plant products (made from plant extracts containing phytochemicals) was approximately US$60 billion in 2017 and is expected to reach more than US$129 billion by 2023 (Market Research Future 2018). Yet only 15% of medicinal plants globally have been evaluated to determine their phytochemical and phytopharmacological potential (De Luca et al. 2012).
Southeast Asia and South Asia are hotspots for medicinal plants used for traditional healthcare practices. Bangladesh, a South Asian country in which about 75% of the country’s total population lives in rural areas, has almost 80% of its population reliant on plant-based ethnomedicine for their primary healthcare purposes, such as treating fever, coughs and colds, diarrhoea and dysentery (Ahmed 2009; FAO 2010). Bangladesh is thought to be home to about 6500 plants, of which more than 500 species have medicinal value, with 250 regularly used in preparing medicines for healthcare purposes (Ahmed et al. 2009). In the country’s rural areas, knowledge of medicinal plant use has historically originated from forest-dependent communities across the country, particularly in the central (Islam et al. 2014); northeastern (Khan et al. 2011); southwestern (Mollik et al. 2009); and southeastern regions (Faruque et al. 2018). The traditional knowledge of these communities also significantly contributes to the origin and evolution of many effective herbal medicines, including those for treatments of cancer and cardiovascular diseases (Chowdhury and Koike 2010). According to Bangladesh’s Directorate General of Drug Administration (available at www.dgda.gov.bd/), the number of plant-based medicine manufacturers is 528 (Unani 272, Ayurvedic 201 and herbal 55), with their registered medicines totalling 11,290 (Unani 6630, Ayurvedic 4110 and herbal 550). No restrictions apply to the sale of medicinal plant products in Bangladesh, with the quality of these medicines lagging due to various bottlenecks and stakeholders’ lack of goodwill.
Bangladesh’s traditional ethnomedicine sector has long been established in an important position in rural and forest-dependent communities' socio-cultural, spiritual, economic, and healthcare arenas (Chowdhury and Koike 2010). Plant-based herbal medicines are easily available and cost-effective for these communities (Faruque et al. 2018). Over the last two decades, medicinal plants and ethnomedicinal studies have been carried out in different parts of Bangladesh, receiving significant attention from the government and pharmaceuticals sector. At the same time, medicinal plants are rarely commercially farmed in Bangladesh and are mostly used when gathered from the wild. However, the growing demand for herbal products has led to a quantum leap in the volume of plant materials traded within and across the country (Shahidullah and Haque 2010). In Bangladesh, the rural people conserve their traditional ethnomedicinal knowledge through their experience and practice from generation to generation, handed down orally with no documentation (Bregum 2010; Rahman 2013). Motaleb and Khan (2012) reported that the age-old practice of traditional ethnomedicine is highly threatened by deforestation, land-use change and unsustainable harvesting. In contrast, the growing demand for medicinal products incentivises further over-exploitation. Other studies (e.g., Khan et al. 2011; Rahman et al. 2011a; Rahman 2013) indicated that this invaluable traditional knowledge is now under threat of extinction due to its limited inter-generational transfer and inadequate documentation.
Additionally, the coronavirus disease (COVID-19) pandemic, caused by the severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) has spread to 226 countries and territories worldwide since December 2019 and is now the topmost global public health concern. As of 14 April 2022, there have been 500,186,525 confirmed cases of COVID-19, including 6,190,349 deaths (WHO 2022). Several studies (e.g., Adeleye et al. 2021; Ang et al. 2020a, b; Benarba and Pandiella 2020; Deng et al. 2020; El Alami et al. 2020; Jahan and Onay 2020; Khadka et al. 2021; Lee et al. 2020; Luo et al. 2020a, b; Runfeng et al. 2020; Shawky et al. 2020; Silveira et al. 2020; Vardanjani et al. 2020; Weng 2020; Zhou et al. 2020; Zhuang et al. 2020) have suggested that ethnomedicine from traditional Chinese, Indian and Persian medicine could be considered as rich sources of ingredients to be used in drug discovery to combat COVID-19. These studies confirmed that China, South Korea and India have widely used medicinal plants for COVID-19 treatment, with several clinical practice results showing significant roles. Moreover, studies conducted in Bangladesh (e.g., Ahmed et al. 2020; Azam et al. 2020; Bhuiyan et al. 2020; Bachar et al. 2021; Dutta et al. 2021; Islam et al. 2021; Shahriar et al. 2022) have reported more than 30–149 plant species that have been found useful for COVID-19 treatment as home remedies by Bangladeshi COVID-19 patients. These shreds of evidence support the effective use of these plants and their products in preventing and managing COVID-19 symptoms.
Scientific studies on Bangladesh have claimed that one of the best ways to conserve medicinal plants and the related traditional knowledge is through documentation and stimulating traditional practices involving local people. However, documentation has not previously been undertaken of traditional healthcare knowledge in study area of present study, Chunati Wildlife Sanctuary (CWS), located in southeastern Bangladesh. Despite its many unique features, the flora diversity of CWS and, more specifically, of plants used by local people to treat various ailments remains unexplored. Regarding the natural growth of medicinal plants in the CWS wilderness, the ethnobotanical knowledge of forest-dependent communities in and around CWS must be documented and conserved. The objectives of this study were:
-
(i)
to evaluate and document the plant-based ethnomedicinal practices and traditional knowledge of the utilisation of plants for curing ailments, using this to construct a database of medicinal plants and their traditional uses in and around CWS.
-
(ii)
to perform quantitative analysis of the documented data using quantitative ethnobotanical indices.
-
(iii)
to evaluate the role of cultural and traditional beliefs regarding medicinal plant conservation across these poorly studied communities.
-
(iv)
to record the available medicinal plant species in CWS potential for use in COVID-19 treatment as home remedies by Bangladeshi COVID-19 patients.
This pioneering attempt to conduct a quantitative ethnomedicinal study in and around CWS aims to provide a useful guideline for further phytochemical and phytopharmacological investigations to discover new drugs. We hope that the documentation in the present study of the traditional knowledge and practices associated with these plant resources will form part of an important strategy linked to the ex situ and in situ conservation of medicinal plants, sustainable management of CWS, and improvement in the quality of life of poor forest-dependent communities. Furthermore, this study’s findings are intended to be helpful for Bangladesh’s Forest Department and non-governmental organisations (NGOs) when working in and around CWS on community-based medicinal plant cultivation, management and commercialisation.
Materials and methods
Description of Chunati Wildlife Sanctuary
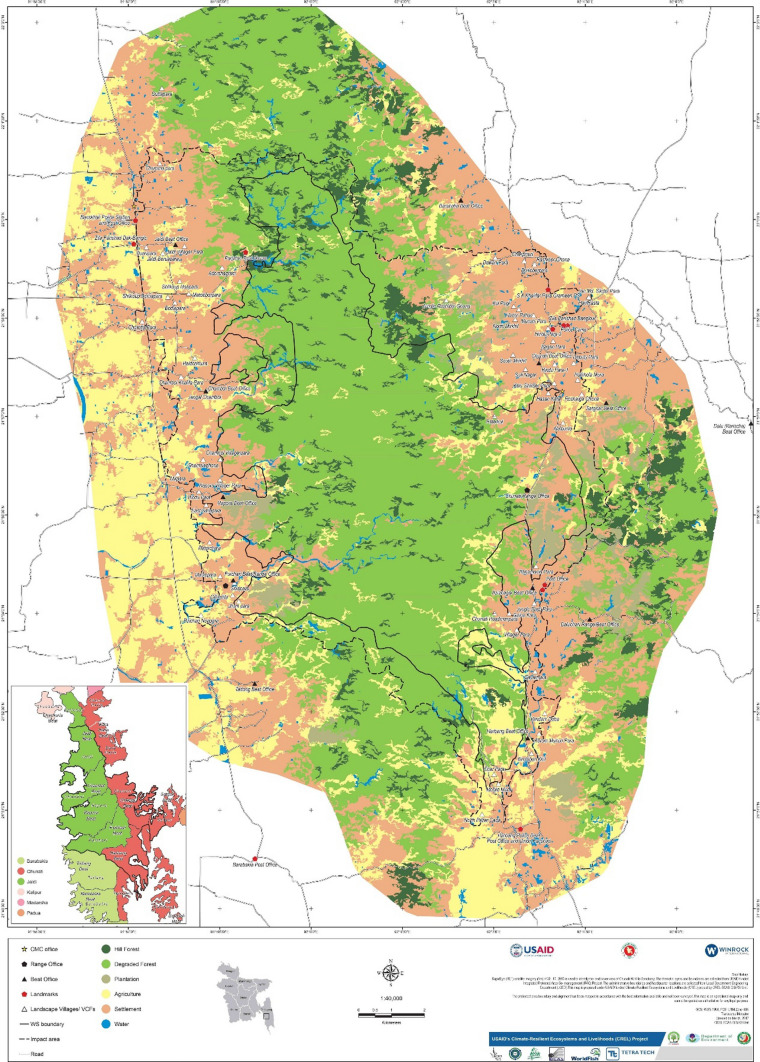
The CWS is located at 21° 40′ N and 92° 07′ E in the Chattogram Division of southeastern Bangladesh (Fig. 1). With an area of 7764 hectares (ha), CWS was established in 1986 to reduce the rate of deforestation and forest degradation and to conserve the habitat of the Asian elephant (Elephas maximus). It comprises two Forest Ranges and seven Forest Beats (the lowest forest administration unit) (Mollah et al. 2004). The physiography of CWS is generally hilly (average elevation is 30–90 m above sea level [m asl]). Inside the sanctuary, many places are traversed by numerous creeks with beds of gravel or stone. These creeks provide a good drainage facility, supplying water within the sanctuary for wildlife, people and irrigation in agricultural fields (GIZ 2011).
Fig. 1.
Location map of Chunati Wildlife Sanctuary in southeastern Bangladesh
(source: http://nishorgo.org/project/)
The CWS enjoys a tropical moist climate (temperature ranges from 14 to 32 °C) characterised by frequent rainfall (annual precipitation is 3000 mm) from April to September. The original semi-evergreen forests have been degraded due to heavy anthropogenic interferences, including cultivating betel leaf (Piper betle, Piperaceae family) inside the sanctuary. A little natural forest area exists in CWS, with only a few scattered patches of Dipterocarpus spp. For management purposes, CWS is divided into five designated habitat types, namely, scattered grasslands and bamboo patches; cultivated lands; patches of secondary forests, wetlands and water bodies; and short and long rotation plantations (BFD 2015).
The CWS is the remaining vital habitat in Bangladesh of the globally threatened E. maximus. Therefore, CWS has experienced more research activity and positive attention from donors since its establishment than any protected forests in Bangladesh. Habitat fragmentation and degradation caused by anthropogenic forest use activities have increased conflict between humans and E. maximus. The major damaged areas are paddy fields, homestead forests, vegetable gardens and settlements (Sarker and Røskaft 2010; Kabir 2013).
This sanctuary harbours diverse flora resources, namely, 691 plant species comprising 240 tree species (96 of which are exotic tree species), 102 shrub species, 211 herb species, 106 climber species, 19 epiphyte species, 7 parasite species and 6 fern species (Hossain and Hossain 2014). The average tree density per ha is only 239 trees, and seedling density per ha is 77,000, with more than 60% of the trees being exotic tree species that have been planted (GIZ 2011). The status of the CWS’s carbon stock is low, at only 136.48 CO2 Mg ha1, indicating the degraded condition of this sanctuary (Fakir et al. 2015).
Local community members’ livelihoods in and around the sanctuary
About 57,000 people from 10,200 households live in and around CWS in 69 registered forest villages (locally called para) (BFD 2015). Over 50% of the population is dependent on forest resources for their livelihoods (GIZ 2011), with nearly 65% living on the poverty line. About 48% of the villages are located inside and at the edge of CWS, while the remaining villages are located outside but adjacent to and near the sanctuary. The only indigenous community living in CWS is called Mog (Hoque 2009).
Nearly 50% of the population is engaged in agriculture, 10% in fishing, 20% are day labourers, and the remaining 20% are involved in other occupations (BFD 2015). The women are housewives and involved in poultry, duck and cattle rearing to generate extra household income (Tamima 2016). The collection of forest resources, such as timber and non-timber forest products (NTFPs), by both men and women is considered a secondary occupation in and around CWS, which plays a vital role in income generation (BFD 2015). About 80% of households depend on NTFPs (e.g., fuelwood, bamboo, medicinal plants, Imperata cylindrica and wild fruits). Unfortunately, over-exploitation of these NTFPs has resulted in the degradation of CWS resources.
People have encroached on and used forestland to expand settlements, agricultural farming, vegetable gardening, fish cultivation, betel leaf cultivation and cattle grazing. Landless poor people usually lease land (from local elites who lease the forestland from local forest offices) for agricultural farming for their consumption and to sell farm produce at the market for subsistence income (GIZ 2011). Agricultural labourers find work for 6 months in a year but have no income-earning work for the remaining 6 months. They are engaged in illegal harvesting of timber and NTFPs and selling these products at the nearest market to generate income during the unemployed period (BFD 2015). Consequently, conflict arises between local people and the Forest Department. The former use the forestland for their livelihood, and the latter seek to restrict the forestland’s use for biodiversity conservation (Rahman et al. 2017a).
The CWS is one of the pilot sites in Bangladesh for co-management project implementation with financial and technical assistance from the United States Agency for International Development (USAID), in partnership with the Forest Department (Rahman 2013). Between 2004 and 2018, three co-management projects have been implemented in this sanctuary, aiming to restore, protect and conserve the remaining forest biodiversity, undertake sustainable use of forest resources and reduce forest dependency among forest-dependent communities through alternative income-generating (AIG) activities (Rahman et al. 2017a, b). Furthermore, the Deutsche Gesellschaft für Internationale Zusammenarbeit (GIZ)-funded Management of Natural Resources and Community Forestry (MNRCF)-Chunati project (2009–2015) implemented pilot reforestation and sustainable forest management measures in CWS based on cooperation between local co-management organisations and the Forest Department. This project further strengthened co-management structures through different non-forestry income-generating, cultural and awareness-raising activities (GIZ 2015; Rahman et al. 2017a, b).
The co-management projects increased households’ average monthly non-forestry income by US$140 and decreased their average monthly forest income by US$25 (Rahman et al. 2017a). At the end of these co-management projects, Islam et al. (2019) assessed that people were still entering the CWS to collect forest products with a total estimated market value of about US$1856 a day. The local people were still practising betel leaf farming inside the sanctuary.
Villagers have no legal rights to collect forest resources and use forestland for settlements, farming and fishing. The co-management and participatory social forestry schemes evolved to give forest-dependent people ownership and a stake in managing forest resources, incentivise them to protect forest resources, and involve them in non-forest-related livelihood options. However, forest use rights for the sustainable harvest of both timber and NTFPs are granted to local communities involved in protection activities through Participatory Benefit Sharing Agreements (PBSAs) in the buffer zone (an area of 4615 ha) (BFD 2015).
Study methods
Conceptual framework of the study
Forest-dependent communities have used plants, plant parts and plant-derived products for healthcare purposes in Bangladesh since time immemorial. Unfortunately, detailed plant information and complete inventories on these plants often do not exist. Moreover, studies that combine the investigation of the traditional use of medicinal plants and their quantitative values are also minimal. Moreover, the 2050 vision of the Convention on Biological Diversity (CBD 2010) and the 2020 Aichi Biodiversity’s Target 14 call for increased efforts to conserve, restore, and safeguard those areas that ‘contribute to health, livelihoods, and well-being’ and ‘deliver benefits essential for all people’ (CBD 2010). To meet these goals, a necessary first step is to document and accurately quantify the ecosystem services for conservation and sustainable management (Mitchell et al. 2021). Consequently, this study aims to identify and record the CWS-dependent communities’ traditional ethnomedicinal knowledge that contributes to their health, livelihoods and well-being. Every one of these communities has unique styles for preparing medicine from plants.
Therefore, in this study, we evaluate the traditional mode of medicine preparation and utilisation of these plants for curing ailments. Due to the importance of the plant conservation, we identified the sources of medicinal plants and evaluated the cultural and traditional beliefs regarding the conservation of medicinal plants. Finally, we analyse the medicinal plant use data by employing different quantitative ethnobotanical indices. From the existing literature (e.g., Vandebroek et al. 2020), we learn that medicinal plants have been used globally to treat the novel coronavirus disease (COVID-19). In this paper, we record medicinal plants from the literature similar to those already listed in this study. Pharmaceutical companies could find these plants useful for phytochemical and phytopharmacological evaluation for effective drug preparation for COVID-19 treatments. Considering the present situation and future needs, the present study results could be useful for medicinal plants’ conservation and sustainable management, particularly in CWS and other protected forests in Bangladesh.
Reconnaissance survey
Prior to data collection, a reconnaissance survey was carried out in June 2013 in the study area to gain some basic ideas about the CWS’s medicinal plants through personal discussion with staff from the Forest Department, the MNRCF-Chunati project and the Climate-Resilient Ecosystems and Livelihoods (CREL) project, as well as with local herbal practitioners (called Kabiraj). A complete list of villages in and around CWS was collected from the MNRCF-Chunati project. A draft household questionnaire was pre-tested with five forest-dependent people during that time. With their input, some questions were added, with some deleted, to finalise the questionnaire for the field survey. A Kabiraj was also hired and contracted for work on the final field survey.
Data collection procedures
The primary data for the study were collected through a household questionnaire survey (HQS), key informant interviews (KIIs) and focus group discussions (FGDs). Informal discussions were also conducted in tea stalls where local people gathered for refreshment, conversation and social interaction from morning to night. Secondary data were collected from published books, journal articles, and pamphlets of the Forest Department and the MNRCF-Chunati and CREL projects. Two Forestry Master’s graduates were employed in this research to help the researchers during data collection from July to October 2013.
Household questionnaire survey
A household-level ethnobotanical survey was conducted using a semi-structured questionnaire. The study applied a purposive sampling technique (e.g., village → household → respondent) to select households for survey interviews. The survey was deliberately targeted toward experienced people, mostly of older age, who attempted to identify the medicinal plants used by local people, documenting their traditional knowledge and perceptions of medicinal plant use and tracing the patterns (if any) in the harvesting and management of particular medicinal plant species.
HQS were conducted in all seven Forest Beats inside the CWS. From the 69 villages, 18 (26%) villages were selected randomly for data collection from respondents. From these 18 villages, 231 respondents (both male and female) from 231 households (covering 26% of households) were randomly selected and interviewed for the study (see details in Online Resource 1).
A semi-structured questionnaire was designed to collect information from respondents about what medicinal plant species and which plant parts they used, what ailments were treated, what usage patterns were followed, the collection sources for plants, the reasons for conservation of specific plants, etc. Interviews were conducted in each respondent’s home using the native language (Bangla), sometimes with more than one respondent participating simultaneously, with everyone’s opinion recorded for the study. The researchers and the research assistants both conducted the HQS. When needed, local dialects were interpreted by the Kabiraj.
Key informant interviews
In total, 18 KIIs (one KII from each village) were conducted using a checklist (Online Resource 1). These interviews helped to obtain more candid or in-depth answers about the CWS’s medicinal plants. The selected key informants were the local Kabiraj, herbal businessmen, nursery owners and members of the Co-Management Committee (CMC) and Village Common Forest (VCF). All KIIs were conducted by the researchers.
Focus group discussion (FGD)
In total, 18 FGDs (one FGD from each village) were conducted using a guideline (Online Resource 1). Some FGDs were conducted in the local markets, inside houses and some at the front of house-yards. For FGDs conducted at tea stalls in the market, male participants were usually dominant. In the inside house and house-yard FGDs, female participants were dominant but male participants also responded. In some cases, respondents interviewed for HQSs were also FGD participants. On average, each FGD involved participation by 10 participants. The FGDs only involved those who were knowledgeable about medicinal plant resources and the uses of medicinal plants for healthcare purposes. The FGDs were facilitated by the research assistants and moderated by the researchers. Questions in the FGDs were particularly focused on sustainable harvesting and conservation of the CWS’s medicinal plants. During the FGDs, data from the HQSs and KIIs were verified, cross-checked and validated.
Data analysis
During the field survey, the name of each medicinal plant was first recorded by its local name. Subsequently, local names were cross-referenced with the established Bangla names from the Encyclopaedia of Flora and Fauna of Bangladesh published by the Asiatic Society of Bangladesh. The species’ scientific name was recorded from the same source (see Siddique et al. 2007, 2008; Ahmed et al. 2008a, b, c, 2009, 2010). Finally, each species’ scientific name and family name were verified with “The Plant List” website (available at: www.theplantlist.org).
Quantitative status
Descriptive statistics were used to quantitatively describe or summarise the features of the data, using suitable tables and figures whenever possible. The use value (UV) score of plant species and values for the frequency of citation (FC), relative frequency of citation (RFC) and informant consensus factor (ICF) indices were also calculated using the specific equations provided below:
Use value
The UV score was calculated for individual plant species using the following equation, as explained by Phillips et al. (1994), to provide a quantitative and objective measure of its relative importance to informants:
| 1 |
where UV refers to the use value of a species; Ui refers to the number of uses reported by each informant for that plant species; and N refers to the total number of informants in the survey. A high UV score for a plant species indicated that it received many use reports (i.e., it was most frequently indicated), while a low score indicated that informants cited fewer use reports (Islam et al. 2014; Umair et al. 2017; Faruque et al. 2018).
Informant consensus factor
Before calculating the ICF value, ailments were broadly categorised into different ailment categories (Heinrich et al. 1998). The ICF values ranged from 0.00 to 1.00. The maximum ICF value, that is, a value close to 1, indicated that a well-known species was used by a large proportion of informants due to its authenticity in the treatment of ailments. However, a low ICF index value close to 0 specified that informants used this species randomly to treat reported ailments (Heinrich et al. 1998). The ICF value was calculated using the following equation:
| 2 |
where Nur referred to the total number of use reports for a particular ailment category, and Nt referred to the total number of species used for that ailment category.
Frequency of citation and relative frequency of citation indices
The FC index score was calculated using the following equation:
| 3 |
where Ns referred to the number of times a particular species was mentioned and Nt referred to the total number of times all species were mentioned.
The RFC index score was determined by dividing the FC index score by the total number of informants in the survey (N). The RFC index scores ranged from 0 when no one referred to a plant as useful to 1 when all informants referred to a plant as useful. The RFC index score was calculated using the following equation, as described by Tardío and Pardo-De-Santayana (2008):
| 4 |
Results
Demographic profile of surveyed respondents
Of the surveyed 231 respondents, about 55.41% were female. The highest number of respondents (45.89%) were 41–50 years old. Regarding educational qualifications, 62.77% of respondents completed primary education, with about one-quarter (24.68%) illiterate or only able to sign their name. As female respondents were the majority in this survey, most surveyed respondents (53.68%) cited ‘housewife’ as their occupation, followed by farmers (29.87%). About 70.13% of respondents were highly dependent on CWS to support their livelihoods. In all, 73.16% respondents reported that they collected medicinal plants from CWS, with the highest collection frequency being 1–2 times per month (62.13%) (Table 1).
Table 1.
Basic demographic features of surveyed 231 respondents living in and around Chunati Wildlife Sanctuary
| Parameter | Categories | Number of respondents | Percentage of respondents |
|---|---|---|---|
| Sex | Male | 103 | 44.59 |
| Female | 128 | 55.41 | |
| Age class (year) | 30–40 | 71 | 30.74 |
| 41–50 | 106 | 45.89 | |
| 51–60 | 41 | 17.75 | |
| > 60 | 13 | 5.63 | |
| Educational qualification | Illiterate/can sign | 567 | 24.68 |
| Primary | 145 | 62.77 | |
| Junior | 22 | 9.52 | |
| Secondary | 4 | 1.73 | |
| Higher Secondary | 3 | 1.30 | |
| Occupation | Housewife | 124 | 53.68 |
| Farmer | 69 | 29.87 | |
| Day labour | 15 | 6.49 | |
| Businessmen | 10 | 4.33 | |
| Others | 13 | 5.63 | |
| Forest dependency | High | 162 | 70.13 |
| Medium | 61 | 26.41 | |
| Low | 8 | 3.46 | |
| Collection of medicinal plants from forest | Yes | 169 | 73.16 |
| No | 62 | 26.84 | |
| Frequency of medicinal plants collection from forest | 1–2 times per month | 105 | 62.13 |
| 2–3 times per month | 41 | 24.26 | |
| 3–4 times per month | 23 | 13.61 |
Medicinal plant resources in CWS
From the household survey, the study documented 134 species of medicinal plants with curative values that were traditionally used by forest-dependent communities in and around CWS for their daily healthcare purposes (Table 2). Of the documented species, 37.31% species were trees, 28.36% species were herbs, and 20.15% species were shrubs (Fig. 2). Table 2 lists the botanical description of each species recorded, the plant parts used, the ailments treated, the usage pattern and the UV, FC and RFC values.
Table 2.
Details of 134 recorded medicinal plant species used by forest-dependent communities in and around Chunati Wildlife Sanctuary, Bangladesh
| Family | Local name | Scientific name | Life form | Habit | Plant parts used | Treating ailments | Mode of preparation and utilisation | UV | FC (%) | RFC (%) |
|---|---|---|---|---|---|---|---|---|---|---|
| Acanthaceae | Bashok | Adhatoda vasica Nees | Shrub | Forest, homestead forest, roadside | Leaf | Cough and cold, asthma, piles, pneumonia, malarial fever | Juice extracted by crushing leaves and heated slightly then drunk with honey | 0.31 | 1.78 | 0.61 |
| Kalomegh | Andrographis paniculata (Burm.f.) Nees | Herb | Forest | Whole plant | Fever, worms, dysentery, astringent, piles, physical weakness | Juice is made from plant parts and drunk | 0.24 | 1.36 | 0.47 | |
| Actinidiaceae | Bhola kadam | Saurauia roxburghii Wall | Tree | Forest | Leaf | Skin diseases | To treat boils, leaf infusion is used in baths | 0.08 | 0.48 | 0.16 |
| Alangiaceae | Akarkanta | Alangium salvifolium (L.f.) Wangerin | Tree | Forest | Fruit | Hair fall, dandruff | Paste made from leaves is rubbed on head for hair fall and dandruff problems | 0.07 | 0.39 | 0.13 |
| Amaranthaceae | Apang | Achyranthes aspera L. | Herb | Forest, homestead forest | Whole plant | Dysentery, piles, skin diseases, rheumatism, stop bleeding, cough and cold, fever, snake bite | Juice made from leaves and roots and drunk | 0.29 | 1.63 | 0.56 |
| Helencha | Alternanthera philoxeroides (Mart.) Griseb | Herb | Fallow land | Leaf | Dysentery, eye diseases, liver problems, jaundice | Leaves are cook and eaten as vegetables | 0.32 | 1.84 | 0.64 | |
| Kanta mali | Amaranthus spinosus L. | Herb | Forest, fallow land | Leaf, root | Stomach pain | Leaves and roots are crushed, made juice and drunk | 0.13 | 0.76 | 0.26 | |
| Amaryllidaceae | Piaj | Allium cepa L. | Herb | Homestead forest | Whole plant | Stomach pain, cough and cold, hair fall, dandruff | Rhizome are eaten as raw with salt; whole plant is used with curry | 0.35 | 2.01 | 0.70 |
| Rashun | Allium sativum L. | Herb | Homestead forest | Whole plant | Stomach pain, teeth ache, heart diseases, urinal problem, snake bite | Rhizome are eaten as raw with salt; whole plant is used with curry | 0.36 | 2.03 | 0.70 | |
| Anacardiaceae | Aam | Mangifera indica L. | Tree | Forest, homestead forest, roadside | Leaf, fruit, tender twig | Fat burning, teeth ache, cut and wounds, diabetes, dysentery, jaundice, asthma, piles, diarrhoea, cough and cold | Tender leaves are cook and eaten as vegetables; tender leaves are eaten mixing with salt; green and ripe fruits are eaten; tender twig used as toothbrush; paste made from leaves used on wounded place | 0.37 | 2.08 | 0.72 |
| Amra | Spondias pinnata (L.f.) Kurz | Tree | Forest, homestead forest | Fruit, bark | Fever, skin diseases, vitamin deficiencies, taste increaser | Green and ripe fruits are eaten; juice made from bark used on skin | 0.29 | 1.65 | 0.57 | |
| Lota aam | Mangifera sylvatica Roxb | Tree | Forest | Bark | Cough and cold, fever | Powder made from dry bark and mixed with honey | 0.15 | 0.88 | 0.30 | |
| Annonaceae | Ata | Annona squamosa L. | Tree | Forest, homestead forest | Leaf, fruit | Worms, vomiting | Juice of leaves are feed to children; ripe fruits are eaten | 0.27 | 1.54 | 0.53 |
| Apiaceae | Dhonia pata | Coriandrum sativum L. | Herb | Homestead forest | Leaf, seed, root | Stomach pain, digestive problem | Roots are crushed and eaten raw with sugar; seeds and leaves are used in curry | 0.34 | 1.94 | 0.67 |
| Thankuni | Centella asiatica (L.) Urban | Herb | Forest, homestead forest, fallow land | Whole plant | Diarrhoea, dysentery, gastritis, piles, tonic, hypertension | Whole plant is blended and eaten; green leaves are eaten as vegetables; green leaves also cooked and eaten as vegetables | 0.37 | 2.11 | 0.73 | |
| Apocynaceae | Chatim | Alstonia scholaris (L.) R.Br | Tree | Forest, roadside | Leaf, bark | Stimulate lactation, jaundice, malarial fever, snake bite | Juice made from crushing bark and leaves; bark exudates for snake bite | 0.27 | 1.51 | 0.52 |
| Kurchi | Holarrhena antidysenterica (L.) Wall. ex A. DC | Tree | Forest, fallow land | Whole plant | Dysentery, asthma, skin diseases, cut and wounds, fever, worms | Boiling with water and mixing with honey or sugar; bark and seeds paste are used in skin diseases; paste made from leaves are used on wounded place | 0.23 | 1.31 | 0.45 | |
| Rupatola | Tabernaemontana recurva Roxb. ex Lindl | Shrub | Forest | Root | Snake bite | Paste made from roots and placed around the place | 0.09 | 0.49 | 0.17 | |
| Akanda | Calotropis gigantea (L.) Dryand | Shrub | Forest, homestead forest, roadside | Leaf, latex | Cut and wounds, arthritis | Leaves are heated and placed on pain place; latex are placed on injured place | 0.36 | 2.05 | 0.71 | |
| Araceae | Kachu | Colocasia esculenta (L.) Schott | Shrub | Forest, homestead forest, fallow land | Whole plant | Eye diseases, anaemia, cut and wounds, stop bleeding, constipation, earache, mouth blow | Whole plant (leaves and rhizome) is used as vegetable; latex is placed on wounded place | 0.32 | 1.84 | 0.64 |
| Mankachu | Colocasia affinis Schott | Shrub | Forest, homestead forest, fallow land | Whole plant | Gout pain, constipation, rheumatism | Leaves are heated on fire and place in the affected area; leaves and rhizome are eaten as vegetable | 0.28 | 1.59 | 0.55 | |
| Arecaceae | Khejur | Phoenix dactylifera L. | Tree | Forest, homestead forest, roadside | Fruit, root | Worms, jaundice, constipation, | Juice is made by crushing roots and drunk; ripe fruits are eaten | 0.24 | 1.39 | 0.48 |
| Narikel | Cocos nucifera L. | Tree | Homestead forest | Fruit, root | Worms, jaundice, diarrhoea, hair fall, dandruff, burn, dysentery, physical weakness, skin diseases | Fleshy part of the fruit is mixed with water and sugar and taken in every morning; water of green coconut is drunk; oil made from fruits used in hair; paste made from roots used in the burnt places | 0.34 | 1.91 | 0.66 | |
| Supari | Areca catechu L. | Tree | Homestead forest, roadside | Root, seed | Worms, vomiting, sex stimulant, astringent, heart diseases, digestive problems | Roots are crushed and drunk mixing with sugar; raw and dried seeds are chew and eaten with betel leaf | 0.36 | 2.06 | 0.71 | |
| Asparagaceae | Shatomuli | Asparagus racemosus Willd | Climber | Forest | Leaf, root | Sexual weakness, sex stimulant, fever, dysentery | Juice made from roots and leaves are drunk regularly | 0.25 | 1.44 | 0.50 |
| Asteraceae | Assam lata | Mikania cordata (Burm.f.) B.L.Rob | Climber | Forest, homestead forest, roadside, fallow land | Whole plant | Cut and wounds, stop bleeding | Whole plant is squeezed and the juice is used externally on the wounded places | 0.37 | 2.08 | 0.72 |
| Assam pata | Chromolaena odorata (L.) R.M.King & H.Rob | Shrub | Forest, homestead forest, roadside, fallow land | Leaf | Cut and wounds, stop bleeding | Whole plant is squeezed and the juice is used externally on the wounded places | 0.35 | 2.01 | 0.70 | |
| Gendha ful | Tagetes erecta L. | Herb | Homestead forest | Leaf | Cut and wounds | Juice is made from leaves and placed over the wounded spot | 0.14 | 0.80 | 0.28 | |
| Shillata | Vernonia cinerea (L.) Less | Climber | Forest | Stem | Gastritis | Juice made from stem and drunk | 0.13 | 0.74 | 0.26 | |
| Tora gash | Blumea clarkei Hook. f | Herb | Forest | Leaf | Jaundice, bone fracture | To treat bone fracture, paste of leaves of these plants is applied to affected areas and bandaged tightly with a piece of coarse cloth for several days. To treat jaundice, pills prepared from the leaf paste are taken thrice daily | 0.09 | 0.49 | 0.17 | |
| Athyriaceae | Dhai sak | Diplazium esculentum (Retz.) Sw | Herb | Forest, fallow land | Leaf | Gastritis, eye diseases, stomach pain | Tender leaves are cooked and eaten as vegetables | 0.30 | 1.69 | 0.58 |
| Bignoniaceae | Thona | Oroxylum indicum (L.) Benth. ex Kurz | Tree | Forest | Bark, stem, seed | Jaundice, diarrhoea, scabies | Juice made and drunk directly | 0.11 | 0.60 | 0.21 |
| Bromeliaceae | Anarosh | Ananas comosus (L.) Merr | Herb | Homestead forest | Leaf, fruit | Worms, stomach pain, jaundice | Green and ripe fruits are eaten; tender leaves are crushed then feed to children | 0.30 | 1.73 | 0.60 |
| Cactaceae | Cactus | Cactus spp. | Cactus | Forest | Leaf | Blood pressure | Boiled water of leaves is drunk with sugar | 0.04 | 0.24 | 0.08 |
| Caesalpiniaceae | Daud pata | Cassia alata L. | Tree | Forest | Leaf | Scabies, eczema | Leaves are crushed, mixing with salt and kerosene and rubbed on wounded places | 0.07 | 0.39 | 0.13 |
| Sonalu | Cassia fistula (L.) Gaertn | Tree | Forest | Leaf | Ulcer, cut and wounds | Powder made from dry leaves and rubbed on wounded places; leaves are soaked in water and drunk for ulcer treatment | 0.23 | 1.31 | 0.45 | |
| Caricaceae | Pepe | Carica papaya L. | Shrub | Homestead forest | Fruit | Worms, dysentery, jaundice, stomach pain | Green ad ripe fruits are eaten; green fruits are cooked as vegetables | 0.36 | 2.05 | 0.71 |
| Caryophyllaceae | Ghima | Polycarpon prostratum (Forssk.) Asch. & Schweinf | Herb | Homestead forest, fallow land | Whole plant | Diarrhoea, dysentery, fever, gastritis, earache | Leaves are eaten as vegetables; juice made from whole plant is drunk; paste made from leaves used for earache | 0.33 | 1.88 | 0.65 |
| Combretaceae | Arjun | Terminalia arjuna (Roxb. ex DC.) Wight & Arn | Tree | Forest, homestead forest | Bark | Diabetes, stomach pain, taste increaser, fever, heart diseases, asthma, dysentery, digestive problem, hypertension, cough and cold, piles, burn | Boiled water of bark is drunk; keeping bark into water for 1 night then drunk; powder made from dry bark and mixing with honey | 0.38 | 2.14 | 0.74 |
| Bohera | Terminalia bellirica (Gaertn.) Roxb | Tree | Forest | Fruit, bark | Astringent, piles, constipation, gastritis, stomach pain, fever, jaundice, asthma, heart diseases | Fruits and bark are kept in water and drunk in every morning; made powder after crushing dried fruits | 0.34 | 1.93 | 0.67 | |
| Horitoki | Terminalia chebula Retz | Tree | Forest | Fruit | Astringent, piles, constipation, gastritis, stomach pain, fever, cough and cold, anaemia, dysentery, eye diseases, rheumatism, asthma | Fruits are kept in water and drunk in every morning | 0.34 | 1.91 | 0.66 | |
| Convolvulaceae | Kalmi sak | Ipomoea aquatica Forssk | Climber | Homestead forest, fallow land | Whole plant | Asthma, constipation, eye diseases | Eaten as vegetable; paste made from dry leaves | 0.37 | 2.11 | 0.73 |
| Misti alu | Ipomea batatus (L.) Lam | Climber | Homestead forest | Leaf, rhizome | Urinal problem, jaundice, rheumatism | Leaves are eaten as vegetable; rhizome also eaten raw | 0.31 | 1.79 | 0.62 | |
| Swarno lata | Cuscuta reflexa Roxb | Climber | Forest, homestead forest | Whole plant | Cough and cold, gastritis | Whole plants are crushed and feed cow; juice feed to children | 0.23 | 1.30 | 0.45 | |
| Voi kumra | Ipomoea mauritiana Jacq | Climber | Forest | Root | Cough and cold, tonic, alterative, demulcent, digestive problem | Juice made from root | 0.16 | 0.89 | 0.31 | |
| Crassulaceae | Pathorkuci | Bryophyllum pinnatum (Lam.) Oken | Herb | Forest, homestead forest | Leaf | Cough and cold | Juice made from tender twig are feed to the children for cold ailments | 0.25 | 1.40 | 0.48 |
| Cucurbitaceae | Korolla | Momordica charantia L. | Climber | Homestead forest | Leaf, fruit | Arthritis, digestive problem, constipation, blood purification | Eaten as vegetables; leaves are crushed and placed on wounded place | 0.35 | 2.01 | 0.70 |
| Lau | Lagenaria siceraria (Molina) Standl | Climber | Homestead forest | Whole plant | Diarrhoea, worms, constipation | Fruits and leaves are used as vegetable; juice made from roots are taken for worm diseases | 0.35 | 2.01 | 0.70 | |
| Misti kumra | Cucurbita moschata Duchesne ex Poir | Climber | Homestead forest | Whole plant | Worms, skin diseases | Fruits and leaves are used as vegetable; juice made from roots are taken for worm diseases | 0.35 | 2.01 | 0.70 | |
| Telakucha | Coccinia cordifolia (L.) Cogn | Climber | Forest, homestead forest, roadside | Leaf | Cough and cold, diabetes, hair fall, dandruff | Taken as vegetables after cooking; leaves are crashed and placed in head skin | 0.22 | 1.26 | 0.44 | |
| Dilleniaceae | Chalta | Dillenia indica L. | Tree | Forest, homestead forest | Leaf, fruit | Sex stimulant | Juice obtained from crushed leaves is taken once daily; fruits cooked as curry | 0.27 | 1.53 | 0.53 |
| Dipterocarpaceae | Garjan | Dipterocarpus turbinatus C.F. Gaertn | Tree | Forest | Latex | Diarrhoea | Latex is eaten with honey | 0.14 | 0.79 | 0.27 |
| Ebenaceae | Deshi gab | Diospyros peregrina (Gaertn.) Gürke | Tree | Forest, homestead forest | Fruit | Dysentery | Fruits are squeezed and taken with sugar; ripe fruits are eaten | 0.29 | 1.63 | 0.56 |
| Elaeocarpaceae | Jalpai | Elaeocarpus robustus Roxb | Tree | Forest, homestead forest | Fruit | Vitamin deficiencies, cough and cold, taste increaser | Raw fruits are eaten with salt; also used in curry | 0.33 | 1.89 | 0.65 |
| Euphorbiaceae | Bon morich | Croton bonplandianus Baill | Shrub | Forest, roadside, fallow land | Leaf, flower | Anti-allergic, teeth ache, headache, asthma, skin diseases | Paste made from flower and leaves placed over affected place; juice made from leaves sometimes used for head pain with coconut oil | 0.22 | 1.25 | 0.43 |
| Gundi gach | Mallotus roxburghianus Muell. Arg | Tree | Forest | Leaf, root | Dysentery, jaundice | Fruits are boiled and taken as vegetables; paste made from leaves | 0.09 | 0.51 | 0.18 | |
| Patabahar | Cobiaeum variegatum (L.) A.Juss | Shrub | Homestead forest | Leaf | Cut and wounds | Juice made from leaves | 0.16 | 0.90 | 0.31 | |
| Pitali | Trewia nudiflora L. | Tree | Forest | Leaf | Cut and wounds | Juice made from leaves | 0.20 | 1.15 | 0.40 | |
| Fabaceae | Arol | Cajanus cajan (L). Millsp. | Shrub | Forest, homestead forest | Leaf, seed | Jaundice, gout pain | Juice made from leaves; leaves are heated and rubbed on affected place; seeds cooked as vegetables | 0.27 | 1.54 | 0.53 |
| Mandar | Erythrina variegata L. | Tree | Forest, homestead forest | Bark | Worms, gastritis, sexual weakness, jaundice, stimulate lactation | Bark are crashed and juice is also used | 0.19 | 1.08 | 0.37 | |
| Shim | Phaseolus vulgaris L. | Climber | Homestead forest | Leaf, seed | Scabies, earache | Dried seeds are crushed and made paste with water then applied on wounded place; the decoction of leaves and roots are heated slightly, and the warm liquid is poured into the ear in case of ear pain | 0.35 | 2.01 | 0.70 | |
| Sisoo | Dalbergia sissoo DC | Tree | Forest, roadside | Leaf | Cut and wounds | Tender leaves are squeezed and juice placed in affected area | 0.13 | 0.71 | 0.25 | |
| Gentianaceae | Cirota | Swertia chirata Buch.-Ham. ex Wall | Herb | Forest | Branch | Fever, taste increaser, physical weakness, stomach pain, blood poisoning, malarial fever | Branches are cut into small pieces and soaked on water for drinking in the morning | 0.33 | 1.89 | 0.65 |
| Lamiaceae | Dondokolos | Leucas aspera Link | Herb | Forest | Leaf | Pneumonia | Extracted juice from leaves | 0.20 | 1.15 | 0.40 |
| Pudina pata | Mentha piperita L. | Herb | Homestead forest | Leaf | Dysentery, tonic | Leaves are crushed and taken with rice as vegetables | 0.25 | 1.40 | 0.48 | |
| Gamar | Gmelina arborea (Roxb.) ex Sm | Tree | Forest, homestead forest | Leaf | Hair fall, dandruff | Juice is extracted by blending leaves then rubbed on hair | 0.10 | 0.58 | 0.20 | |
| Vatpata | Clerodendrum viscosum Vent | Shrub | Forest, homestead forest, roadside | Leaf, branch, root | Stomach pain, vomiting, earache, fever | Tender leaves, branches and roots are squeezed and juice taken with sugar | 0.26 | 1.50 | 0.52 | |
| Tukma | Hyptis suaveolens (L.) Poit | Herb | Forest, homestead forest | Seed | Urinary problem, stomach pain, constipation, sexual weakness, fever | Seeds are soaked in water and taken in the morning | 0.33 | 1.89 | 0.65 | |
| Tulsi | Ocimum sanctum L. | Herb | Forest, homestead forest | Leaf, seed | Cough and cold, cut and wounds, constipation, antiseptic | Leaves are squeezed and taken with honey after heating; juice of leaves are placed on wounded place; seeds are soaked in water and taken in the morning | 0.36 | 2.03 | 0.70 | |
| Lecyphidaceae | Hizol | Barringtonia acutangula Gaertn | Tree | Forest | Bark | Physical weakness | Juice is made after boiling with water | 0.08 | 0.44 | 0.15 |
| Leguminosae | Tetul | Tamarindus indica L. | Tree | Forest, homestead forest | Leaf, fruit | Cough and cold, fever, loss of appetite, dysentery, lethargy to food | Water of boiled leaves is drunk; green and ripe fruits are eaten with salt | 0.34 | 1.94 | 0.67 |
| Minijiri | Senna siamea (Lamk.) Irwin & Barneby | Tree | Forest, homestead forest | Flower | Diabetes | Flowers are baked and eaten with rice | 0.22 | 1.23 | 0.42 | |
| Lozzabati | Mimosa pudica L. | Herb | Forest, roadside | Whole plant | Scabies, teeth ache, chicken pox, jaundice, sexual weakness | Leaves are crashed and paste is placed on wounded place, roots are used in sexual weakness and teeth ache | 0.35 | 2.01 | 0.70 | |
| Loranthaceae | Orsallu | Macrosolen cochinchinensis (Lour.) Teigh | Tree | Forest | Leaf | Jaundice | Fresh leaf juice is taken twice daily to treat jaundice | 0.06 | 0.36 | 0.13 |
| Parula | Scurrula parasitica L. | Shrub | Forest | Stem | Teeth ache | Cutting into small pieces, boiled and used for mouth wash | 0.06 | 0.35 | 0.12 | |
| Lythraceae | Mehendi | Lawsonia inermis L. | Shrub | Homestead forest | Leaf | Sexual weakness, sex stimulant, urinal problem, skin diseases, dandruff, hair fall, hair and beard colour, colouring nails and palm | Dry leaves are crushed and taken with water; paste made from leaves used in hair and skin | 0.34 | 1.95 | 0.68 |
| Dalim | Punica granatum L. | Shrub | Homestead forest | Fruit | Increase in red blood cell count | Ripe fruits are eaten and juice made by crushing it to drunk | 0.32 | 1.81 | 0.63 | |
| Malvaceae | Chatehata | Sida mysorensis Wight & Arn | Herb | Forest | Root | Piles, jaundice, malarial fever, diarrhoea | Juice after crushing root | 0.21 | 1.18 | 0.41 |
| Joba | Hibiscus rosa-sinensis L. | Shrub | Homestead forest | Leaf, flower | Dysentery, cut and wounds | Flowers are squeezed and taken with sugar; paste is made from young leaf | 0.22 | 1.28 | 0.44 | |
| Shimul | Bombax ceiba L. | Tree | Forest, homestead forest | Leaf, root | Worms, sexual weakness, sex stimulant | Juice made from roots and drunk. Leaves and roots are soaked in water overnight followed by drinking the water early in the morning | 0.22 | 1.24 | 0.43 | |
| Udal | Sterculia villosa Roxb | Tree | Forest | Leaf, tender twig | Dysentery, jaundice, rheumatism | Leaves are cut into small pieces and soaked into water; to treat rheumatism, water extract of petioles is given to drink with sugar | 0.23 | 1.30 | 0.45 | |
| Ulat kambal | Abroma augusta L. | Shrub | Forest | Bark, root | Dysmenorrhoeal, sexual weakness | Bark and roots are soaked into water and drunk | 0.15 | 0.88 | 0.30 | |
| Asar | Grewia paniculata Roxb | Shrub | Forest | Leaf | Cut and wounds | Paste made from leaves and rubbed on the wounded area | 0.15 | 0.86 | 0.30 | |
| Pisla | Grewia nervosa (L.) G.Panigrahi | Shrub | Forest | Latex | Diarrhoea, dysentery | Latex is taken with honey | 0.13 | 0.74 | 0.26 | |
| Melastomataceae | Bontej pata | Melastoma malabathricum L. | Shrub | Forest, roadside, fallow land | Leaf, fruit, bark, flower | Dysentery, diarrhoea, skin diseases | Leaves, flowers, barks and fruits are cut and crushed for making paste and juice | 0.22 | 1.26 | 0.44 |
| Meliaceae | Neem | Azadirachta indica A. Juss | Tree | Forest, homestead forest | Leaf, tender twig, bark | Chicken pox, teeth ache, fever, asthma, worms, skin diseases, antiseptic, rheumatism | Bath with boiled leaves water; teeth are brushed with twigs; dry leaves and bark are eaten with honey after making powder | 0.39 | 2.21 | 0.77 |
| Menispermaceae | Gulanci lata | Tinospora cordifolia Miers | Climber | Forest | Leaf, tender twig | Arthritis, fever | Boiling with water | 0.13 | 0.76 | 0.26 |
| Moraceae | Dumur | Ficus roxburghii Wall. ex Steud | Tree | Forest, homestead forest | Fruit | Dysentery, diabetes | Fruits are eaten as vegetables | 0.25 | 1.43 | 0.49 |
| Fala | Ficus racemosa L. | Tree | Forest | Root | Tonsillitis | Juice made from root and eaten with rice | 0.06 | 0.31 | 0.11 | |
| Kanthal | Artocarpus heterophyllus Lamk | Tree | Forest, homestead forest | Fruit, latex, seed | Skin diseases, eczema, constipation, stomach pain | Latex is placed on wounded place; fruits are eaten as raw; seeds are eaten after baked | 0.38 | 2.15 | 0.74 | |
| Khaiz bichi | Ficus religiosa L. | Tree | Forest | Leaf | Tonsillitis | Paste made from leaves and roots then place on wounded place | 0.05 | 0.30 | 0.10 | |
| Shewra | Streblus asper Lour | Tree | Forest, homestead forest, roadside | Leaf, latex | Scabies, dysentery, skin diseases, arthritis, female sexual disorders | Paste made from leaves are placed on wounded place; latex of leaves is eaten with honey; juice made from leaves is drunk for dysentery | 0.29 | 1.64 | 0.57 | |
| Moringaceae | Sojina | Moringa oleifera Lamk | Tree | Homestead forest | Leaf, fruit | Dysentery, malarial fever, arthritis, sexual weakness | Leaves and fruits are eaten as vegetable, juice from leaves is drunk | 0.33 | 1.89 | 0.65 |
| Musaceae | Kola | Musa sapientum L. | Shrub | Forest, homestead forest | Whole plant | Dysentery, cut and wounds, anaemia | Inner part of bark is eaten as vegetables; fruits are eaten raw; roots are crushed and given on wounded place | 0.37 | 2.09 | 0.72 |
| Myrtaceae | Eucalyptus | Eucalyptus camaldulensis Dehnh | Tree | Forest, homestead forest, roadside | Leaf, bark | Malarial fever, hair fall, dandruff | Soaked on water for a night then eaten with honey; oil from leaves used in hair | 0.07 | 0.41 | 0.14 |
| Guava | Psidium guajava L. | Tree | Forest, homestead forest | Leaf, fruit | Stomach pain, vitamin deficiencies, dysentery, diarrhoea, fever, cut and wounds | Juice made from tender leaves are taken; fruits are eaten for deficiency of vitamin C, juice made from young leaves are placed on wounded place | 0.39 | 2.23 | 0.77 | |
| Jam | Syzygium cumini (L.) Skeels | Tree | Forest, homestead forest | Fruit, seed | Typhoid, diabetes, blood purification | Fruits are eaten raw; powder made from dry seeds and mixed with honey | 0.32 | 1.83 | 0.63 | |
| Puti jam | Syzygium fruticosum DC | Tree | Forest | Fruit | Fever | Eaten raw | 0.26 | 1.49 | 0.52 | |
| Oxalidaceae | Kamranga | Averrhoa carambola L. | Tree | Forest, homestead forest | Fruit | Jaundice, hair fall, Datura poisoning, physical weakness, constipation, diarrhoea, vitamin deficiencies | Green and ripe fruits are eaten; juice made from fruits and drunk | 0.31 | 1.78 | 0.61 |
| Papveraceae | Shial kanta | Argemone mexicana L. | Herb | Forest, roadside, fallow land | Leaf | Dysentery, cut and wounds | Leaves are eaten as vegetables | 0.09 | 0.51 | 0.18 |
| Phyllanthaceae | Lotkon | Baccaurea ramiflora Lour | Tree | Forest | Fruit | Headache, stomach pain | Ripe fruits are eaten; fruits washed water is drunk for stomach problem | 0.23 | 1.33 | 0.46 |
| Amloki | Phyllanthus emblica L. | Tree | Forest, homestead forest | Leaf, fruit | Astringent, constipation, gastritis, stomach pain, fever, jaundice, skin diseases, hair fall, digestive problem | Fruits and leaves are kept in water and drunk in every morning | 0.34 | 1.94 | 0.67 | |
| Piperaceae | Paan | Piper betle L. | Climber | Forest | Tender twig | Cut and wounds, loss of appetite, dysentery, indigestion, stomach pain, sex stimulant | Leaves are crushed and applied in wounded area; green leaves are eaten with betel nut | 0.38 | 2.16 | 0.75 |
| Plantaginaceae | Isopgul | Plantago ovata Forssk | Herb | Homestead forest | Seed | Constipation | Seeds are kept in water then drunk in the morning | 0.34 | 1.95 | 0.68 |
| Brahmmi sak | Bacopa monniera (L.) Pennell | Herb | Forest, homestead forest, roadside, fallow land | Leaf, seed | Cough and cold, fever, asthma, mental depression, heart diseases | Juice from leaves for drunk; green leaves cooked as vegetables; seeds are used in curry | 0.25 | 1.44 | 0.50 | |
| Poaceae | Akh | Saccharum bengalense Retz | Shrub | Homestead forest | Stem | Jaundice | Stem is eaten and made juice by crushing it to drunk | 0.31 | 1.76 | 0.61 |
| Durba grass | Cynodon dactylon (L.) Pers | Grass | Forest, homestead forest, roadside, fallow land | Whole plant | Cut and wounds, stop bleeding, diabetes, teeth ache | The paste made from whole plant is placed in the wounded places | 0.40 | 2.29 | 0.79 | |
| Goicha | Paspalum scrobiculatum L. | Herb | Forest | Leaf | Skin diseases | Leaves are squeezed and given between fingers of toe | 0.07 | 0.43 | 0.15 | |
| Bansh | Bambusa spp. | Grass | Forest, homestead forest | Leaf, bark | Teeth ache, cut and wounds, stop bleeding | Boiled water of leaves are used for teeth ache; green portion of bark is used for stopping bleeding | 0.25 | 1.41 | 0.49 | |
| Polygonaceae | Bon palong | Rumex dentatus L. | Herb | Forest, fallow land | Leaf, stem | Anti-allergic, fever, scabies | Soup is made from leaves and used to prevent fever; leaves also used for scabies; stem is used as anti-allergic | 0.17 | 0.99 | 0.34 |
| Rhamnaceae | Boroi | Zizyphus mauritiana Lamk | Tree | Forest, homestead forest | Fruit | Fever, cough and cold, digestive problem | Green and ripe fruits are eaten | 0.34 | 1.94 | 0.67 |
| Rubiaceae | Bishma | Hydyotis scandens Roxb | Herb | Forest | Leaf | Stomach pain | Infusion of leaves is taken 2–3 times a day to treat stomach pain | 0.07 | 0.40 | 0.14 |
| Haru lodi | Tarenna campaniflora (Hook. f.) N.P. Balak | Tree | Forest, homestead forest | Leaf, fruit, root | Eczema, diarrhoea, fever, scabies | Leaves extract is applied externally in the affected area to treat eczema; root extract is given to drink to treat abdominal pain caused by diarrhoea; root extract is given to drink to treat fever; leaf infusion is used for bathing to treat scabies | 0.21 | 1.20 | 0.42 | |
| Kodom ful | Anthocephalus chinensis (Lamk.) A. Rich. ex Walp | Tree | Forest, homestead forest, roadside | Leaf | Arthritis, cut and wounds, skin diseases | Paste made from leaves are placed on the affected area | 0.21 | 1.21 | 0.42 | |
| Gandha bhaduli | Paederia foetida L. | Herb | Forest, roadside | Tender twig; rhizome | Arthritis, fever | Twigs are boiling with water and used externally; rhizome is eaten raw with salt | 0.20 | 1.16 | 0.40 | |
| Rutaceae | Baruna shak | Zanthoxylum budrunga DC | Herb | Forest, homestead forest | Whole plant | Jaundice | Cooked and eaten as vegetables | 0.23 | 1.30 | 0.45 |
| Batabi lebu | Citrus maxima (Burm.) Merr | Shrub | Homestead forest | Fruit | Cough and cold, vitamin deficiencies | Ripe fruits are eaten; juice made from fruits to drunk | 0.24 | 1.38 | 0.48 | |
| Bel | Aegle marmelos (L.) Correa ex Roxb | Tree | Forest, homestead forest | Leaf, fruit | Dysentery, stomach pain, worms, diarrhoea, physical weakness, constipation, | Fleshy soft part of ripe fruit is eaten; young leaves are eaten | 0.34 | 1.93 | 0.67 | |
| Jambura | Citrus grandis (L.) Osb | Shrub | Homestead forest | Fruit | Dysentery, fever, jaundice, lethargy to food, vitamin deficiencies | Ripe fruits are eaten; juice made from fruits to drunk | 0.31 | 1.76 | 0.61 | |
| Lebu | Citrus limon (L.) Burm. f | Shrub | Forest, homestead forest | Leaf, fruit | Vitamin deficiencies, cut and wounds, liver problems, snake bite, lethargy to food, physical weakness | Green and ripe fruits are eaten; juice made from fruits to drunk; green leaves are eaten; green leaves also used in curry | 0.32 | 1.81 | 0.63 | |
| Motkila pata | Glycosmis pentaphylla (Retz.) A. DC | Herb | Forest | Leaf | Jaundice, cough and cold, cut and wounds | Juice made from leaves are used for jaundice and cough and cold; paste is used on cut and wounded place | 0.23 | 1.31 | 0.45 | |
| Smilacaceae | Kumarilata | Smilax macrophylla Poepp. ex A.DC | Climber | Forest | Leaf | Sexual weakness, sex stimulant | Juice from top tender leaves are eaten raw | 0.22 | 1.26 | 0.44 |
| Solanaceae | Dhutura | Datura innoxia Mill | Herb | Forest | Leaf, seed, fruit | Gout pain, dog bite, diarrhoea, dysentery, mental depression | Leaves and fruit are heated on fire and place on affected place; seeds are eaten with betel leaf; grinding to make juice | 0.21 | 1.19 | 0.41 |
| Kanta morich | Solanum surattense Burm.f | Herb | Forest, fallow land | Leaf, root | Gastritis, worms, dysentery, bee sting | Juice made from leaves and roots are used for gastritis and worms; leaves also eaten as vegetables | 0.13 | 0.76 | 0.26 | |
| Kantakari | Solanum xanthocarpum Schrad. & Wendl | Herb | Forest | Leaf, tender twig | Sexual weakness, hair fall, dandruff | Plant parts are boiled for drunk; fresh juice of leaves applied on head to prevent hair fall and removes dandruff | 0.09 | 0.50 | 0.17 | |
| Morich | Capsicum annuum L. | Herb | Homestead forest | Fruit | Mouth blow, eye disease, bee sting | Green and ripe fruits are eaten and sued in curry; dried fruits are used in curry also made powder after crushing | 0.39 | 2.20 | 0.76 | |
| Tit begun | Solanum violaceum Ortega | Shrub | Forest, fallow land | Fruit | Dysentery | Fruits are cooked and eaten as vegetables | 0.25 | 1.40 | 0.48 | |
| Theaceae | Cha gach | Camellia sinensis O. Kuntze | Shrub | Forest | Leaf | Teeth ache | Green leaves are chewed for tooth ache; green leaves are mixed with smashed potato and eaten as vegetables | 0.13 | 0.71 | 0.25 |
| Verbenaceae | Lantana | Lantana camara L. | Shrub | Homestead forest, roadside, fallow land | Leaf, stem | Antiseptic, arthritis, skin diseases, stop bleeding | Leaves are used for antiseptic and skin diseases; crushed leaves and stems are used for arthritis and stop bleeding | 0.25 | 1.41 | 0.49 |
| Vitaceae | Harzora lata | Cissus quadrangularis Linn | Climber | Forest | Stem | Bone fracture, blood pressure | Paste made of blended climbers is placed on broken place and bandaged | 0.28 | 1.56 | 0.54 |
| Zingiberaceae | Ada | Zingiber officinale Roscoe | Herb | Homestead forest | Rhizome | Gastritis, stomach pain, cough and cold, tonsillitis, vomiting, teeth ache, cut and wounds, hypertension | Rhizome eaten raw with salt; rhizome paste used in curry | 0.36 | 2.04 | 0.71 |
| Bhulchengi | lpinia nigra (Gaertn.) B.L.Burtt | Herb | Forest | Root | Jaundice, gastritis | Roots extract is taken thrice daily to treat jaundice; for gastritis, decoction of roots is taken twice daily | 0.07 | 0.40 | 0.14 | |
| Go-ada | Zingiber zerumbet (L.) Sm | Herb | Forest, fallow land | Rhizome | Gastritis, diarrhoea, dysentery | Rhizome eaten raw with salt; rhizome paste used in curry | 0.15 | 0.84 | 0.29 | |
| Holud | Curcuma longa L. | Herb | Homestead forest | Rhizome | Blood purification, skin diseases, gastritis | Rhizome crushed and eaten; rhizome paste used in curry; rhizome paste mixed with milk and drunk | 0.36 | 2.04 | 0.71 |
UV use value, FC frequency of citation, RFC relative frequency of citation
Fig. 2.
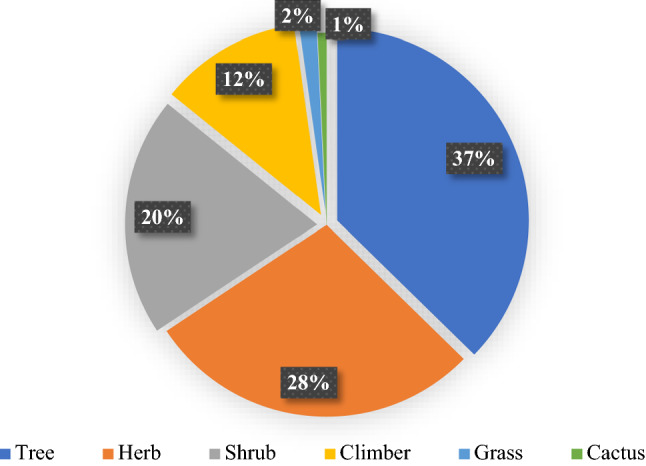
Life form categorisation of recorded medicinal plant from Chunati Wildlife Sanctuary
The 134 species recorded belong to 60 families. The highest number of species belonged to the Malvaceae family with seven species; followed by the Lamiaceae and Rutaceae families (six species each); the Moraceae, Solanaceae and Asteraceae families (five species each); and the Apocynaceae, Convolvulaceae, Cucurbitaceae, Euphorbiaceae, Fabaceae, Myrtaceae, Poaceae, Rubiaceae and Zingiberaceae families (four species each) (Fig. 3 and Online Resource 2).
Fig. 3.
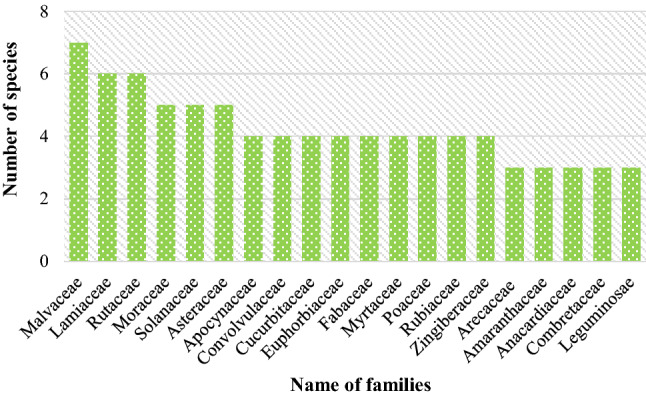
Dominant families of recorded medicinal plant species
Sources and mode of preparation and utilisation of recorded medicinal plants
About half the medicinal plant species (46.02%) were collected from CWS, as reported by respondents, followed by 34.07% plant species from their homestead forest (Fig. 4). People harvested medicinal plants from CWS throughout the year but mostly in the winter and summer seasons and less in monsoon. Due to heavy rainfall and the chance of landslides, it was extremely difficult to enter CWS in the monsoon season for medicinal plant harvesting. Both the above-ground and below-ground plant parts were used to prepare medicine from plants. In most cases, different plant parts from the same plant were used to prepare medicine to treat different ailments in respondents’ everyday healthcare. In other cases, similar or different parts of more than one plant were mixed to prepare medicine to treat a single ailment. Based on the field survey, leaves from 66 medicinal plant species were used to prepare medicine. These also comprised fruits from 33 species, roots from 18 species, bark from 13 species, and seeds from 11 species (Fig. 5).
Fig. 4.
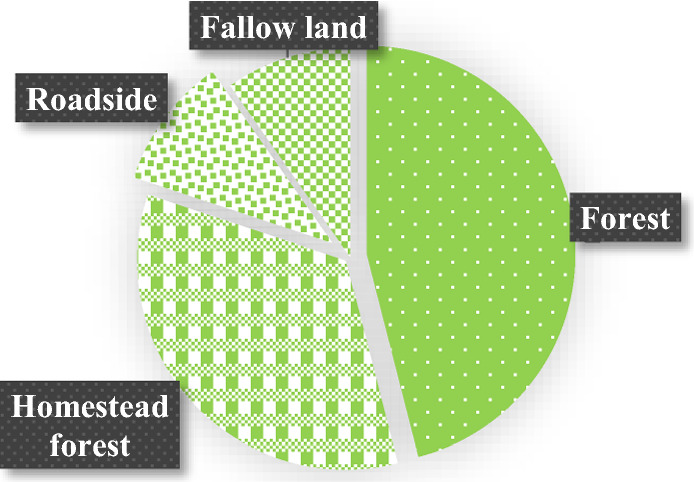
Sources of recorded medicinal plant species
Fig. 5.
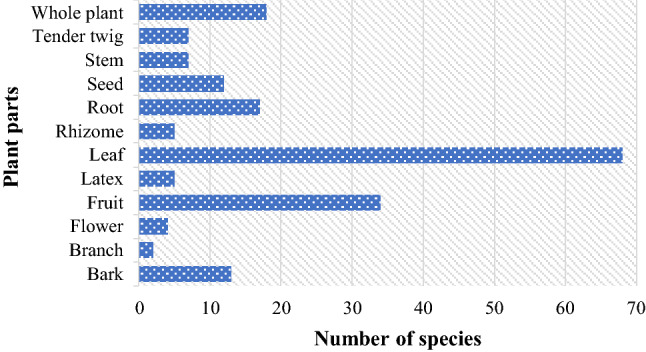
Distribution of plant parts used for preparing medicine from recorded medicinal plant species
Generally, respondents made juice after processing, with this involving pasting, squeezing and blending leaves, rhizomes, bark and roots to use as medicine, while fresh and ripened fruits (Mangifera indica, Spondias pinnata, Ammona squamosa, Phoenix dactylifera, Averrhoa carambola, Ananas comosus, Carica papaya, etc.) were eaten. Sometimes plant parts (Bombax ceiba, Terminalia bellirica, T. chebula, Plantago ovata, Phyllanthus emblica, Hyptis suaveolens, Ocimum sanctum, Swertia chirata, etc.) were soaked in water either for the person to drink on an empty stomach in the morning or to soften the skin before being eaten. Most plant parts were consumed orally or were used by rubbing or burning; some were taken raw after being soaked or boiled in water; while some were eaten after being cooked as vegetables, particularly the herbs (Alternanthera philoxeroides, Diplazium esculentum, Polycarpon prostratum, etc.), shrubs (Colocasia affinis, C. esculenta, Cajanus cajan, etc.) and climbers (Ipomoea aquatic, I. balatus, Momordica charantia, Lagenaria siceraria, etc.). Medicines prepared from plant parts were sometimes applied externally to wounded or sore body parts to treat cuts and wounds, scabies, pain or skin diseases. Fresh plant parts were used to prepare medicine; dried parts were also used when fresh was not available. In some cases, dried fruits and seeds (T. belerica, Areca catechu, Phaseolus vulgaris, Capsicum annuum, etc.) were used to prepare medicine (Table 2). However, the dosage pattern varied with the age of the patient, severity of the ailment and mode of medicine preparation by the practitioner.
Traditional uses of medicinal plant species for curing ailments
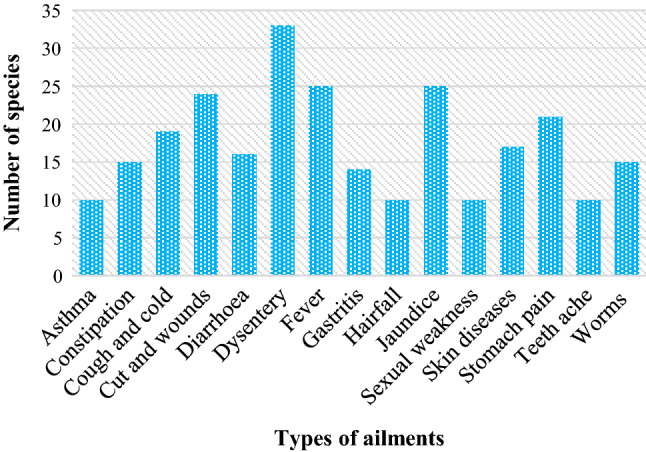
Figure 6 shows the traditional uses of plant species for treating 71 types of ailments. In summary, respondents cited a total of 454 times in which they treated 71 ailments. Trees were dominant (44.71%) for treating ailments, followed by herbs (27.97%), shrubs (15.20%), climbers (10.35%), grasses (1.54%) and cacti (0.22%) (Online Resource 3). Among the recorded species, 33 species were used to treat dysentery, 25 each for fever and jaundice, 24 for cuts and wounds, 21 for stomach pain, 19 for coughs and colds, 17 for skin diseases, 16 for diarrhoea and 15 each for constipation and worms. One species was used to treat each of the following 14 ailments: as an alterative, increase in red blood cell count, blood poisoning, colouring nails and palm, Datura poisoning, as a demulcent, dog bite, dysmenorrhoea, fat burning, female sexual disorders, hair and beard colour, indigestion, typhoid and ulcers. Furthermore, more than one species was used to treat the remaining 57 ailments (Online Resource 3).
Fig. 6.
Dominant uses of recorded medicinal plant species for treating different ailments
Cultural and traditional beliefs regarding medicinal plants’ conservation
Input from the FGDs on cultural and traditional beliefs regarding medicinal plant conservation was evaluated. Participants stated that some important medicinal plant species, such as Aegle marmelos, A. indica, Cocos nucifera, Hibiscus rosa-sinensis, Hyptis suaveolens, Lawsonia inermis, M. indica, M. sapientum, O. sanctum, P. betle, P. ovata, Punica granatum, Tagetes erecta and Zizyphus mauritiana were regarded as culturally significant and traditionally sacred plants by the Hindu and Muslim religious communities in the studied forest-dependent villages. Hindu communities used parts of some of these plants, such as Anthocephalus chinensis, A. marmelos, C. nucifera, Colacasia esculenta, H. rosa-chinenesis, M. indica, M. sapientum, O. sanctum, P. betle and P granatum during their worship; consequently, they planted and conserved these specific species in their homestead forest. Moreover, worship by members of the Hindu community involved the whole O. sanctum plant every morning and evening, with the earth around the base of this species kept neat and clean, with regular mud paste added by older women. The Muslim community used the leaves of the Z. mauritiana species to shower the dead body before its burial.
The FGD participants also advised that the orange colour from the paste of the leaves of L. inermis was often used to colour the palms of the hands of both the bride and groom and of women and children on cultural, ceremonial and religious occasions in Muslim, Hindu and Christian religious communities. People in Bangladesh, including in the study area, used paste made from leaves to colour hair and fingernails (for both men and women) and men’s beards. The yellow paste made from the Curcuma longa rhizome was used to colour the whole body of both the bride and groom in Muslim, Hindu and Christian communities. During the entire wedding ceremony (from pre- to post-ceremony), a plate (dala) was decorated nicely with colourful patterns containing grains from Areca catechu, C. dactylon, P. betle, C. longa and Oryza sativa as a sign of purity and piousness. It was presented with a flaming light as everybody blessed the bridal couple.
Findings from the FGDs also revealed that most people planted some species with valuable medicinal properties, such as Areca catechu, A. indica, Citrus grandis, C. limon, C. nucifera, Elaeocarpus robustus, Lawsonia inermis, M. indica and O. sanctum, in their homestead forests. A. indica, in particular, was usually planted on the southern side of homesteads, purifying the air from the south side with its foliage. A. marmelos, Bambusa spp., C. nucifera, Ricinus communis, Streblus asper and Tamarindus indica were planted on the periphery of homestead forests, based on the belief that evil spirits take shelter in tree foliage. Some species, such as Kalanchoe pinnata, Cobiaeum variegatum, H. rosa-chinenesis and Tagetes erecta, serving both beautification and medicinal purposes, were grown and maintained in front of dwelling houses. People also created living fences by planting H. rosa-chinenesis surrounding their homesteads. A. indica and C. papaya were planted in homestead forests to prevent ailments from entering. Similar beliefs were also reported by people in other areas of Bangladesh, as mentioned by Chowdhury et al. (2009) and Rahman (2013).
Quantitative status of recorded medicinal plants
Use value and relative frequency of citation
The average UV score in the present study was 0.24 and ranging between 0.04 and 0.40. Based on UV scores, the ethnomedicinal plant species most commonly used was Cynodon dactylon (UV 0.40); followed by A. indica, C. annuum and Psidium guajava (UV 0.39 each); Piper betle, Artocarpus heterophyllus and T. arjuna (UV 0.38 each); and I. aquatic, Centella asiatica, Musa sapientum, M. indica and Mikania cordata (UV 0.37 each) (Table 2). The least used species were Ficus racemosa (UV 0.06), F. religiosa (UV 0.05) and Cactus spp. (UV 0.04). Most species with higher UV scores were used for diverse purposes, including treating cuts and wounds; diarrhoea; dysentery; fever; coughs and colds; stomach pain; toothache; vitamin deficiencies; to stop bleeding; diabetes; chicken pox; worms; heart diseases; digestive problems; hypertension; constipation; asthma; skin diseases, etc. The three species with the lowest UV scores were solely used to treat tonsillitis and blood pressure.
On the other hand, the average RFC value in this study was found 0.47%, with this score ranging from 0.08 to 0.79%. The highest RFC value was recorded for C. dactylon (0.79%); followed by P. guajava and A. indica (0.77% each); C. annuum (0.76%); P. betle (0.75%); A. heterophyllus and T. arjuna (0.74% each); I. aquatic and C. asiatica (0.73% each); and M. sapientum, M. indica and M. cordata (0.72% each) (Table 2).
Informant consensus factor
The reported ailments were first classified into 21 different ailment categories based on their use reports to calculate the ICF, with the recorded plant species distributed according to these categories. The average ICF value for all categories was 0.99 (ranging from 0.99 to 1.00). The highest ICF values were found for female sexual disorders, heart diseases, lactation, mental disorders, and urinary and rectal diseases (1.00 each) (Table 3). This may be due to the small number of species (ranging from only one to four species) used to treat these ailment categories.
Table 3.
Ailments grouped by major ailment categories, ICF values and medicinal plants used to treat these major ailments
| Ailment categories | Common ailments and features | No. of species | ICFa | Most frequently cited plants |
|---|---|---|---|---|
| Dental care | Teeth ache and decay, mouth blow, bad breath, mouth sores | 12 (2.67) | 0.99 | Cynodon dactylon, Azadirachta indica |
| Dermatological problems | Cut and wounds, burn, scabies, chickenpox, eczema, itching, allergic, astringent, prickly heat | 63 (14.03) | 0.99 | Cynodon dactylon, Psidium guajava |
| Ear nose throat problems | Earache, tonsillitis | 6 (1.34) | 0.99 | Zingiber officinale, Phaseolus vulgaris |
| Endocrinal disorders | Diabetes | 7 (1.56) | 0.99 | Cynodon dactylon, Terminalia arjuna |
| Female sexual disorders | Dysmenorrhoeal, excessive vaginal discharge, severe bleeding in vagina | 2 (0.45) | 1.00 | Streblus asper |
| Fever | Fever, malarial fever, typhoid | 33 (7.35) | 0.99 | Psidium guajava, Azadirachta indica |
| Gastrointestinal disorders | Gastric irritation and disorders, ulcer and peptic ulcer, constipation, diarrhoea, dysentery, digestive problem, dysentery, indigestion, vomiting, piles, lethargy to food | 102 (22.72) | 0.99 | Psidium guajava, Piper betle, Terminalia chebula |
| General health | High blood pressure, hypertension, blood purification, headache, fat burning | 11 (2.45) | 0.99 | Terminalia arjuna, Centella asiatica |
| Hair growth | Hair colour, hair fall or loss, dandruff | 19 (4.23) | 0.99 | Allium cepa, Lawsonia inermis |
| Heart diseases | Abnormal heartbeats, heart failure, heart attack | 5 (1.11) | 0.99 | Terminalia arjuna, Areca catechu |
| Helminthiasis | Ringworm, tapeworm, roundworm | 15 (3.34) | 0.99 | Azadirachta indica, Areca catechu |
| Inflammation and pain | Arthritis, alterative, stomach pain, gout pain, rheumatism, demulcent, stop bleeding, bone fracture | 49 (10.91) | 0.99 | Psidium guajava, Azadirachta indica |
| Lactation | Enhance milk secretion | 2 (0.45) | 1.00 | Alstonia scholaris |
| Liver disorders | Jaundice, abdominal pain and swelling, loss of appetite | 29 (6.46) | 0.99 | Piper betle, Mangifera indica |
| Mental disorders | Depression, anxiety, nervous illness | 2 (0.45) | 1.00 | Bacopa monniera |
| Nutritional deficiencies | Anaemia, tonic, vitamin deficiencies, blood increaser, physical weakness, taste increaser | 25 (5.57) | 0.99 | Psidium guajava, Terminalia arjuna |
| Respiratory complaints | Cough and cold, tuberculosis, asthma, bronchitis, pneumonia, influenza, nasal catarrh | 31 (6.90) | 0.99 | Azadirachta indica, Terminalia arjuna |
| Sexual disorders | Sexual weakness, sex stimulant | 17 (4.01) | 0.99 | Piper betle, Areca catechu |
| Toxicity complaints | Snake bite, blood poisoning, bee sting, dog bite, Dhatura | 10 (2.23) | 0.99 | Allium sativum, Capsicum annuum |
| Urinary and rectal diseases | Urine colour and odour, burning with urination, blood in the urine, kidney disorders | 3 (0.67) | 1.00 | Allium sativum |
| Vision problems | Eye pain, hazy, blurred or double vision, night blindness, glaucoma | 5 (1.11) | 0.99 | Ipomoea aquatica, Terminalia chebula |
Parentheses shows the percentage values
aInformant Consensus Factor (ICF)
Among the five major ailment categories, gastrointestinal disorders were dominant with 102 (22.72%) plant species used, followed by dermatological problems (63 species, 14.03%), inflammation and pain (49 species, 10.91%), fever (33 species, 7.35%) and respiratory complaints (31 species, 6.46%). P. guajava, T. chebula (UV 0.34) and P. betle were the plant species most frequently used to treat gastrointestinal disorders. C. dactylon and P. guajava were the plant species most frequently used to treat dermatological problems. A. indica and P. guajava were also the plant species most frequently used to treat inflammation and pain. P. guajava and A. indica were the most frequently used plant species to treat fever. To treat respiratory complaints, A. indica and T. arjuna were the most frequently used plant species. To treat these ailments, P. guajava, C. dactylon, A. indica and T. arjuna were the most frequently used medicinal plants (Table 3). These findings indicate that gastrointestinal disorders and dermatological, inflammation and pain, fever and respiratory complaints were prevalent in the study area.
Potential of medicinal plant species for COVID-19 treatment
Considering the existing literature, such as Ahmed et al. (2020), Azam et al. (2020), Dutta et al. (2021), Islam et al. (2021), Bachar et al. (2021), and Shahriar et al. (2022) we identified the following 42 medicinal plant species (i.e., Adhatoda vasica, A. marmelos, Allium sativum, A. cepa, A. comosus, Andrographis paniculate, A. carambola, Azadirachta indica, Bacopa monniera, B. ceiba, Bryophyllum pinnatum, C. annuum, C. sinensis, Cassia fistula, C. asiatica, Citrus spp., Cocos nucifera, C. longa, Calotropis gigantea, Camellia sinensis, Coriandrum sativum, Elaeocarpus robustus, Eucalyptus spp., H. rosa-sinensis, Ipomoea mauritiana, Mentha piperita, Moringa oleifera, O. sanctum, P. emblica, P. granatum, Polycarpon prostratum, P. guajava, P. dactylifera, Solanum spp., S. pinnata, Swertia chirata, Syzygium spp., T. indica, Terminalia spp., Tinospora cordifolia, Zizyphus mauritiana, and Zingiber officinale) are using by the CWS-dependent communities that could be favourably considered for the treatment of COVID-19 patients in Bangladesh.
Discussion
Medicinal plants for traditional healthcare practices
As shown in the present study’s findings, the use of plant species indicated that local people had good ethnobotanical knowledge about the specific plants and plant parts to use for their daily healthcare purposes. Other studies in Bangladesh have found similar findings. For example, Faruque et al. (2018) listed 159 plants from 62 families in the hilly Bandarban District; Islam et al. (2014) documented 78 plants from 45 families in the Madhupur forest area; and Rahman and Roy (2014) found 43 invasive medicinal plant species belonging to 28 families in two forest-protected areas (FPAs). Similarly, Khan et al. (2011) recorded 39 invasive medicinal plants belonging to 29 families in two FPAs in north-eastern Bangladesh; Rahman et al. (2011b) listed 50 plant species from 42 families in Khadimnagar National Park; and Chowdhury and Koike (2010) recorded 44 plant species belonging to 28 families in Rema-Kalenga Wildlife Sanctuary. Similar to the present study’s 50 tree species, Rahman and Hossain (2002) recorded 55 medicinal tree species from 26 families in CWS.
In addition, several similar studies conducted in protected areas in other parts of the world indicated the following: da Silva et al. (2019) documented 167 medicinal plant species in the Araripe National Forest of Brazil; de Brito et al. (2017) enlisted 71 local medicinal plant species in the Tambaba Environmental Protected Area of north-east Brazil; while Flavien et al. (2016) reported 195 medicinal plant species around a traditional protected area in the Democratic Republic of the Congo. Furthermore, Kala (2005) documented 60 threatened medicinal plant species in protected areas of the Indian Himalayas; Betti (2004) recorded 102 medicinal plants in Dja Biosphere Reserve in Cameroon; and Dzerefos and Witkowski (2001) reported 51 species in Abe Bailey Nature Reserve of South Africa. Moreover, Gumisiriza et al. (2019) recorded 211 medicinal plant species in southwestern Uganda; Umair et al. (2017) found 85 plants belonging to 34 families in Punjab in Pakistan; and Ahmad et al. (2016) recorded 217 plant species belonging to 69 families in different districts of Pakistan.
In the present study, survey data and field observation confirmed that older family members were knowledgeable and experienced in ethnomedicinal plant species (e.g., which species have which medicinal value and which species are used to treat which ailments), with these family members generally preparing the medicine for treating ailments. The survey also found that people shared plant parts and produced medicine with friends and neighbours, enabling everybody to easily meet their needs, especially when medicinal plant resources were scarce. Similar findings were also noticed by Chowdhury et al. (2009) and Rahman (2013) in rural areas of Bangladesh.
Quantitative importance of medicinal plants for traditional healthcare
The UV scores of plant species show the relative importance of medicinal plant species and plant families for a specific population (Islam et al. 2014; Umair et al. 2017; Faruque et al. 2018). In the present study, the species with high UV scores in CWS need specific medicinal plant conservation measures to maintain forest biodiversity. Similarly, the ethnomedicinal plant species with high RFC values indicate specific species that are widely distributed and easily accessible and plant species about which the communities have widespread knowledge (Umair et al. 2017; Faruque et al. 2018; Dixit and Tiwari 2020). Therefore, the medicinal plants with high UV scores and RFC values should be further evaluated for their phytochemically and phytopharmacologically important substances to identify their active constituents for discovering new drugs (Vitalini et al. 2009; Ahmad et al. 2016).
Furthermore, the ICF value calculation helped us identify homogeneity in the users’ ethnobotanical evidence (Faruque et al. 2018). The higher the ICF value, higher the number of healthcare services provided by a specific species, with most species in our study scoring a higher ICF value (0.99). Islam et al. (2014) found a higher ICF value for mental disorders in central Bangladesh. Rahman and Roy (2014) found the highest ICF values for gastrointestinal disorders and respiratory complaints in northeastern Bangladesh. High ICF values were found for sexual disorders and respiratory complaints by Rana et al. (2010) in Bangladesh. In north-eastern Bangladesh, Chowdhury and Koike (2010) found the highest ICF values for respiratory complaints, liver disorders, and urinary and rectal ailments. Other studies found higher ICF values for digestive disorders, general health and unspecified disorders in Uganda (Gumisiriza et al. 2019), and nervous system disorders and skin diseases in India (Dhakal et al. 2020).
As in the present study, other studies reported that more species were used to treat gastrointestinal diseases than other ailments (Chowdhury and Koike 2010; Kadir et al. 2012; Singh et al. 2012; Islam et al. 2014; Umair et al. 2017). Conversely, Faruque et al. (2018) recorded the second-highest number of species for the treatment of inflammation and pain; Chowdhury and Koike (2010) for treating respiratory complaints; and Rahman and Roy (2014) for the treatment of dermatological problems.
Sustainable harvesting, commercialisation and conservation of medicinal plants
The plant species diversity of CWS has been deteriorating day by day due to local people’s significant dependency on daily resource collection for their livelihoods (Rahman et al. 2017a, b). From our FGDs and KIIs, the present study identified the following major problems for medicinal plant conservation in CWS: extensive plantations of exotic tree species, especially Acacia and Eucalyptus spp., with plantations inside the sanctuary; forest area encroached upon and slash-burned for betel leaf (P. betle) cultivation; overharvesting of important medicinal plants; lack of awareness-raising programs on medicinal plants; no recorded documentation of medicinal plants; no income-generating activity from medicinal plants; and no organised marketing channel for commercialisation of medicinal plants and herbal medicine products (Online Resource 4). Key informants stated that, although no restrictions have been placed on harvesting medicinal plants from the sanctuary for individual use, the Forest Department has placed restrictions on unsustainable harvesting for commercial purposes. The local Co-Management Committee through the volunteer Community Patrol Group (CPG) plays a significant role in guarding and monitoring forest resources.
In response to these problems, key informants advised that the Forest Department and NGOs had undertaken some initiatives, such as distributing seedlings of different medicinal and fruit tree species, such as T. arjuna, P. emblica, T. chebula, T. belerica and C. papaya; provided support for the cultivation of medicinal plants in homestead forests as well as inside the sanctuary; distributed seeds of different seasonal vegetables for immediate cash returns; and formed a committee through the Village Conservation Forum to protect these plantations. Moreover, the following suggestions, abridged from the FGD and KII input, could further improve the situation: massive plantations of native fruit trees and medicinal plant species on denuded and degraded hills; minimisation of the land tenure problem for tree plantations; controlling the overharvesting of important medicinal plant species; raising awareness about the curative value of medicinal plants, especially among the young generation; provision of financial aid, seedlings and training to develop nurseries for the conservation of medicinal plants; documentation of traditional and cultural beliefs of local communities on plant utilisation; and commercialisation of local medicinal plant resources, with linkages formed with the pharmaceutical industry (Online Resource 4).
Cultural and religious beliefs have a strong connection with plant species conservation, especially with the conservation of specific plant species believed to bring good health and fortune into people’s lives (Anderson et al. 2005). For example, the Mising tribal community of Assam (India) uses 30 plant species for their religious purposes and the treatment of different ailments (Sharma and Pegu 2011). As in the present study’s findings, Cartwright-Jones (2006) found that paste made from L. inermis leaves was popular as an integral part of weddings and other cultural and religious festivals in South Asia, the Middle East and Africa. Interestingly, Chowdhury et al. (2009) mentioned that young girls sometimes put blood from their fingers at the base of this plant when planting, hoping for its long life and darker leaf colour.
Phytochemical and phytopharmacological evaluation of medicinal plants
Bangladesh is suffering from the continual decline of medicinal plant availability from forest and non-forest sources, the decline in the number of traditional practitioners, the loss of their ethnomedicinal knowledge, and the lack of interest in knowledge transfer to the young generation. Several published studies in Bangladesh, such as Rahman et al. (2001), Ghani (2003), Mazumder and Rahman (2008), Rahmatullah et al. (2010), Kaisar et al. (2011), Haque et al. (2013), Islam et al. (2016), Ghosh et al. (2018), Mohiuddin (2019) and others, have discovered the lead compounds (phytochemical, phytopharmacological, biological, toxicological and other medicinal properties) of important medicinal plants in Bangladesh, which can lead to better drug preparation for healthcare purposes. These scientific studies have suggested that all the documented medicinal plant species in Bangladesh could be a promising source of new drug discovery to treat many ailments, with even a single species able to be used to treat multiple ailments. Therefore, medicinal plant species used for traditional healthcare in and around CWS should be evaluated for essential lead compounds, showing economic, industrial and environmental importance of these species for ex-situ and in-situ conservation.
Role of ethnomedicine in COVID-19 treatment
Deng et al. (2020) recommended ‘cheap kitchen medicine’, such as A. sativum, A. cepa, Cliteria ternatia, Morus alba, Solanum melongena and Z. officinale to fight against COVID-19. Shawky et al. (2020) suggested the following medicinal plants such as Anastatica hierochuntica, Cichorium intybus, Chrysanthemum coronarium, Epilobium hirsutum, Euphorbia spp., Glycyrrhiza glabra, Hibiscus sabdariffa, Nigella sativa and P. guajava to mitigate COVID-19. Jahan and Onay (2020) documented more than 40 medicinal plants for possible treatment of COVID-19 such as C. sinensis, C. annuum, Citrus spp., C. longa, Mentha longıfolia, Olea europaea, Phoenix hanceana, Eucalyptus spp., etc.
Silveira et al. (2020) identified 39 herbal medicines among five species (i.e., Althaea officinalis, Commiphora molmol, Glycyrrhiza glabra, Hedera helix and Sambucus nigra) were found to have a positive effect on the COVID-19 patient; 10 species were found to be promising (A. sativum, Andrographis paniculata, Echinacea angustifolia, Echinacea purpurea, Eucalyptus globulus, Justicia pectoralis, Magnolia officinalis, Pelargonium sidoides, Salix sp. and Z. officinale), while the remainder were continuing to be tested.
A mixture of 11 medicinal plant species called ‘Lianhuaqingwen’ was used in China for the COVID-19 treatment (Runfeng et al. 2020). Luo et al. (2020a, b) reported that Astragalus mongholicus, Atractylodes lancea, A. macrocephala, Forsythia suspensa, Glycyrrhiza glabra, Lonicera japonica and Saposhnikovia divaricate were found to be the most frequently used in China. Furthermore, Ang et al. (2020a) and Weng (2020) recorded the widely used medicinal plants in China: Agastache rugosa, Alisma plantago-aquatica, Armeniacae semen, A. Amarum, Asarum sieboldii, Aster tataricus, A Rhizoma, A. macrocephala, Bupleurum chinense, Cinnamomum cassia, Citrus aurantium, Dioscorea polystachya, Ephedra sinica, Forsythiae fructus, Glycyrrhizae Radix et Rhizoma (comprising 20 species of Fabaceae family), Iris domestica, Lepidii seu Descurainiae Semen (seeds of inauthentic plant species), Pinellia ternate, Polyporus umbellatus, Prunus armeniaca, Radix scutellariae, Scutellaria baicalensis, Tussilago farfara and Wolfiporia extensa.
Furthermore, the following medicinal plants have already been reported for the treatment and management of COVID-19 in previous studies and were found to be used for treating different ailments in CWS: Achyranthes aspera, A. sativum, A. indica, C. longa, M. oleifera, P. guajava, Z. officinale in Africa (Adeleye et al. 2021). Adhatoda spp., A. sativum, A. indica, A. marmelos, B. ceiba, C. longa, Citurs spp., and Z. officinale (Bachar et al. 2021) and Calotropis gigantea in Bangladesh (Dutta et al. 2021). Allium cepa, A. sativum, A. indica, A. carambola, A. marmelos, C. asiatica, C. sativum, C. papaya, C. annuum, C. sinensis, Ficus religiosa, M. piperita, P. guajava, P. emblica, T. bellirica, Terminalia chebula, T. cordifolia, Syzygium cumini and Z. officinale in Nepal (Khadka et al. 2021). A. sativum, Citrus limon, C. sinensis, O. sanctum and Z. officinale in Bangladesh (Ahmed et al. 2020). A. Sativum, A. cepa, E. globulus, P. dactylifera and Z. officinale in Morocco (El Alami et al. 2020). C. limon, O. sanctum and Z. officinale in Bangladesh (Azam et al. 2020). A. cepa, A. comosus, A. indica, A. sativum, C. annuum, C. sativum, C. sinensis, M. piperita, O. sanctum, P. emblica, P. granatum, P. guajava, S. pinnata and Z. officinale in Bangladesh (Islam et al. 2021). A. cepa, A. sativum, A. paniculate, A. indica, C. sinensis, Cassia fistula, C. nucifera, C. longa, P. granatum, M. oleifera, O. sanctum, T. indica, T. chebula, T. cordifolia, Z. officinale in Bangladesh (Shahriar et al. 2022). A. sativum, E. globulus and Z. officinale in Peru (Villena-Tejada et al. 2021). A. cepa, A. sativum, A. comosus, C. sinensis, C. annuum, C. limon, C. nucifera, Colocasia esculenta, C. longa, Dalbergia sissoo, E. globulus, Ficus spp., M. indica, Mentha spp., M. cordata, M. oleifera, Musa spp., P. dactylifera, Syzygium spp., and Zingiber officinale, etc. are common medicinal plants used in China, Italy, Spain, USA, Brazil, Jamaica, Bolivia, Romania, Belarus, Lithuania, Poland, Georgia, Turkey, Pakistan, Cambodia, and South Africa (Pieroni et al. 2020).
The above studies suggested that plant-based drugs could be used alone or in combination as alternative medicines to treat/prevent COVID-19. While these plants will not cure or prevent COVID-19, they may improve the well-being of patients, offering an opportunity to personalise the therapeutic approaches taken. However, standard clinical trials should be carried out to prove the efficacy of these medicinal plant species.
Conclusion
Our exhaustive survey of medicinal plants and traditional healthcare practices revealed that CWS-dependent communities rely exclusively on plant-based ethnomedicine for their daily healthcare purposes. The quantitative assessment indicates that each species has been used to treat multiple ailments. This study also proposes standard clinical trials by pharmaceutical companies to prove the efficacy of locally available medicinal plant species for treating COVID-19 patients in Bangladesh. The results suggest that community awareness of sustainable harvesting and cultivation at the homestead forests and commercial level could lead to sustainable conservation of these invaluable plant species for healthcare use, increased income and dietary quality of communities, and sustainable forest management by involving them. The study findings can potentially lead to the development of new therapeutic uses and may represent novel bioresources for phytochemical and pharmacological studies. The preservation, propagation and conservation of vulnerable but commercially important plant species are further essential research areas. The collaboration between universities, research organisations, pharmaceutical companies and Forest Department could boost the country’s medicinal plant production and use. Finally, medicinal plant conservation and sustainable forest management are essential for meeting the rural sustainable development in Bangladesh.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
This work was supported by the Deutsche Gesellschaft für Internationale Zusammenarbeit (GIZ) (83143484) GmbH, Bangladesh under “IPAC/GIZ Youth Research Award 2012” of MHR. The authors are indebted to the respondents, herbal practitioners and local people for cooperating and sharing their indigenous knowledge regarding ethnomedicine. Authors are grateful to the Bangladesh Forest Department, GIZ, and Society for Health Extension and Development (SHED). A special thanks go to Md. Ekramul Haque for all his efforts in data collection.
Declarations
Conflict of interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Ethical approval
The survey and data collection permission were approved by the authority.
Consent to participate
Verbal consent to participate in the survey was obtained from all respondents.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Adeleye OA, Femi-Oyewo MN, Bamiro OA, Bakre LG, Alabi A, Ashidi JS, Balogun-Agbaje OA, Hassan OM, Fakoya G. Ethnomedicinal herbs in African traditional medicine with potential activity for the prevention, treatment, and management of Coronavirus Disease 2019. Future J Pharm Sci. 2021;7:72. doi: 10.1186/s43094-021-00223-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ahmad M, Khan MPZ, Mukhtar A, Zafar M, Sultana S, Jahan S. Ethnopharmacological survey on medicinal plants used in herbal drinks among the traditional communities of Pakistan. J Ethnopharmacol. 2016;184:154–186. doi: 10.1016/j.jep.2016.02.039. [DOI] [PubMed] [Google Scholar]
- Ahmed FU. Production, processing and marketing of medicinal plants in Bangladesh. Dhaka: Arannayk Foundation; 2009. [Google Scholar]
- Ahmed ZU, Begum ZNT, Hassan MA, Khondker M, Kabir SMH, Ahmad M, Ahmed ATA, Rahman AKA, Haque EU, editors. Encyclopaedia of flora and fauna of Bangladesh, volume 6. Angiosperms: Dicotyledons (Acanthaceae-Asteraceae) Dhaka: Asiatic Society of Bangladesh; 2008. [Google Scholar]
- Ahmed ZU, Hassan MA, Begum ZNT, Khondker M, Kabir SMH, Ahmad M, Ahmed ATA, Rahman AKA, Haque EU, editors. Encyclopaedia of flora and fauna of Bangladesh, volume 12. Angiosperms: Monocotyledons (Orchidaceae-Zingiberaceae) Dhaka: Asiatic Society of Bangladesh; 2008. [Google Scholar]
- Ahmed ZU, Hassan MA, Begum ZNT, Khondker M, Kabir SMH, Ahmad M, Ahmed ATA, Rahman AKA, Haque EU, editors. Encyclopaedia of flora and fauna of Bangladesh, volume 7. Angiosperms: Dicotyledons (Balsaminaceae-Euphorbiaceae) Dhaka: Asiatic Society of Bangladesh; 2008. [Google Scholar]
- Ahmed ZU, Hassan MA, Begum ZNT, Khondker M, Kabir SMH, Ahmad M, Ahmed ATA, editors. Encyclopaedia of flora and fauna of Bangladesh, volume 9. Angiosperms: Dicotyledons (Magnoliaceae-Ponicaceae) Dhaka: Asiatic Society of Bangladesh; 2009. [Google Scholar]
- Ahmed ZU, Hassan MA, Begum ZNT, Khondker M, Kabir SMH, Ahmad M, Ahmed ATA, Rahman AKA, Haque EU, editors. Encyclopaedia of flora and fauna of Bangladesh, volume 8. Angiosperms: Dicotyledons (Fabaceae-Lythraceae) Dhaka: Asiatic Society of Bangladesh; 2009. [Google Scholar]
- Ahmed ZU, Begum ZNT, Hassan MA, Khondker M, Kabir SMH, Ahmad M, Ahmed ATA, Rahman AKA, Haque EU, editors. Encyclopaedia of flora and fauna of Bangladesh: cumulative index volume-Flora, vol 13. Dhaka: Asiatic Society of Bangladesh; 2009. [Google Scholar]
- Ahmed ZU, Hassan MA, Begum ZNT, Khondker M, Kabir SMH, Ahmad M, Ahmed ATA, editors. Encyclopaedia of flora and fauna of Bangladesh, volume 10. Angiosperms: Dicotyledons (Ranunculaceae-Zygophyllaceae) Dhaka: Asiatic Society of Bangladesh; 2010. [Google Scholar]
- Ahmed I, Hasan M, Akter R, Sarkar BK, Rahman M, Sarker MS, Samad MA. Behavioral preventive measures and the use of medicines and herbal products among the public in response to COVID-19 in Bangladesh: a cross-sectional study. PLoS One. 2020;15(12):e0243706. doi: 10.1371/journal.pone.0243706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alamgir ANM. Therapeutic use of medicinal plants and their extracts: Volume 1 (Pharmacognosy) Berlin: Springer; 2017. [Google Scholar]
- Anderson DM, Salick J, Moseley RK, Ou XK. Conserving the sacred medicine mountains: a vegetation analysis of Tibetan sacred sites in Northwest Yunnan. Biodivers Conserv. 2005;14(13):3065–3091. doi: 10.1007/s10531-004-0316-9. [DOI] [Google Scholar]
- Ang L, Lee HW, Choi JY, Zhang J, Lee MS. Herbal medicine and pattern identification for treating COVID-19: a rapid review of guidelines. Integr Med Res. 2020;9:100407. doi: 10.1016/j.imr.2020.100407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ang L, Lee HW, Kim A, Lee MS. Herbal medicine for the management of COVID-19 during the medical observation period: a review of guidelines. Integr Med Res. 2020;9:100465. doi: 10.1016/j.imr.2020.100465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Azam MNK, Mahamud RA, Hasan A, Jahan R, Rahmatullah M. Some home remedies used for treatment of COVID-19 in Bangladesh. J Med Plants Stud. 2020;8(4):27–32. [Google Scholar]
- Bachar SC, Mazumder K, Bachar R, Aktar A, Al Mahtab M. A review of medicinal plants with antiviral activity available in Bangladesh and mechanistic insight into their bioactive metabolites on SARS-CoV-2, HIV and HBV. Front Pharmacol. 2021;12:732891. doi: 10.3389/fphar.2021.732891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benarba B, Pandiella A. Medicinal plants as sources of active molecules against COVID-19. Front Pharmacol. 2020;11:1189. doi: 10.3389/fphar.2020.01189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Betti JL. An ethnobotanical study of medicinal plants among the Baka Pygmies in the Dja Biosphere Reserve. Cameroon Afr Study Monogr. 2004;25(1):1–27. doi: 10.14989/68229. [DOI] [Google Scholar]
- BFD . Management plan for Chunati Wildlife Sanctuary. Climate-Resilient Ecosystems and Livelihoods (CREL) Project. Dhaka: Bangladesh Forest Department; 2015. [Google Scholar]
- Bhuiyan FR, Howlader S, Raihan T, Hasan M. Plants metabolites: possibility of natural therapeutics against the COVID-19 pandemic. Front Med. 2020;7:444. doi: 10.3389/fmed.2020.00444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bieski IGC, Leonti M, Arnason JT, Ferrier J, Rapinski M, Violante IMP, et al. Ethnobotanical study of medicinal plants by population of Valley of Juruena Region, Legal Amazon, Mato Grosso, Brazil. J Ethnopharmacol. 2015;173:383–423. doi: 10.1016/j.jep.2015.07.025. [DOI] [PubMed] [Google Scholar]
- Bregum F. The present status of medicinal plants in Bangladesh. Iran J Pharm Res. 2010;3(Supplement 2):34–34. doi: 10.22037/ijpr.2010.394. [DOI] [Google Scholar]
- Cartwright-Jones C. Developing guidelines on henna: a geographical approach. Ohio: TapDancing Lizard Publishing; 2006. [Google Scholar]
- CBD (Convention on Biological Diversity) (2010) Strategic plan for biodiversity 2011–2020, including Aichi Biodiversity Targets (https://www.cbd.int/sp/)
- Chowdhury MSH, Koike M. Therapeutic use of plants by local communities in and around Rema-Kalenga Wildlife Sanctuary: implications for protected area management in Bangladesh. Agrofor Syst. 2010;80:241–257. doi: 10.1007/s10457-010-9316-9. [DOI] [Google Scholar]
- Chowdhury MSH, Koike M, Muhammed N, Halim MA, Saha N, Kobayashi H. Use of plants in healthcare: a traditional ethnomedicinal practice in rural areas of southeastern Bangladesh. Int J Biodivers Sci Ecosyst Serv Manag. 2009;5(1):41–51. doi: 10.1080/17451590902771342. [DOI] [Google Scholar]
- da Silva NF, Hanazaki N, Albuquerque UP, Campos JLA, Feitosa IS, Araújo EL. Local knowledge and conservation priorities of medicinal plants near a protected area in Brazil. Evid Based Complement Alternat Med. 2019 doi: 10.1155/2019/8275084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Brito MFM, Marín EA, da Cruz DD. Medicinal plants in rural settlements of a protected area in the litoral of northeast Brazil. Ambient Soc. 2017;XX(1):83–104. doi: 10.1590/1809-4422asoc20150034r2v2012017. [DOI] [Google Scholar]
- De Luca V, Salim V, Atsumi SM, Yu F. Mining the biodiversity of plants: a revolution in the making. Science. 2012;336(6089):1658–1661. doi: 10.1126/science.1217410. [DOI] [PubMed] [Google Scholar]
- Deng J, Hou X, Zhang T, Bai G, Hao E, Chu JJH, Wattanathorn J, Sirisa-ard P, Ee CS, Low J, Liu C. Carry forward advantages of traditional medicines in prevention and control of outbreak of COVID 19 pandemic. Chin Herb Med. 2020;12:207–213. doi: 10.1016/j.chmed.2020.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dhakal P, Chettri B, Lepcha S, Acharya BK. Rich yet undocumented ethnozoological practices of socio-culturally diverse indigenous communities of Sikkim Himalaya. India J Ethnopharmacol. 2020;249:112386. doi: 10.1016/j.jep.2019.112386. [DOI] [PubMed] [Google Scholar]
- Dixit S, Tiwari S. Investigation of anti-diabetic plants used among the ethnic communities of Kanpur division. India J Ethnopharmacol. 2020;253:112639. doi: 10.1016/j.jep.2020.112639. [DOI] [PubMed] [Google Scholar]
- Dutta M, Nezam M, Chowdhury S, Rakib A, Paul A, Sami SA, Uddin MZ, Rana MS, Hossain S, Effendi Y, Idroes R, Tallei T, Alqahtani AM, Emran TB. Appraisals of the Bangladeshi medicinal plant Calotropis gigantea used by folk medicine practitioners in the management of COVID-19: a biochemical and computational approach. Front Mol Biosci. 2021;8:625391. doi: 10.3389/fmolb.2021.625391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dzerefos CM, Witkowski ETF. Density and potential utilization of medicinal grassland plants from Abe Bailey Nature Reserve, South Africa. Biodivers Conserv. 2001;10:1875–1896. doi: 10.1023/A:1013177628331. [DOI] [Google Scholar]
- El Alami A, Fattah A, Chait A. Medicinal plants used for the prevention purposes during the COVID-19 pandemic in Morocco. J Anal Sci Appl Biotechnol. 2020;2(1):4–11. [Google Scholar]
- Fakir MAL, Consultant NM, Banik H, Chowdhury RM. Forest carbon inventory 2014 at eight protected areas in Bangladesh. Dhaka: Bangladesh Forest Department and Winrock International; 2015. [Google Scholar]
- FAO (Food and Agriculture Organization of the United Nations) (2010) State of the world’s forests 2009. Rome, Italy
- Faruque MO, Uddin SB, Barlow JW, Hu S, Dong S, Cai Q, Li X, Hu X. Quantitative ethnobotany of medicinal plants used by indigenous communities in the Bandarban District of Bangladesh. Front Pharmacol. 2018;9:40. doi: 10.3389/fphar.2018.00040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flavien NB, Vanhove W, Termote C, Van PD. Importance of traditional protected areas for the collection of medicinal plants, Kongo-Central (DRC) Afr J Ecol. 2016;54(4):479–487. doi: 10.1111/aje.12307Ci. [DOI] [Google Scholar]
- Ghani A. Medicinal plants of Bangladesh with chemical constituents and uses. Dhaka: Asiatic Society of Bangladesh; 2003. [Google Scholar]
- Ghosh MK, Kumar A, Barman RK, Wahed MII. Current status of phytochemical and phytopharmacological study of some medicinal plants used by the tribes in Bangladesh: a review. J Pharmacogn Phytochem. 2018;7(5):1089–1095. [Google Scholar]
- GIZ (Deutsche Gesellschaft für Internationale Zusammenarbeit) (2011) Baseline survey report for management of natural resources and community forestry in Chunati Wildlife Sanctuary project. Dhaka, Bangladesh
- GIZ (Deutsche Gesellschaft für Internationale Zusammenarbeit) (2015) Final report of the final survey of indicators of “Management of Natural Resources and Community Forestry Project (MNRCF-Chunati)” in Chunati Wildlife Sanctuary (CWS), Chittagong, Bangladesh. Dhaka, Bangladesh
- Gumisiriza H, Birungi G, Olet EA, Sesaazi CD. Medicinal plant species used by local communities around Queen Elizabeth National Park, Maramagambo Central Forest Reserve and Ihimbo Central Forest Reserve, Southwestern Uganda. J Ethnopharmacol. 2019;239:111926. doi: 10.1016/j.jep.2019.111926. [DOI] [PubMed] [Google Scholar]
- Haque MM, Ahsan MA, Akbor MA, Rashid MM, Sultana N. Phytochemical screening of some Bangladeshi medicinal plants. Bangladesh J Sci Ind Res. 2013;48(3):193–196. doi: 10.3329/bjsir.v48i3.17330. [DOI] [Google Scholar]
- Heinrich M, Ankli A, Frei B, Weimann C, Sticher O. Medicinal plants in Mexico: Healers’ consensus and cultural importance. Soc Sci Med. 1998;47:1859–1871. doi: 10.1016/S0277-9536(98)00181-6. [DOI] [PubMed] [Google Scholar]
- Hoque ME. Evaluating co-management as a tool for the reduction of poverty and inequality in Chunati Wildlife Sanctuary. In: Fox J, Mustafa MG, Quazi SA, Miles WB, Cunninghum EJ, Chassels M, editors. Connecting communities and conservation: collaborative management of protected areas in Bangladesh. Dhaka: Nishorgo Support Project, Bangladesh Forest Department; 2009. pp. 227–246. [Google Scholar]
- Hossain MK, Hossain MA. Biodiversity of Chunati Wildlife Sanctuary: Flora. Dhaka: Arannayk Foundation; 2014. [Google Scholar]
- Islam MK, Saha S, Mahmud I, Mohamad K, Awang K, Uddin SJ, Rahman MM, Shilpi JA. An ethnobotanical study of medicinal plants used by tribal and native people of Madhupur forest area, Bangladesh. J Ethnopharmacol. 2014;151:921–930. doi: 10.1016/j.jep.2013.11.056. [DOI] [PubMed] [Google Scholar]
- Islam MT, Mamun MAA, Rahman MH, Rahman MA, Akter MM, Ashraf MS. Qualitative and quantitative analysis of phytochemicals in some medicinal plants in Bangladesh. J Chem Biol Phys Sci A. 2016;6(2):530–540. [Google Scholar]
- Islam K, Nath TK, Jashimuddin M, Rahman MF. Forest dependency, co-management and improvement of peoples’ livelihood capital: evidence from Chunati Wildlife Sanctuary. Bangladesh Environ Dev. 2019;32:100456. doi: 10.1016/j.envdev.2019.100456. [DOI] [Google Scholar]
- Islam ATMR, Ferdousi J, Shahinozzaman M. Previously published ethno-pharmacological reports reveal the potentiality of plants and plant-derived products used as traditional home remedies by Bangladeshi COVID-19 patients to combat SARS-CoV-2. Saudi J Biol Sci. 2021;28(11):6653–6673. doi: 10.1016/j.sjbs.2021.07.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jahan I, Onay A. Potentials of plant-based substance to inhabit and probable cure for the COVID-19. Turk J Biol. 2020;44:228–241. doi: 10.3906/biy-2005-114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jamshidi-Kia F, Lorigooini Z, Amini-Khoei H. Medicinal plants: past history and future perspective. J HerbMed Pharmacol. 2018;7(1):1–7. doi: 10.15171/jhp.2018.01. [DOI] [Google Scholar]
- Kabir MJ. Elephant habitat and human-elephant conflict: a case study in Chunati Wildlife Sanctuary. In: Fox J, Mustafa MG, Bushley BR, Brennan SM, Durand L, editors. Connecting communities and conservation: co-management initiatives implemented by IPAC in wetlands and forests of Bangladesh. Dhaka: Integrated Protected Area Co-management Project, Bangladesh Forest Department; 2013. pp. 159–176. [Google Scholar]
- Kadir MF, Sayeed MSB, Mia M. Ethnopharmacological survey of medicinal plants used by indigenous and tribal people in Rangamati, Bangladesh. J Ethnopharmacol. 2012;144:627–637. doi: 10.1016/j.jep.2012.10.003. [DOI] [PubMed] [Google Scholar]
- Kaisar MA, Rahman MS, Rahman MZ, Hasan CM, Rashid MA. A review on phytochemicals from some medicinal plants of Bangladesh. J Pharm Nutr Sci. 2011;1:87–95. doi: 10.6000/1927-5951.2011.01.01.14. [DOI] [Google Scholar]
- Kaky E, Gilbert F. Using species distribution models to assess the importance of Egypt’s protected areas for the conservation of medicinal plants. J Arid Environ. 2016;135:140–146. doi: 10.1016/j.jaridenv.2016.09.001. [DOI] [Google Scholar]
- Kala CP (2005) Indigenous uses, population density, and conservation of threatened medicinal plants in protected areas of the Indian Himalayas. Conserv Biol 19(2):368–378. http://www.jstor.org/stable/3591249.
- Khadka D, Dhamala MK, Li F, Aryal PC, Magar PR, Bhatta S, Thakur MS, Basnet A, Cui D, Shi S. The use of medicinal plants to prevent COVID-19 in Nepal. J Ethnobiol Ethnomed. 2021;17:26. doi: 10.1186/s13002-021-00449-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khan MASA, Sultana F, Rahman MH, Roy B, Anik SI. Status and ethnomedicinal usage of invasive plants in traditional healthcare practices: a case study from northeastern Bangladesh. J for Res. 2011;22(4):649–658. doi: 10.1007/s11676-011-0174-8. [DOI] [Google Scholar]
- Lee B-J, Lee JA, Kim K, Choi J-Y, Jung H-J. A consensus guideline of herbal medicine for coronavirus disease 2019. Integr Med Res. 2020;9:100470. doi: 10.1016/j.imr.2020.100470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luo CH, Ma L, Liu H, Liao W, Chun XR, Zhi-Min C, Jun-Zhi L, Li H, Zhang D. Research progress on main symptoms of novel coronavirus pneumonia improved by traditional Chinese medicine. Front Pharmacol. 2020;11:556885. doi: 10.3389/fphar.2020.556885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luo H, Tang QL, Shang YX, Liang SB, Yang M, Robinson N, Liu J-P. Can Chinese medicine be used for prevention of Corona virus disease 2019 (COVID-19)? A review of historical classics, research evidence and current prevention programs. Chin J Integr Med. 2020;26(4):243–250. doi: 10.1007/s11655-020-3192-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Market Research Future . Herbal medicine market report—forecast 2018–2023. Maharashtra: WantStats Research and Media Pvt. Ltd.; 2018. [Google Scholar]
- Mazumder MEH, Rahman S. Pharmacological evaluation of Bangladeshi medicinal plants for antioxidant activity. Pharm Biol. 2008;46(10–11):704–709. doi: 10.1080/13880200802215735. [DOI] [Google Scholar]
- Mitchell MGE, Schuster R, Jacob AL, Hanna DEL, Dallaire CO, Raudsepp-Hearne C, Bennett EM, Lehner B, Chan KMA. Identifying key ecosystem service providing areas to inform national-scale conservation planning. Environ Res Lett. 2021;16:014038. doi: 10.1088/1748-9326/abc121. [DOI] [Google Scholar]
- Mohiuddin AK. A brief review of traditional plants as sources of pharmacological interests. Open J Plant Sci. 2019;4(1):001–008. doi: 10.17352/ojps.000015. [DOI] [Google Scholar]
- Mollah AR, Rahman MM, Rahman MS. Site-level field appraisal for protected area co-management: Chunati Wildlife Sanctuary. Dhaka: Nishorgo Support Project, Bangladesh Forest Department; 2004. [Google Scholar]
- Mollik MAH, Faruque MR, Badruddaza M, Chowdhury A, Rahman MS. Medicinal plants from Sundarbans used for the prevention of cardiovascular diseases: a pragmatic randomized ethnobotanical survey in Khulna division of Bangladesh. Eur J Integr Med. 2009;1(4):231–232. doi: 10.1016/j.eujim.2009.08.018. [DOI] [Google Scholar]
- Motaleb MA, Khan NA. Community-based conservation of medicinal plants and traditional herbal practice and knowledge: sharing a Bangladeshi experience. Int J for Usufructs Manag. 2012;13(2):53–65. [Google Scholar]
- Phillips O, Gentry AH, Reynel C, Wilkin P, Galvez-Durand BC. Quantitative ethnobotany and Amazonian conservation. Conserv Biol. 1994;8(1):225–248. doi: 10.1046/j.1523-1739.1994.08010225.x. [DOI] [Google Scholar]
- Pieroni A, Vandebroek I, Prakofjewa J, Bussmann RW, Paniagua-Zambrana NY, Maroyi A, Torri L, Zocchi DM, Dam ATK, Khan SM, Ahmad H, Yeşil Y, Huish R, Pardo-de-Santayana M, Mocan A, Hu X, Boscolo O, Sõukand R. Taming the pandemic? The importance of homemade plant-based foods and beverages as community responses to COVID-19. J Ethnobiol Ethnomed. 2020;16:75. doi: 10.1186/s13002-020-004269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rahman MH. A study on exploration of ethnobotanical knowledge of rural community in Bangladesh: basis for biodiversity conservation. ISRN Biodivers. 2013 doi: 10.1155/2013/369138. [DOI] [Google Scholar]
- Rahman ML, Hossain MK. Distribution pattern of medicinal tree species in Chunati Wildlife Sanctuary of Chittagong. Trop J Med Plants. 2002;3(1):65–72. [Google Scholar]
- Rahman MH, Roy B. Population structure and curative uses of invasive plants in and around the protected forests of Bangladesh: a means of utilization of potential invasive species. J Ecosyst. 2014 doi: 10.1155/2014/249807. [DOI] [Google Scholar]
- Rahman S, Hasnat A, Hasan CM, Rashid MA, Ilias M. Pharmacological evaluation of Bangladeshi medicinal plants—a review. Pharm Biol. 2001;39(1):1–6. doi: 10.1076/phbi.39.1.1.5939. [DOI] [Google Scholar]
- Rahman MH, Fardusi MJ, Reza MS. Traditional knowledge and use of medicinal plants by the Patra tribe community in the north-eastern region of Bangladesh. Proc Pak Acad Sci. 2011;48(3):159–167. [Google Scholar]
- Rahman MH, Rahman M, Islam MM, Reza MS. The importance of forests to protect medicinal plants: a case study of Khadimnagar National Park, Bangladesh. Int J Biodivers Sci Ecosyst Serv Manag. 2011;7(4):283–294. doi: 10.1080/21513732.2011.645071. [DOI] [Google Scholar]
- Rahman MM, Mahmud MAA, Ahmed FU. Restoration of degraded forest ecosystem through non-forestry livelihood supports: experience from the Chunati Wildlife Sanctuary in Bangladesh. For Sci Tech. 2017;13:109–115. doi: 10.1080/21580103.2017.1349003. [DOI] [Google Scholar]
- Rahman MM, Mahmud MAA, Ahmed FU, Deb R. Developing alternative income generation activities reduces forest dependency of the poor and enhances their livelihoods: the case of the Chunati Wildlife Sanctuary. Bangladesh for Trees Livelihoods. 2017;26(4):256–270. doi: 10.1080/14728028.2017.1320590. [DOI] [Google Scholar]
- Rahmatullah M, Rahman MA, Hossan MS, Taufiq-Ur-Rahman M, Jahan R, Mollik MAH. A pharmacological and phytochemical evaluation of medicinal plants used by the Harbang Clan of the Tripura tribal community of Mirsharai area, Chittagong District. Bangladesh J Altern Complement Med. 2010;16(7):769–785. doi: 10.1089/acm.2009.0497. [DOI] [PubMed] [Google Scholar]
- Rana MP, Sohel MSI, Akhter S, Islam MJ. Ethnomedicinal plants use by the Manipuri tribal community in Bangladesh. J for Res. 2010;21(1):85–92. doi: 10.1007/s11676-010-0015-1. [DOI] [Google Scholar]
- Runfeng L, Yunlong H, Jicheng H, Weiqi P, Qinhai M, Yongxia S, Chufang L, Jin Z, Zhenhua J, Haiming J, Kui Z, Shuxiang H, Jun D, Xiaobo L, Xiaotao H, Lin W, Nanshan Z, Zifeng Y. Lianhuaqingwen exerts anti-viral and anti-inflammatory activity against novel coronavirus (SARS-CoV-2) Pharmacol Res. 2020;156:104761. doi: 10.1016/j.phrs.2020.104761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sarker AHMR, Røskaft E. Human–wildlife conflicts and management options in Bangladesh, with special reference to Asian elephants (Elephas maximus) Int J Biodivers Sci Ecosyst Serv Manag. 2010;6(3–4):164–175. doi: 10.1080/21513732.2011.554867. [DOI] [Google Scholar]
- Shahidullah AKM, Haque CE. Linking medicinal plant production with livelihood enhancement in Bangladesh: implications of a vertically integrated value chain. J Transdiscipl Environ Stud. 2010;9(2):1–18. [Google Scholar]
- Shahriar S, Sarker MMR, Soma MA, Jannat T, Mina ST, Rahman R, Rahman MS, Rashid MA. Potential of prospective medicinal plants of Bangladesh for the complementary management of COVID-19. Bangladesh Pharma J. 2022;25(1):89–114. doi: 10.3329/bpj.v25i1.57845. [DOI] [Google Scholar]
- Sharma UK, Pegu S. Ethnobotany of religious and supernatural beliefs of the Mising tribes of Assam with special reference to the ‘Dobur Uie’. J Ethnobiol Ethnomed. 2011;7:16. doi: 10.1186/1746-4269-7-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shawky E, Nada AA, Ibrahim RS. Potential role of medicinal plants and their constituents in the mitigation of SARS-CoV-2: identifying related therapeutic targets using network pharmacology and molecular docking analyses. RSC Adv. 2020;10:27961. doi: 10.1039/D0RA05126H. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siddiqui KU, Islam MA, Ahmed ZU, Begum ZNT, Hassan MA, Khondker M, Rahman MM, Kabir SMH, Ahmad M, Ahmed ATA, Rahman AKA, Haque EU, editors. Encyclopaedia of flora and fauna of Bangladesh, volume 11: angiosperms: Monocotyledons (Agavaceae-Najadaceae) Dhaka: Asiatic Society of Bangladesh; 2007. [Google Scholar]
- Siddiqui KU, Islam MA, Ahmed ZU, Begum ZNT, Hassan MA, Khondker M, Rahman MM, Kabir SMH, Ahmad M, Ahmed ATA, Rahman AKA, Haque EU, editors. Encyclopaedia of flora and fauna of Bangladesh, volume 5: bryophytes, pteridophytes, gymnosperm. Dhaka: Asiatic Society of Bangladesh; 2008. [Google Scholar]
- Silveira D, Prieto-Garcia JM, Boylan F, Estrada O, Fonseca-Bazzo YM, Jamal CM, Magalhães PO, Oliveira E, Tomczyk M, Heinrich M. COVID-19: is there evidence for the use of herbal medicines as adjuvant symptomatic therapy? Front Pharmacol. 2020;11:581840. doi: 10.3389/fphar.2020.581840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh AG, Kumar A, Tewari DD. An ethnobotanical survey of medicinal plants used in Terai forest of western Nepal. J Ethnobiol Ethnomed. 2012;8:19. doi: 10.1186/1746-4269-8-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tamima U. Performance evaluation of forest co-management: a case study of Chunati Wildlife Sanctuary, Bangladesh. J for Res. 2016;27:853–861. doi: 10.1007/s11676-015-0198-6. [DOI] [Google Scholar]
- Tardío J, Pardo-De-Santayana M. Cultural importance indices: a comparative analysis based on the useful wild plants of Southern Cantabria (Northern Spain) Econ Bot. 2008;62(1):24–39. doi: 10.1007/s12231-007-9004-5. [DOI] [Google Scholar]
- Umair M, Altaf M, Abbasi AM. An ethnobotanical survey of indigenous medicinal plants in Hafizabad district, Punjab-Pakistan. PLoS One. 2017;12(6):e0177912. doi: 10.1371/journal.pone.0177912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vandebroek I, Pieroni A, Stepp JR, Hanazaki N, Ladio A, Alves RRN, Picking D, Delgoda R, Maroyi A, van Andel T, Quave CL, Paniagua-Zambrana NY, Bussmann RW, Odonne G, Abbasi AM, Albuquerque UP, Baker J, Kutz S, Timsina S, Shigeta M, Oliveira TPR, Hurrell JA, Arenas PM, Puentes JP, Hugé J, Yeşil Y, Pierre LJ, Olango TM, Dahdouh-Guebas F. Reshaping the future of ethnobiology research after the COVID-19 pandemic. Nat Plants. 2020;6:723–730. doi: 10.1038/s41477-020-0691-6. [DOI] [PubMed] [Google Scholar]
- Vardanjani HM, Heydari ST, Dowran B, Pasalar M. A cross-sectional study of Persian medicine and the COVID-19 pandemic in Iran: rumors and recommendations. Integr Med Res. 2020;9:100482. doi: 10.1016/j.imr.2020.100482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Villena-Tejada M, Vera-Ferchau I, Cardona-Rivero A, Zamalloa-Cornejo R, Quispe- Florez M, Frisancho-Triveño Z, Abarca-Meléndez RC, Alvarez-Sucari SG, Mejia CR, Yañez JA. Use of medicinal plants for COVID-19 prevention and respiratory symptom treatment during the pandemic in Cusco, Peru: a cross sectional survey. PLoS ONE. 2021;16(9):e0257165. doi: 10.1371/journal.pone.0257165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vitalini S, Tomè F, Fico G. Traditional uses of medicinal plants in Valvestino (Italy) J Ethnopharmacol. 2009;121:106–116. doi: 10.1016/j.jep.2008.10.005. [DOI] [PubMed] [Google Scholar]
- Weng J-K. Plant solutions for the COVID-19 pandemic and beyond: historical reflections and future perspectives. Mol Plant. 2020;13:803–807. doi: 10.1016/j.molp.2020.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO (World Health Organization) Ecosystems and human well-being: Health synthesis: a report of the Millennium Ecosystem Assessment. Geneva: WHO; 2005. [Google Scholar]
- WHO (World Health Organization) (2022) WHO Coronavirus (COVID-19) dashboard. https://covid19.who.int/
- Zhou Z, Gao N, Meng WY, Chang P, Tong Y, Fu S. Clinical studies on the treatment of novel coronavirus pneumonia with traditional Chinese medicine—a literature analysis. Front Pharmacol. 2020;11:560448. doi: 10.3389/fphar.2020.560448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhuang W, Fan Z, Chu Y, Wang H, Yang Y, Wu L, Sun N, Sun G, Shen Y, Lin X, Guo G, Xi S. Chinese patent medicines in the treatment of Coronavirus Disease 2019 (COVID-19) in China. Front Pharmacol. 2020;11:1066. doi: 10.3389/fphar.2020.01066. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.