Ghost infarct core has been described to account for overestimating core infarct size in the early time period (<3 hours). The authors describe the phenomenon of underestimating core infarct size on CT perfusion in the later time period (>6 hours), which they have termed perfusion scotoma.
SUMMARY:
With the growing rise in utilization of CT perfusion for selecting patients for thrombectomy in acute ischemic stroke from large vessel occlusion, some potential pitfalls are becoming more commonly seen particularly when it comes to estimating the core infarct size on CT perfusion. Ghost infarct core has been described to account for overestimating core infarct size in the early time period (<3 hours). Herein, we describe the phenomenon of underestimating core infarct size on CT perfusion in the later time period (>6 hours), which we have termed perfusion scotoma.
As CT perfusion has grown in practice in aiding the selection of patients eligible for thrombectomy in acute ischemic stroke, some potential pitfalls are becoming more commonly seen when it is used to estimate the core infarct size. While DWI remains the criterion standard for visualizing the ischemic stroke core, most patients do not undergo MR imaging at initial presentation. Most institutions that are part of a stroke network use multimodal CT, which includes CTA and CT perfusion. This algorithm works well for most institutions due to the speed and availability of CT imaging.
Following the multiple, positive trials in 2015 for thrombectomy in large-vessel occlusion,1-3 CT perfusion use started to grow exponentially, including for patients in the <6-hour time window. Soon after this growth occurred, reports of “ghost infarct core” were published.4 Ghost infarct core was defined as a core infarct on perfusion (defined as CBF of <30%) that overestimated the final core infarct size. This was seen most commonly in patients presenting in the <3-hour time period. Another study noted this phenomenon in the <6-hour time period.5
Further increasing the demand for this technology were the positive results of the Clinical Mismatch in the Triage of Wake Up and Late Presenting Strokes Undergoing Neurointervention with Trevo (DAWN)6 (2017) and Endovascular Therapy Following Imaging Evaluation for Ischemic Stroke 3 (DEFUSE 3)7 (2018) trials, which used quantitative CT perfusion to stratify which patients would benefit from thrombectomy in the >6-hour time period. Now that the eligible time period was increased in patients last known healthy up to 24 hours (DAWN) or up to 16 hours (DEFUSE 3), widespread CT perfusion has become far more prevalent. With this increase in use, we have seen a new pitfall in estimating the core infarct volume on CT perfusion: underestimating the core infarct volume. This phenomenon was described by Copelan et al,8 who looked at patients in the >6-hour time period who underwent CTA at a spoke hospital before undergoing CT perfusion (RAPID Software; https://www.rapidsoftware.shop/) at the hub hospital. They found that the core infarct was underestimated in this scenario and hypothesized that recent contrast administration rendered the core infarct estimation inaccurate. However, even more recently, Voleti et al9 published an article correlating the ASPECTS with the CT perfusion core in large-vessel occlusion. In general, as the ASPECTS number decreases, one would expect core infarct volume to increase. The scatterplot from that article demonstrated outliers in the correlation of the core infarct volume in patients with a lower ASPECTS who also showed low core infarct volumes on perfusion. We have termed this phenomenon of a small core infarct on CT perfusion but a low ASPECTS “perfusion scotoma.”
We have seen this phenomenon in our clinical practice almost exclusively in the >6-hour time period, when ASPECTS abnormalities are apparent. These findings appear to be independent of the vendor used for CT perfusion, judging by what has appeared in the literature as well as our own clinical experience.
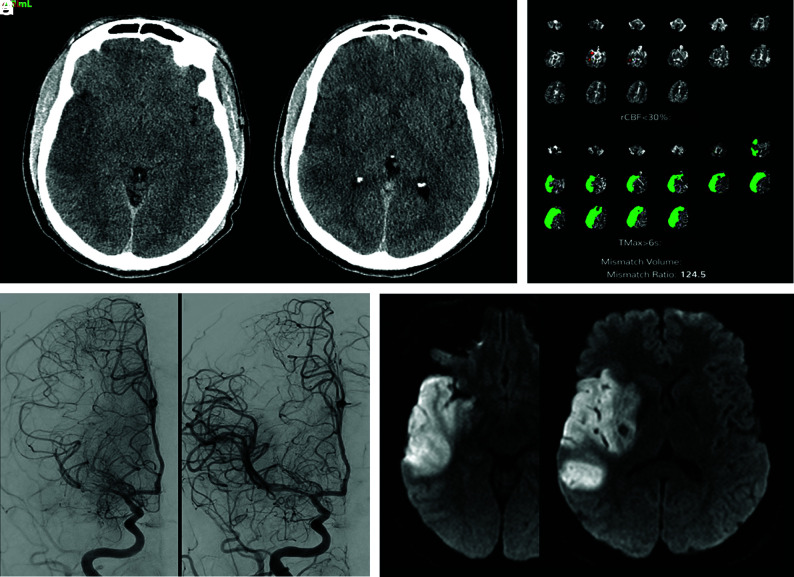
Figure 1 is an example of the perfusion scotoma from our clinical practice where a patient presented to one of our spoke hospitals last known healthy more than 8 hours before arrival. Only noncontrast CT of the brain was performed before transfer to our Comprehensive Stroke Center. The initial brain CT demonstrated a hyperdense acute clot in the M1 segment of the right MCA, with early acute ischemic changes and an ASPECTS of 6. On arrival at our comprehensive stroke center, CTA and CT perfusion were performed and demonstrated an occlusive or near-occlusive clot in the M1 segment of the right MCA, with a large area of acute ischemia (time-to-maximum, >6 seconds of 249 mL), but a minimal core infarct (CBF of <30% of 2 mL). The patient underwent angiography and successful thrombectomy of a nearly totally occlusive clot of the M1 segment of the right MCA. Follow-up MR imaging demonstrated areas of restricted diffusion corresponding to the areas of ASPECTS abnormality on the original CT scan, the “perfusion scotoma.”
FIG 1.
A patient presented with right MCA syndrome to an outside hospital, last known healthy >8 hours before arrival. The initial brain CT at the outside institution demonstrated acute ischemic changes in the right temporal lobe and insula with an ASPECTS of 6 (A and B). CT perfusion performed at our hospital reconstructed using both manual (Advantage Workstation; GE Healthcare, not shown) and automated (Viz.ai Intelligent Care Coordination; https://www.viz.ai; C) perfusion software demonstrates a large area of acute ischemia (time-to maximum, >6 seconds of 249 mL), but a minimal core infarct (CBF of <30% of 2 mL). Cerebral angiography prethrombectomy demonstrates partial recanalization of the right M1 segment with some antegrade flow (D). The patient underwent successful thrombectomy of the M1 segment (E). Follow-up MR imaging demonstrates areas of restricted diffusion corresponding to the areas of ASPECTS abnormality on the original CT scan, the “perfusion scotoma” (F and G). rCBF indicates relative CBF; Tmax, time-to-maximum.
The likely etiology for this case and many cases of this perfusion scotoma is early reperfusion from partial recanalization as well as luxury perfusion. Although we tend to think of luxury perfusion in the 48- to 72-hour timeframe, it can also be seen within 24 hours and may contribute to this phenomenon.10 We can think of the infarcted tissue on perfusion as a continuum from reduced CBF in the <6-hour timeframe, slowly increasing with time to when it may become equivalent to normal tissue in the 6- to 24-hour timeframe and elevated in the >24-hour timeframe.
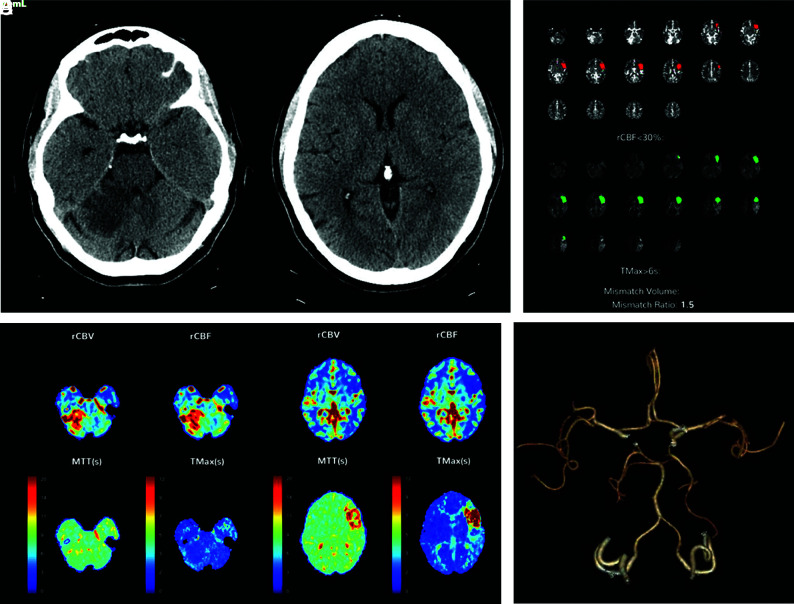
Figure 2 is an example of a patient with a subacute right superior cerebellar infarct >24 hours old but who presented with an acute left MCA syndrome. Note on the quantitative perfusion maps, not only the acute left MCA ischemia but also the absence of core infarct in the right superior cerebellar hemisphere. However, elevated CBF and CBV were noted in the cerebellar infarct on the qualitative color maps, consistent with reperfusion. The CTA also demonstrated that the right superior cerebellar artery was patent and the M2 segment of the left middle cerebral artery was occluded.
FIG 2.
A patient presenting with an acute left MCA syndrome. CT also demonstrates an acute/subacute right superior cerebellar infarct (A and B). CT perfusion was performed and reconstructed using both manual (Advantage Workstation, not shown) and automated (C–E) perfusion software and demonstrates similar results. The quantitative perfusion maps demonstrate acute left MCA ischemia but no evidence of core infarct in the right superior cerebellar hemisphere (C). D and E, Qualitative color maps demonstrate elevated CBF and CBV in the right superior cerebellar infarct, consistent with reperfusion. CTA also demonstrates the right superior cerebellar artery to be patent and the M2 segment of the left MCA to be occluded (F). rCBF indicates relative CBF; rCBV, relative CBV; Tmax, time-to-maximum.
Why does the perfusion scotoma matter? When communicating the quantitative CT perfusion findings, it is imperative for the radiologist to also incorporate the ASPECTS to accurately assess the true ischemic penumbra. For example, in a patient with large-vessel occlusion and a large time-to-maximum of >6 seconds (eg, 150 mL) as the area of acute ischemia, the CBF of <30% (core infarct) being very low (eg, 5 mL), with a high ASPECTS (eg, >6), would imply that the patient is a thrombectomy candidate. However, if in that same patient, the ASPECTS is low (eg, 3 as seen in the scatterplot), this patient would, most likely, not be a thrombectomy candidate, even though the mismatch may be listed as 145 mL in this example; furthermore, thrombectomy may even be deleterious. It also allows the neurointerventionalist to give realistic expectations to the family regarding the procedure. Although we have not correlated the CT perfusion images to DWI in the early phase (our patients had MRIs at later time periods), we believe that this finding can be extrapolated, and it may represent a future area for research.
In summary, like the importance of understanding the concept of overestimating the core infarct in the <3-hour time period (ghost infarct core), physicians involved in acute stroke care should understand the concept of underestimating the infarct core in the >6-hour time period (perfusion scotoma).
Footnotes
Disclosure forms provided by the authors are available with the full text and PDF of this article at www.ajnr.org.
References
- 1. Goyal M, Demchuk AM, Menon BK, et al. ; ESCAPE Trial Investigators. Randomized assessment of rapid endovascular treatment of ischemic stroke. N Engl J Med 2015;372:1019–30 10.1056/NEJMoa1414905 [DOI] [PubMed] [Google Scholar]
- 2. Saver JL, Goyal M, Bonafe A, et al. ; SWIFT PRIME Investigators. Stent-retriever thrombectomy after intravenous t-PA vs. t-PA alone in stroke. N Engl J Med 2015;372:2285–95 10.1056/NEJMoa1415061 [DOI] [PubMed] [Google Scholar]
- 3. Campbell BC, Mitchell PJ, Kleinig TJ, et al. ; EXTEND-IA Investigators. Endovascular therapy for ischemic stroke with perfusion-imaging selection. N Engl J Med 2015;372:1009–18 10.1056/NEJMoa1414792 [DOI] [PubMed] [Google Scholar]
- 4. Martins N, Aires A, Mendez B, et al. Ghost infarct core and admission computed tomography perfusion: redefining the role of neuroimaging in acute ischemic stroke. Interv Neurol 2018;7:513–21 10.1159/000490117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Rodrigues GM, Mohammaden MH, Haussen DC, et al. Ghost infarct core following endovascular reperfusion: a risk for computed tomography perfusion misguided selection in stroke. Int J Stroke 2021. Nov 19. [Epub ahead of print] 10.1177/17474930211056228 [DOI] [PubMed] [Google Scholar]
- 6. Nogueira RG, Jadhav AP, Haussen DC, et al. ; DAWN Trial Investigators. Thrombectomy 6 to 24 hours after stroke with a mismatch between deficit and infarct. N Engl J Med 2018;378:11–21 10.1056/NEJMoa1706442 [DOI] [PubMed] [Google Scholar]
- 7. Albers GW, Marks MP, Kemp S, et al. ; DEFUSE 3 Investigators. Thrombectomy for stroke at 6 to 16 hours with selection by perfusion imaging. N Engl J Med 2018;378:708–18 10.1056/NEJMoa1713973 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Copelan AZ, Smith ER, Drocton GT, et al. Recent administration of iodinated contrast renders core infarct estimation inaccurate using RAPID software. AJNR Am J Neuroradiol 2020;41:2235–42 10.3174/ajnr.A6908 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Voleti S, Vidovich J, Corcoran B, et al. Correlation of Alberta Stroke Program Early Computed Tomography Score with computed tomography perfusion core in large vessel occlusion in delayed time windows. Stroke 2021;52:498–504 10.1161/STROKEAHA.120.030353 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Nagar VA, McKinney AM, Karagulle AT, et al. Reperfusion phenomenon masking acute and subacute infarcts at dynamic perfusion CT: confirmation by fusion of CT and diffusion-weighted MR images. AJNR Am J Neuroradiol 2009;193:1629–38 10.2214/AJR.09.2664 [DOI] [PubMed] [Google Scholar]