The frequency of e-cigarette vaping of nicotine and marijuana products is increasing among adolescents and young adults; the detrimental effects of vaping on general and oral health have not yet been thoroughly defined. It is speculated that nicotine, marijuana/cannabis products including cannabidiol (CBD), and added flavoring chemicals in e-cigarettes may alter the inflammatory response and periodontal tissue remodeling processes during orthodontically induced tooth movement, leading to potential oral side effects in patients undergoing orthodontic therapy such as increased alveolar bone loss and root resorption. The present editorial discusses the state of current evidence regarding the impact of rising vaping on orthodontically induced tooth movement and periodontal health in patients undergoing orthodontic therapy and suggests possible directions for future research.
Tobacco smoking is a leading cause of preventable mortality worldwide and is associated with the development of various diseases, such as cancer, heart, and respiratory diseases. Nicotine is one of the most detrimental toxic compounds of tobacco products/smoke; it causes tissue alterations including impaired angiogenesis, tissue perfusion, and healing as well as altered collagen synthesis and bone remodeling [1,2]. From an orodental aspect, tobacco smoking induces changes in the oral microflora, promoting the colonization of key periodontal pathogens such as Porphyromonas gingivalis and Candida species [3,4]. Nicotine consumption has also been associated with an increased risk of oral cancer and oral inflammatory and periodontal diseases such as periodontitis [5].
Electronic cigarettes (E-cigarettes) are battery-powered devices containing a tank filled with liquid (which is usually flavored) and they deliver varying degrees of nicotine after heating the liquid into an inhalable aerosol [6]. It is commonly perceived that vaping e-cigarettes is less harmful to health compared with conventional tobacco products [7]. This potentially flawed assumption has led to a rapid emergence of e-cigarette vaping, especially among adolescents and young adults attempting to quit/reduce tobacco smoking. Nonetheless, e-cigarette vaping causes health effects similar to cigarette smoking [8].
In addition to nicotine, e-cigarette liquid also contains propylene glycol (PG), vegetable glycerin (VG) along with traditional (taste of tobacco, menthol, or mint) and nontraditional flavoring chemicals (with tastes such as candy and fruit), which are not found and are even prohibited in combustible cigarettes [9,10]. The use of nontraditional flavors in e-cigarettes has increased the frequency of vaping among youth, and it has been positively associated with vaping continuation in adolescents [9]. There are over 8000 different flavors/chemicals used in e-cigarettes with unknown and potentially deleterious health effects [11]. For instance, vanillin, menthol, and ethyl maltol (which can be found in major e-cigarette brands) have been associated with cytotoxic effects, the induction of oxidative stress and inflammation, and DNA damage in lung cells [10]. Moreover, various toxicity and inflammatory biomarkers have been found to be elevated in e-cigarette vapers compared to never-smokers in biofluids including serum, urine, and saliva [12]. Furthermore, e-cigarette-derived nicotine and flavoring chemicals have several effects on cellular and mitochondrial function, including the inhibition of myofibroblast differentiation, which may in turn lead to impaired wound healing and gel contraction in lung tissues [13,14].
Flavored e-cigarettes have also been shown to cause alterations in oral tissues including increased oxidative and inflammatory responses in human periodontal ligament fibroblasts and lead to a state of irreversible growth arrest in the oral epithelium [15]. In this regard, e-cigarette vaping increases oral inflammation [16], and it may increase the risk of periodontal tissue destruction, oral submucous fibrosis, and oral cancer [17]. Nicotine binds to its nicotinic receptors (alpha3 and alpha7 nicotinic acetylcholine receptors (AChRs)) and flavor aldehydes potentially with TRP receptors. Similarly, it is perceived that synthetic nicotine and their isomers will have the same effects [18,19]. Further a recent emergence of synthetic cooling agents along with nicotine will aggravate the toxicities [15,20,21,22,23,24,25].
Marijuana (Cannabis sativa) contains over 100 cannabinoids with the main compounds being the psychoactive synthetic delta-9-tetrahydrocannabinol (THC) and non-psychoactive cannabidiol (CBD) compound [26]. Vaping cannabis (THC or CBD) among adolescents and adults is rising, particularly in the U.S. where the legalization of recreational cannabis use has occurred in several states [27,28]. Moreover, it has been reported that Cannabis use has increased during the COVID-19 pandemic [29] potentially due to its neuropsychiatric effects including euphoria and axiolysis [30]. Cannabis has been associated with health problems such as addiction, psychosis, and high-risk behaviors including higher alcohol consumption [31]. It has also been suggested that Cannabis consumption is harmful to periodontal tissues; however, current evidence regarding the effect of Cannabis on oral health is in general sparse and inconclusive [32]. Although both THC and CBD bind to cannabinoid receptors in the human brain and body, they produce different effects; CBD (a non-psychoactive component) has been reported to offer a wide range of health benefits including a decrease in inflammation, chronic pain, and anxiety [33]. Thus, the use of CBD and hemp oils is increasing in popularity due to medical benefits without the psychoactive effects of marijuana (low THC content) [33]. In this regard, it is pertinent to consider the ratio of THC/CBD when evaluating systemic and oral effects of vaping marijuana products. Furthermore, since e-cigarettes can be used for vaping both nicotine and cannabis compounds (THC and CBD), the co-occurring use of nicotine and cannabis is common among individuals who vape both substances [34].
Orthodontic tooth movement (OTM) depends on an active process of bone remodeling, during which alveolar bone is resorbed in the pressure side of the periodontal ligament while bone apposition occurs in the tension side [35]. This force-induced aseptic inflammation is regulated by key factors such as osteoprotegerin, prostaglandins, and cytokines [36]. Inflammation control is pertinent during OTM to avoid side effects such as alveolar bone loss, root resorption, and periodontal tissue destruction [36]. The authors of the present editorial speculate that e-cigarette vaping of nicotine, cooling agents, and/or cannabis products might alternate the inflammatory response to orthodontically induced tooth movement. Two systematic reviews have shown that the influence of nicotine on OTM has solely been examined in animal studies (mainly rats) and concluded that nicotine increases the rate of OTM by increasing alveolar bone loss and root resorption (Table 1) [1,37]. In addition, the influence of cannabis on OTM has only been examined in an experimental study in rats, which showed that THC attenuates OTM by decreasing bone resorption (Table 2) [26]. These limited experimental findings highlight the need of well-designed clinical studies to assess the influence of vaping nicotine/synthetic nicotine, cooling agents/coolants, THC/CBD, or both on OTM and periodontal tissues of patients (especially adolescents and young adults) undergoing OT with fixed appliances and/or clear aligners. Such studies will help identify whether vaping is a risk factor for periodontal diseases and bone loss during orthodontically induced tooth movement and will highlight the potential need of patient counseling for vaping cessation prior to the initiation of OT.
Table 1.
Studies evaluating the effect of nicotine administration and/or vaping nicotine on the rate and biology of orthodontically induced tooth movement and periodontal tissue response. OTM, orthodontic tooth movement; OIIRR, orthodontically induced inflammatory root resorption.
| Effect of Nicotine Administration on OTM | Effect of Vaping Nicotine on OTM | ||||
|---|---|---|---|---|---|
| Reference | Study Design | Influence on OTM and Periodontal Tissue Response Compared with Control Group | Reference | Study Design | Influence on OTM and Periodontal Tissue Response Compared with Control Group |
| Experimental studies on animal models | |||||
| Sodagar et al. [38] | Experimental study on rats | Increased OTM and bone resorption | No studies in indexed literature | ||
| Shintcovsk et al. [39] | Experimental study on rats | Reduced angiogenesis and delayed collagen maturation | |||
| Kirschneck et al. [40] | Experimental study on rats | Increased bone loss | |||
| Li et al. [41] | Experimental study on rats | Increased odontoclastogenesis and OIIRR | |||
| Bakathir et al. [42] | Experimental study on rats | Increased OTM and unbalanced bone remodeling | |||
| Kirshneck et al. [43] | Experimental study on rats | Increased OTM, bone loss and OIIRR | |||
| Araujo et al. [44] | Experimental study on rats | No significant difference in the rate of OTM, altered collagen maturation | |||
| Ferreira et al. [45] | Experimental study on rats | No significant difference on OTM | |||
| Ullrich et al. [46] | Experimental study on rats | Increased OIIRR and osteoclastogenesis | |||
| Lee et al. [47] | Experimental study on rats | No significant difference on OTM | |||
| Clinical studies | |||||
| No studies in indexed literature | |||||
Table 2.
Studies evaluating the effects of marijuana product administration and/or marijuana vaping on the rate and biology of orthodontically-induced tooth movement and periodontal tissue response. OTM, orthodontic tooth movement.
| Effect of Marijuana Product Administration on OTM | Effect of Vaping Marijuana on OTM | ||||
|---|---|---|---|---|---|
| Reference | Study Design | Influence on OTM and Periodontal Tissue Response Compared with Control Group | Reference | Study Design | Influence on OTM and Periodontal Tissue Response Compared with Control Group |
| Experimental studies on animal models | |||||
| Klein et al. [26] | Experimental study on rats | Dronabinol attenuates OTM by decreasing bone resorption | No studies in indexed literature | ||
| Clinical studies | |||||
| No studies in indexed literature | |||||
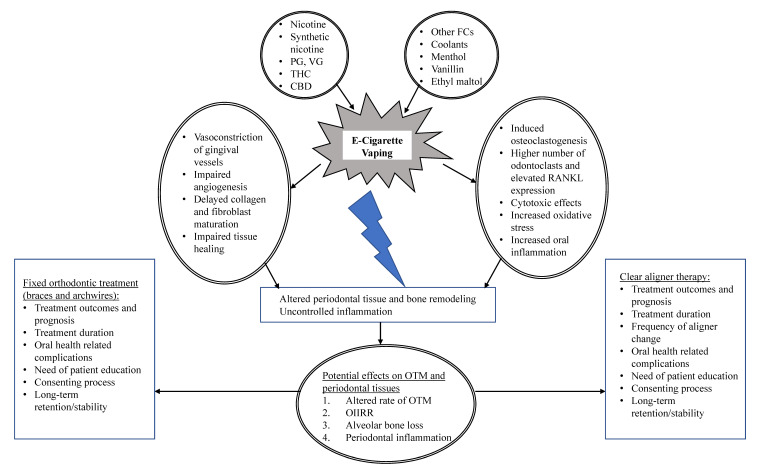
In summary, it is well known that the control of oral/periodontal inflammation and periodontal tissue remodeling is pertinent during OTM to prevent side effects such as alveolar bone loss and root resorption. Nicotine has been shown to increase alveolar bone loss during experimental OTM in rats potentially by impairing angiogenesis and collagen synthesis and by promoting oral inflammation and bone resorption. In addition, THC has been shown to attenuate OTM by decreasing bone resorption in rats. Overall, there is a lack of clinical and experimental studies assessing the effects of vaping nicotine, menthol or mint, VG, PG, nontraditional flavoring chemicals, and CBD and/or THC on the periodontal tissues and orthodontically induced tooth movement. The authors of the present Editorial speculate that the aforementioned vaping compounds might influence OTM and periodontal health by altering angiogenesis, wound healing, bone remodeling, and oral inflammation during the course of OT (Figure 1). Moreover, vaping these products might alter the oral microflora, further promoting periodontal and oral diseases particularly in patients undergoing OT who often find oral health maintenance challenging. In this respect, experimental studies should be conducted by examining the individual effects (and critical dosages) of these chemicals/substances on OTM and oral/periodontal health as well as their potential synergistic mechanisms. Finally, clinical studies are warranted to understand the increasing impact of vaping on the oral health of individuals undergoing OT. From a clinical perspective, it is crucial to understand the impact of rising vaping on the planned outcomes and prognosis of OT, long-term retention, and stability, as well as treatment duration and optimal frequency of orthodontic appliances activation (or frequency of tray changes in the case of clear aligner therapy). From an ethical standpoint, such studies will also highlight the potential need of patient education regarding the deleterious effects of vaping on general health and OTM and will help develop community-based programs to support vaping cessation, particularly in adolescents and young adults undergoing OT.
Figure 1.
E-cigarette vaping as a risk factor for potential complications during orthodontically-induced tooth movement. Possible biological mechanisms and clinical considerations. Abbreviations: VG, vegetable glycerin; PG, propylene glycol; CBD, cannabidiol; THC, tetrahydrocannabinol; FC, flavoring chemicals; RANKL, receptor activator of nuclear factor kappa-Β ligand, OTM, orthodontic tooth movement; OIIRR, orthodontically-induced inflammatory root resorption.
Author Contributions
D.M. and I.R. conceived, wrote, and revised the manuscript. All authors have read and agreed to the published version of the manuscript.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This research received no external funding.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Michelogiannakis D., Rossouw P.E., Al-Shammery D., Akram Z., Khan J., Romanos G.E., Javed F. Influence of nicotine on orthodontic tooth movement: A systematic review of experimental studies in rats. Arch. Oral Biol. 2018;93:66–73. doi: 10.1016/j.archoralbio.2018.05.016. [DOI] [PubMed] [Google Scholar]
- 2.Davies C.S., Ismail A. Nicotine has deleterious effects on wound healing through increased vasoconstriction. BMJ. 2016;353:i2709. doi: 10.1136/bmj.i2709. [DOI] [PubMed] [Google Scholar]
- 3.Hanioka T., Morita M., Yamamoto T., Inagaki K., Wang P.L., Ito H., Morozumi T., Takeshita T., Suzuki N., Shigeishi H., et al. Smoking and periodontal microorganisms. Jpn. Dent. Sci. Rev. 2019;55:88–94. doi: 10.1016/j.jdsr.2019.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mokeem S.A., Abduljabbar T., Al-Kheraif A.A., Alasqah M.N., Michelogiannakis D., Samaranayake L.P., Javed F. Oral Candida carriage among cigarette- and waterpipe-smokers, and electronic cigarette users. Oral Dis. 2019;25:319–326. doi: 10.1111/odi.12902. [DOI] [PubMed] [Google Scholar]
- 5.Chaffee B.W., Couch E.T., Vora M.V., Holliday R.S. Oral and periodontal implications of tobacco and nicotine products. Periodontology 2000. 2021;87:241–253. doi: 10.1111/prd.12395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dinakar C., O’Connor G.T. The Health Effects of Electronic Cigarettes. N. Engl. J. Med. 2016;375:1372–1381. doi: 10.1056/NEJMra1502466. [DOI] [PubMed] [Google Scholar]
- 7.Zainol Abidin N., Abidin E.Z., Zulkifli A., Syed Ismail S.N., Karuppiah K., Amer Nordin A.S., Musbah Z., Zulkipli N.F., Praveena S.M., Rasdi I., et al. Vaping Topography and Reasons of Use among Adults in Klang Valley, Malaysia. Asian Pac. J. Cancer Prev. 2018;19:457–462. doi: 10.22034/APJCP.2018.19.2.457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tsai M., Byun M.K., Shin J., Crotty Alexander L.E. Effects of e-cigarettes and vaping devices on cardiac and pulmonary physiology. J. Physiol. 2020;598:5039–5062. doi: 10.1113/JP279754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Leventhal A.M., Goldenson N.I., Cho J., Kirkpatrick M.G., McConnell R.S., Stone M.D., Pang R.D., Audrain-McGovern J., Barrington-Trimis J.L. Flavored E-cigarette Use and Progression of Vaping in Adolescents. Pediatrics. 2019;144:e20190789. doi: 10.1542/peds.2019-0789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Muthumalage T., Lamb T., Friedman M.R., Rahman I. E-cigarette flavored pods induce inflammation, epithelial barrier dysfunction, and DNA damage in lung epithelial cells and monocytes. Sci. Rep. 2019;9:19035. doi: 10.1038/s41598-019-51643-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bals R., Boyd J., Esposito S., Foronjy R., Hiemstra P.S., Jiménez-Ruiz C.A., Katsaounou P., Lindberg A., Metz C., Schober W., et al. Electronic cigarettes: A task force report from the European Respiratory Society. Eur. Respir. J. 2019;53:1801151. doi: 10.1183/13993003.01151-2018. [DOI] [PubMed] [Google Scholar]
- 12.McDonough S.R., Rahman I., Sundar I.K. Recent updates on biomarkers of exposure and systemic toxicity in e-cigarette users and EVALI. Am. J. Physiol. Lung Cell Mol. Physiol. 2021;320:L661–L679. doi: 10.1152/ajplung.00520.2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lei W., Lerner C., Sundar I.K., Rahman I. Myofibroblast differentiation and its functional properties are inhibited by nicotine and e-cigarette via mitochondrial OXPHOS complex III. Sci. Rep. 2017;7:43213. doi: 10.1038/srep43213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lucas J.H., Muthumalage T., Wang Q., Friedman M.R., Friedman A.E., Rahman I. E-Liquid Containing a Mixture of Coconut, Vanilla, and Cookie Flavors Causes Cellular Senescence and Dysregulated Repair in Pulmonary Fibroblasts: Implications on Premature Aging. Front Physiol. 2020;11:924. doi: 10.3389/fphys.2020.00924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sundar I.K., Javed F., Romanos G.E., Rahman I. E-cigarettes and flavorings induce inflammatory and pro-senescence responses in oral epithelial cells and periodontal fibroblasts. Oncotarget. 2016;7:77196–77204. doi: 10.18632/oncotarget.12857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Figueredo C.A., Abdelhay N., Figueredo C.M., Catunda R., Gibson M.P. The impact of vaping on periodontitis: A systematic review. Clin. Exp. Dent. Res. 2021;7:376–384. doi: 10.1002/cre2.360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Niaz K., Maqbool F., Khan F., Bahadar H., Ismail Hassan F., Abdollahi M. Smokeless tobacco (paan and gutkha) consumption, prevalence, and contribution to oral cancer. Epidemiol. Health. 2017;39:e2017009. doi: 10.4178/epih.e2017009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yogeswaran S., Rahman I. Differences in Acellular Reactive Oxygen Species (ROS) Generation by E-Cigarettes Containing Synthetic Nicotine and Tobacco-Derived Nicotine. Toxics. 2022;10:134. doi: 10.3390/toxics10030134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Yogeswaran S., Muthumalage T., Rahman I. Comparative Reactive Oxygen Species (ROS) Content among Various Flavored Disposable Vape Bars, including Cool (Iced) Flavored Bars. Toxics. 2021;9:235. doi: 10.3390/toxics9100235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kaur G., Gaurav A., Lamb T., Perkins M., Muthumalage T., Rahman I. Current Perspectives on Characteristics, Compositions, and Toxicological Effects of E-Cigarettes Containing Tobacco and Menthol/Mint Flavors. Front. Physiol. 2020;11:613948. doi: 10.3389/fphys.2020.613948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Muthumalage T., Prinz M., Ansah K.O., Gerloff J., Sundar I.K., Rahman I. Inflammatory and Oxidative Responses Induced by Exposure to Commonly Used e-Cigarette Flavoring Chemicals and Flavored e-Liquids without Nicotine. Front. Physiol. 2018;8:1130. doi: 10.3389/fphys.2017.01130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kaur G., Muthumalage T., Rahman I. Mechanisms of toxicity and biomarkers of flavoring and flavor enhancing chemicals in emerging tobacco and non-tobacco products. Toxicol. Lett. 2018;288:143–155. doi: 10.1016/j.toxlet.2018.02.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ye D., Gajendra S., Lawyer G., Jadeja N., Pishey D., Pathagunti S., Lyons J., Veazie P., Watson G., McIntosh S., et al. Inflammatory biomarkers and growth factors in saliva and gingival crevicular fluid of e-cigarette users, cigarette smokers, and dual smokers: A pilot study. J. Periodontol. 2020;91:1274–1283. doi: 10.1002/JPER.19-0457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Javed F., ALHarthi S.S., BinShabaib M.S., Gajendra S., Romanos G.E., Rahman I. Toxicological impact of waterpipe smoking and flavorings in the oral cavity and respiratory system. Inhal. Toxicol. 2017;29:389–396. doi: 10.1080/08958378.2017.1384084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Javed F., Kellesarian S.V., Sundar I.K., Romanos G.E., Rahman I. Recent updates on electronic cigarette aerosol and inhaled nicotine effects on periodontal and pulmonary tissues. Oral Dis. 2017;23:1052–1057. doi: 10.1111/odi.12652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Klein K.P., Guastaldi F.P.S., Pereira H.S.G., He Y., Lukas S.E. Dronabinol inhibits alveolar bone remodeling in tooth movement of rats. Am. J. Orthod. Dentofac. Orthop. 2022;161:e215–e222. doi: 10.1016/j.ajodo.2021.07.012. [DOI] [PubMed] [Google Scholar]
- 27.Carliner H., Brown Q.L., Sarvet A.L., Hasin D.S. Cannabis use, attitudes, and legal status in the U.S.: A review. Prev. Med. 2017;104:13–23. doi: 10.1016/j.ypmed.2017.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Boyer E.W., Levy S., Smelson D., Vargas S., Casey A. The Clinical Assessment of Vaping Exposure. J. Addict. Med. 2020;14:446–450. doi: 10.1097/ADM.0000000000000634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Imtiaz S., Wells S., Rehm J., Hamilton H.A., Nigatu Y.T., Wickens C.M., Jankowicz D., Elton-Marshall T. Cannabis Use During the COVID-19 Pandemic in Canada: A Repeated Cross-sectional Study. J. Addict. Med. 2021;15:484–490. doi: 10.1097/ADM.0000000000000798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Jett J., Stone E., Warren G., Cummings K.M. Cannabis Use, Lung Cancer, and Related Issues. J. Thorac. Oncol. 2018;13:480–487. doi: 10.1016/j.jtho.2017.12.013. [DOI] [PubMed] [Google Scholar]
- 31.Wilkinson S.T., Yarnell S., Radhakrishnan R., Ball S.A., D’Souza D.C. Marijuana Legalization: Impact on Physicians and Public Health. Annu. Rev. Med. 2016;67:453–466. doi: 10.1146/annurev-med-050214-013454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Keboa M.T., Enriquez N., Martel M., Nicolau B., Macdonald M.E. Oral Health Implications of Cannabis Smoking: A Rapid Evidence Review. J. Can. Dent. Assoc. 2020;86:k2. [PubMed] [Google Scholar]
- 33.VanDolah H.J., Bauer B.A., Mauck K.F. Clinicians’ Guide to Cannabidiol and Hemp Oils. Mayo Clin. Proc. 2019;94:1840–1851. doi: 10.1016/j.mayocp.2019.01.003. [DOI] [PubMed] [Google Scholar]
- 34.Smith D.M., Hyland A., Kozlowski L., O’Connor R.J., Collins R.L. Use of Inhaled Nicotine and Cannabis Products among Adults Who Vape Both Substances. Subst. Use Misuse. 2022;57:432–441. doi: 10.1080/10826084.2021.2019773. [DOI] [PubMed] [Google Scholar]
- 35.Meikle M.C. The tissue, cellular, and molecular regulation of orthodontic tooth movement: 100 years after Carl Sandstedt. Eur. J. Orthod. 2006;28:221–240. doi: 10.1093/ejo/cjl001. [DOI] [PubMed] [Google Scholar]
- 36.Li Y., Jacox L.A., Little S.H., Ko C.C. Orthodontic tooth movement: The biology and clinical implications. Kaohsiung J. Med. Sci. 2018;34:207–214. doi: 10.1016/j.kjms.2018.01.007. [DOI] [PubMed] [Google Scholar]
- 37.Jyothish S., Athanasiou A.E., Makrygiannakis M.A., Kaklamanos E.G. Effect of nicotine exposure on the rate of orthodontic tooth movement: A meta-analysis based on animal studies. PLoS ONE. 2021;16:e0247011. doi: 10.1371/journal.pone.0247011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sodagar A., Donyavi Z., Arab S., Kharrazifard M.J. Effect of nicotine on orthodontic tooth movement in rats. Am. J. Orthod. Dentofac. Orthop. 2011;139:e261–e265. doi: 10.1016/j.ajodo.2010.08.018. [DOI] [PubMed] [Google Scholar]
- 39.Shintcovsk R.L., Knop L., Tanaka O.M., Maruo H. Nicotine effect on bone remodeling during orthodontic tooth movement: Histological study in rats. Dental. Press J. Orthod. 2014;19:96–107. doi: 10.1590/2176-9451.19.2.096-107.oar. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kirschneck C., Proff P., Maurer M., Reicheneder C., Römer P. Orthodontic forces add to nicotine-induced loss of periodontal bone: An in vivo and in vitro study. J. Orofac. Orthop. 2015;76:195–212. doi: 10.1007/s00056-015-0283-7. [DOI] [PubMed] [Google Scholar]
- 41.Li J., Wang X., Li N., Zhenga D., Su Y., Zhang J. Short-term effects of nicotine on orthodontically induced root resorption in rats. Angle Orthod. 2016;86:199–205. doi: 10.2319/101014-727.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Bakathir M.A., Linjawi A.I., Omar S.S., Aboqura A.B., Hassan A.H. Effects of nicotine on bone during orthodontic tooth movement in male rats. Histological and immunohistochemical study. Saudi Med. J. 2016;37:1127–1135. doi: 10.15537/smj.2016.10.15159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kirschneck C., Maurer M., Wolf M., Reicheneder C., Proff P. Regular nicotine intake increased tooth movement velocity, osteoclastogenesis and orthodontically induced dental root resorptions in a rat model. Int. J. Oral. Sci. 2017;9:174–184. doi: 10.1038/ijos.2017.34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Araujo C.M., Rocha A.C., Araujo B.M.M., Johann A., Pereira L.F., Tanaka O.M., Guariza Filho O., Camargo E.S. Effect of acute administration of nicotine and ethanol on tooth movement in rats. Braz. Oral. Res. 2018;32:e96. doi: 10.1590/1807-3107bor-2018.vol32.0096. [DOI] [PubMed] [Google Scholar]
- 45.Ferreira C.L., Nunes C.M.M., Bernardo D.V., Pedroso J.F., Longo M., Santamaria M., Jr., Santamaria M.P., Jardini M.A.N. Effect of orthodontic force associated with cigarette smoke inhalation in healthy and diseased periodontium. A histometric and immunohistochemistry analysis in rats. J. Periodontal Res. 2018;53:924–931. doi: 10.1111/jre.12584. [DOI] [PubMed] [Google Scholar]
- 46.Ullrich N., Schröder A., Bauer M., Spanier G., Jantsch J., Deschner J., Proff P., Kirschneck C. The role of HIF-1α in nicotine-induced root and bone resorption during orthodontic tooth movement. Eur. J. Orthod. 2021;43:516–526. doi: 10.1093/ejo/cjaa057. [DOI] [PubMed] [Google Scholar]
- 47.Lee S.H., Cha J.Y., Choi S.H., Kim B.I., Cha J.K., Hwang C.J. Effect of nicotine on orthodontic tooth movement and bone remodeling in rats. Korean J. Orthod. 2021;51:282–292. doi: 10.4041/kjod.2021.51.4.282. [DOI] [PMC free article] [PubMed] [Google Scholar]