Abstract
Aim
To present a chin wing osteotomy in two patients who had undergone a virtual surgical planning workflow for surgical procedures and were followed up for 4 years.
Case reports
Two retrognathic patients with normal occlusion were evaluated by means of dental and facial photographs, cone beam computed tomographs and digitization of dental arches. Virtual surgical planning was performed by using the Dolphin Imaging software to simulate the chin wing osteotomy. Next, three-dimensional models were imported into computer-aided design system (Rhino 6) for designing two hybrid (dental-bone supported) cutting and repositioning guides. Chin wing osteotomies were carried out by using the cutting guides and the osteotomized segments were placed by using L-shaped plates and screws assisted by the repositioning guides. Bone grafts were interposed in the mandibular angle region bilaterally. In both cases, the patients reported aesthetically and functionally favorable outcomes.
Conclusion
Chin wing osteotomy is an appropriate treatment for retrognathic mandible in patients with normal occlusion and no additional discrepancies as the technique provided chin advancement and improvement in facial contour. The post-operative outcomes showed reliable workflow of virtual planning and surgical procedures, which could be adopted as an alternative in similar cases.
Keywords: Chin, Genioplasty, Mandibular osteotomy, Three-dimensional imaging, Orthognathic surgery
Introduction
The chin area is an important key to achieve a harmonious facial profile in patients with dentofacial deformities. With regard to the facial clinical features, the chin area may show morphological abnormalities in the sagittal (i.e. pro or retrognathism), vertical (i.e. deficient or excessive height) and transversal (i.e. asymmetry) planes, either individually or associated with each other [1].
Classical genioplasty techniques have often been associated with Le Fort I and bilateral sagittal split osteotomies in orthognathic surgeries in order to modify the dimension and position at the middle of the lower third face by optimizing facial profile, lip competence and positioning of the lower lip and mentolabial fold [2].
A modified genioplasty technique was shown ten years ago in a case report by Triaca et al. [3], who named it as wing genioplasty considering that the anterior mandibular genioplasty extends the osteotomy posteriorly to the posterior border of the mandible beneath the mandibular canal. As usual, chin wing osteotomy has been used to change the basal morphology of the mandible in patients with mandibular deficiency and/or asymmetries associated with normal dental occlusion, thus improving aesthetic and functional requirements for the lower third face contour [4]. However, current technical notes have recommended that modifications can be done in osteotomy designs according to the clinical indication for skeletal class III patients [5] and to optimize the aesthetic and functional results associated with bilateral sagittal split osteotomy for skeletal class II patients [6].
Regardless of the modifications in the technique, the chin wing osteotomy has to be performed beneath the mandibular canal, which can reduce the possibility of damage to the inferior alveolar nerve. Although oral and maxillofacial surgeons can assess the distances between anatomical structures on a computerized tomography scan, this does not ensure that osteotomy will be safely performed by using either conventional or free-hand (i.e. with no guide) method [7].
Therefore, our purpose was to present case reports of chin wing osteotomy in skeletal class II patients with normal occlusion who had undergone a virtual surgical planning workflow for surgical procedures and followed up for 4 years.
Case Reports
The patients were healthy 32-year-old (Case A) and 31-year-old (Case B) females who presented complaints regarding mandible contour and chin deficiency. Both patients had their heads examined in estimated natural head position [8], so that facial and dental analysis could be performed as described by Arnett and Bergman [9]. It was found that skeletal class II facial profile and mandibular retrognathism was associated with deep mentolabial fold, everted lower lips, shortened lower third face, deficient mandibular angles and normal Angle’s class I occlusion (Figs. 1 and 2). There were also no vertical and transversal discrepancies in dental and gingival display at rest and smiling, and interocclusal relationship, respectively. The patients had already been long treated for orthodontic compensation or camouflage before being evaluated by our oral and maxillofacial surgeon team.
Fig. 1.
a–f: Pre-operative evaluation at rest and smiling in Case A. g–i: Intra-oral images in Case A
Fig. 2.
a–f: Pre-operative evaluation at rest and smiling in Case B. g–i: Intra-oral images in Case B
Virtual Surgical Planning
CBCT scans of both patients were taken by using an i-CAT scanner (Image Sciences International, Hatfield, PA, USA) according to a standardized image acquisition protocol for virtual surgical planning in orthognathic surgery [10]. The patients’ dental arches were scanned with an intra-oral scanner (CS3600 Access, Carestream Dental, Atlanta, USA) according to the manufacturer’s instructions. The DICOM files were segmented into three-dimensional reconstructions by using the Dolphin Imaging software (Dolphin Imaging and Management Solutions, Chatsworth, CA, USA) according to the virtual surgical planning as described by Bobek et al. [11] and Marlière et al. [12]. Next, the digital dental models were superimposed on each image of the dental surface to replace digitally the distorted dentition by using metallic restoration. Two operators (M.S.D. and H.L.M.B.) performed the design of the chin wing osteotomy for each three-dimensional virtual model (Cases A and B) by using a surgical planning tool, which simulated the chin area and the mandibular border movements according to the patient’s aesthetic-functional complaints and facial analysis (Fig. 3). The results of the post-operative virtual relationships are shown in Table 1.
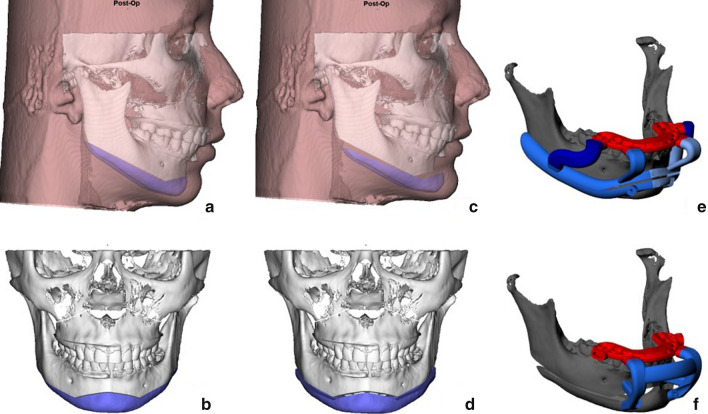
Fig. 3.
a–d: Chin wing osteotomy was designed to simulate movements of the chin and mandibular inferior border on the Dolphin Imaging software. e–f: Cutting and repositioning guides were designed by using Rhino 6 software
Table 1.
Measurements of the movements of virtual surgical planning in millimeters (mm).
| Cephalometric references | Case A | Case B | ||||
|---|---|---|---|---|---|---|
| *A+/P− | *L+/P− | *D+/U− | *A+/P− | *L+/P− | *D+/U− | |
| Pogonion | + 7 mm | 0 | + 1.4mm | + 6.5 mm | 0 | + 1 mm |
| Gonion (L) | + 4.3 mm | 0 | + 6.2mm | + 4 mm | 0 | + 4.53 mm |
| Gonion (R) | + 4.3 mm | 0 | + 6.1mm | + 4 mm | 0 | + 4.07 mm |
*A – Anterior and P – posterior, L – left and R – right, D – down and U – up;
After the surgical planning, the three-dimensional models (Cases A and B) were converted into STL format so that they could be used by a computer-aided design (CAD) system (Rhino 6, Rhinoceros, Barcelona, Spain) for designing the bone-tooth supported cutting and repositioning guides. These guides were essential to generate a customized osteotomy in a virtual set-up, which allowed orienting and transferring the surgical planning to the surgical procedure accurately (Fig. 3). Finally, the guides were manufactured by using a 3D printer (Formlabs Form 2).
Surgical Procedures
The surgical procedures were performed under general anesthesia. Firstly, local infiltration into the mandibular buccal mucosa was performed with lidocaine 2% with epinephrine at a ratio of 1:100.000. Three buccal incisions were made by using an electric scalpel, in which 5 mm of free gingiva was preserved in each side of the mandible, that is, distally from the second molar to the first molar mesially, similarly to a regular genioplasty from lower canine to canine. Subperiosteal dissections were performed on the buccal bone surface of the mandible with no periosteal detachment from the mandibular inferior border, thus exposing the cortical bone to adjust the cutting guide and perform osteotomies (Fig. 4).
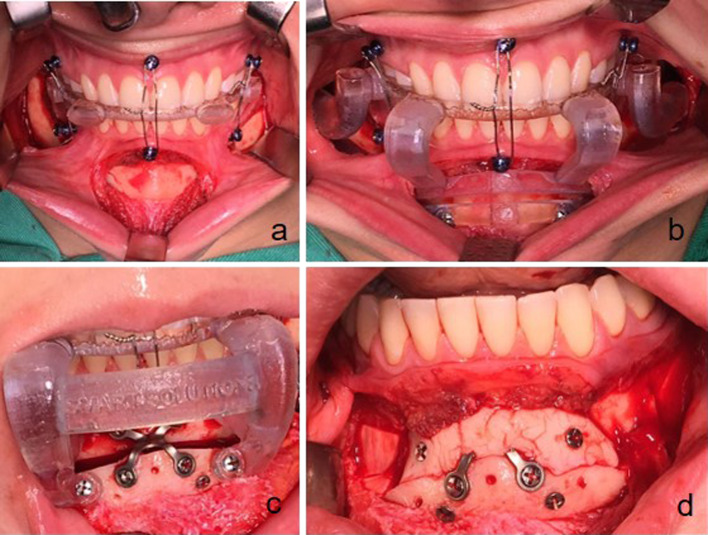
Fig. 4.
a Buccal incision and periosteal detachment. b Cutting guide was fitted by using inter-occlusal splint as reference to be positioned on the buccal mandibular surface. c Internal fixation supported by repositioning guide associated with inter-occlusal splint and fixed with two screws in the chin area. d Alloplastic material was stabilized in the symphyseal area for optimizing labiomental fold
An interocclusal splint was positioned between maxillary and mandibular arches for adjusting the cutting guides, which were fixed with two screws and positioned on the buccal bone of the mandible (Fig. 4). Micro reciprocating saws (Stryker-CORE System) were used at the beginning of the chin wing osteotomy to cut the buccal cortical surface and medullary bones beneath the mandibular canal. The surgical procedure was finished after reaching the lingual bone area by using an ultrasound or piezoelectric device (PIEZOSURGERY® touch; Mectron, Carasco, Italy). After the osteotomies, the repositioning guides were fixed with two screws in the same previous holes in order to stabilize the mandibular basal border for rigid internal fixation with regular stock plates, using one chin mini-plate at the symphyseal area (Fig. 4) and two L-shaped mini-plates at the lateral region of the mandible associated with mono-cortical screws (System 2.0—KLS Martin, Germany).
Due to the chin advancement, the labiomental fold became deeper in Case B as the immediate outcome was an aesthetically poor appearance. To solve this drawback, alloplastic material (i.e. polymethyl methacrylate) was fitted to the symphysis (next to the point B region between the osteotomized bone segments) and fixed with screws for increasing the labiomental angle (Fig. 4), as described by Esteves et al. [13]. As a result of the downward movements for optimizing the mandibular contour, bone gaps were observed between the osteotomized bone segments (i.e. mandibular inferior border and mandibular body), mainly next to the angle of the mandibular region. For achieving a favorable bone healing, the inter-positional bone-grafting technique was performed in both cases by using blocks (10 × 10 × 5 mm) of heterogeneous bone grafts (Bio-graft; Bio-oss, Geistlich, São Paulo, Brazil).
Post-Operative Period
The patients were satisfied with the results both aesthetically and functionally. CBCT scans taken immediately after the surgery, three-dimensional reconstructions show osteotomy designs and fixation methods in both cases (Fig. 5). After 4 years, the outcomes were stable for Cases A and B (Figs. 6 and 7).
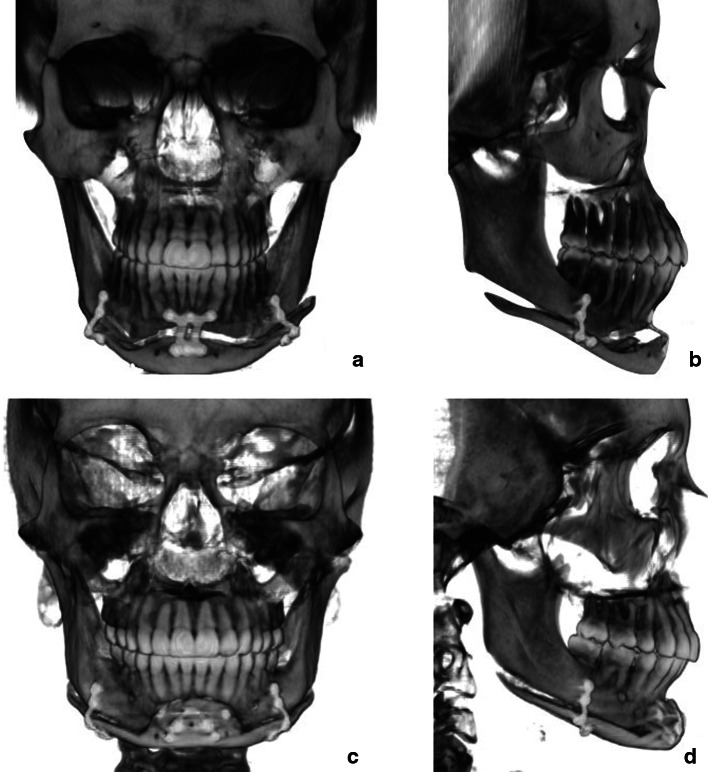
Fig. 5.
Three-dimensional reconstruction immediately after the surgery
Fig. 6.
a–f: Post-operative evaluation at rest and smiling in Case A
Fig. 7.
a–f: Post-operative evaluation at rest and smiling in Case B
Discussion
Ortho-surgical treatment is recommended for correction of dentofacial deformities and often involves bi-maxillary orthognathic surgery, which can be performed by altering the maxillomandibular complex in order to optimize functional (dental occlusion, upper airway, temporomandibular joint and long-term stability) and aesthetic results [14]. Although our case reports did not require a bimaxillary orthognathic surgery (i.e. bilateral sagittal split osteotomy associated with Le Fort I osteotomy) to correct the retrognathic mandibles as usually occur. Other osteotomies can be carried out to improve facial appearance and functional outcomes [1, 15].
In class II patients, orthodontic camouflage can be a treatment option when mandible growth is not sufficient or when patients do not accept ortho-surgical treatment [16]. According to Khechoyan [17], most class II patients follow recommendations from their orthodontists, because patients think that all their complaints could be solved by orthodontic treatments. However, they should be recommended an appointment with an oral and maxillofacial surgeon for proper evaluation. Perhaps, treatments related to class II patients may be underestimated or conditioned by the orthodontist's decision or by the patient's own choice. Even though our case reports have shown normal and stable occlusion after the orthodontic camouflage treatment, aesthetic complaints still persisted among the patients.
From the facial analysis and patients’ complaints, we could observe lack of chin projection and mandible contour although they had no discrepancy in the maxilla position as neither functional (labial incompetence) nor aesthetic complaints regarding the positioning of teeth (i.e. upper labial support, nasolabial fold, tooth display at rest or smiling). Therefore, we could not have considered a counterclockwise rotation of the occlusal plane for planning a bimaxillary orthognathic surgery to obtain the mandibular advancement regardless of class II overjet. Otherwise, if we had planned to provide an antero-posterior projection of the pogonion area in our case reports, the rotation of the maxillomandibular complex would have been based on maintaining the anteroposterior and vertical incisal positions and on downward repositioning the posterior teeth area in the maxilla [18]. However, counterclockwise rotation could not bring aesthetic benefits because there might be retrusion of the nasolabial fullness and labial support (i.e. setback of anterior nasal spine) and inverted smile, resulting in excessive gingival display in the region of the maxillary molars.
Several alloplastic materials have been used to improve the aesthetics of the lower face [19]. In fact, among the advantages of silicone implants, we can cite the lower risk of sensory loss and the possibility of removing them if the outcome is unsatisfactory. On the other hand, there are disadvantages such as asymmetry, poor positioning, haematoma, seroma, infection, mobility, extrusion and bone resorptions [20, 21]. Therefore, if the surgeon wants stability and good outcomes in the immediate and long terms, silicone implant should not be used.
In the cases presented in this study, aesthetic results would not have been favorable if only genioplasty had been performed as the advancements in the chin region would have occurred with no changes in the mandibular angle and mandibular facial contour. In addition, Pouzoulet et al. [1] and Cordier et al. [6] pointed out that genioplasty does really decrease the symphyseal height as the osteotomized segment of the chin advances forward. In addition, this osteotomy can often generate a notch in the lower edge of the jaw behind the chin segment, resulting in an external aesthetic deformity which is visible and accentuates the soft tissue of the jaws. This results in aesthetic changes which can be uncomfortable, providing no gain in the mandibular contour [22].
Chin wing osteotomy can correct the position of the chin by changing the aspect of the lower third of the face and the divergent mandibular plane of inferior border, thus improving lip competence when necessary [1, 3, 5]. The choice of wing osteotomy was based on the fact that it is a technique enabling to change the mandibular plane with lower replacement of the osteotomized region of the gonion, which improves the contour of the mandibular angle. It is possible to move the pogonion forward and the entire mandible, which improves the definition of the mandible, without changing the patients' occlusion.
With regard to the functional results, Tabrizi et al. [23] performed a prospective study in 10 patients who had been diagnosed with obstructive sleep apnoea and underwent chin wing osteotomy. The authors concluded that chin wing osteotomy can be considered as an option for improving the obstructive sleep apnoea in retrognathic patients. Based on their results, we may suppose that the upper airway of our patients might have been optimized at the oropharynx dimension after surgical advancement, which affected the suprahyoid muscles.
For these reported cases, the guides may have overcome our concerns regarding osteotomy design, potential damage to lower alveolar nerve and replacement of osteotomized structures as planned virtually. As for the chin wing osteotomy, Coopman et al. [7] made a technical modification in which a cutting surgical guide was included to support the basilar region at the level of the mandibular angle, thus allowing to perform a standardized cut so that injuries to the lower alveolar nerve can be prevented. Similarly, we developed a virtual surgical planning workflow by using two software to manufacture hybrid (dental-bone supported) cutting and repositioning guides, ensuring safe osteotomy and precise fixation of osteotomized segments. In this sense, a systematic review was performed based on 16 studies demonstrating the benefits of using surgical guides and three-dimensional technology to assist with genioplasty. These studies concluded that the degree of precision of the obtained results can be increased with the use of the CAD/CAM methodology [24].
In addition, we suppose that some steps of the technique should be followed, such as the minimally invasive approach used in these patients instead of a mandibular degloving and partial periosteal detachment at the lower edge of the mandible, thus decreasing oedema and improving the post-operative recovery [25, 26]. We strongly encourage all oral and maxillofacial surgeons to use inter-positional autogenous or heterogeneous bone grafts, mainly when there is a gap between osteotomized segments. This contributes to bone neoformation and avoids bone resorption or pseudo-arthrosis, which can cause notch in the mandible [27, 28]. After wing osteotomy, the main complication is inferior alveolar paresthesia, which can be avoided by using cutting and repositioning guides, scaping from a direct damage to the nerve. To be careful of a large tissue detachment is mandatory to not affect the blood supply of the osteotomized segment [29].
Conclusion
Chin wing osteotomy is a very accessible and safe option for treatment of patients with mandibular retrognathism who have been orthodontically compensated and would benefit aesthetically only from a mandibular re-contouring and increased projection of the pogonion. The post-operative outcomes demonstrated that the virtual surgical planning workflow was reliable and could be adopted by other surgeons for similar cases.
Funding
There was no funding for this study.
Declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Approval
All patients assigned a release form because data (pre- and post-operative photographs, computerized tomographs) from subjects who had been undergone orthognathic surgery were used and they can be analyzed. All procedures were carried out ethical standards applicable in 1964 Helsinki Declaration.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Pouzoulet P, Cheynet F, Guyot L, Foletti JM, Chossegros C, Cresseaux P. Chin wing: technical note. J Stomatol Oral Maxillofac Surg. 2018;119(4):315–318. doi: 10.1016/j.jormas.2017.11.015. [DOI] [PubMed] [Google Scholar]
- 2.Pary A. Application of angular measurements in the correction of the asymmetric chin. J Oral Maxillofac Surg. 2013;71(7):1231–1238. doi: 10.1016/j.joms.2012.12.021. [DOI] [PubMed] [Google Scholar]
- 3.Triaca A, Minoretti R, Saulacic N. Mandibular wing osteotomy for correction of the mandibular plane: a case report. Br J Oral Maxillofac Surg. 2010;48:182–184. doi: 10.1016/j.bjoms.2009.08.011. [DOI] [PubMed] [Google Scholar]
- 4.Lopez PE, Guerrero CA, Mujica EU. Mandibular basal osteotomy: new designs and fixation techniques. J Oral Maxillofac Surg. 2011;69:786–797. doi: 10.1016/j.joms.2010.11.038. [DOI] [PubMed] [Google Scholar]
- 5.Triaca A, Brusco D, Guijarro-Martínez R. Chin wing osteotomy for correction of hyperdivergent skeletal class III deformity: technical modification. Br J Oral Maxillofac Surg. 2015;53(8):775–777. doi: 10.1016/j.bjoms.2015.05.015. [DOI] [PubMed] [Google Scholar]
- 6.Cordier G, Sigaux N, Carlier A, Ibrahim B, Cresseaux P. Mini Wing osteotomy: a variant of Chin Wing osteotomy. J Stomatol Oral Maxillofac Surg. 2020;121(3):282–285. doi: 10.1016/j.jormas.2019.10.010. [DOI] [PubMed] [Google Scholar]
- 7.Coopman R, Aerden T, De Temmernan G, Politis C. Mandibular wing osteotomy: technical modification. Br J Oral Maxillofac Surg. 2017;55:635–636. doi: 10.1016/j.bjoms.2017.04.005. [DOI] [PubMed] [Google Scholar]
- 8.Demétrio MS, Marlière DAA, Barbosa SM, Pereira RA, Silveira HM. Different modalities to record and transfer natural head position to virtual planning in orthognathic surgery: case reposts of asymmetric patients. J Maxillofac Oral Surg. 2020;20:443–454. doi: 10.1007/s12663-020-01376-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Arnett GA, Bergman RT. Facial Keys to orthodontic diagnosis and treatment planning. Part I. Am J Orthod Dentofac Orthop. 1993;103(4):299–312. doi: 10.1016/0889-5406(93)70010-L. [DOI] [PubMed] [Google Scholar]
- 10.Canellas JVS, Barros HLM, Medeiros PJD, Ritto FG. Effects of surgical correction of class III malocclusion on the pharyngeal airway and its influence on sleep apnoea. Int Oral Maxillofac Surg. 2016;45:1508–1512. doi: 10.1016/j.ijom.2016.09.002. [DOI] [PubMed] [Google Scholar]
- 11.Bobek S, Farrell B, Choi C, Farrell B, Weimer K, Tucker M. Virtual surgical planning for orthognathic surgery using digital data transfer and an intraoral fiducial marker: the charlotte method. J Oral Maxillofac Surg. 2015;73(6):1143–1158. doi: 10.1016/j.joms.2014.12.008. [DOI] [PubMed] [Google Scholar]
- 12.Marlière DAA, Demétrio MS, Schmitt AR, Lovisi CB, Asprino L, Chaves Netto HD. Accuracy between virtual surgical planning and actual outcomes in orthognathic surgery by iterative closest point algorithm: a retrospective cohort study. Med Oral Patol Oral Cir Bucal. 2019;24(2):e243–e253. doi: 10.4317/medoral.22724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Esteves LS, Rodrigues DB, Ávila C, Campos PSF, Santos JN. Preenchimentos estéticos na cirurgia ortognática: há indicações? Rev Clín Ortod Dental Press. 2016;15(3):33–59. doi: 10.14436/1676-6849.15.3.033-059.art. [DOI] [Google Scholar]
- 14.Sonego CL, Bobrowski AN, Chagas OL, Torriani MA. Aesthetic and functional implications following rotation of the maxillomandibular complex in orthognathic surgery: a systematic review. Int J Oral Maxillofac Surg. 2014;43(1):40–45. doi: 10.1016/j.ijom.2013.07.738. [DOI] [PubMed] [Google Scholar]
- 15.Mittal G, Garg R, Rathi A, Deb SP. The Art of Genioplasty: an Insight. Int J Oral Health Med Res. 2017;4(3):86–94. [Google Scholar]
- 16.Raposo R, Peleteiro B, Paço M, Pinho T. Orthodontic camouflage versus orthodontic-orthognathic surgical treatment in class II malocclusion: a systematic review and meta-analysis. Int Oral Maxillofac Surg. 2018;47(4):445–455. doi: 10.1016/j.ijom.2017.09.003. [DOI] [PubMed] [Google Scholar]
- 17.Khechoyan DY. Orthognathic surgery: general considerations. Semin Plast Surg. 2013;27(3):133–136. doi: 10.1055/s-0033-1357109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wolford LM, Chemello PD, Hilliard F. Occlusal plane alteration in orthognathic surgery—part I: effects on function and esthetics. Am J Orthod Dentofac Orthoped. 1994;106(3):304–316. doi: 10.1016/S0889-5406(94)70051-6. [DOI] [PubMed] [Google Scholar]
- 19.Yaremchuk M, Chen Y. Enlarging the deficient mandible. Aesthetic Surg J. 2007;27(5):539–550. doi: 10.1016/j.asj.2007.07.002. [DOI] [PubMed] [Google Scholar]
- 20.Cuzalina LA, Hlavacek MR. Complications of Facial Implants. Oral Maxillofac Surg Clin North Am. 2009;21(1):91–104. doi: 10.1016/j.coms.2008.10.009. [DOI] [PubMed] [Google Scholar]
- 21.Scaccia FJ, Allphin AL, Stepnick DW. Complications of Augmentation mentoplasty: a review of 11,095 cases. Am J Cosmet Surg. 1993;10(3):189–195. doi: 10.1177/074880689301000306. [DOI] [Google Scholar]
- 22.Lindquist CC, Obeid G. Complications of genioplasty done alone or in combination with sagittal split-ramus osteotomy. Oral Surg Oral Med Oral Pathol. 1988;66(1):13–16. doi: 10.1016/0030-4220(88)90057-6. [DOI] [PubMed] [Google Scholar]
- 23.Tabrizi R, Pourdanesh F, Soleimanpour M, Shafie E. Evaluation of mandibular wing osteotomy in obstructive sleep apnea cases with retrognathia. J Maxillofac Oral Surg. 2013;14(1):46–50. doi: 10.1007/s12663-013-0588-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Oth O, Durieux V, Orellana MF, Glineur R. Genioplasty with surgical guide using 3D-printing technology: a systematic review. J Clin Exp Dent. 2020;12(1):e85–92. doi: 10.4317/medoral.56145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Brusco D. Re: mandibular wing osteotomy: technical modification. Brit J Oral Maxillofac Surg. 2017;55(8):868. doi: 10.1016/j.bjoms.2017.07.013. [DOI] [PubMed] [Google Scholar]
- 26.AlAsseri N, Swennen G. Minimally invasive orthognathic surgery: a systematic review. Int J Oral Maxillofac Surg. 2018;47(10):1299–1310. doi: 10.1016/j.ijom.2018.04.017. [DOI] [PubMed] [Google Scholar]
- 27.Agbaje JO, Sun Y, Vrielinck L, Schepers S, Lambrichts I, Politis C. Risk factors for the development of lower border defects after bilateral sagittal split osteotomy. J Oral Maxillofac Surg. 2013;71(3):588–596. doi: 10.1016/j.joms.2012.07.003. [DOI] [PubMed] [Google Scholar]
- 28.Alyahya A, Swennen GRJ. Bone grafting in orthognathic surgery: a systematic review. Int J Oral Maxillofac Surg. 2018;48(13):322–331. doi: 10.1016/j.ijom.2018.08.014. [DOI] [PubMed] [Google Scholar]
- 29.Brusco D. Re: Mandibular wing osteotomy: technical modification. Br J Oral Maxillofac Surg. 2017;55(8):868. doi: 10.1016/j.bjoms.2017.07.013. [DOI] [PubMed] [Google Scholar]