Key Points
Question
Are social, economic, and geographic factors independently associated with diet quality?
Findings
In this cross-sectional analysis of 155 331 adults participating in a nationwide US cohort study, Black individuals, White individuals with limited income, participants with low educational attainment, and people living in rural areas or food deserts were more likely to have overall poor diet quality. All dietary components, but especially sugar-sweetened beverages and processed meats, contributed to the disparities observed.
Meaning
These findings suggest that multiple individual-level socioeconomic and neighborhood-level factors were independently associated with poor diet quality in this US cohort.
This cross-sectional study examines socioeconomic and geographic factors associated with diet quality in US adults.
Abstract
Importance
Poor diet quality is a key factor associated with obesity and chronic disease. Understanding associations of socioeconomic and geographic factors with diet quality can inform public health and policy efforts for advancing health equity.
Objective
To identify socioeconomic and geographic factors associated with diet quality in a large US cohort study.
Design, Setting, and Participants
This cross-sectional study included adult men and women who enrolled in the Cancer Prevention Study-3 at American Cancer Society community events in 35 US states, the District of Columbia, and Puerto Rico between 2006 and 2013. Participants completed a validated food frequency questionnaire between 2015 and 2017. Data were analyzed from February to November 2021.
Exposures
The main exposures included self-reported race and ethnicity, education, and household income. Geocoded addresses were used to classify urbanization level using Rural-Urban Commuting Area codes; US Department of Agriculture’s Food Access Research Atlas database classified residence in food desert.
Main Outcomes and Measures
Poor diet quality was defined as lowest quartile of dietary concordance with the 2020 American Cancer Society recommendations for cancer prevention score, based on sex-specific intake categories of vegetables and legumes, whole fruits, whole grains, red and processed meat, highly processed foods and refined grains, and sugar-sweetened beverages.
Results
Among 155 331 adults, 123 115 were women (79.3%), and the mean (SD) age was 52 (9.7) years), and there were 1408 American Indian or Alaskan Native individuals (0.9%); 2721 Asian, Native Hawaiian, or Pacific Islander individuals (1.8%); 3829 Black individuals (2.5%); 7967 Hispanic individuals (5.1%); and 138 166 White individuals (88.9%). All key exposures assessed were statistically significantly and independently associated with poor diet quality. Compared with White participants, Black participants had a 16% (95% CI, 8%-25%) higher risk of poor diet quality, while Hispanic/Latino had 16% (95% CI, 12%-21%) lower risk and Asian, Native Hawaiian, and Pacific Islander participants had 33% (95% CI, 26%-40%) lower risk of poor diet quality. After controlling for other characteristics, rural residence was associated with a 61% (95% CI, 48%-75%) higher risk of poor diet quality, and living in a food desert was associated with a 17% (95% CI, 12%-22%) higher risk. Associations of income with diet quality and education with diet quality varied by race and ethnicity (income: P for interaction = .01; education: P for interaction < .001). All diet score components were associated with disparities observed.
Conclusions and Relevance
This cross-sectional study found that multiple individual-level socioeconomic and geographic variables were independently associated with poor diet quality among a large, racially and ethnically and geographically diverse US cohort. These findings could help to identify groups at highest risk of outcomes associated with poor diet to inform future approaches for advancing health equity.
Introduction
Poor diet quality is associated with the leading causes of death in the US, including cancer.1,2 Diet quality tends to be lower among historically marginalized groups, such as American Indian and Alaska Native and Black communities, with roots in structural racism3,4 and among rural and economically disadvantaged communities that may have limited access to healthy food.5,6 These same communities have generally experienced disproportionately higher death rates of chronic diseases associated with obesity, in part owing to the association of diet quality with prevalence of obesity.6 A deeper understanding of how social, economic, and environmental factors affect diet quality could be helpful in addressing health disparities and advancing health equity.
For decades, numerous health organizations7,8,9,10,11 have published guidelines on healthy diet and lifestyle for prevention of cancer and other chronic diseases. A body of evidence suggests that greater dietary and behavioral concordance with the these guidelines is associated with significantly lower mortality from cancer, cardiovascular diseases, and all causes,12,13,14 including among people from historically marginalized racial and ethnic groups and individuals with limited resources.15,16 In the US, the proportion of cancers attributable to poor diet alone is estimated to be 4.2%17 to 5.2%18 and has recently been reported to vary substantially by race and ethnicity, education, and income.19 For example, in the US, non-Hispanic Black men and women were estimated to experience 214 more diet-associated cancer deaths per 100 000 population compared with non-Hispanic White individuals.19
However, the prevalence of obesity, poor diet, and physical inactivity in the US remains high. Two-thirds of US adults have overweight or obesity, and rates continue to increase.20 In the US and other high-income Western countries, the proportionate increase in body mass index (BMI; calculated as weight in kilograms divided by height in meters squared) over 30 years is greater in rural vs urban areas.21 Intakes of fruits, vegetables, and whole grains in the US are far below recommended intakes,22,23 and processed meat and added sugar intakes are above24 recommended intakes. Ultraprocessed foods, high in sugar, fat, and salt, contribute almost 60% of calories and 90% of added sugars in US diets.25 While trends in overall diet quality have improved in the US between 1999 and 2012 across race and ethnicity, education, and income groups, disparities in those improvements widened over time.5 Analyses that simultaneously evaluate socioeconomic and geographic factors associated with diet quality, and their interactions, are lacking.
The goal of this cross-sectional study was to identify socioeconomic and geographic factors associated with lower diet quality7 in the American Cancer Society’s (ACS) Cancer Prevention Study-3 (CPS-3),26 a large and diverse prospective cohort of US adults. Findings may reveal population subgroups that could benefit from targeted efforts to improve dietary behaviors for chronic disease prevention.
Methods
The CPS-3 study protocol was approved by the institutional review board of Emory University. All participance provided written informed consent. This study follows the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline for observational studies.
Study Population
Approximately 304 000 US adults aged 30 to 65 years with no history of cancer from 35 states, the District of Columbia, and Puerto Rico–which together account for 93% of the US population—voluntarily enrolled in CPS-3 between 2006 and 2013.26 The study was not designed to be nationally representative but to include participants with geographic and racial and ethnic diversity.26 During in-person enrollment at ACS fundraising events (eg, Relay for Life) or community enrollment drives designed for recruitment, participants completed a survey with questions on race and ethnicity and highest level of education attained, and provided written informed consent.26 After enrollment, participants completed a comprehensive baseline survey at home. Individuals who returned the baseline survey were recontacted every 3 years (ie, the active cohort) to update medical, demographic, and lifestyle information (254 650 individuals). Diet was assessed on the 2015 follow-up survey returned by 186 638 participants between 2015 and 2017; 177 345 participants (69.6% of the active cohort, including 36 419 men and 140 926 women) completed the food frequency questionnaire (FFQ).
Diet Assessment
The CPS-3 FFQ was modified from the Willett/Harvard FFQ27,28,29 using 24-hour recalls and focus groups among Hispanic/Latino, non-Hispanic/Latino Black and non-Hispanic/Latino White, participants in CPS-3.30 It included 191 line items listing standard portion sizes and queried usual consumption over the past year with frequency ranging from never or fewer than 1 time per month to 4 times per day or more for foods and 6 times per day or more for beverages. The FFQ was validated for assessment of foods31 and nutrients,30 overall and within racial and ethnic groups and by education. The CPS-3 diet validation study was conducted in English, and less than 1% of Hispanic/Latino participants completed the Spanish language FFQ.
Outcome: Dietary Quality
The ACS diet score reflects dietary recommendations of the 2020 ACS Guideline on Diet and Physical Activity for Cancer Prevention,7 which are consistent with recommendations for prevention of other chronic diseases9,11 (eTable 1 in the Supplement). Sex-specific consumption quartiles were used in scoring all components except for sugar-sweetened beverages (SSBs). Greater consumption quartile of vegetables and legumes, whole fruits, and variety of both (contributing 0-3 points), and of whole grains (0-3 points) earned higher points. Greater consumption quartile of red and processed meat was reverse-scored (3-0 points). Due to irregular intake distribution, SSB subcomponent scoring used absolute cut points for both sexes. Together, highly processed foods (HPF), refined grains, and SSB scores contributed 3 to 0 points. The final score ranged from 0 to 12, with 12 representing the highest diet quality. Poor overall diet quality was defined as a diet score in the bottom sex-specific quartile (men: 0 to <4.50; women: 0 to <4.75). For component scores, the poor scores were a score of 0 (lowest sex-specific quartile) for each component of the overall score (defined as vegetables: men, ≤2.1 servings per day; women, ≤2.4 servings per day; fruit: men, ≤0.9 servings per day; women, ≤1.1 servings per day; whole grains: men, ≤0.7 servings per day; women, ≤0.7 servings per day; red and processed meat: men, >1.5 servings per day; women, >1.2 servings per day; HPF and refined grains: men, >39% kcal; women, >40% kcal; SSB: ≥3 servings per week for men and women).
Exposure Variables
The National Institutes of Health definition of Health Disparate Populations, which covers key aspects of social determinants of health,32 guided our selection of variables for this analysis. At enrollment, participants were asked if they consider themselves to be Hispanic or Latina/o (no/yes). Participants self-reported race as: American Indian or Alaskan Native; Asian; Native Hawaiian, or Pacific Islander; Black or African American; White; and/or other. If 2 races were selected and 1 included White, participants were categorized as the other race. Race and ethnicity was categorized as American Indian or Alaskan Native; Asian, Native Hawaiian, or Pacific Islander (grouped together because of small numbers); Hispanic or Latino; non-Hispanic Black (hereafter, Black); non-Hispanic White (hereafter, White; reference group owing to higher numbers); and other (also included multiple racial and ethnic designations, each too small to examine separately). Hispanic participants who did not identify as White (3.5% of Hispanic participants) were classified as other. Other individual-level exposures included household income, education, and residence. Participants’ home addresses were geocoded by Texas A&M University GeoServices.33 Rural-urban commuting area (RUCA) codes, which classify US census tracts according to urbanization, daily commuting, and population density from 2010 census and 2006 to 2010 American Community Survey data,34 were categorized as metropolitan, micropolitan, small town, and rural. The US Department of Agriculture Food Access Research Atlas database was used to define residence in a food desert, defined as the nearest grocery being farther than 1 mile in metropolitan and micropolitan settings, and farther than 10 miles for rural settings.35
Exclusions
Among 177 345 CPS-3 participants who completed the FFQ, additional exclusions included 7484 participants for poor FFQ reporting (defined elsewhere31), 457 participants for top 0.05% of food group scores, 10 223 participants for geocode match score less than 80, 178 participants missing RUCA code, 42 participants missing food desert status, 280 participants missing race and ethnicity data, 2745 participants missing income data, and 605 participants missing education data.
Statistical Analysis
Logistic regression models were used to cross-sectionally examine factors associated with poor diet quality, defined as lowest sex-specific category. Model 1 adjusted for age, sex, and energy intake; model 2 additionally included all key exposures; and model 3 included other potential confounders (ie, BMI, alcohol intake, and a comorbidity score) selected using backward elimination. To avoid controlling for consequences of poor diet, model 2 was considered the main model.
Two-way interactions of all key exposures compared all combinations to a common referent group and evaluated statistical significance of the cross-product term using the Wald Test. Two-sided P < .05 was considered statistically significant. SAS statistical software version 9.4 (SAS Institute) was used for all statistical analyses. Data were analyzed from February to November 2021.
Results
The final analytic cohort included 155 331 participants, with a mean (SD) age of 52 (9.7) years and 32 216 men (20.7%) and 123 115 (79.3%) women. There were 1408 American Indian or Alaskan Native individuals (0.9%); 2721 Asian, Native Hawaiian, or Pacific Islander individuals (1.8%); 3829 Black individuals (2.5%); 7967 Hispanic individuals (5.1%); and 138 166 White individuals (88.9%). Characteristics according to quartile of ACS diet score are provided in Table 1. Poorer diet quality was observed among participants who were younger, American Indian or Alaska Native or Black, had lower income, had lower educational attainment, lived in a nonmetropolitan area, and lived in a food desert (Table 1). Those with lower diet quality were more likely to have never married, to work full time, to have obesity, to report minimal exercise, to currently smoke, to drink less alcohol, and to have 2 or more chronic medical conditions (Table 1). In addition, they were less likely to cook at home and more likely to frequent fast-food and full-service restaurants.
Table 1. Participant Characteristics by Adherence to the 2020 American Cancer Society Dietary Guidelines Score Among Adults in the Cancer Prevention Study-3.
| Characteristic | Dietary score, No. (%) (N = 155 331)a | |||
|---|---|---|---|---|
| Quartile 1 (n = 37 366) | Quartile 2 (n = 36 567) | Quartile 3 (n = 40 659) | Quartile 4 (n = 40 739) | |
| Age, mean (SD), y | 49.5 (9.64) | 51.6 (9.69) | 52.7 (9.63) | 53.9 (9.48) |
| BMI, mean (SD) | 29.5 (6.94) | 28.2 (6.26) | 27.2 (5.91) | 25.5 (5.09) |
| Recreational physical activity, mean (SD), MET-h/wk | 9.2 (8.54) | 10.3 (8.75) | 10.9 (8.82) | 11.9 (9.08) |
| Sex | ||||
| Men | 7262 (19.4) | 8624 (23.6) | 7460 (18.3) | 8870 (21.8) |
| Women | 30 104 (80.6) | 27 943 (76.4) | 33 199 (81.7) | 31 869 (78.2) |
| Race and ethnicity | ||||
| American Indian or Alaskan Native | 387 (1.0) | 325 (0.9) | 370 (0.9) | 326 (0.8) |
| Asian, Native Hawaiian, or Pacific Islander | 471 (1.3) | 619 (1.7) | 732 (1.8) | 899 (2.2) |
| Black | 1056 (2.8) | 867 (2.4) | 964 (2.4) | 942 (2.3) |
| Hispanic | 1896 (5.1) | 1827 (5.0) | 2085 (5.1) | 2159 (5.3) |
| White | 33 300 (89.1) | 32 650 (89.3) | 36 187 (89.0) | 36 029 (88.4) |
| Otherb | 256 (0.7) | 279 (0.8) | 321 (0.8) | 384 (0.9) |
| Income, $ | ||||
| <25 000 | 1868 (5.0) | 1462 (4.0) | 1472 (3.6) | 1409 (3.5) |
| 25 000 to <50 000 | 5396 (14.4) | 4258 (11.6) | 4327 (10.6) | 3913 (9.6) |
| 50 000 to <75 000 | 7519 (20.1) | 6632 (18.1) | 6969 (17.1) | 6595 (16.2) |
| 75 000 to <100 000 | 6981 (18.7) | 6493 (17.8) | 7170 (17.6) | 6910 (17.0) |
| 100 000 to <125 000 | 5992 (16.0) | 5983 (16.4) | 6668 (16.4) | 6582 (16.2) |
| 125 000 to <150 000 | 3420 (9.2) | 3796 (10.4) | 4315 (10.6) | 4268 (10.5) |
| ≥150 000 | 6190 (16.6) | 7943 (21.7) | 9738 (24.0) | 11 062 (27.2) |
| Educational level | ||||
| ≤High school | 4152 (11.1) | 2953 (8.1) | 2443 (6.0) | 1689 (4.1) |
| Some college or 2-y degree | 12 393 (33.2) | 10 492 (28.7) | 10 415 (25.6) | 8079 (19.8) |
| College graduate | 12 381 (33.1) | 12 773 (34.9) | 14 496 (35.7) | 14 349 (35.2) |
| Graduate degree | 8440 (22.6) | 10 349 (28.3) | 13 305 (32.7) | 16 622 (40.8) |
| Rural-urban commuting area | ||||
| Metropolitan | 30 387 (81.3) | 31 360 (85.8) | 35 810 (88.1) | 36 967 (90.7) |
| Micropolitan | 4593 (12.3) | 3496 (9.6) | 3211 (7.9) | 2613 (6.4) |
| Small town | 1478 (4.0) | 1050 (2.9) | 1033 (2.5) | 728 (1.8) |
| Rural | 908 (2.4) | 661 (1.8) | 605 (1.5) | 431 (1.1) |
| Residing in a food desert | ||||
| No | 34 010 (91) | 33 917 (92.8) | 38 051 (93.6) | 38 374 (94.2) |
| Yes | 3356 (9.0) | 2650 (7.2) | 2608 (6.4) | 2365 (5.8) |
| Marital status | ||||
| Married or living with partner | 28 174 (76.3) | 28 024 (77.6) | 31 251 (77.7) | 31 358 (77.9) |
| Never married | 3170 (8.6) | 2655 (7.4) | 2798 (7.0) | 2848 (7.1) |
| Divorced, separated, or widowed | 5588 (15.1) | 5425 (15.0) | 6184 (15.4) | 6038 (15.0) |
| Work status | ||||
| Full time | 27 469 (74.8) | 25 371 (70.5) | 26 540 (66.6) | 24 840 (62.3) |
| Part time | 3545 (9.7) | 3901 (10.8) | 5125 (12.9) | 5934 (14.9) |
| Retired | 3087 (8.4) | 4153 (11.5) | 5264 (13.2) | 6146 (15.4) |
| Other | 2600 (7.1) | 2546 (7.1) | 2942 (7.4) | 2939 (7.4) |
| Smoking status | ||||
| Never | 25 791 (69.2) | 25 102 (68.9) | 27 904 (68.8) | 28 298 (69.7) |
| Current | 1952 (5.2) | 1123 (3.1) | 873 (2.2) | 492 (1.2) |
| Former | 9509 (25.5) | 10 213 (28.0) | 11 754 (29.0) | 11 816 (29.1) |
| Alcohol intake, drinks/d | ||||
| None | 13 132 (35.2) | 10 047 (27.5) | 9957 (24.5) | 9426 (23.2) |
| >0-1 | 18 944 (50.8) | 19 268 (52.8) | 21 845 (53.8) | 21 592 (53.1) |
| >1 | 5240 (14.0) | 7202 (19.7) | 8783 (21.6) | 9667 (23.8) |
| Family history of cancer | ||||
| No | 14 047 (38.9) | 13 195 (37.3) | 14 345 (36.3) | 14 060 (35.6) |
| Yes | 22 091 (61.1) | 22 216 (62.7) | 25 141 (63.7) | 25 481 (64.4) |
| Comorbiditiesc | ||||
| None | 19 777 (52.9) | 19 402 (53.1) | 22 476 (55.3) | 23 834 (58.5) |
| 1 | 10 477 (28.0) | 10 253 (28.0) | 11 278 (27.7) | 11 115 (27.3) |
| ≥2 | 7112 (19.0) | 6912 (18.9) | 6905 (17.0) | 5790 (14.2) |
| Full-service restaurant | ||||
| None or rarely | 6797 (18.4) | 6442 (17.8) | 7288 (18.1) | 8296 (20.6) |
| 1 time/mo to 2 times/wk | 27 546 (74.4) | 27 231 (75.1) | 30 538 (75.8) | 29 792 (74.0) |
| ≥3 times/wk | 2675 (7.2) | 2580 (7.1) | 2458 (6.1) | 2183 (5.4) |
| Fast food consumption | ||||
| None or rarely | 9166 (24.6) | 13 814 (38.0) | 19 921 (49.3) | 27 025 (66.8) |
| 1 time/mo to 2 times/wk | 20 789 (55.9) | 18 725 (51.5) | 17 971 (44.4) | 12 408 (30.6) |
| ≥3 times/wk | 7231 (19.4) | 3838 (10.6) | 2538 (6.3) | 1053 (2.6) |
| Homecooked meals | ||||
| None or rarely | 1819 (4.9) | 1173 (3.2) | 844 (2.1) | 552 (1.4) |
| 1 time/mo to 2 times/wk | 10 259 (27.6) | 7481 (20.6) | 6268 (15.5) | 3877 (9.6) |
| ≥3 times/wk | 25 059 (67.5) | 27 708 (76.2) | 33 297 (82.4) | 36 077 (89.1) |
Abbreviations: BMI, body mass index (calculated as weight in kilograms divided by height in meters squared); MET, metabolic equivalent of task.
Total scores range from 0 to 12, with higher score indicating better diet quality. Quartiles are calculated using sex-specific cut points (men: quartile 1: 0 to <4.50; quartile 2: 4.50 to <6.25; quartile 3: 6.25 to <7.75; quartile 4: 7.75 to 12; women: quartile 1: 0 to <4.75; quartile 2: 4.75 to <6.25; quartile 3: 6.25 to <8.00; quartile 4: 8.00 to 12).
Includes individuals who identified as more than 1 minority race or ethnicity.
Comorbidities include diabetes; high blood pressure; high cholesterol; cancer; myocardial infarction; heart bypass surgery, angioplasty, or stent; stroke; and emphysema, chronic bronchitis, or chronic obstructive pulmonary disease.
All key exposures were statistically significantly associated with overall poor diet quality (Table 2; eFigures 1-5 in the Supplement). Adjusting for age, sex, and energy intake (model 1), American Indian and Alaska Native participants had 18% (95% CI, 5%-33%) higher odds of poor overall diet quality, and Black participants had 14% (95% CI, 6%-23%) higher odds of poor overall diet quality, compared with White participants. However, with mutual adjustment for other key exposures (model 2), the association for American Indian and Alaska Native participants was no longer statistically significant (eFigure 1 in the Supplement). American Indian and Alaska Native participants had higher odds of poor scores for red and processed meats and SSBs. Black participants had higher risk of poor vegetable and SSB scores, and lower risk of a poor HPF and refined grains score (ie, better concordance with recommendations) compared with White participants. In models including BMI, alcohol, and comorbidity score (model 3), Black race and ethnicity was no longer associated with poor diet quality. Study participants who identified as Asian, Native Hawaiian, and Pacific Islander; Hispanic/Latino; and as other race and ethnicity had significantly lower odds of poor diet quality, compared with White participants. Asian, Native Hawaiian, and Pacific Islander participants had lower odds of poor component scores (except for whole grains) compared with White participants (Table 2).
Table 2. Socioeconomic and Geographic Factors Associated With Poor Diet Quality Overall and Poor Diet Quality Component Scoresa .
| Factor | Outcome, OR (95% CI) | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Poor overall diet quality | Poor individual diet component scoreb | ||||||||
| Model 1c | Model 2d | Model 3e | Vegetables | Fruits | Whole grains | RP meats | SSB | HPF/RG | |
| Race and ethnicity | |||||||||
| American Indian or Alaska Native | 1.18 (1.05-1.33) | 1.04 (0.92-1.18) | 0.96 (0.85-1.09) | 0.88 (0.76-1.03) | 1.12 (0.98-1.29) | 0.99 (0.87-1.13) | 1.18 (1.04-1.34) | 1.21 (1.07-1.38) | 0.78 (0.69-0.89) |
| Asian, Native Hawaiian, or Pacific Islander | 0.54 (0.49-0.60) | 0.67 (0.60-0.74) | 0.69 (0.62-0.77) | 0.56 (0.50-0.64) | 0.77 (0.69-0.86) | 1.19 (1.08-1.30) | 0.66 (0.60-0.74) | 0.67 (0.59-0.75) | 0.83 (0.76-0.91) |
| Black | 1.14 (1.06-1.23) | 1.16 (1.08-1.25) | 0.96 (0.89-1.03) | 1.10 (1.01-1.20) | 1.09 (1.00-1.18) | 0.92 (0.85-1.00) | 1.03 (0.95-1.12) | 2.30 (2.14-2.48) | 0.58 (0.53-0.63) |
| Hispanic | 0.87 (0.82-0.92) | 0.84 (0.79-0.88) | 0.81 (0.76-0.85) | 0.97 (0.91-1.03) | 0.87 (0.82-0.93) | 0.91 (0.86-0.97) | 0.92 (0.87-0.98) | 1.00 (0.94-1.06) | 0.74 (0.70-0.79) |
| White | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| Otherf | 0.71 (0.62-0.82) | 0.71 (0.61-0.81) | 0.66 (0.57-0.76) | 0.72 (0.61-0.85) | 0.84 (0.72-0.99) | 1.03 (0.89-1.18) | 0.76 (0.66-0.88) | 1.03 (0.89-1.18) | 0.55 (0.48-0.64) |
| Income, $ | |||||||||
| <25 000 | 1.25 (1.17-1.33) | 1.08 (1.02-1.15) | 1.01 (0.94-1.07) | 1.27 (1.18-1.37) | 1.26 (1.17-1.35) | 1.06 (0.99-1.14) | 0.88 (0.83-0.95) | 1.28 (1.19-1.36) | 0.93 (0.87-0.99) |
| 25 000 to <50 000 | 1.20 (1.15-1.26) | 1.10 (1.05-1.15) | 1.06 (1.02-1.11) | 1.14 (1.08-1.20) | 1.14 (1.09-1.20) | 1.03 (0.99-1.08) | 1.01 (0.96-1.05) | 1.17 (1.12-1.23) | 1.02 (0.98-1.07) |
| 50 000 to <75 000 | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| 75 000 to <100 000 | 0.89 (0.85-0.92) | 0.95 (0.92-0.99) | 0.98 (0.94-1.02) | 0.91 (0.87-0.96) | 0.91 (0.87-0.95) | 1.02 (0.98-1.06) | 1.00 (0.96-1.04) | 0.85 (0.81-0.88) | 0.94 (0.90-0.98) |
| 100 000 to <125 000 | 0.78 (0.75-0.81) | 0.89 (0.86-0.93) | 0.96 (0.92-1.00) | 0.86 (0.82-0.90) | 0.85 (0.81-0.89) | 0.98 (0.94-1.02) | 1.00 (0.96-1.05) | 0.77 (0.73-0.80) | 0.94 (0.90-0.97) |
| 125 000 to <150 000 | 0.69 (0.65-0.72) | 0.83 (0.79-0.87) | 0.92 (0.87-0.97) | 0.74 (0.70-0.78) | 0.81 (0.77-0.86) | 1.03 (0.98-1.08) | 0.97 (0.92-1.02) | 0.69 (0.65-0.73) | 0.89 (0.85-0.93) |
| ≥150 000 | 0.54 (0.52-0.56) | 0.71 (0.68-0.74) | 0.84 (0.80-0.87) | 0.69 (0.65-0.72) | 0.77 (0.73-0.80) | 1.03 (0.99-1.07) | 0.86 (0.83-0.90) | 0.55 (0.53-0.58) | 0.78 (0.75-0.81) |
| Educational level | |||||||||
| ≤High school | 2.35 (2.25-2.46) | 1.99 (1.90-2.09) | 1.83 (1.75-1.92) | 1.50 (1.42-1.58) | 1.63 (1.55-1.72) | 1.63 (1.55-1.71) | 1.43 (1.36-1.50) | 1.66 (1.58-1.75) | 1.29 (1.23-1.35) |
| Some college or 2-y degree | 1.57 (1.53-1.62) | 1.42 (1.38-1.47) | 1.32 (1.28-1.36) | 1.11 (1.07-1.15) | 1.23 (1.19-1.28) | 1.33 (1.29-1.38) | 1.33 (1.29-1.37) | 1.36 (1.32-1.41) | 1.08 (1.05-1.12) |
| College graduate | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| Graduate degree | 0.72 (0.70-0.74) | 0.76 (0.73-0.78) | 0.77 (0.75-0.80) | 0.84 (0.81-0.87) | 0.84 (0.81-0.88) | 0.88 (0.85-0.91) | 0.76 (0.74-0.79) | 0.82 (0.79-0.85) | 0.97 (0.94-1.00) |
| RUCA | |||||||||
| Metropolitan | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| Micropolitan | 1.76 (1.69-1.83) | 1.50 (1.44-1.56) | 1.43 (1.38-1.49) | 1.21 (1.15-1.26) | 1.18 (1.12-1.23) | 1.01 (0.97-1.06) | 1.46 (1.40-1.52) | 1.37 (1.31-1.43) | 1.20 (1.15-1.24) |
| Small town | 1.89 (1.77-2.01) | 1.54 (1.44-1.64) | 1.48 (1.38-1.59) | 1.22 (1.12-1.32) | 1.14 (1.05-1.23) | 1.03 (0.95-1.11) | 1.64 (1.53-1.76) | 1.28 (1.19-1.38) | 1.12 (1.05-1.20) |
| Rural | 1.99 (1.83-2.16) | 1.61 (1.48-1.75) | 1.55 (1.42-1.69) | 1.34 (1.21-1.48) | 1.19 (1.07-1.32) | 1.00 (0.91-1.10) | 1.80 (1.65-1.96) | 1.19 (1.08-1.32) | 1.12 (1.02-1.22) |
| Residing in a food desert | |||||||||
| No | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] |
| Yes | 1.43 (1.37-1.50) | 1.17 (1.12-1.22) | 1.12 (1.07-1.17) | 1.05 (0.99-1.10) | 1.08 (1.03-1.14) | 1.08 (1.03-1.14) | 1.14 (1.09-1.20) | 1.17 (1.11-1.22) | 0.99 (0.95-1.04) |
Abbreviations: HPF/RG, highly processed foods and refined grains; RP, red and processed; RUCA, rural-urban commuting area; SSB, sugar sweetened beverages.
Total scores range from 0 to 12, with higher score indicating better diet quality. Poor overall diet quality is defined as a diet score in the bottom sex-specific quartile (men: 0 to <4.50; women: 0 to <4.75); poor component scores have a score of 0 (lowest sex-specific quartile) for servings per day (vegetables: men, ≤2.1; women, ≤2.4; fruit: men, ≤0.9; women, ≤1.1; whole grains: men, ≤0.7; women, ≤0.7; RP meat: men, >1.5; women, >1.2; HPF/RG: men, >39% kcal; women, >40% kcal). Poor SSB scores are defined as 3 or more servings per week in men and in women. Poor SSB scores were liberalized from the 7 or more servings per week cut point for the overall score (eTable 1 in the Supplement) to increase the percentage exposed to 26% for men and 16% for women, comparable to proportions for other components.
Model 2 (adjusted for age, sex, energy intake, and mutually adjusted for all main exposures) was used for the analyses by diet score components. Poor component scores represented less vegetables, fruits, whole grains and more RP meats, SSBs, and HPF/RG.
Adjusted for age, sex, and energy intake.
Mutually adjusted for all main exposures, age, sex, and energy intake.
Mutually adjusted for all main exposures, age, sex, energy intake, and additional covariates, including body mass index (calculated as weight in kilograms divided by height in meters squared and categorized as <25, 25 to <30, 30 to <35, ≥35, and missing), alcohol intake (none, >0 to 1 drink per day, >1-2 drinks per day, >2 drinks per day, and missing), and a comorbidity score (includes diabetes; high blood pressure; high cholesterol; cancer; myocardial infarction; heart bypass surgery, angioplasty, or stent; stroke; and emphysema, chronic bronchitis, or chronic obstructive pulmonary disease; 1 point for each; modeled as 0, 1, and ≥2).
Includes individuals who identified as more than 1 minority race or ethnicity.
Higher income and education were inversely and independently associated with risk of poor diet quality (Table 2; eFigure 2 and eFigure 3 in the Supplement). Each were each associated with better component scores, except income was not associated with higher whole grain scores. Participants in the lowest and highest income levels had higher (better) scores for red and processed meat recommendations than other income categories. Living in a nonmetropolitan area was associated with poorer diet quality, except for whole grains (Table 2; eFigure 4 in the Supplement), and residence in a food desert was independently associated with overall poor diet quality and poor diet components except HPF and refined grains (Table 2; eFigure 5 in the Supplement).
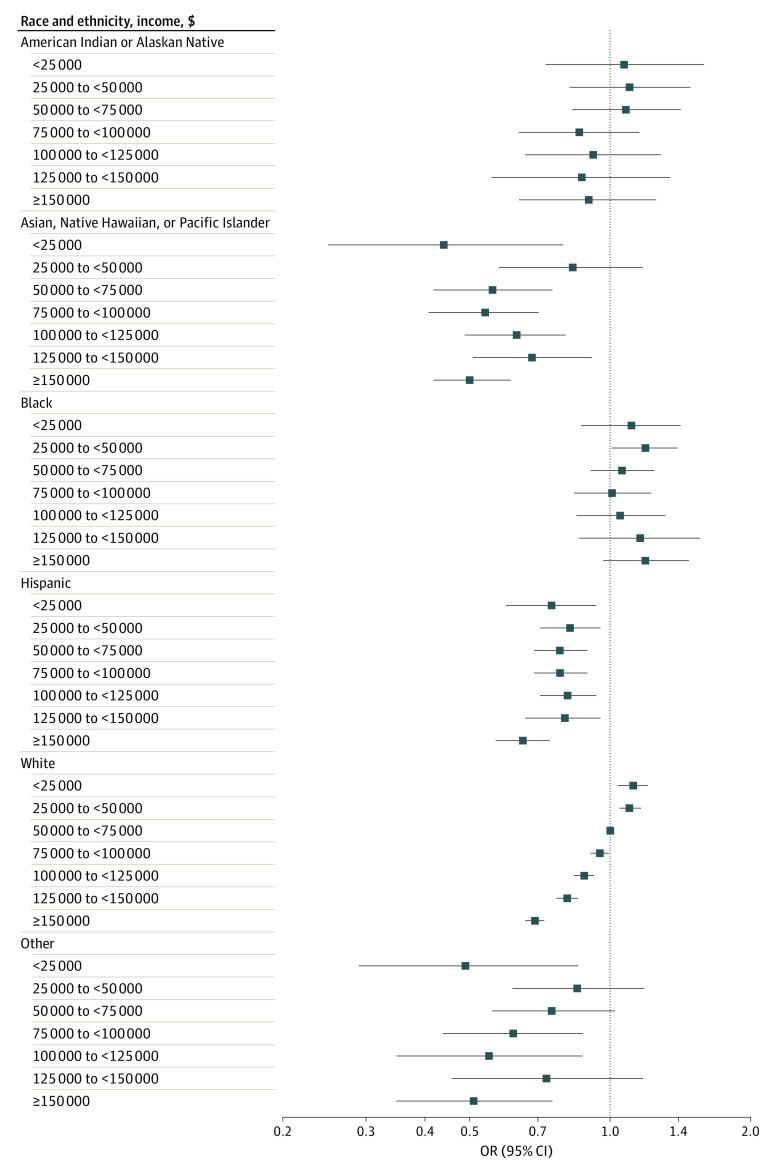
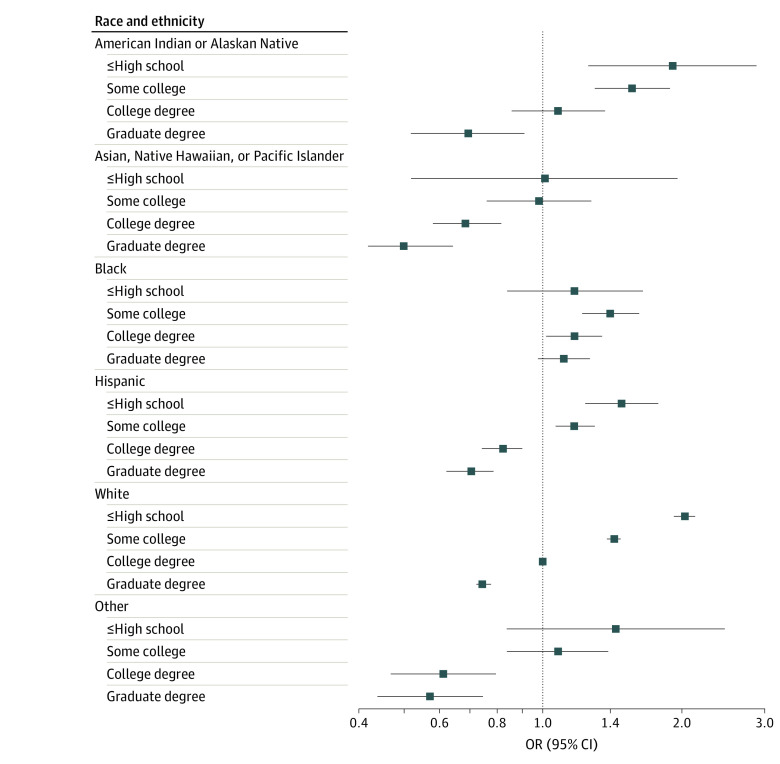
Several significant interactions emerged across the exposures examined. Among White participants, higher income was incrementally associated with lower risk of poor diet quality (Figure 1; eTable 2 in the Supplement). However, compared with White participants earning $50 000 to less than $75 000, Black participants had 19% higher odds of poor diet quality at $25 000 to less than $50 000 per year (odds ratio, 1.19, 95% CI, 1.01-1.39) and diet quality was not higher with greater income. Asian, Native Hawaiian, or Pacific Islander individuals; Hispanic individuals; and individuals in the other racial and ethnic group had better diet quality at almost all income levels compared with the reference group. Educational attainment was associated with diet quality in all racial and ethnic groups, except for Black participants (Figure 2; eTable 2 in the Supplement). Greater educational attainment was also linearly associated with better diet quality in all rural and urban settings (eTable 3 and eFigure 6 in the Supplement). However, compared with college-educated participants residing in a metropolitan setting, individuals at all education levels in nonmetropolitan settings had higher risk of poor diet quality. Living in a food desert was associated with higher risk of poor diet quality in all 4 residential groups compared with individuals residing in a metropolitan setting who are not in a food desert; however, within micropolitan and rural locations, living in a food desert did not further increase risk (eTable 3 in the Supplement). No other statistically significant interactions were observed.
Figure 1. Association of Income Level and Risk of Poor Diet Quality, by Race and Ethnicity.
Odds ratio (OR) and 95% CI of lowest quartile of American Cancer Society diet quality score overall by income and stratified by race and ethnicity. Models included age, sex, energy intake, race and ethnicity, income, education, Rural-Urban Commuting Area code, and residence in a food desert, and a race × income interaction term. The reference group was White participants with income $50 000 to less than $75 000. P for interaction = .01.
Figure 2. Association of Educational Attainment With Risk of Poor Diet Quality, by Race and Ethnicity.
Odds ratio (OR) and 95% CI of lowest quartile of American Cancer Society diet score overall, by attained education, stratified by race and ethnicity. Models included age, sex, energy intake, race and ethnicity, income, education, Rural-Urban Commuting Area code, and residence in a food desert, and a race × education interaction term. The Reference group was White participants with a college degree. P for interaction < .001.
Discussion
In this cross-sectional study of a demographically and geographically diverse cohort of 155 331 US adults, race and ethnicity, income, education, rural vs urban residence, and living in a food desert all were independently associated with poor diet quality. Compared with White participants, Black participants were at higher risk of poor diet quality and Asian, Native Hawaiian, and Pacific Islander and Hispanic/Latino participants were at lower risk in models mutually adjusted for socioeconomic and geographic factors. Higher income and education had protective associations against poor diet quality, but these associations were not the same across all racial and ethnic groups. In addition, while higher education was associated with better diet quality across the urban-rural spectrum, people with higher education living in nonmetropolitan areas still had lower diet quality than their counterparts living in metropolitan areas.
Disparities across poor dietary component scores are worth noting. Black participants had lower vegetable and fruit scores compared with White participants, consistent with national data showing Black persons having the lowest percentage meeting recommended vegetable intake (5.5% of Black persons; 10.5% of Hispanic/Latino persons; 9.5% of White persons).22 In this study, Black participants had 130% higher risk of a poor SSB score compared with White participants, while American Indian and Alaska Native adults had a 21% higher risk and Asian, Native Hawaiian, and Pacific Islander adults had a 33% lower risk. Data from NHANES36 show that the proportion of total beverage consumption as SSBs in the US is highest among Black (15%) and Hispanic/Latino (14%) adults, compared with Asian (4%) and White (9%) adults. While estimates of SSB intake in American Indian and Alaska Native adults are scant, a narrative review37 and NHIS data38 suggest high intakes in this group. Among other factors, SSBs are associated with weight gain, overweight, and obesity,8 and the prevalence of obesity in US adults is highest for non-Hispanic Black people, lowest for non-Hispanic Asian people, and similar among Hispanic/Latino and non-Hispanic White adults.39 White participants consumed more HPFs compared with other racial and ethnic groups, consistent with studies of shopping behaviors40 and data from NHANES.41 American Indian and Alaska Native participants in this study scored poorly for red and processed meats,42 which are associated with increased risk of several chronic diseases.7,8,43,44,45 American Indian and Alaska Native persons have higher rates of diabetes,37 obesity,46 and colorectal cancer47 than other groups, and are the only racial and ethnic group among whom mortality rates from colorectal cancer are not declining.
Gaps in diet quality by income and education have widened over the past decade in the US.5 Consistent with previous studies,22,48,49,50,51,52,53,54,55 our findings support an association of both income and education with consumption of a healthy diet, but this was not equal across racial and ethnic and geographic groups. Income was associated with diet quality only among White participants; it is possible that other groups have more resiliency (including likelihood to participate in subsidized food programs).56 However, compared with White participants, Black participants at all income and education levels had poorer diet quality. Poorer diet quality among Black participants at all income and education levels highlights the need to better understand factors that influence dietary intake in this population.
Multiple factors may shape diet quality among US Black persons, including cultural traditions, targeted advertising, and food availability, some regardless of income. Cultural eating practices may be influenced by historical trauma, limited access and resulting adaptation,3,57 and social aspects of eating.58 Prime time television shows oriented to Black people assessed in 1999 were 2-fold as likely to air food advertisements as general programming.59 Moreover, programming oriented to Black individuals featured more overweight characters and advertisements for SSBs and candy than general programming. Advertising is also targeted to local geographic areas based on demographic characteristics, such as racial and ethnic composition. In a study of 87 Designated Marketing Areas, each percentage increase in the proportion of the population that was Black was associated with 2.9 additional beverage advertisements and 2.2 additional food advertisements viewed.60 Advertisements of fast food, sweets, and SSBs were particularly prevalent in areas with larger proportions of Black residents with lower income. Furthermore, fewer supermarkets are found in Black vs White neighborhoods,61,62 while prevalence of fast-food restaurants is much higher.63 That risk of poorer diet quality in Black participants was attenuated with control for BMI, comorbidities, and alcohol likely reflects the correlates and/or consequences of dietary behaviors in this population.
The neighborhoods and built environments where people live are important social determinants of health.64 Foods available in rural areas tend to be less healthy, and healthy foods may be more expensive compared with that available in more urban areas.65,66 In the US, trends in diet quality were recently reported to vary by food source, with the retail grocery environment offering the best opportunity for improvements in diet quality.67 However, in rural areas, availability of grocery stores may be lower and availability of convenience stores higher.68 We found that individuals residing in all nonmetropolitan areas had a higher risk of poor diet quality than those in metropolitan areas. Although higher education was associated with mitigating that risk, it did not fully compensate for this increase. Finding solutions to improve diet quality among persons residing in food deserts has been challenging69; such initiatives require community- and system-level partnerships70,71 with attention to cultural relevance of healthy food options.72
Because poor diet quality is influenced by a complex range of interrelated factors, including structural factors, changes in health policies may be required to make a change.73 Health policy initiatives focusing on advertising, taxation, and pricing strategies to increase the competitiveness of more nutritionally dense foods and beverages could play a role in shifting diet quality. For example, SSB taxation is associated with successfully reducing SSB intake in the United Kingdom74 and in other countries, regions, and cities,75 although progress is lagging in the US.
Limitations
This study has some limitations. Findings from this study may not be generalizable to the US population, as CPS-3 had a comparatively higher proportion of women and participants had relatively higher income and educational attainment and less racial and ethnic diversity. However, this large, nationwide cohort included sufficient numbers to examine associations of individual-level geographic and socioeconomic factors simultaneously. Furthermore, the direction of individual associations observed were generally consistent with nationally representative samples. This study included 66 participants who completed the Spanish-language questionnaire; as the diet validation study was conducted in English, we may have overestimated validity of the FFQ in Hispanic/Latino participants. The ideal score we created may not represent an ideal diet in all populations, and the FFQ was likely to lack some important foods in different subpopulations assessed, such as for Asian, Native Hawaiian, and Pacific Islander participants. An additional limitation to this research is the grouping together of heterogenous racial and ethnic groups to preserve statistical power, although variations within these groups are expected. Furthermore, since we categorized biracial White participants as the other race and ethnicity provided, dietary behaviors of these participants may not resonate fully with those of participants who self-identify as primarily American Indian or Alaska Native; Asian, Native Hawaiian, or Pacific Islander; Black; or Hispanic/Latino.
Conclusions
In this cross-sectional study, we found multiple independent factors associated with diet quality in the CPS-3 cohort, including novel interactions among these factors. The ACS Guideline on Diet and Physical Activity for Cancer Prevention,7 provides dietary and lifestyle recommendations to reduce the cancer burden across all populations. These7 and other recommendations76 emphasize the need to examine the social, economic, and environmental contexts that may determine our dietary and lifestyle patterns, which also drive existing health disparities in the US. Further research to understand underlying social constructs driving diet quality, as well as potential barriers to consumption of healthier foods among individuals at risk of poor diet quality, is needed. These factors could be targeted for improved messaging, behavioral interventions, programs, and policies for everyone to have an equal opportunity to eat a healthy diet.
eTable 1. 2020 American Cancer Society Diet Guideline Score
eFigure 1. Association of Race and Ethnicity With Risk of Poor Diet Quality Overall and Poor Diet Component Scores
eFigure 2. Association of Income With Risk of Poor Diet Quality Overall and Poor Diet Component Scores
eFigure 3. Association of Education With Risk of Poor Diet Quality Overall and Poor Diet Component Scores
eFigure 4. Association of RUCA Code With Risk of Poor Diet Quality Overall and Poor Diet Component Scores
eFigure 5. Association of Residence in a Food Desert and Risk of Poor Diet Quality Overall and Poor Diet Component Scores
eTable 2. Social and Demographic Factors Associated With Poor Diet Quality by Race and Ethnicity
eTable 3. Social and Demographic Factors Associated With Poor Diet Quality by Rural-Urban Commuting Area
eFigure 6. Association of Educational Attainment With Risk of Poor Diet Quality, by RUCA
References
- 1.Fleischhacker SE, Woteki CE, Coates PM, et al. Strengthening national nutrition research: rationale and options for a new coordinated federal research effort and authority. Am J Clin Nutr. 2020;112(3):721-769. doi: 10.1093/ajcn/nqaa179 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Siegel RL, Miller KD, Jemal A. Cancer statistics, 2020. CA Cancer J Clin. 2020;70(1):7-30. doi: 10.3322/caac.21590 [DOI] [PubMed] [Google Scholar]
- 3.Lunsford L, Arthur ML, Porter CM. African and Native American foodways and resilience: from 1619 to COVID-19. J Agric Food Syst Community Dev. 2021;10(4):241-265. doi: 10.5304/jafscd.2021.104.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Odoms-Young A, Bruce MA. Examining the impact of structural racism on food insecurity: implications for addressing racial/ethnic disparities. Fam Community Health. 2018;41(Suppl 2 Suppl, Food Insecurity and Obesity):S3-S6. doi: 10.1097/FCH.0000000000000183 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rehm CD, Peñalvo JL, Afshin A, Mozaffarian D. Dietary intake among US adults, 1999-2012. JAMA. 2016;315(23):2542-2553. doi: 10.1001/jama.2016.7491 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Belanger MJ, Hill MA, Angelidi AM, Dalamaga M, Sowers JR, Mantzoros CS. COVID-19 and disparities in nutrition and obesity. N Engl J Med. 2020;383(11):e69. doi: 10.1056/NEJMp2021264 [DOI] [PubMed] [Google Scholar]
- 7.Rock CL, Thomson C, Gansler T, et al. American Cancer Society guideline for diet and physical activity for cancer prevention. CA Cancer J Clin. 2020;70(4):245-271. doi: 10.3322/caac.21591 [DOI] [PubMed] [Google Scholar]
- 8.World Cancer Research Fund . Diet, nutrition, physical activity and cancer: a global perspective. Accessed May 4, 2022. https://www.wcrf.org/wp-content/uploads/2021/02/Summary-of-Third-Expert-Report-2018.pdf
- 9.Arnett DK, Blumenthal RS, Albert MA, et al. 2019 ACC/AHA guideline on the primary prevention of cardiovascular disease: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2019;140(11):e563-e595. doi: 10.1161/CIR.0000000000000677 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Evert AB, Dennison M, Gardner CD, et al. Nutrition therapy for adults with diabetes or prediabetes: a consensus report. Diabetes Care. 2019;42(5):731-754. doi: 10.2337/dci19-0014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.US Department of Agriculture; US Department of Health and Human Services . Dietary guidelines for Americans, 2020-2025. 2020. Accessed May 4, 2022. https://www.dietaryguidelines.gov/sites/default/files/2020-12/Dietary_Guidelines_for_Americans_2020-2025.pdf
- 12.Liese AD, Krebs-Smith SM, Subar AF, et al. The Dietary Patterns Methods Project: synthesis of findings across cohorts and relevance to dietary guidance. J Nutr. 2015;145(3):393-402. doi: 10.3945/jn.114.205336 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kabat GC, Matthews CE, Kamensky V, Hollenbeck AR, Rohan TE. Adherence to cancer prevention guidelines and cancer incidence, cancer mortality, and total mortality: a prospective cohort study. Am J Clin Nutr. 2015;101(3):558-569. doi: 10.3945/ajcn.114.094854 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.McCullough ML, Patel AV, Kushi LH, et al. Following cancer prevention guidelines reduces risk of cancer, cardiovascular disease, and all-cause mortality. Cancer Epidemiol Biomarkers Prev. 2011;20(6):1089-1097. doi: 10.1158/1055-9965.EPI-10-1173 [DOI] [PubMed] [Google Scholar]
- 15.Thomson CA, McCullough ML, Wertheim BC, et al. Nutrition and physical activity cancer prevention guidelines, cancer risk, and mortality in the women’s health initiative. Cancer Prev Res (Phila). 2014;7(1):42-53. doi: 10.1158/1940-6207.CAPR-13-0258 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Warren Andersen S, Blot WJ, Shu XO, et al. Adherence to cancer prevention guidelines and cancer risk in low-income and African American populations. Cancer Epidemiol Biomarkers Prev. 2016;25(5):846-853. doi: 10.1158/1055-9965.EPI-15-1186 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Islami F, Goding Sauer A, Miller KD, et al. Proportion and number of cancer cases and deaths attributable to potentially modifiable risk factors in the United States. CA Cancer J Clin. 2018;68(1):31-54. doi: 10.3322/caac.21440 [DOI] [PubMed] [Google Scholar]
- 18.Zhang FF, Cudhea F, Shan Z, et al. Preventable cancer burden associated with poor diet in the United States. JNCI Cancer Spectr. 2019;3(2):pkz034. doi: 10.1093/jncics/pkz034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wang L, Du M, Cudhea F, et al. Disparities in health and economic burdens of cancer attributable to suboptimal diet in the United States, 2015‒2018. Am J Public Health. 2021;111(11):2008-2018. doi: 10.2105/AJPH.2021.306475 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.American Cancer Society . Cancer prevention and early detection facts and figures 2021-2022. Accessed May 4, 2022. https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/cancer-prevention-and-early-detection-facts-and-figures/2021-cancer-prevention-and-early-detection.pdf
- 21.NCD Risk Factor Collaboration (NCD-RisC) . Rising rural body-mass index is the main driver of the global obesity epidemic in adults. Nature. 2019;569(7755):260-264. doi: 10.1038/s41586-019-1171-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lee-Kwan SH, Moore LV, Blanck HM, Harris DM, Galuska D. Disparities in state-specific adult fruit and vegetable consumption—United States, 2015. MMWR Morb Mortal Wkly Rep. 2017;66(45):1241-1247. doi: 10.15585/mmwr.mm6645a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.US Department of Agriculture; US Department of Health and Human Services . Scientific report of the 2015. U.S. Dietary Guidelines Advisory Committee. Accessed May 4, 2022. https://health.gov/sites/default/files/2019-09/Scientific-Report-of-the-2015-Dietary-Guidelines-Advisory-Committee.pdf
- 24.Zeng L, Ruan M, Liu J, et al. Trends in processed meat, unprocessed red meat, poultry, and fish consumption in the United States, 1999-2016. J Acad Nutr Diet. 2019;119(7):1085-1098.e12. doi: 10.1016/j.jand.2019.04.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Martínez Steele E, Baraldi LG, Louzada ML, Moubarac JC, Mozaffarian D, Monteiro CA. Ultra-processed foods and added sugars in the US diet: evidence from a nationally representative cross-sectional study. BMJ Open. 2016;6(3):e009892. doi: 10.1136/bmjopen-2015-009892 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Patel AV, Jacobs EJ, Dudas DM, et al. The American Cancer Society’s Cancer Prevention Study 3 (CPS-3): recruitment, study design, and baseline characteristics. Cancer. 2017;123(11):2014-2024. doi: 10.1002/cncr.30561 [DOI] [PubMed] [Google Scholar]
- 27.Willett WC, Reynolds RD, Cottrell-Hoehner S, Sampson L, Browne ML. Validation of a semi-quantitative food frequency questionnaire: comparison with a 1-year diet record. J Am Diet Assoc. 1987;87(1):43-47. doi: 10.1016/S0002-8223(21)03057-1 [DOI] [PubMed] [Google Scholar]
- 28.Rimm EB, Giovannucci EL, Stampfer MJ, Colditz GA, Litin LB, Willett WC. Reproducibility and validity of an expanded self-administered semiquantitative food frequency questionnaire among male health professionals. Am J Epidemiol. 1992;135(10):1114-1126. doi: 10.1093/oxfordjournals.aje.a116211 [DOI] [PubMed] [Google Scholar]
- 29.Feskanich D, Rimm EB, Giovannucci EL, et al. Reproducibility and validity of food intake measurements from a semiquantitative food frequency questionnaire. J Am Diet Assoc. 1993;93(7):790-796. doi: 10.1016/0002-8223(93)91754-E [DOI] [PubMed] [Google Scholar]
- 30.McCullough ML, Wang Y, Hartman TJ, et al. The Cancer Prevention Study-3 FFQ is a reliable and valid measure of nutrient intakes among racial/ethnic subgroups, compared with 24-hour recalls and biomarkers. J Nutr. 2021;151(3):636-648. doi: 10.1093/jn/nxaa358 [DOI] [PubMed] [Google Scholar]
- 31.Troeschel AN, Hartman TJ, Flanders WD, et al. The American Cancer Society Cancer Prevention Study-3 FFQ has reasonable validity and reproducibility for food groups and a diet quality score. J Nutr. 2020;150:1566-1578. doi: 10.1093/jn/nxaa082 [DOI] [PubMed] [Google Scholar]
- 32.Havranek EP, Mujahid MS, Barr DA, et al. ; American Heart Association Council on Quality of Care and Outcomes Research, Council on Epidemiology and Prevention, Council on Cardiovascular and Stroke Nursing, Council on Lifestyle and Cardiometabolic Health, and Stroke Council . Social determinants of risk and outcomes for cardiovascular disease: a scientific statement from the American Heart Association. Circulation. 2015;132(9):873-898. doi: 10.1161/CIR.0000000000000228 [DOI] [PubMed] [Google Scholar]
- 33.Texas A&M University . TAMU GeoServices. Accessed August 31, 2020. https://geoservices.tamu.edu/
- 34.USDA Economic Research Service . Rural-urban commuting area codes. Accessed August 31, 2020. https://www.ers.usda.gov/data-products/rural-urban-commuting-area-codes/https://www.ers.usda.gov/data-products/rura-urban-communiting-area-codes
- 35.USDA Economic Research Service . Food Access Research Atlas. Accessed October 30, 2020. https://www.ers.usda.gov/data-products/food-access-research-atlas/
- 36.Martin CB, Wambogo EA, Ahluwalia N, Ogden CL. Nonalcoholic beverage consumption among adults: United States, 2015-2018. NCHS Data Brief. 2020;(376):1-8. [PubMed] [Google Scholar]
- 37.Yracheta JM, Lanaspa MA, Le MT, et al. Diabetes and kidney disease in American Indians: potential role of sugar-sweetened beverages. Mayo Clin Proc. 2015;90(6):813-823. doi: 10.1016/j.mayocp.2015.03.018 [DOI] [PubMed] [Google Scholar]
- 38.Thompson FE, McNeel TS, Dowling EC, Midthune D, Morrissette M, Zeruto CA. Interrelationships of added sugars intake, socioeconomic status, and race/ethnicity in adults in the United States: National Health Interview Survey, 2005. J Am Diet Assoc. 2009;109(8):1376-1383. doi: 10.1016/j.jada.2009.05.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hales CM, Carroll MD, Fryar CD, Ogden CL. Prevalence of obesity and severe obesity among adults: United States, 2017-2018. NCHS Data Brief. 2020;(360):1-8. [PubMed] [Google Scholar]
- 40.Poti JM, Mendez MA, Ng SW, Popkin BM. Highly processed and ready-to-eat packaged food and beverage purchases differ by race/ethnicity among US households. J Nutr. 2016;146(9):1722-1730. doi: 10.3945/jn.116.230441 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Eicher-Miller HA, Fulgoni VL III, Keast DR. Energy and nutrient intakes from processed foods differ by sex, income status, and race/ethnicity of US adults. J Acad Nutr Diet. 2015;115(6):907-18.e6. doi: 10.1016/j.jand.2014.11.004 [DOI] [PubMed] [Google Scholar]
- 42.IARC Working Group . Red Meat and Processed Meat: IARC Working Group on the Evaluation of Carcinogenic Risks to Humans. International Agency for Research on Cancer; 2015. [PubMed] [Google Scholar]
- 43.Fretts AM, Howard BV, McKnight B, et al. Associations of processed meat and unprocessed red meat intake with incident diabetes: the Strong Heart Family Study. Am J Clin Nutr. 2012;95(3):752-758. doi: 10.3945/ajcn.111.029942 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Schwingshackl L, Hoffmann G, Lampousi AM, et al. Food groups and risk of type 2 diabetes mellitus: a systematic review and meta-analysis of prospective studies. Eur J Epidemiol. 2017;32(5):363-375. doi: 10.1007/s10654-017-0246-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Wang X, Lin X, Ouyang YY, et al. Red and processed meat consumption and mortality: dose-response meta-analysis of prospective cohort studies. Public Health Nutr. 2016;19(5):893-905. doi: 10.1017/S1368980015002062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Steele CB, Cardinez CJ, Richardson LC, Tom-Orme L, Shaw KM. Surveillance for health behaviors of American Indians and Alaska Natives—findings from the Behavioral Risk Factor Surveillance System, 2000-2006. Cancer. 2008;113(5)(suppl):1131-1141. doi: 10.1002/cncr.23727 [DOI] [PubMed] [Google Scholar]
- 47.Siegel RL, Miller KD, Goding Sauer A, et al. Colorectal cancer statistics, 2020. CA Cancer J Clin. 2020;70(3):145-164. doi: 10.3322/caac.21601 [DOI] [PubMed] [Google Scholar]
- 48.Park SY, Shvetsov YB, Kang M, et al. Changes in diet quality over 10 years are associated with baseline sociodemographic and lifestyle factors in the Multiethnic Cohort Study. J Nutr. 2020;150(7):1880-1888. doi: 10.1093/jn/nxaa102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Hsiao PY, Mitchell DC, Coffman DL, et al. Dietary patterns and diet quality among diverse older adults: the University of Alabama at Birmingham Study of Aging. J Nutr Health Aging. 2013;17(1):19-25. doi: 10.1007/s12603-012-0082-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Irala-Estévez JD, Groth M, Johansson L, Oltersdorf U, Prättälä R, Martínez-González MA. A systematic review of socio-economic differences in food habits in Europe: consumption of fruit and vegetables. Eur J Clin Nutr. 2000;54(9):706-714. doi: 10.1038/sj.ejcn.1601080 [DOI] [PubMed] [Google Scholar]
- 51.Gibson R, Eriksen R, Singh D, et al. A cross-sectional investigation into the occupational and socio-demographic characteristics of British police force employees reporting a dietary pattern associated with cardiometabolic risk: findings from the Airwave Health Monitoring Study. Eur J Nutr. 2018;57(8):2913-2926. doi: 10.1007/s00394-017-1562-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Maugeri A, Barchitta M, Fiore V, et al. Determinants of adherence to the Mediterranean diet: findings from a cross-sectional study in women from Southern Italy. Int J Environ Res Public Health. 2019;16(16):E2963. doi: 10.3390/ijerph16162963 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Petrenya N, Rylander C, Brustad M. Dietary patterns of adults and their associations with Sami ethnicity, sociodemographic factors, and lifestyle factors in a rural multiethnic population of northern Norway—the SAMINOR 2 clinical survey. BMC Public Health. 2019;19(1):1632. doi: 10.1186/s12889-019-7776-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Marques-Vidal P, Waeber G, Vollenweider P, Guessous I. Socio-demographic and lifestyle determinants of dietary patterns in French-speaking Switzerland, 2009-2012. BMC Public Health. 2018;18(1):131. doi: 10.1186/s12889-018-5045-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Grech A, Rangan A, Allman-Farinelli M. Social determinants and poor diet quality of energy-dense diets of Australian young adults. Healthcare (Basel). 2017;5(4):E70. doi: 10.3390/healthcare5040070 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Allen AJ, Kuczmarski MF, Evans MK, Zonderman AB, Waldstein SR. Race differences in diet quality of urban food-insecure Blacks and Whites reveals resiliency in Blacks. J Racial Ethn Health Disparities. 2016;3(4):706-712. doi: 10.1007/s40615-015-0189-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Airhihenbuwa CO, Kumanyika S, Agurs TD, Lowe A, Saunders D, Morssink CB. Cultural aspects of African American eating patterns. Ethn Health. 1996;1(3):245-260. doi: 10.1080/13557858.1996.9961793 [DOI] [PubMed] [Google Scholar]
- 58.Sankofa J, Johnson-Taylor WL. News coverage of diet-related health disparities experienced by Black Americans: a steady diet of misinformation. J Nutr Educ Behav. 2007;39(2)(suppl):S41-S44. doi: 10.1016/j.jneb.2006.08.014 [DOI] [PubMed] [Google Scholar]
- 59.Tirodkar MA, Jain A. Food messages on African American television shows. Am J Public Health. 2003;93(3):439-441. doi: 10.2105/AJPH.93.3.439 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Powell LM, Wada R, Kumanyika SK. Racial/ethnic and income disparities in child and adolescent exposure to food and beverage television ads across the U.S. media markets. Health Place. 2014;29:124-131. doi: 10.1016/j.healthplace.2014.06.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Zenk SN, Schulz AJ, Israel BA, James SA, Bao S, Wilson ML. Neighborhood racial composition, neighborhood poverty, and the spatial accessibility of supermarkets in metropolitan Detroit. Am J Public Health. 2005;95(4):660-667. doi: 10.2105/AJPH.2004.042150 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Larson NI, Story MT, Nelson MC. Neighborhood environments: disparities in access to healthy foods in the U.S. Am J Prev Med. 2009;36(1):74-81. doi: 10.1016/j.amepre.2008.09.025 [DOI] [PubMed] [Google Scholar]
- 63.James P, Arcaya MC, Parker DM, Tucker-Seeley RD, Subramanian SV. Do minority and poor neighborhoods have higher access to fast-food restaurants in the United States? Health Place. 2014;29:10-17. doi: 10.1016/j.healthplace.2014.04.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Centers for Disease Control and Prevention . Social determinants of health. Accessed September 7, 2021. https://www.cdc.gov/publichealthgateway/sdoh/index.html
- 65.Hardin-Fanning F, Rayens MK. Food cost disparities in rural communities. Health Promot Pract. 2015;16(3):383-391. doi: 10.1177/1524839914554454 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Darmon N, Drewnowski A. Contribution of food prices and diet cost to socioeconomic disparities in diet quality and health: a systematic review and analysis. Nutr Rev. 2015;73(10):643-660. doi: 10.1093/nutrit/nuv027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Liu J, Micha R, Li Y, Mozaffarian D. Trends in food sources and diet quality among US children and adults, 2003-2018. JAMA Netw Open. 2021;4(4):e215262. doi: 10.1001/jamanetworkopen.2021.5262 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Liese AD, Weis KE, Pluto D, Smith E, Lawson A. Food store types, availability, and cost of foods in a rural environment. J Am Diet Assoc. 2007;107(11):1916-1923. doi: 10.1016/j.jada.2007.08.012 [DOI] [PubMed] [Google Scholar]
- 69.Block JP, Subramanian SV. Moving beyond “food deserts”: reorienting United States policies to reduce disparities in diet quality. PLoS Med. 2015;12(12):e1001914. doi: 10.1371/journal.pmed.1001914 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Larson C, Haushalter A, Buck T, Campbell D, Henderson T, Schlundt D. Development of a community-sensitive strategy to increase availability of fresh fruits and vegetables in Nashville’s urban food deserts, 2010-2012. Prev Chronic Dis. 2013;10:E125. doi: 10.5888/pcd10.130008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Shahid SM, Bishop KS. Comprehensive approaches to improving nutrition: future prospects. Nutrients. 2019;11(8):E1760. doi: 10.3390/nu11081760 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Grigsby-Toussaint DS, Zenk SN, Odoms-Young A, Ruggiero L, Moise I. Availability of commonly consumed and culturally specific fruits and vegetables in African-American and Latino neighborhoods. J Am Diet Assoc. 2010;110(5):746-752. doi: 10.1016/j.jada.2010.02.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Brug J, van der Ploeg HP, Loyen A, et al. ; DEDIPAC consortium . Determinants of diet and physical activity (DEDIPAC): a summary of findings. Int J Behav Nutr Phys Act. 2017;14(1):150. doi: 10.1186/s12966-017-0609-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Bandy LK, Scarborough P, Harrington RA, Rayner M, Jebb SA. Reductions in sugar sales from soft drinks in the UK from 2015 to 2018. BMC Med. 2020;18(1):20. doi: 10.1186/s12916-019-1477-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Krieger J, Bleich SN, Scarmo S, Ng SW. Sugar-sweetened beverage reduction policies: progress and promise. Annu Rev Public Health. 2021;42:439-461. doi: 10.1146/annurev-publhealth-090419-103005 [DOI] [PubMed] [Google Scholar]
- 76.Dietary Guidelines Advisory Committee . Scientific Report of the 2020 Dietary Guidelines Advisory Committee: Advisory Report to the Secretary of Agriculture and Secretary of Health and Human Services. US Department of Agriculture, Agricultural Research Service; 2020. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable 1. 2020 American Cancer Society Diet Guideline Score
eFigure 1. Association of Race and Ethnicity With Risk of Poor Diet Quality Overall and Poor Diet Component Scores
eFigure 2. Association of Income With Risk of Poor Diet Quality Overall and Poor Diet Component Scores
eFigure 3. Association of Education With Risk of Poor Diet Quality Overall and Poor Diet Component Scores
eFigure 4. Association of RUCA Code With Risk of Poor Diet Quality Overall and Poor Diet Component Scores
eFigure 5. Association of Residence in a Food Desert and Risk of Poor Diet Quality Overall and Poor Diet Component Scores
eTable 2. Social and Demographic Factors Associated With Poor Diet Quality by Race and Ethnicity
eTable 3. Social and Demographic Factors Associated With Poor Diet Quality by Rural-Urban Commuting Area
eFigure 6. Association of Educational Attainment With Risk of Poor Diet Quality, by RUCA