Introduction
Angiofibroma is a benign, locally aggressive, fibrovascular neoplasm with distinctive morphological and clinical features. They virtually always arise from the nasopharynx in the region of the sphenopalatine foramen and pterygopalatine fossa and termed as nasopharyngeal angiofibroma (NA). Though it is the most common benign neoplasm of the nasopharynx, it accounts for only 0.05–0.5% of all head-and-neck neoplasms [1]. Angiofibromas have been sporadically described in extranasopharyngeal sites. The infratemporal fossa is an uncommon location, and only 7 cases have been reported [2]. The clinical characteristics of extranasopharyngeal angiofibroma (ENA) do not conform to that of NA, thus diagnostically challenging. Here, we present a case of ENA involving the infratemporal fossa presenting as a painless swelling of the cheek.
Case Report
A 24-year-old male patient presented to the Oral and Maxillofacial Surgery OPD with a complaint of slow growing, painless, swelling over the left side of his face in the cheek region for the past 3 and a half years. He reported a progressive increase in the swelling. There was no history of fever, dysphagia, or difficulty in breathing. There was no history of trauma; no other skin lesion was present.
On extraoral inspection, a diffuse swelling extending antero-posteriorly from left nasolabial fold till 1 cm anterior to the posterior border of the mandible and supero-inferiorly from the left temporal region till 1 cm above the inferior border of the mandible was seen with the overlying skin appearing normal (Fig. 1). Palpation revealed a firm, non-tender, non-fluctuant, non-mobile swelling with no local rise in temperature, and the skin over the swelling was pinchable. There was no regional lymphadenopathy. Intraorally, swelling was seen in respect to left buccal mucosa with an obliteration of maxillary vestibular fold from 25 to 28 region without any occlusal derangement or restriction in mouth opening.
Contrast-enhanced computed tomography (CECT) imaging of the head and neck region was suggestive of a well-defined, homogenous, enhancing soft tissue lesion in the left infratemporal fossa: superiorly, extending to the temporal fossa, and inferiorly, into the buccal space. The lesion is seen causing anterior bowing of the posterior wall of the maxillary sinus (Holman–Miller sign) with minimal intra-orbital extension through the inferior orbital fissure with no obvious destruction to the bone (Fig. 2). The nasopharynx and oropharynx were normal.
Surgical excision was carried out under general anaesthesia using an intraoral approach. A maxillary vestibular incision was made, and the tumour was exposed (Fig. 3). Blunt dissection was done, and the tumour was freed from all its margins (Fig. 4). While dissecting the tumour from the infratemporal fossa, haemorrhage was encountered from the pterygoid venous plexus which was controlled using appropriate haemostatic measures. A ribbon gauze pack was placed into the defect space and was removed after 3 days (Fig. 5).
On gross examination, the specimen was a well-encapsulated, lobulated, white-tan mass measuring about 7.5 × 4.5 cm (Fig. 6). Histopathological examination showed a biphasic pattern having a fibrous component admixed with a rich vascular proliferation showing no specific pattern which was suggestive of angiofibroma, thus co-relating with the clinical findings and location of the tumour a final diagnosis of ENA of the infratemporal fossa was made (Fig. 7).
The patient recovered uneventfully without immediate or late post-operative complications. No recurrence was noted during the subsequent follow-up visits (Fig. 8).
Fig. 1.

Pre-operative frontal view showing a diffuse swelling over the left side of the face with the overlying skin appearing normal
Fig. 2.

CECT showing well-defined homogenous enhancing soft tissue lesion in the left infratemporal fossa and anterior bowing of the posterior wall of the maxillary antrum (Holman–Miller sign)
Fig. 3.

Intraoperatively, a maxillary vestibular incision was made and the tumour was exposed
Fig. 4.
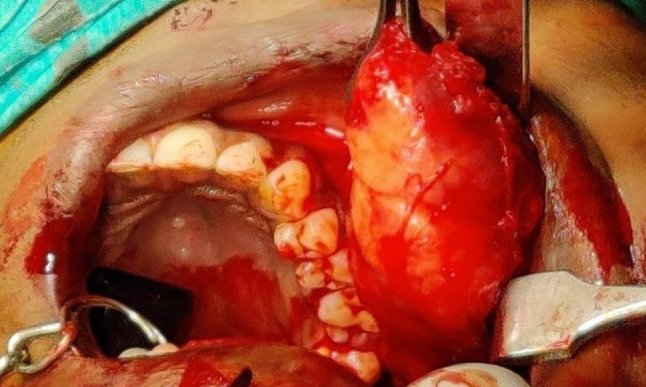
Blunt dissection carried out and tumour mass being excised
Fig. 5.

Closure with ribbon gauze pack in situ
Fig. 6.

On gross examination, the specimen was a well-encapsulated, lobulated, white-tan mass measuring about 7.5 × 4.5 cm
Fig. 7.

Histopathological examination showed a biphasic pattern having a fibrous component admixed with a rich vascular proliferation showing no specific pattern
Fig. 8.

Post-operative frontal view at 9 months
Discussion
Angiofibromas are highly vascular tumours which are locally invasive and have the potential to erode the adjacent bone and involve the contiguous structures. ENAs occur more frequently in females, which accounts for 25–26% of all cases and an older age group with a mean age of presentation of 22 years [3,4].
The clinical presentation of ENA will depend on the site and extent of the tumour and may present with symptoms such as rhinolalia, headache, dysphagia, dyspnoea, stridor, pain, fever, rhinorrhea, swelling of the face, proptosis, progressive nasal obstruction and occasional epistaxis [5]. However, all the previous reported cases of ENA of infratemporal fossa presented with painless facial swelling, except for two cases, where one presented with occasional pain and tenderness and another presented with symptoms of proptosis and headache as radiologically the tumour was seen invading the orbit, sphenoid sinus and middle cranial fossa on the right side [3,6]. Table 1 summarizes the details and clinical features of the reported cases as well as the present case.
Table 1.
Global summary of 8 cases of ENAs presenting in infratemporal fossa and cheek
| No. | Reference | Patient’s age and sex | Site | Clinical features |
|---|---|---|---|---|
| 1 | Irby [7] | 21/M | Right cheek, parapharyngeal space, infratemporal fossa | Premaxillary swelling for the past 1 year |
| 2 | Hora et al. [6] | 21/M | Right cheek, infratemporal fossa, temporal fossa, pterygomaxillary and parapharyngeal space | Swelling of the cheek and pain for the past 7 months |
| 3 | Whitlock [8] | 16/M | Left cheek, infratemporal fossa | Painless, cheek swelling |
| 4 | Isherwood et al. [9] | 13/M | Right pterygomaxillary fissure, infratemporal fossa | Painless facial swelling for the past 3 weeks |
| 5 | Gupta et al. [3] | 13/M | Right ITF, pterygomaxillary fossa. Also invading the right orbit, sphenoid sinus and middle cranial fossa on the right side | Facial swelling for the past 5 months, proptosis for 2 months and headache for 1 month |
| 6 | Szymanska et al. [10] | 23/M | Left infratemporal fossa, cheek and pterygopalatine fossa | Painless, cheek swelling for the past 12 months |
| 7 | Mishra et al. [2] | 16/M | Right sphenopalatine foramina, infratemporal fossa, cheek | Collapsible, painless facial swelling for the past 7 months |
| 8 | Present (2020) | 24/M | Left infratemporal fossa, temporal fossa, cheek with minimal intra-orbital extension through the inferior orbital fissure | Painless, firm, non-fluctuant, cheek swelling for the past 3 and a half years |
Based on the clinical presentation of the current case, the differential diagnoses include neurogenic tumours such as neurofibroma, schwannoma; fibroma; lipoma; fibrovascular tumours such as angiofibroma, capillary haemangioma, haemangiopericytoma; benign salivary gland tumours of the parotid gland such as pleomorphic adenoma; and tumours of muscular origin such as leiomyoma.
CECT and magnetic resonance image (MRI) studies are the primary imaging techniques. Radiologically, ENAs present as a lobulated, non-encapsulated, soft tissue mass which may be associated with opacification of the involved sinuses, anterior bowing of the posterior wall of the maxillary antrum (Holman–Miller sign), displacement of the pterygoid plates and erosion of surrounding bones [11]. Other imaging diagnostic aids include carotid angiography, ultrasonography, colour Doppler and nasal endoscopy.
On gross examination, angiofibroma presents as a smooth, rounded lobulated or multinodular mass with a grey-pink or grey-white cut surface [11]. Histopathological examination reveals varied sizes of thin-walled blood vessels admixed in a dense fibrous stroma with ovoid to spindle-shaped fibroblasts and abundant collagen tissue. Dogan et al. stated that ENAs have interstitial stromal predominance with less vascular elements [12].
Surgery is the gold standard for management of ENA. Endoscopic procedures are less invasive and have been found to cause lesser post-operative morbidity. A multidisciplinary approach may be required for cases with intracranial extension and may include embolization, hormone therapy, radiotherapy, arterial ligation and use of sclerosing agents [1,5].
A recurrence rate of 2.3% has been reported and has mainly been attributed to advanced disease and inexperienced surgeons [5].
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Garça MF, Yuca SA, Yuca K. Juvenile nasopharyngeal angiofibroma. Eur J Gen Med. 2010;7(4):419–425. [Google Scholar]
- 2.Mishra A, Verma V, Mishra SC. Juvenile ‘Perinasal’ angiofibroma. Indian J Otolaryngol Head Neck Surg. 2017;69:67–71. doi: 10.1007/s12070-016-1050-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gupta M, Motwani G, Gupta P. Extranasopharyngeal angiofibroma arising from the infratemporal region. Indian J Otolaryngol Head Neck Surg. 2006;58(3):312–315. doi: 10.1007/BF03050857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Singhal SK, Gupta N, Verma H, et al. Extranasopharyngeal angiofibroma: report of two cases. EJENTAS. 2014;15:73–76. [Google Scholar]
- 5.Windfuhr JP, Vent J. Extranasopharyngeal angiofibroma revisited. Clin Otolaryngol. 2017;00:1–24. doi: 10.1111/coa.12939. [DOI] [PubMed] [Google Scholar]
- 6.Hora JF, Weller WA. Extranasopharyngeal juvenile angiofibroma. Ann Otol. 1961;70:164–170. doi: 10.1177/000348946107000112. [DOI] [PubMed] [Google Scholar]
- 7.Irby WB. Angiofibroma of cheek and infratemporal fossa. J Oral Surg. 1961;19:296–301. [PubMed] [Google Scholar]
- 8.Whitlock RIH. Angiofibroma of the cheek. Br Dental J. 1961;111(10):372–374. [Google Scholar]
- 9.Isherwood I, Dogra TS, Farrington WT. Extranasopharyngeal juvenile angiofibroma. J Laryngol Otol. 1975;89:535–544. doi: 10.1017/S0022215100080725. [DOI] [PubMed] [Google Scholar]
- 10.Szyman´ska A, Szyman´ski M, Skomra D, et al. Extranasopharyngeal angiofibroma of the infratemporal fossa. Otolaryngol Head Neck Surg. 2009;140:433–434. doi: 10.1016/j.otohns.2008.09.025. [DOI] [PubMed] [Google Scholar]
- 11.Barnes L. Surgical pathology of the head and neck. NewYork: Informa Healthcare; 2009. pp. 834–837. [Google Scholar]
- 12.Dogan S, Yazici H, Baygit Y, Metin M, et al. Extranasopharyngeal angiofibroma of the nasal septum: a rare clinical entity. J Craniofac Surg. 2013;24:e390–e393. doi: 10.1097/SCS.0b013e318290344d. [DOI] [PubMed] [Google Scholar]


