Abstract
Background
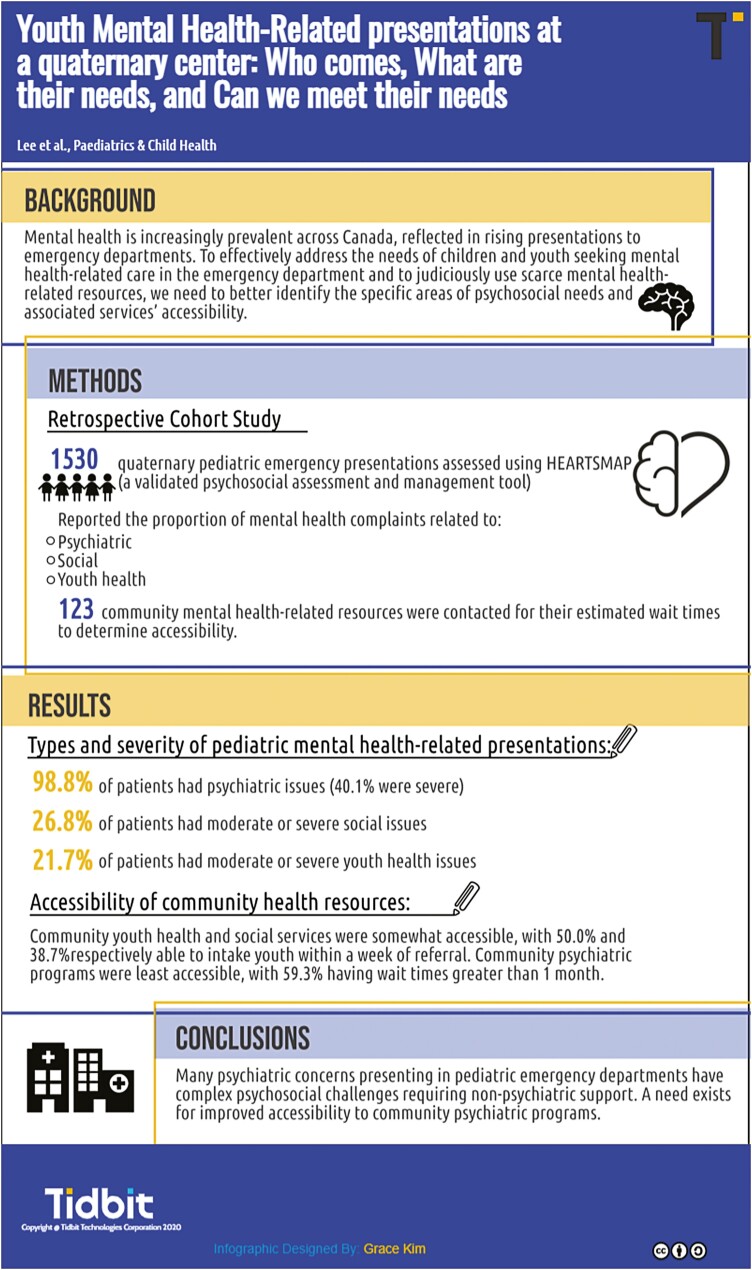
Mental health issues are increasingly prevalent across Canada, reflected in rising presentations to emergency departments. To effectively address the needs of children and youth seeking mental health-related care in the emergency department and to judiciously use scarce mental health-related resources, we need to better identify the specific areas of psychosocial needs and accessibility of associated services.
Objective
To describe the types and severity of paediatric mental health-related presentations evaluated at a quaternary paediatric emergency department, and to explore the accessibility of community mental health-related resources.
Methods
We conducted a retrospective cohort study of children and youth presenting to a quaternary paediatric emergency department who were assessed using HEARTSMAP, a validated mental health assessment and management tool. We reported the proportion who sought care for a psychiatric, social, or youth health-related mental health complaint. We contacted community mental health-related resources for their estimated wait times to determine accessibility.
Results
Of 1,530 paediatric emergency presentations, 98.8% of patients had psychiatric issues (40.1% were severe), 78.0% of patients had social issues (17.1% were severe), and 71.5% had youth health issues (18.1% were severe). We contacted 123 community mental health-related resources. Community youth health and social services were somewhat accessible, with 50.0% and 38.7%, respectively, able to intake youth within a week of referral. Community psychiatric programs were least accessible, with 59.3% having wait times greater than 1 month.
Conclusions
Many psychiatric concerns presenting in paediatric emergency departments have complex psychosocial challenges requiring non-psychiatric support. A need exists for improved accessibility to community psychiatric programs.
Keywords: Child, Emergency medicine, Mental disorders, Mental health, Youth
Graphical Abstract
pxab091_graphical_abstract.
BACKGROUND AND RATIONALE
Paediatric mental health conditions are increasingly prevalent in Canada. In British Columbia (BC), it is estimated that 12.6% of children and youth have a clinically diagnosable mental health disorder (1). Mental health-related presentations are also increasing in emergency departments (EDs) across North America at rates of 3.1% to 8.6% per year (2–4).
A large proportion of the increase in mental health-related presentations is attributed to lower acuity presentations that do not require hospitalization (2,5–7). A study in Ontario, Canada, found that more than 50% of families presenting to the ED for mental health-related concerns had no previous contact with the mental health care system (8). While acute psychiatric crises requiring medical management or emergent psychiatric stabilization are best addressed through the ED, many undifferentiated psychosocial concerns and resource navigation questions are being queried (2,5,7,9). Given that the majority of patients presenting with mental health concerns do not require hospitalization and can be directed to outpatient programs (9), it is pertinent to determine the range of resources needed by this population.
Mental health-related presentations encompass a broad range of psychosocial concerns, many of which are best served by specialized multidisciplinary teams in the community (10). Emergency physicians often lack the expertise and knowledge of community resources when managing less acute psychosocial concerns (11–13). HEARTSMAP was created in 2016 as an assessment and management tool to better address the wide berth of mental health presentations in the ED. This validated online tool distinguishes severity, acuity, and type of mental health concerns, and provides appropriate management recommendations (14–16).
HEARTSMAP standardizes care and management in the ED, but also documents resource needs of children and youth with mental health-related presentations upon discharge from the ED. Previous literature has shown that both patients and clinicians perceive difficulty in accessing community resources (12,17,18), and mainstream media has discussed general provincial mental health resource shortages (19). In BC and Alberta, over 30% of patients with mental health-related concerns present to the ED multiple times, suggesting a lack of timely resources available (2,3).
Although HEARTSMAP is currently implemented at our ED to standardize and guide the management for ED mental health-related presentations (14,20), its ultimate disposition plans and resource referral distribution have not yet been evaluated. This study aims to describe the range of psychosocial issues of patients presenting to a quaternary ED with a mental health-related concern and document the types of mental health resources recommended for management. We will also reflect the resource needs distribution against BC’s infrastructure to explore its readiness to meet the needs of our youth with mental health-related emergency presentations. Youth mental health resource needs have garnered increasing attention and funding announcements during the current pandemic. The outcomes of this study will inform funding allocation to address unmet needs of children and youth seeking mental health-related care in the ED setting.
METHODS
Design, population, and setting
We conducted a retrospective cohort study of children and youth seeking care at the BC Children’s Hospital (BCCH) ED with a mental health-related presentation, assessed and managed using HEARTSMAP, between October 1 2016 and June 30 2019. BCCH is the only quaternary care paediatric emergency department (PED) in the province of British Columbia, Canada. This study was reviewed and approved by the University of British Columbia Children’s and Women’s Health Centre of British Columbia Research Ethics Board.
Objectives and outcome measures
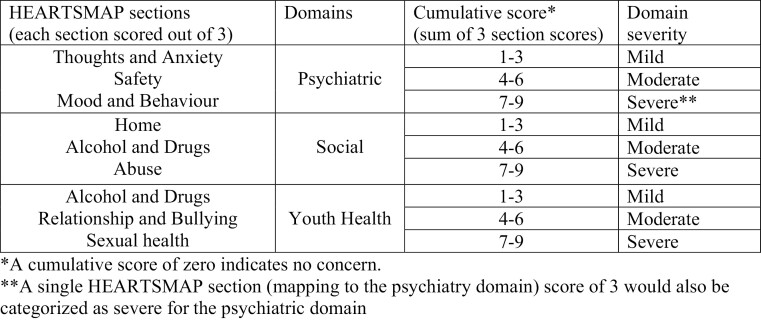
The primary objective was to describe both the types (psychiatric, youth health—pertaining to sexual health and substance-related issues, social) and severity of mental health issues (mild, moderate, or severe) presenting to a PED and to document the types and urgency levels of mental health resources needed. The severity of psychosocial issues was determined using HEARTSMAP cumulative domain scores. The severity scoring scheme is shown in Figure 1. To determine the types of mental health resources needed by this population, we collected and reported on the frequency of specific resources recommended by HEARTSMAP to address (a) psychiatric concerns, (b) social concerns, and (c) youth health concerns. We further stratified the acuity of psychiatric concerns and determined the proportion of presentations requiring (i) emergent in-house psychiatry consultation in the PED, (ii) urgent community crisis response team, and (iii) non-urgent community mental health consultation. To address social concerns, we reported the frequency of mental health-related presentations requiring social work or involvement with the Ministry of Child and Family Development (MCFD), the ministry responsible for all children and youth’s welfare through safe and nurturing homes and connectivity to their community. We determined the frequency of youth health concerns requiring community youth health or addiction and drug resources.
Figure 1.
Schemata of determining domain severity. *A cumulative score of zero indicates no concern. **A single HEARTSMAP section (mapping to the psychiatry domain) score of 3 would also be categorized as severe for the psychiatric domain.
Secondarily, we examined the availability of commonly recommended resources to determine if an unmet need exists in the Vancouver lower mainland. To determine the accessibility of community resources, we liaised with local psychiatrists and established mental health community programs who have expert knowledge on available resources. These included Compass Mental Health (www.CompassBC.ca), a province wide program that provides healthcare providers with telephone advice and/or online and community resources for patients, and Foundry (www.foundrybc.ca), a province wide network providing youth and families with community health and social resources. We categorized these community resources into type (mental health, youth health, or social) and contacted each resource to inquire about anticipated wait times to access their services (<1 week, 1 week to <1 month, 1 month to <3 months, 3 months to <6 months, and >6 months).
Intervention and study procedures
Children and youth presenting to BCCH PED and triaged as having a mental health-related concern, including anxiety, unusual behaviour, concern for patient’s welfare, self-harm, depression/suicidal, homicidal behaviour, insomnia, disruptive behaviour, situational crisis, or violent behaviour, were eligible to be assessed using HEARTSMAP (accessible digitally at openheartsmap.ca). A clinician trained in using HEARTSMAP performed the assessment. Relevant information was documented in 10 free-text boxes pertaining to each section of HEARTSMAP (home, education and activities, alcohol and drugs, relationships and bullying, thoughts and anxiety, safety [suicidality], sexual health, mood, abuse, and professionals). Clinicians rated the severity of each section using a score of 0 to 3. A validated embedded algorithm then mapped these section scores into mental health domains (Social, Youth health, Psychiatry) and recommendations for mental health support resources were triggered for each domain, as appropriate (14). Assessment notes and resource recommendations were printed and became part of the patient’s chart. Despite HEARTSMAP being the expected standard care process at BCCH ED, not all mental health-related presentations are managed using the tool. This may be due to variable clinician practice or patient factors that rendered the tool less ideal to use. Since the initiation of HEARTSMAP, we have been collecting and storing data on the Research Electronic Data Capture (REDCap), a secure web-based application used for data capture for clinical research.
Analyses approach
To explore the generalizability of our study population, we compared the distribution in demographic characteristics for our cohort with the general population presenting with mental health issues to the BCCH ED. Demographic information for all mental health-related presentations to the ED was collected on a biweekly basis during this study period.
We used descriptive statistics (proportions with 95% confidence intervals for frequency measures and means with standard deviations, or median with IQR as appropriate for continuous variables) to report our findings concerning our primary and secondary study objectives.
RESULTS
From October 1, 2016 until June 30, 2019, our ED received 3,327 mental health-related visits, among which 1,530 (46%) had the HEARTSMAP tool applied and recorded into RedCAP. Table 1 describes these populations’ demographic distribution.
Table 1.
Study population (ED mental health-related visits) demographic and visit characteristics stratified by assessment with and without HEARTSMAP
| Age, mean (95% CI), years | HEARTSMAP n=1,530 13.6 (12.3, 14.9) |
All PED mental health-related presentations n=3,327 13.1* |
P-value |
|---|---|---|---|
| Sex, n (%) | |||
| Male | 537 (35.1) | 1,431 (43.0) | |
| Female | 873 (57.1) | 1,896 (57.0) | 0.48 |
| Unknown | 120 (7.8) | ||
| Acuity†, n (%) | |||
| CTAS 1 | 30 (2.0) | 51 (1.5) | 0.28 |
| CTAS 2 | 676 (44.2) | 1,441 (43.3) | |
| CTAS 3 | 803 (52.5) | 1,706 (51.3) | |
| CTAS 4 | 16 (1.0) | 107 (3.2) | |
| CTAS 5 | 1 (0.1) | 6 (0.2) | |
| Undetermined | 4 (0.3) | 16 (0.5) | |
| Day of week, n (%) | |||
| Weekday | 1,226 (80.1) | 2,529 (76.0) | 0.0015 |
| Weekend | 304 (19.9) | 798 (24.0) | |
| Previous visit in the last 30 days, n (%) | 294 (19.2) | 452 (13.6) | <0.00001 |
*P-value for age not attainable as unable to obtain 95% confidence intervals for general population.
†CTAS = Canadian Triage and Acuity Scale.
CTAS Level 1 = resuscitation; Level 2 = emergent; Level 3 = urgent; Level 4 = less urgent; Level 5 = non-urgent.
The average sex distribution and acuity of patients who had HEARTSMAP applied were comparable to the general population of patients who presented with a mental health complaint. Neither HEARTSMAP nor general population statistics collected information on gender or nonbinary identities. There was a higher percentage of patients who had previously presented to the ED within the last 30 days in the HEARTSMAP group. The HEARTSMAP cohort also had a higher proportion of patients presenting on weekdays.
The rest of our analyses only includes data obtained from the HEARTSMAP database (N=1,530 visits). A negligible proportion (1.2%) of mental health-related presentations had no psychiatric features, but 40.1% were assessed to have severe psychiatric concerns. 21.7% had moderate or severe youth health-related concerns, and 26.8% had moderate or severe social concerns.
Triggered recommendations by the HEARTSMAP indicated that in-emergency acute psychiatric consultation was warranted in just over half (50.7%) of the patients. Of the 776 emergent psychiatric recommendations, 410 (or 52%) were triggered due to suicidal ideation on history alone. Table 2 reports in detail the distribution in resource needs as per HEARTSMAP triggered recommendations.
Table 2.
Triggered HEARTSMAP recommendations
| Emergent Psychiatry consultation in ED, n (%) | 776 (50.7) |
|---|---|
| Crisis response team*, n (%) Recommend† |
483 (31.6) |
| Consider‡ | 404 (26.4) |
| Community Child and Youth Mental Health services, n (%) | |
| Recommend | 484 (31.6) |
| Consider | 736 (48.1) |
| Social work/services involvement, n (%) | |
| Recommend | 379 (24.8) |
| Consider | 401 (26.2) |
| Youth Health resources (either sexual or drug related), n (%) | |
| Recommend | 485 (31.7) |
| Consider | 336 (22.0) |
*Crisis Response Team defined as outpatient urgent follow-up within 3 days.
†Recommend defined as advised management.
‡Consider defined as optional management.
Through discussions with psychiatrists, COMPASS, Foundry, MCFD, and online searching, we identified 123 community mental health programs within the Lower Mainland, of which 62 were psychiatric specific resources, 30 were youth health programs, and 31 were social programs. Among the psychiatric resources, 8 were crisis response teams, which provide urgent services to a specific geographic location within the Lower Mainland.
All crisis response teams were able to respond to referrals within a 72-hour timeframe. The 54 community-based programs in the Vancouver Lower Mainland offer psychiatric assessment or support through group programs, counsellors, and/or psychiatrists. The majority (59.3%) of community psychiatric programs reported having wait times greater than 1 month for accessing services. Community social programs address issues including violence and abuse, social work needs, and homelessness. Over one third (38.7%) of these social programs reported they were accessible within a week. Youth health programs in the community provide support with concurrent disorders including drugs, addictions, and sexual health. Of these, 50% of programs reported being able to intake youth within a week. The distribution of wait times to access various mental health programs in the community are reported in Table 3.
Table 3.
Wait times for accessing mental health community resources
| Community Mental Health programs | Wait times | |||||
|---|---|---|---|---|---|---|
| <1 week | 1 week to <1 month | 1 to <3 months | 3 to <6 months | >6 months | Unavailable/unknown | |
| Psychiatric, n (%) | 4 (7.4) | 7 (13.0) | 17 (31.5) | 10 (18.5) | 5 (9.3) | 11 (20.4) |
| Social, n (%) | 12 (38.7) | 1 (3.2) | 4 (12.9) | 4 (12.9) | 3 (9.7) | 7 (22.6) |
| Youth health, n (%) | 15 (50.0) | 3 (10.0) | 2 (6.7) | 2 (6.7) | 2 (6.7) | 6 (20.0) |
Discussion
Our study found that concurrent psychosocial concerns among children and youth with mental health-related presentations were common. A quarter of all patients had moderate or severe social concerns and a fifth had moderate or severe youth health concerns. For patients with psychosocial concerns appropriate for community resources, the largest proportion of social and youth health programs were accessible within 1 week. Conversely, the majority of community psychiatric programs were less accessible, with wait times of longer than one month to access services.
Our findings are consistent with prior reports that psychiatric issues comprise the majority of mental health-related ED presentations (4,21–23), but our study adds that concurrent social and youth health issues may sometimes be the main concern that requires addressing in the PED. Beyond comprehensive psychiatric assessment, many families are challenged by social conflicts which are best addressed by social workers or counsellors. This reinforces a previous finding that family, peer and school conflict comprised the majority of triggers leading to PED mental health-related presentations (9). Similarly, a study in Toronto found that patients commonly had significant Axis IV psychosocial stressors including adjustment to new environment, academic difficulties, parental conflict and/or peer conflict precipitating a PED visit, and suggested that there may be a role for ED-based allied health professionals to address these issues and facilitate community follow-up (24). In institutions where social workers are accessible, one study found that more than half of all emergency mental health-related presentations required social work consultation (25). In the older adolescent population, the parallel challenge becomes substance use and control. It is well known that mental health issues can predispose youth to self-medicate or cope through using substances (26). Conversely, substance use may also unveil or exacerbate psychiatric symptoms (26,27). Newton et al. found that mental health complaints due to substance abuse or misuse comprised close to one third of all mental health-related presentations (3). However, previous studies have found that assessment and appropriate referrals to address youth substance use is lacking in EDs (28,29). Given our finding that concurrent social and youth issues are prevalent and may precipitate PED visits, we propose improved access to allied health professionals in the ED to better address these psychosocial triggers and facilitate improved follow-up in the community.
We identified that the largest gap in mental health care is the lack of easily accessible long-term psychiatry based programs. Similar frustration with inaccessibility of community psychiatric resources has been highlighted by the Canadian Mental Health Association (30) and American College of Emergency Physicians (31). Locally, one report found that while mental health services do exist to provide care to those with severe psychiatric needs, it lacks accessibility to 20% of Canadians with mild or moderate problems (32). Our study found that at least 60% of the psychiatric community mental health resources had wait times between 1 and 6 months. Delayed access to local community psychiatric resources was highlighted in Doan et al.’s study, in which 50% of subjects who attempted to access community resources were waitlisted at 30 days after they had a positive mental health screen in the ED (33). Amongst psychiatric mental health-related presentations to the PED, over half had mild or moderate concerns, suggesting that community psychiatric resources are not meeting the needs of local youth and the PED is a last resort safety net. Similar disparities in community psychiatric resources exist across the USA (34). Conversely, social and youth health community programs had improved accessibility. This is surprising given the high prevalence of concurrent social and youth health issues we found in patients presenting with mental health complaints. Further investigations to determine if this is due to lack of knowledge and decreased use, perceived stigma from families preventing access, or other reasons, are needed.
Limitations in this study include the potential for sample bias. When HEARTSMAP was first introduced, about 50% of eligible patients were assessed using the tool, and over time the rate has risen to 80 to 90%. Although the demographic comparison did not show significant differences, it is unclear if clinicians selected more or less complex patients to utilize HEARTSMAP, which would affect the distribution of resource recommendations. When designing the HEARTSMAP algorithm, sensitivity was prioritized and lower specificity was accepted to ensure it would be safe. It was therefore anticipated that HEARTSMAP would recommend emergent psychiatric consultation at a higher rate than required and more frequently than hospitalization would occur (14). Finally, when contacting our local community resources, we noted a number of programs were restructuring, or had staffing changes, suggesting a rapidly changing landscape of community mental health resources. Particularly in the context of the COVID-19 pandemic, it is unclear how generalizable our findings will be in the post-pandemic context. We explored accessibility before and during the pandemic and found that almost 90% of the programs continued to have similar wait times, with transition to online services.
Children and youth seeking emergency mental health care often have complex psychosocial challenges in addition to psychiatric specific concerns. Our findings support efforts to increase the range of psychosocial resources accessible upon discharge from the ED, along with more widely accessible community psychiatric programs to meet the needs of children and youth with lower acuity psychiatric concerns, sparing families from having to access non emergent care in EDs.
Contributor Information
Alison Lee, Department of Pediatrics, University of British Columbia, Vancouver, British Columbia, Canada.
Jana Davidson, Department of Psychiatry., BC Children’s Hospital Research Institute, University of British Columbia, Vancouver, British Columbia, Canada.
Tyler Black, Department of Psychiatry, University of British Columbia, Vancouver, British Columbia, Canada.
Grace G Kim, Faculty of Medicine, University of British Columbia, Vancouver, British Columbia, Canada.
Quynh Doan, Department of Pediatrics, BC Children’s Hospital Research Institute, University of British Columbia, Vancouver, British Columbia, Canada.
Funding
There are no funders to report.
Potential Conflicts of Interest
JD is past president of Canadian Academy of Child and Adolescent Psychiatry, a Board member of the Canadian Psychiatric Association and Founding Director of the National Institute of Families for Child and Youth Mental Health. There are no other disclosures. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
- 1. Waddell C, Shepherd C, Schwartz C, Barican J.. Child and Youth Mental Disorders: Prevalence and Evidence-Based Interventions. Vancouver: Children’s Health Policy Centre; 2014. [Google Scholar]
- 2. Mapelli E, Black T, Doan Q. Trends in pediatric emergency department utilization for mental health-related visits. J Pediatr 2015;167(4):905–10. [DOI] [PubMed] [Google Scholar]
- 3. Newton AS, Ali S, Johnson DW, et al. . A 4-year review of pediatric mental health emergencies in Alberta. Cjem 2009;11(5):447–54. [DOI] [PubMed] [Google Scholar]
- 4. Larkin GL, Claassen CA, Emond JA, Pelletier AJ, Camargo CA. Trends in U.S. emergency department visits for mental health conditions, 1992 to 2001. Psychiatr Serv 2005;56(6):671–7. [DOI] [PubMed] [Google Scholar]
- 5. Lynch S, Bautista M, Freer C, Kalynych C, Hendry P. Child mental health services in the emergency department: Disparities in access. Pediatr Emerg Care 2015;31(7):473–8. [DOI] [PubMed] [Google Scholar]
- 6. Sills MR, Bland SD. Summary statistics for pediatric psychiatric visits to US emergency departments, 1993-1999. Pediatrics 2002;110(4):e40. [DOI] [PubMed] [Google Scholar]
- 7. Brown JF, Schubert CM. An examination of emergency department pediatric psychiatric services. J Behav Health Serv Res 2010;37(4):412–26. [DOI] [PubMed] [Google Scholar]
- 8. Gill PJ, Saunders N, Gandhi S, et al. . Emergency department as a first contact for mental health problems in children and youth. J Am Acad Child Adolesc Psychiatry 2017;56(6):475–82.e4. [DOI] [PubMed] [Google Scholar]
- 9. Soto EC, Frederickson AM, Trivedi H, et al. . Frequency and correlates of inappropriate pediatric psychiatric emergency room visits. J Clin Psychiatry 2009;70(8):1164–77. [DOI] [PubMed] [Google Scholar]
- 10.American Academy of Pediatrics, Committee on Pediatric Emergency Medicine; American College of Emergency Physicians and Pediatric Emergency Medicine Committee, Dolan MA, Mace SE. Pediatric mental health emergencies in the emergency medical services system. Pediatrics. 2006;118(4):1764–7. doi:10.1542/peds.2006-1925. PMID: 17015573. [DOI] [PubMed] [Google Scholar]
- 11. Zun L. Care of psychiatric patients: The challenge to emergency physicians. West J Emerg Med 2016;17(2):173–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Reder S, Quan L. Emergency mental health care for youth in Washington State: Qualitative research addressing hospital emergency departments’ identification and referral of youth facing mental health issues. Pediatr Emerg Care 2004;20(11):742–8. [DOI] [PubMed] [Google Scholar]
- 13. Chun TH, Mace SE, Katz ER, et al. . Evaluation and management of children and adolescents with acute mental health or behavioral problems. Part I: Common clinical challenges of patients with mental health and/or behavioral emergencies. Pediatrics. 2016;138(3):e20161570. [DOI] [PubMed] [Google Scholar]
- 14. Lee A, Deevska M, Stillwell K, et al. . A psychosocial assessment and management tool for children and youth in crisis. CJEM 2019;21(1):87–96. [DOI] [PubMed] [Google Scholar]
- 15. Virk P, Stenstrom R, Doan Q. Reliability testing of the HEARTSMAP psychosocial assessment tool for multidisciplinary use and in diverse emergency settings. Paediatr Child Health 2018;23(8):503–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Gill C, Arnold B, Nugent S, et al. . Reliability of HEARTSMAP as a tool for evaluating psychosocial assessment documentation practices in emergency departments for pediatric mental health complaints. Acad Emerg Med 2018;25(12):1375–84. [DOI] [PubMed] [Google Scholar]
- 17. Christodulu KV, Lichenstein R, Weist MD, Shafer ME, Simone M. Psychiatric emergencies in children. Pediatr Emerg Care 2002;18(4):268–70. [DOI] [PubMed] [Google Scholar]
- 18. Stefan S. Emergency department treatment of the psychiatric patient: Policy issues and legal requirements.New York: Oxford Press; 2006. [Google Scholar]
- 19. Woo A. Mental health and addiction services lacking in B.C., report says.The Globe and Mail. 2016. [Google Scholar]
- 20. Ishikawa T, Chin B, Meckler G, Hay C, Doan Q. Reducing length of stay and return visits for emergency department pediatric mental health presentations. CJEM 2021;23(1):103–10. [DOI] [PubMed] [Google Scholar]
- 21. Sheridan DC, Spiro DM, Fu R, et al. . Mental health utilization in a pediatric emergency department. Pediatr Emerg Care 2015;31(8):555–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Newton AS, Rathee S, Grewal S, Dow N, Rosychuk RJ. Children’s mental health visits to the emergency department: Factors affecting wait times and length of stay. Emerg Med Int 2014;2014:897904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Case SD, Case BG, Olfson M, Linakis JG, Laska EM. Length of stay of pediatric mental health emergency department visits in the United States. J Am Acad Child Adolesc Psychiatry 2011;50(11):1110–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Lee J, Korczak D. Emergency physician referrals to the pediatric crisis clinic: reasons for referral, diagnosis and disposition. J Can Acad Child Adolesc Psychiatry 2010;19(4):297–302. [PMC free article] [PubMed] [Google Scholar]
- 25. Grupp-Phelan J, Mahajan P, Foltin GL, et al. ; Pediatric Emergency Care Applied Research Network . Referral and resource use patterns for psychiatric-related visits to pediatric emergency departments. Pediatr Emerg Care 2009;25(4):217–20. [DOI] [PubMed] [Google Scholar]
- 26. Skinner W, O’Grady C, Bartha C, Parker C.. Concurrent substance use and mental health disorders. Toronto, Ontario: Centre for Addiction and Mental Health; 2004. [Google Scholar]
- 27. Canadian Institute for Health Information. Hospital stays for harm caused by substance use among youth age 10 to 24, September 2019. Ottawa, ON: CIHI; 2019.
- 28. Woolfenden S, Dossetor D, Williams K. Children and adolescents with acute alcohol intoxication/self-poisoning presenting to the emergency department. Arch Pediatr Adolesc Med 2002;156(4):345–8. [DOI] [PubMed] [Google Scholar]
- 29. Yu AY, Ata N, Dong K, Newton AS. A description of emergency care received by children and youth with mental health presentations for alcohol and other drug use in two Alberta Emergency Departments. J Can Acad Child Adolesc Psychiatry 2010;19(4):290–6. [PMC free article] [PubMed] [Google Scholar]
- 30. Canadian Mental Health Association. Ending the healthcare disparity in Canada. 2018;(September): 24. https://cmha.ca/brochure/mental-health-in-the-balance-ending-the-health-care-disparity-in-canada/. Accessed August 19, 2021.
- 31. Committee ACOEPPEM. ACEP Psychiatric and Substance Abuse Survey 2008. Am Coll Emerg Physicians. 2008;1–3. https://www.acep.org/globalassets/uploads/uploaded-files/acep/advocacy/federal-issues/psychiatricboardingsummary.pdf. Accessed July 3, 2021. [Google Scholar]
- 32. Backer E, Carten R, Emberley J, et al. . Vancouver Mental Health and Addictions Systems Barrier Report 2018/2019. British Columbia, Canada: Canadian Mental Health Association, Vancouver-Fraser Branch; 2019. [Google Scholar]
- 33. Doan Q, Wright B, Atwal A, et al. . Utility of MyHEARTSMAP for psychosocial screening in the emergency department. J Pediatr. 2020;219:54–61.e1. [DOI] [PubMed] [Google Scholar]
- 34. Kim WJ; American Academy of Child and Adolescent Psychiatry Task Force on Workforce Needs . Child and adolescent psychiatry workforce: A critical shortage and national challenge. Acad Psychiatry 2003;27(4):277–82. [DOI] [PubMed] [Google Scholar]