Figure 2.
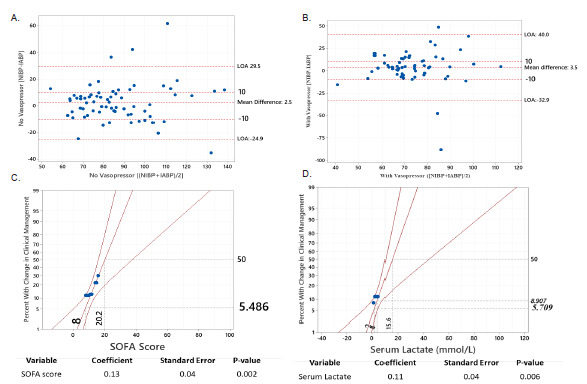
(A)Bland-Altman plot displaying blood pressure differences among septic patients without vasopressors. The noninvasive blood pressure (NIBP) and invasive arterial (IA) BP discrepancy was distributed evenly throughout the X-axis, demonstrating that the difference between the two modalities occurred when patients were hypotensive or normotensive. Additionally, the difference between NIBP and IABP on the Y-axis was mostly concentrated between the level of −10 mm Hg and +10 mm Hg, demonstrating that the NIBP modality has equal likelihood to be higher or lower than IABP. (B) Bland-Altman plot displaying blood pressure differences among septic patients with vasopressors. There were even distributions of NIBP-IABP* discrepancies along the X-axis, demonstrating that the difference between the two modalities occurred when patients were hypotensive or normotensive. However, most values for [NIBP-IABP] difference were above the level of +10 mm Hg, demonstrating that NIBP measurements were usually greater than IABP in our patient population with sepsis requiring vasopressors. (C) Probit logit analysis showing probability of having clinically significant discrepancy between noninvasive and intra-arterial blood pressure (Y-axis) and its association with SOFA score (X-axis). Patients who had a SOFA* score of 20 (X-axis) would have 50% probability (Y-axis) of requiring change in clinical management when arterial catheters were inserted. (D) Probit logit analysis showing probability of having a clinically significant discrepancy between noninvasive and intra-arterial blood pressure (Y-axis) and its association with serum lactate level. Patients who had serum lactate of 4 mmol/L (X-axis) would be associated with approximately 9% probability (Y-axis) of having change of clinical management when arterial catheters were present.
IABP, invasive arterial blood pressure; LOA, limit of agreement; mm Hg, millimeter of mercury; NIBP, non-invasive blood pressure; SOFA, Sequential Organ Failure Assessment; mmol/L, millimoles per liter.
