Abstract
Purpose
Differences in metformin effect on glycemic control in type 2 Diabetes (T2D) have been associated with diet, obesity, years since T2D diagnosis and genetic factors, such as the Met408Val (rs628031) SLC22A1/OCT1 gene polymorphism. This study aimed to analyze the effect of metformin and diet on glycemic control and its association with the Met408Val polymorphism in patients with T2D from western Mexico.
Patients and Methods
A total of 240 T2D adult patients were enrolled in this cross-sectional study. Anti-hyperglycemic therapy, dietary intake, body composition and glycemic profile were recorded and the determination of genotypes of SLC22A1/OCT1 gene (rs628031) was performed using an allelic discrimination assay.
Results
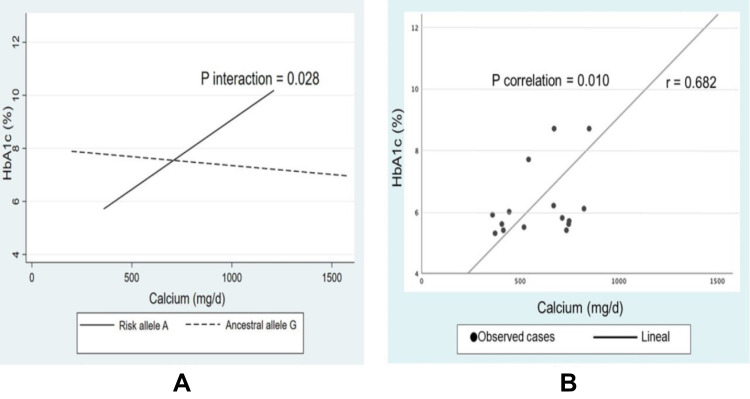
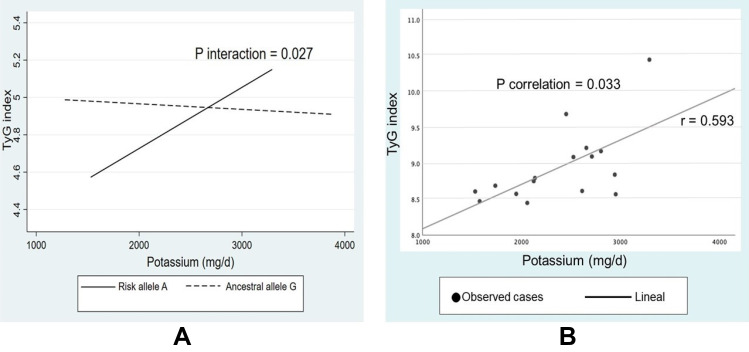
The type of metformin therapy was 47% monotherapy, 45% dual therapy (metformin+glibenclamide or metformin+insulin) and 8% triple therapy (metformin+glibenclamide+insulin). Individuals with metformin monotherapy had a higher glycemic control frequency (%HbA1c <7.0) compared with the dual and triple treatment schemes (77% vs 35% and 15%, respectively; p<0.001). Interestingly, a high potassium intake was documented in the three anti-hyperglycemic therapies and a lower intake of micronutrients, including calcium, magnesium, and zinc. An interaction was found between calcium intake and carriers of the risk allele A (408Val) with %HbA1c (P interaction=0.028), and potassium intake with the TyG index (P interaction=0.027). In addition, there was a positive correlation between calcium intake and %HbA1c (r=0.682; p=0.010), and potassium intake vs TyG index (r=0.593; p=0.033) in risk allele A (408Val) carriers with metformin monotherapy. Genotype frequencies were GG homozygotes (76.6%), GA heterozygotes (21.5%) and AA homozygotes (1.9%). The allele frequency was 87.4% for the ancestral allele G and 12.6% for the risk allele A.
Conclusion
These findings suggest a differing effect of metformin on glycemic control regarding calcium and potassium intake and the Met408Val SLC22A1/OCT1 gene polymorphism in T2D patients.
Keywords: nutrigenetic, pharmacogenetic, SLC22A1/OCT1 gene, gene-nutrient interactions, calcium intake, potassium intake
Introduction
Globally, metformin is favored as first-line anti-hyperglycemic therapy for type 2 diabetes (T2D). It is consumed by more than 150 million people annually due to its affordable price, safety, and considerable pleiotropic effects that have a positive impact on glycemic control, insulin resistance, cardiovascular health, and cancer in T2D patients.1 Its main anti-hyperglycemic effects described as suppression of hepatic glucose production and increased insulin-induced glucose uptake in skeletal muscle without stimulating insulin secretion, make this biguanide a prominent drug for treatment naïve TD2 patients.1
In addition, metformin improves obesity-associated inflammatory effects and reduces body weight, thus, it is widely prescribed in countries with a high prevalence of obesity and T2D, such as the United States and Mexico.2–4 The pharmacodynamics of this biguanide is decisive to achieve the therapeutic goal, including the gastrointestinal side effects involved in non-adherence to treatment.5 In the enterocyte, the OCT1 protein is the transmembrane channel through which metformin is absorbed to reach the circulation, and consequently, the liver. In hepatocytes, OCT1 is the main route of metformin uptake due to its subsequent effect on the phosphorylation of T172 in the alpha subunit of AMP-activated protein kinase (AMPK), promoting the inhibition of the mitochondrial respiratory chain complex 1 and mG3PDH enzymatic activity, which leads to one of its main anti-hyperglycemic effects: a decrease in hepatic gluconeogenesis.5
Lifestyle modifications, such as diet, physical activity, and psychology counseling are essential to achieve glycemic control in patients with T2D. In particular, the nutritional approach is directly related to the success of the pharmacological therapy since nutrient absorption may influence the pharmacokinetics of metformin and its subsequent anti-hyperglycemic effects.6,7 However, the traditional nutritional approach for T2D patients is focused on weight control and macronutrient quantification, such as complex and simple carbohydrates, soluble fiber and saturated fats since international guidelines for these patients provide limited information on the role of most micronutrients on glycemic control. Furthermore, the interaction between micronutrients and metformin therapy on glycemic and metabolic control in patients with T2D has been poorly explored.6
Recent studies have identified more than 30 polymorphisms in the SLC22A1/OCT1 gene with different effects associated with the metformin response in various ethnic groups. The Met408Val polymorphism (rs628031) of the SLC22A1/OCT1 gene has been the most explored with metformin responses and its genetic effect has differed between studied populations.8,9 Another study using a mouse model with a high-fat-diet (HFD) for 24 weeks reported a decrease in OCT1 mRNA expression of up to 79% in the liver, kidney and intestine of HFD-fed mice, and the expression of OCT1 protein was significantly down-regulated in obese mice at week 12, suggesting that the HFD may have effects on SLC22A1/OCT1 expression, including the pharmacodynamic and therapeutic effects described above.7 However, further studies are required to evaluate variability in glycemic responses to metformin in specific populations due to the pronounced differences in dietary habits around the world, particularly in the micronutrient intake.
In this context, providing an education based in precision medicine (considering clinical, biochemical, pharmacological, and genetic information) is becoming the novel therapeutic approach to improve adherence and pharmacological treatment success on glycemic control, according to individual requirements of T2D patients. The aim of this study was to analyze the effect of metformin and diet on glycemic control and its association with the Met408Val SLC22A1/OCT1 polymorphism (rs628031) in patients with T2D from western Mexico.
Materials and Methods
Study Design and Participants
From a cohort of 432 patients with T2D,10 a total of 240 subjects were included in this cross-sectional study. Participants received nutritional consultations and psychological counseling from the nutritional program “DIABETIMSS”. This program aimed to promote and motivate a greater adherence to pharmacological treatment and improve lifestyle to achieve the therapeutic goal involving glycemic control. The inclusion criteria were: (i) T2D diagnosis according to the American Diabetes Association (ADA) criteria:11 fasting glucose level (126 mg/dL) and/or glucose tolerance test >200 mg/dL 2 hours after the glucose load, and (ii) a record of the anti-hyperglycemic treatment. The exclusion criteria were as follows: (i) pregnant or lactating women, (ii) the presence of comorbidities such as cancer, endocrine, gastrointestinal, autoimmune, liver and kidney diseases, (iii) history of substance abuse, and/or (iv) clinically evident complications such as neuropathy or retinopathy. This study was conducted between August and November 2021 at the Specialized Unit in Research, Development and Innovation in Genomic Medicine from the Nayarit Center for Innovation and Technology Transfer of the Autonomous University of Nayarit, Mexico.
This study was reviewed and approved by the Local Health Research and Ethic Committee 1801 (code: R-2021-1801-017), Family Medicine Unit Number 24, Nayarit. Mexican Social Security Institute. We considered the updated version of the Helsinki Declaration-Ethical Principles for Medical Research Involving Human Subject on the “64th WMA General Assembly from, Fortaleza, Brazil, 2013”, in the development of this work.11 All participants were recruited through open invitation and they provided written informed consent for inclusion in this study.
Clinic, Anthropometric Analysis and Nutritional Evaluation
General data, pathological personal history, pharmacological treatment, and the anthropometric variables were collected by a medical team with validated methods and standardized procedures. Anti-hyperglycemic therapy was classified as: (i) metformin monotherapy, (ii) dual therapy: metformin + glibenclamide and metformin + insulin, and (iii) triple therapy: metformin + glibenclamide + insulin. The minimum duration of anti-hyperglycemic therapy was one year and therapeutic efficacy was evaluated with HbA1c values according to the ADA criteria (%HbA1c <7).12
Body composition was determined using an electrical bioimpedance equipment (Tanita SC-331S, body composition analyzer, Tanita Corporation, Japan). Waist circumference (WC) was measured using a stretch-resistant tape.13 The body mass index (BMI kg/m2) results were defined as normal weight (18.5–24.9 kg/m2), overweight (25.0–29.9 kg/m2) and obesity (≥ 30 kg/m2) according to the World Health Organization (WHO) criteria.14
Dietary information was collected using a 24-hour recall. Patients were instructed to illustrate the portion and specify the quantities as precisely as possible using food scale models (Nasco®) based on the Mexican food composition table.15 Energy intake, macronutrient and micronutrient composition were analyzed by trained dietitians using the Nutritionist Pro™ Diet Analysis software (Axxya Systems, Stafford, TX, USA). General recommendations by the Ministry of Health were used to compare the dietary reference values.16
Laboratory Test and SLC22A1/OCT1 Genotyping
After a 12-hour fast, 10 mL of blood sample was taken by venipuncture and immediately centrifuged at 3500 rpm for 15 min to separate serum, then samples were frozen at −80°C and stored until later use. The Cobas 6000 analyzer (Roche Diagnostics International Ltd, Risch-Rotkreuz, Switzerland) was used to quantify biochemical parameters, which include glucose, total cholesterol (TC), triglycerides (TG) and high-density lipoprotein cholesterol (HDL-c) using commercial kits. Glycosylated hemoglobin (%Hb1Ac) was determined using the turbidimetric immunoassay inhibition method. Low-density lipoprotein cholesterol (LDL-c) was calculated with the Friedewald formula, except when TG levels were higher than 400 mg/dL.17 The non-high-density lipoprotein cholesterol (non-HDL-c) was evaluated subtracting TC-HDL-c and the triglyceride-glucose index (TyG index) was estimated with the formula Ln [fasting triglycerides (mg/dL) × fasting glucose (mg/dL)/2] to determine insulin resistance diagnosis.18 Reference values of biochemical tests were according to the ATP III and ADA guidelines.12,19
The modified salting-out method was carried out to extract and purify genomic DNA (gDNA) from whole blood20 and it was quantified using nano spectrophotometry with the Nanodrop One equipment (Thermo ScientificTM, Massachusetts, United States). The genotyping of the Met408Val (rs628031) SLC22A1/OCT1 polymorphism was performed by real-time PCR in a LightCycler® 96 instrument (Roche Diagnostics, Mannheim, Germany) using TaqMan® SNP genotyping assays (catalog number C___8709275_60; ThermoFisher Scientific). The sequence context was CGTGGGCCGCATCTACCCCATGGCC[G/A]TGTCAAATTTGTTGGCGGGGGCAGC.
The accuracy of the genotyping assay was verified using positive controls of DNA samples corresponding to the three possible genotypes (GG, GA & AA) and negative controls in each 96-well plate assay. Twenty percent of the samples were tested in duplicate as a quality control measure and 100% reproducibility was obtained. The Hardy-Weinberg equilibrium (HWE) and analysis of molecular variance (AMOVA) were estimated using Arlequin software (version 3.0).
Statistical Analysis
The sample size was calculated using the formula for a simple correlation where the population genetic data was obtained from the 1000 Genomes Project (America= 0.22). For a 95% confidence level and 80% power, a minimum sample size of 160 participants was required. The data was analyzed using the statistical program Stata 12 (StataCorp LLC, College Station, TX, USA; www.stata.com) and SPSS Statistics software version 25.0 for Windows (IBM Corp, Inc., Chicago, IL, United States). First, the Kolmogorov–Smirnov test was used to evaluate the normality of the data and the Levene’s test to verify the homogeneity of the study variables. Descriptive statistics were used to describe the main characteristics of participants. Data with normal distribution were analyzed through parametric statistical tests (Student’s t-test and one-way ANOVA with their respective post hoc tests) and non-normal data with non-parametric statistical tests (Kruskal–Wallis and Mann–Whitney U). The chi-square test was used when variables were categorical. The interactions between SLC22A1/OCT1 gene and diet nutrients were obtained through multiple linear regression tests adjusted by age, sex, BMI, years with T2D, type of anti-hyperglycemic therapy and energy intake as covariates and %Hb1Ac levels and TyG index as dependent variables. The tests with significant p-values were corrected using the Bonferroni post hoc method. The partial correlation coefficients were performed to assess the relation between nutrient intake with %HbA1c levels and TyG index analyzed by metformin and dual therapy groups considering the carrier allele. A p-value <0.05 was considered statistically significant.
Results
Clinical Characteristics of T2D Patients According to Anti-Hyperglycemic Therapy
The clinical, anthropometric and biochemical characteristics of patients with T2D by anti-hyperglycemic therapy are shown in Table 1. Overall, the total sample had excessive adiposity due to a BMI >30 kg/m2, body fat percentage >30% and waist circumference >100 cm. The time of T2D evolution was different according to the anti-hyperglycemic therapy. Subjects taking metformin as monotherapy had a significantly shorter time with T2D than those taking dual or triple anti-hyperglycemic therapy (4.5±5.4 vs 10.6±9.5 and 12.8±10.4, p<0.001). As expected, this same difference was observed at the time of anti-hyperglycemic therapy consumption (4.3±5.2 vs 9.3±8.0 and 12.4±10.2, p<0.001) (Table 1).
Table 1.
Clinical Features and Biochemical Profile of Patients with T2D According to Anti-Hyperglycemic Therapy
| n=240 | Reference Values | Metformin (Monotherapy) | Dual Therapy (Met+Glib & Met+Ins) | Triple Therapy (Met+Glib+Ins) | p-value |
|---|---|---|---|---|---|
| n (%) | 112 (47) | 108 (45) | 20 (8) | ||
| Age (years) | - | 57.0 ± 12.0 | 58.5 ± 10.0 | 54.8 ± 9.6 | 0.314 |
| Years with T2D | - | 4.5 ± 5.4 | 10.6 ± 9.5 | 12.8 ± 10.4 | 5x10-7a |
| Sex F/M | - | 71/41 | 66/42 | 14/6 | 0.835 |
| Therapy time (years) | - | 4.3 ± 5.2 | 9.3 ± 8.0 | 12.4 ± 10.2 | 1x10-8a |
| Anthropometric profile | |||||
| BMI (kg/m2) | 18.5–24.9 | 30.5 ± 6.3 | 30.4 ± 6.9 | 29.8 ± 6.2 | 0.638 |
| Normal weight n(%) | - | 15 (13.4) | 17 (15.7) | 3 (15.0) | 0.526 |
| Overweight n(%) | - | 34 (30.4) | 33 (30.5) | 8 (40.0) | |
| Obesity n(%) | - | 43 (38.4) | 36 (33.3) | 7 (35.0) | |
| Total body fat (%) | M:12–20 F:20–30 | 34.8 ± 8.6 | 33.6 ± 8.5 | 32.8 ± 8.0 | 0.449 |
| WC (cm) | M:<90 F:<80 | 101.5 ± 14.6 | 101.3 ± 12.9 | 99.0 ± 12.6 | 0.720 |
| Glycemic profile | |||||
| Glucose (mg/dL) | <110 | 126 ± 40.0 | 166 ± 69.3 | 161 ± 57.5 | 2x10-4b |
| HbA1c (%) | <6.5 | 6.6 ± 1.5 | 8.2 ± 2.2 | 8.6 ± 1.6 | 7x10-7a |
| TyG index (ratio) | <8.31 | 9.0 ± 0.5 | 9.4 ± 0.7 | 9.5 ± 0.7 | 0.001a |
| I.R (TyG ratio) | - | 103 (92.0) | 106 (98.1) | 18 (90.0) | 0.049b |
| Glyc Ctrl (HbA1c%) | <7.0 | 86 (76.8) | 38 (35.2) | 3 (15) | 6x10-8a |
| Lipid profile | |||||
| TC (mg/dL) | <200 | 174 ± 31.0 | 179 ± 31.2 | 184 ± 27.4 | 0.671 |
| TG (mg/dL) | <150 | 142 ± 56.5 | 167 ± 80.7 | 192 ± 100.7 | 0.152b |
| HDL-c (mg/dL) | >50 | 46.9 ± 10.9 | 45.4 ± 10.6 | 45.9 ± 9.4 | 0.569 |
| Non-HDL-c (mg/dL) | <130 | 127.8 ± 28.5 | 133.4 ± 30.4 | 138.0 ± 27.6 | 0.458 |
| LDL-c (mg/dL) | <100 | 100.3 ± 25.1 | 100.4 ± 26.3 | 100.7 ± 25.0 | 0.989 |
Notes: Values are presented as mean ± standard deviations, frequencies, and percentages. aBy post hoc tests: Metformin monotherapy vs dual therapy and triple therapy, p<0.001. bBy post hoc tests: Metformin monotherapy vs dual therapy: Glucose, p<0.001; Insulin Resistance (TyG index), p=0.029; Triglycerides, p=0.025. The one-way ANOVA for quantitative variables and Chi-square test for qualitative variables were the statistical approach. The variables of age and years with T2D were used to fit the analysis.
Abbreviations: T2D, Type 2 Diabetes; Met, Metformin; Glib, Glibenclamide; Ins, Insulin; F, Female; M, Male; BMI, Body Mass Index; WC, Waist Circumference; HbA1c, Glycated haemoglobin; TyG index, Triglyceride-Glucose index; I.R, Insulin Resistance; Glyc Ctrl, Glycemic control; TC, Total-cholesterol; TG, Triglycerides; HDL-c, High-density lipoprotein cholesterol; Non-HDL-c, Non-high-density lipoprotein cholesterol; LDL-c, Low-density lipoprotein cholesterol.
With respect to the glycemic profile, T2D patients showed an average of blood concentrations above the reference values, but these parameters were different according to the type of anti-hyperglycemic treatment. Glucose, %HbA1c and TyG index were lower in the metformin monotherapy group than the other anti-hyperglycemic therapy groups, particularly those with dual therapy (p<0.01) (Table 1). Moreover, the individuals with metformin as monotherapy had a higher frequency of glycemic control (%HbA1c <7.0) compared with the dual and triple treatment schemes (77% vs 35% and 15%, respectively; p<0.001). On the other hand, those patients receiving dual therapy (metformin+glibenclamide/metformin+insulin) presented the highest frequency of insulin resistance according to the TyG index, compared to those patients receiving metformin monotherapy (98% vs 92%, p=0.049) (Table 1). No statistically significant differences in age, sex, anthropometric profile, and lipid profile between type of anti-hyperglycemic therapy were found.
Nutrient Intakes According to Anti-Hyperglycemic Therapy
The macronutrient and micronutrient intake by anti-hyperglycemic therapy are shown in Table 2. Regardless of the type of pharmacological treatment, total consumptions of sugar, protein, fat, saturated fatty acids (SFA), and dietary cholesterol for all patients were above the recommendations for a healthy and balanced diet. Also, lower intakes of polyunsaturated fatty acids (PUFA), dietary fiber, and micronutrients as well calcium, magnesium, zinc, and vitamin D were observed in all study groups. Interestingly, a high intake of potassium was documented in the three anti-hyperglycemic therapy groups. There were no direct associations between anti-hyperglycemic therapy (Table 2.)
Table 2.
Nutrient Intakes of T2D Patients According to Anti-Hyperglycemic Therapy
| n=199 | Reference Values | Metformin (Monotherapy) | Dual Therapy (Met+Glib & Met+Ins) | Triple Therapy (Met+Glib+Ins) | p-value |
|---|---|---|---|---|---|
| n= (%) | 90 (45) | 91 (46) | 18 (9) | ||
| Macronutrients | |||||
| Total energy (Kcal/d) | - | 1,575.3 ± 403.3 | 1,583.9 ± 452.5 | 1,659.7 ± 393.8 | 0.858 |
| Total CHO (%E/d) | 50–60 | 51.0 ± 9.6 | 49.1 ± 9.9 | 50.3 ± 9.2 | 0.448 |
| Sugar Total (g/d) | <25 | 59.7 ± 31.1 | 51.1 ± 28.9 | 60.6 ± 29.2 | 0.108 |
| Total protein (%E/d) | 15 | 17.7 ± 3.4 | 17.5 ± 2.9 | 17.4 ± 2.6 | 0.988 |
| Total fat (%E/d) | <30 | 30.8 ± 6.1 | 31.3 ± 6.4 | 31.0 ± 6.2 | 0.911 |
| SFA (%E/d) | <7 | 8.3 ± 2.4 | 8.5 ± 2.5 | 9.1 ± 2.6 | 0.706 |
| MUFA (%E/d) | 10–15 | 10.3 ± 2.8 | 10.0 ± 2.8 | 10.1 ± 2.5 | 0.519 |
| PUFA (%E/d) | >10 | 7.5 ± 2.5 | 7.7 ± 2.4 | 7.4 ± 2.5 | 0.872 |
| Dietary Chol (mg/d) | <200 | 245.8 ± 133.5 | 280.3 ± 174.2 | 268.5 ± 138.4 | 0.341 |
| Dietary Fiber (g/d) | >30 | 20.7 ± 7.1 | 19.7 ± 7.0 | 21.8 ± 6.0 | 0.564 |
| Micronutrients | |||||
| Sodium (g/d) | 2 | 1.4 ± 0.47 | 1.5 ± 0.63 | 1.5 ± 0.48 | 0.148 |
| Calcium (mg/d) | 800 | 604.2 ± 236.3 | 618.0 ± 260.0 | 676.1 ± 251.2 | 0.545 |
| Potassium (mg/d) | 1800 | 2,491.6 ± 719.9 | 2,508.9 ± 733.8 | 2,585.4 ± 914.1 | 0.982 |
| Magnesium (mg/d) | 350 | 291.6 ± 86.7 | 291.7 ± 83.0 | 312.8 ± 94.6 | 0.718 |
| Zinc (mg/d) | 15 | 8.5 ± 2.8 | 8.7 ± 4.4 | 9.0 ± 2.6 | 0.927 |
| Vitamin D (IU) | 400 | 136.9 ± 90.6 | 140.7 ± 92.0 | 168.3 ± 94.1 | 0.364 |
Notes: Values are presented as mean ± Standard deviations. The one-way ANOVA was the statistical approach. The variables of age and years with T2D were used to fit the analysis.
Abbreviations: Met, Metformin; Glib, Glibenclamide; Ins, Insulin; CHO, Carbohydrates; SFA, Saturated fatty acids; MUFA, Monounsaturated fatty acids; PUFA, Polyunsaturated fatty acids; chol, cholesterol; Kcal, kilocalories; d, day; mg, milligrams; g, grams.
Genotype and Allele Frequencies of Met408Val (rs628031) SLC22A1/OCT1 Polymorphism
The distribution of the Met408Val (rs628031) polymorphism in the SLC22A1/OCT1 gene is shown in Table 3. Genotype frequencies were GG homozygotes (76.6%), GA heterozygotes (21.5%) and AA homozygotes (1.9%). The allele frequency was 87.4% for the ancestral allele G and 12.6% for the risk allele A. This polymorphism was in Hardy Weinberg equilibrium (HWE), p=0.750. Also, the analysis of molecular variance (AMOVA) revealed a genetically homogeneous sample (p=0.439). The frequency distribution analysis based on glycemic control (%HbA1c <7) showed a slightly higher frequency trend of the AA risk genotype in T2D patients without glycemic control compared to those with glycemic control (4.5% vs 0.0%, p=0.204). Genotype frequencies of GG and GA were similar in both group analyses (Table 3).
Table 3.
SLC22A1/OCT1 (rs628031) Genotype and Allele Distribution Among Patients with T2D According of the Glycemic and Type of Anti-Hyperglycemic Therapy
| Genotypes | Alleles | |||||||
|---|---|---|---|---|---|---|---|---|
| n | GG | GA | AA | p-value | G | A | p-value | |
| n (%) | 107 | 82 (76.6) | 23 (21.5) | 2 (1.9) | 93.5 (87.4) | 13.5 (12.6) | ||
| Glycemic control | ||||||||
| Glycemic control (HbA1c<7%) | 63 | 48 (76.2) | 15 (23.8) | 0 (0.0) | 0.204 | 55 (88) | 8 (12) | 1.000 |
| No glycemic control (HbA1c ≥7%) | 44 | 34 (77.3) | 8 (18.2) | 2 (4.5) | 38 (86) | 6 (14) | ||
| Type of anti-hyperglycemic therapy | ||||||||
| Monotherapy (Metformin) | 83 | 63 (75.9) | 19 (22.9) | 1 (1.2) | 0.142 | 72 (87) | 11 (13) | 0.208 |
| Dual therapy (Met+Glib/Met+Ins) | 23 | 19 (82.6) | 3 (13.0) | 1 (4.4) | 20 (89) | 3 (11) | ||
| Triple Therapy (Met+Glib+Ins) | 1 | 0 (0) | 1 (100) | 0 (0) | 1 (100) | 0 (0) | ||
Notes: Values are presented as frequencies and percentages. The Chi-square Test was the statistical approach.
Abbreviations: G, Guanine; A, Adenine; Met, Metformin; Glib, Glibenclamide; Ins, Insulin; HbA1c, Glycated hemoglobin.
Regarding the type of anti-hyperglycemic therapy, a higher frequency of genotype GA heterozygote was observed in those patients receiving metformin monotherapy compared to the dual therapy group; however, this difference was not statistically significant (22.9% vs 13.0%, p=0.142). The frequency of the risk AA genotype was 1.2% for the metformin monotherapy group, 4.4% for the dual therapy group and 0.0% for the triple therapy group (Table 3). The frequencies for ancestral allele G and for risk allele A were similar regardless of glycemic control (p=1.000) and type of anti-hyperglycemic therapy (p=0.208).
Clinical and Biochemical Features by Alleles of the Met408Val (rs628031) SLC22A1/OCT1 Polymorphism in T2D Patients with Metformin Monotherapy
Regarding clinical variables of interest by alleles, no differences in age and sex were observed between study groups. In carriers of the risk allele A, the mean duration of T2D was 2.5±2.7 years and 2.2±2.1 years for anti-hyperglycemic therapy, and they were significantly lower than for carriers of the G allele who had a mean T2D duration of 5.3±6.4 years (p=0.047) and 5.0±5.9 years for anti-hyperglycemic therapy (p=0.038) (Table 4). The average BMI in carriers of the risk allele A was 32.1±8.3 kg/m2 and 29.4±4.9 kg/m2 in G allele carriers with no significant differences (p=0.426). The frequency of patients with normal weight was lower (16% allele G vs 10% allele A), while overweight and obesity showed higher frequencies in both groups, however, these differences were not significant (p=0.215) (Table 4).
Table 4.
Clinical Features and Biochemical Profile of T2D Patients According to Alleles of Met408Val (rs628031) SLC22A1/OCT1 Polymorphism in Monotherapy with Metformin
| n= 83 | Reference Values | Allele G | Allele A | p-value |
|---|---|---|---|---|
| n (%) | – | 63 (76) | 20 (24) | |
| Age (years) | – | 58.6 ± 11.8 | 55.0 ± 11.8 | 0.170 |
| Sex, F/M | – | 39/24 | 14/6 | 0.600 |
| Years with T2D | – | 5.3 ± 6.4 | 2.5 ± 2.7 | 0.047a |
| Therapy time (years) | – | 5.0 ± 5.9 | 2.2 ± 2.1 | 0.038a |
| Anthropometric | ||||
| BMI (Kg/m2) | 18.5–24.9 | 29.4 ± 4.9 | 32.1 ± 8.3 | 0.426 |
| Normal weight n (%) | – | 10 (16) | 2 (10) | |
| Overweight n (%) | – | 15 (24) | 10 (50) | 0.215 |
| Obesity n (%) | – | 22 (35) | 8 (40) | |
| Total body fat (%) | M: 12–20 F: 20–30 | 34.3 ± 7.9 | 36.1 ± 8.5 | 0.476 |
| WC (cm) | M:<90 F:<80 | 99.3 ± 11.9 | 106.2 ± 20.0 | 0.567 |
| Glycemic profile | ||||
| Glucose (mg/dL) | < 110 | 127 ± 43.2 | 124 ± 43.7 | 0.454 |
| HbA1c (%) | < 6.5 | 6.6 ± 1.3 | 6.7 ± 1.9 | 0.496 |
| Glyc Ctrl (%HbA1c) | <7.0 | 51 (81) | 15 (75) | 1.000 |
| TyG index (ratio) | < 8.31 | 9.0 ± 0.5 | 8.9 ± 0.5 | 0.532 |
| I.R. (TyG index) | - | 58 (92.1) | 19 (95.0) | 0.568 |
| Lipid Profile | ||||
| TC (mg/dL) | < 200 | 176 ± 30.8 | 174 ± 31.9 | 0.717 |
| TG (mg/dL) | < 150 | 143 ± 63.3 | 132 ± 40.3 | 0.862 |
| HDL-c (mg/dL) | >50 | 49 ± 11.1 | 46 ± 9.9 | 0.696 |
| Non-HDL-c (mg/dL) | <130 | 127 ± 29.6 | 128 ± 28.7 | 0.949 |
| LDL-c (mg/dL) | <100 | 100 ± 26.8 | 102 ± 23.0 | 0.746 |
Notes: Values are presented as mean ± standard deviations, frequencies, and percentages. aThe t-student test was the statistical approach, p<0.05.
Abbreviations: T2D, Type 2 Diabetes; F, Female; M, Male; BMI, Body Mass Index; WC, Waist Circumference; HbA1c, Glycated hemoglobin; TyG index, Triglyceride-Glucose index; I.R, Insulin Resistance; Glyc Ctrl, Glycemic control; TC, Total-cholesterol; TG, Triglycerides; HDL-c, High-density lipoprotein cholesterol; Non-HDL-c, Non-high-density lipoprotein cholesterol; LDL-c, Low-density lipoprotein cholesterol; mg, milligrams; dL, deciliters.
For glycemic control, no significant differences were observed by alleles with mean glucose levels below 130 mg/dL in both study groups. The average %HbA1c reflects that both groups are in glycemic control (<7%), with more than 70% of the subjects achieving this goal, however, the mean TyG index is above the recommended score and more than 90% of the subjects have insulin resistance by this index (Table 4). Serum lipid levels, total cholesterol, triglycerides, and non-HDL-c were within the recommended levels for both groups, but HDL-c was below the suggested range, while LDL-c was close to the recommended value, and no significant differences were found for each of these variables (Table 4).
Nutrient Intake Regarding Alleles of the Met408Val (rs628031) SLC22A1/OCT1 Polymorphism
Nutrient intakes did not show significant differences by group in most of the macronutrient and micronutrient recorded data with an average caloric intake of less than 2000 kilocalories per day. However, it should be highlighted that the total intake of sugar, protein, fat, SFA, and MUFA in both groups was above the recommended values as well as dietary cholesterol and potassium, whereas for PUFA, dietary fiber, magnesium, zinc and calcium, the intake was lower than the recommended intake for both groups. In addition, vitamin D intake in both groups was below the recommended dose and significantly higher in carriers of the risk allele A compared to G allele carriers (p=0.004) (Table 5).
Table 5.
Nutrient Intake of T2D Patients According to Alleles of the SLC22A1/OCT1 (rs628031) Polymorphism in Monotherapy with Metformin
| n= 83 | Reference Values | Allele G | Allele A | p-value |
|---|---|---|---|---|
| n (%) | - | 63 (76) | 20 (24) | |
| Macronutrients | ||||
| Total energy (kcal/d) | - | 1,603.0 ± 418.2 | 1,585.0 ± 368.5 | 1.000 |
| Total CHO (%E/d) | 50–60 | 49.5 ± 10.2 | 51.1 ± 8.8 | 0.531 |
| Sugar total (g/d) | <25 | 55.5 ± 22.3 | 68.6 ± 46.2 | 0.133 |
| Total protein (%E/d) | 15 | 17.6 ± 3.8 | 18.2 ± 3.0 | 0.551 |
| Total fat (%E/d) | <30 | 31.6 ± 6.2 | 30.6 ± 5.9 | 0.345 |
| SFA (%E/d) | <7 | 8.4 ± 2.6 | 8.2 ± 1.8 | 0.701 |
| MUFA (%E/d) | 10–15 | 10.6 ± 2.7 | 9.9 ± 2.3 | 0.330 |
| PUFA (%E/d) | 10 | 7.6 ± 2.3 | 8.3 ± 3.2 | 0.851 |
| Dietary Chol (mg/d) | <200 | 258.4 ± 132.7 | 257.8 ± 138.7 | 0.946 |
| Dietary Fiber (g/d) | >30 | 20.0 ± 7.1 | 21.1 ± 6.1 | 0.369 |
| Micronutrients | ||||
| Sodium (g/d) | 2 | 1.4 ± 0.48 | 1.5 ± 0.38 | 0.300 |
| Calcium (mg/d) | 800 | 608.4 ± 252.7 | 659.2 ± 219.2 | 0.330 |
| Potassium (mg/d) | 1800 | 2,414.3 ± 589.0 | 2,425.1 ± 512.5 | 0.667 |
| Magnesium (mg/d) | 350 | 290.6 ± 92.4 | 296.5 ± 59.8 | 0.635 |
| Zinc (mg/d) | 15 | 8.6 ± 2.9 | 8.3 ± 1.6 | 0.780 |
| Vitamin D (IU) | 400 | 127 ± 72.6 | 192 ± 92.6 | 0.004a |
Notes: Values are presented as mean ± Standard deviations. aThe T-student Test was the statistical method approach. p<0.05.
Abbreviations: %E/d, Percentage of Energy /day; CHO, Carbohydrates; SFA, Saturated fatty acids; MUFA, Monounsaturated fatty acids; PUFA, Polyunsaturated fatty acids; chol, cholesterol; Kcal, kilocalories; d, day; mg, milligrams; g, grams.
SLC22A1/OCT1 Allele-Diet Interaction and Correlation on Glycemic Phenotypes
Statistical analyses showed relevant gene-diet interactions associated with glycemic outcomes. First, risk allele A carriers with a high calcium intake showed increased %HbA1c levels, which was not observed in non-risk allele G carriers (P int.=0.028) (Figure 1A). In this context, only in the group receiving metformin monotherapy and carriers of the risk allele A, we found a positive correlation between calcium intake and %Hb1Ac levels (r=0.682, p=0.010), controlled by age, sex, and energy intake (Figure 1B). Secondly, elevated TyG index levels were found after high potassium intake only in carriers of the risk allele A (P int.=0.027) (Figure 2A), and a positive correlation between potassium intake and TyG index, only in the group receiving metformin monotherapy and carriers of the risk allele A (r=0.593, p=0.033), controlled by age, sex and energy intake (Figure 2B). Additionally, we performed the same correlations of calcium intake vs %Hb1Ac levels (p=0.948) and potassium intake vs TyG index (p=0.159) within all groups, but without statistical significance. Then, we performed the analysis considering drug treatment (monotherapy vs dual or more drugs), but results did not reach statistical significance (p>0.05). Lastly, the only positive correlation was for patients under monotherapy with metformin and carriers of the risk allele A (Figures 1B and 2B).
Figure 1.
Interaction and correlation between dietary calcium and OCT1 polymorphism regarding HbA1c. (A) Interaction between dietary calcium and OCT1 polymorphism regarding HbA1c values. (B) Correlation between dietary calcium and HbA1c values within risk allele A carriers + metformin monotherapy adjusted by age, sex and energy intake.
Figure 2.
Interaction and correlation between dietary potassium and OCT1 polymorphism regarding the TyG index. (A) Interaction between dietary Potassium and OCT1 polymorphism regarding the TyG index values. (B) Correlation between dietary potassium and TyG index values within risk allele A carriers + metformin monotherapy, adjusted by age, s ex and energy intake.
Discussion
Glycemic control is one of the main goals in primary care for T2D patients. Lifestyle along with physical activity, an adjusted diet to nutritional needs, and the anti-hyperglycemic therapy integrated to the right behavioral health of the individual, are the basis for achieving glycemic control in institutional programs such as DIABETIMSS.21,22
In this study, the group of patients who had metformin monotherapy had significantly fewer years with T2D, and consequently, less time with pharmacological therapy than patients with dual or triple therapy. This can be explained by the therapeutic approach according to the international treatment guidelines in which metformin is proposed as a pharmacological therapy of initiation and insulin secretagogues are added when euglycemia is not achieved.23,24 In the natural course of the disease, gradual loss of pancreatic beta-cell function with decreased secretion of insulin have been demonstrated as the pathology progresses in many of the patients, which impact glycemic control.25,26 The best glycemic profile in the group of patients with metformin monotherapy showed a shorter duration with T2D, which is consistent with the Prospective Diabetes Study (UKPDS).25 An important aspect of all patients in this study is the initiation of the diet and pharmacological therapy, which begin technically once the diagnosis is established and as a result, differences in glycemic control and triglycerides were observed, as well a high percentage of patients who achieved the goal of HbA1c <7% and better TyG index in the metformin monotherapy group.
The nutritional analyses in study subjects reflect what previous urban diet studies of western Mexico have published: a high intake of refined sugars accompanied by low fiber intake, an unhealthy composition of dietary fats, as well as micronutrients such as calcium, magnesium, zinc and potassium.10,27,28 In the three anti-hyperglycemic therapy groups, the nutritional composition resembles the “westernized diet”, which is usually deleterious for carbohydrate and lipid metabolism, and is reflected in the BMI with higher frequency of overweight and obesity, total body fat and waist circumference, independently of anti-hyperglycemic therapy.28 In addition, this high dietary fat intake and excessive total body fat could downregulate SLC22A1/OCT1 gene expression as shown by study of Lu et al, and consequently, the pharmacokinetics of metformin and its therapeutic effect.7
The genotypic and allelic frequencies shown in this study are similar to those reported by Reséndiz-Abarca et al, in another group of Mexican patients with T2D where the risk allele A was 16.9%, which is in accordance with the allele A frequency observed in our population.32 In the 1000 Genomes Project Phase 3, the reported global frequency of this polymorphism (rs628031) for the risk allele A is 31%, with Europe being the geographical region where it reaches the highest frequency (41%), followed by Southeast Asia (39%), Africa (27%), East Asia (26%) and the lowest frequency of 22% is reported in America.29
The risk allele A of the Met408Val (rs628031) polymorphism in the SLC22A1/OCT1 gene has been associated with decreased therapeutic efficacy of metformin in several populations worldwide, and recently with a significant increase of %HbA1c in patients with T2D from Mexico, a country that belongs to the North American region.8,29,30 With this low frequency of the A allele in the Mexican population (13% – 17%) and probably in other Latin American countries like Brazil where the prevalence of T2D is high,31 it would be expected that more subjects achieve the goal of glycemic control %HbA1c <7 with metformin therapy. In contrast, the high frequency of this risk allele in Europe and United States of America, could be of clinical consideration in those who do not achieve the glycemic goal of HbA1c <7% with metformin as monotherapy.31,32 However, allele analysis showed that despite the fact that carriers of the risk A allele have significantly less time with T2D and anti-hyperglycemic therapy, they do not shower better glycemic control than carriers of the G allele as it could be expected for a shorter period of time with T2D, which is consistent with a decreased anti-hyperglycemic effect in these carriers as shown in other studies.8,9
A relevant nutrigenetic finding of this study was the interactions between the Met408Val polymorphism (rs628031) of SLC22A1/OCT1 gene and the dietary intakes of calcium and potassium regarding glycemic outcomes as statistically significant differences were found. This data highlights the importance of gene-micronutrient interactions and status monitoring in T2D patients, particularly for SLC22A1/OCT1 (rs628031) risk allele A carriers, to achieve an improved metabolic control within a new metabolic approach that entails personalized medicine. Moreover, our results are consistent with previous reports analyzing the role of DRD2 and APOE gene variants on glycemic outcomes in T2D patients through nutritional interactions.10,33 This association between higher calcium and potassium consumption with the increase in %HbA1c and TyG index in T2D patients carrying the risk allele A of polymorphism of SLC22A1/OCT1 gene (rs628031) has an important clinical significance because there are populations such as the Caucasian European whose prevalence of this risk allele A is close to 50% and the prevalence of osteoporosis after 60 years of age is greater than 10%, and in these adult patients, the recommended calcium daily intake is between 800 and 1200 mg, which could affect glycemic control.34,35
It should be noted that there is a wide acknowledgement on the effect of metformin on the 5’ adenosine monophosphate-activated protein kinase/sirtuin1 (AMPK/Sirt1) pathway activation to modulate blood glucose levels and hepatic glucose production.21,36,37 In type 2 diabetes, obesity and insulin resistance, AMPK and Sirt1 become important targets since they decrease hyperglycemia and show similar metabolic outcomes.38–40
Furthermore, Fu et al, reported synergistic activity between metformin administration and the branched-chain amino acid (BCAA) leucine intake on glycemic control as leucine may activate AMPK/Sirt1 pathway in diet-induced obese mice.41 In this sense, we also suggested possible synergistic activity between calcium intake and metformin in the monotherapy group, since intracellular calcium through calcium/calmodulin-dependent kinase II (CaMKII) increases the AMP/ADP ratio, and consequently activates the AMPK pathway.42–44 This could explain, in part why the individuals with metformin as monotherapy had better glycemic control compared with dual or triple therapy.
Besides, other authors have suggested a possible interaction between the co-administration of metformin. Shibata, et al, reported that peficitinib inhibited Metformin uptake in OCT1 and MATE1/2-K-expressing cells.45 Therefore, we suspect a drug–drug interaction on glycemic control, due to the metformin monotherapy effect, which was not found in the other study groups, but more studies are necessary. Moreover, our findings suggest that polymorphism SLC22A1/OCT1 (rs628031) and the effect of metformin may have modified the expected response between glycemic control and micronutrient intake, since the group with A risk allele + metformin drug and higher calcium intake showed a low diabetes control. From the clinical point of view, it is worth considering that a subject with metformin monotherapy who does not achieve the glycemic control goal of %HbA1c <7 in the early stages of T2D, could be a carrier of the risk allele A with a higher dietary intake of calcium or potassium than the recommended dosage.
A limitation of this study is the population studied as extrapolation to a larger population and the blood concentration of metformin as the main endpoint are needed because other factors in glycemic control might intervene, such as insulin secretion capacity, resistance to the action of this hormone, adiposity, diet, and physical activity. Moreover, although interaction studies are very reliable, type I and type II statistical errors cannot be completely ruled out.
Conclusion
This study reports a relevant interaction between the micronutrient intake of calcium and potassium with the Met408Val (rs628031) polymorphism of the SLC22A1/OCT1 gene regarding the glycemic control of patients with T2D from western Mexico. Subjects who received metformin as monotherapy and are carriers of the risk allele A of the Met408Val (rs628031) polymorphism showed a significant positive correlation between calcium intake and %HbA1c, as well as potassium with the TyG index. These findings suggest a differential effect of metformin on glycemic control depending on calcium and potassium intake regarding the Met408Val (rs628031) polymorphism of the SLC22A1/OCT1 gene in patients with T2D. One perspective to consider with these findings is the relevance of micronutrient interactions for new therapeutic approaches in primary care to contribute to glycemic control.
Acknowledgments
The authors express their gratitude to participants of this cohort study for their enthusiastic support and the staff of Family Medicine Unit No. 24 of Mexican Institute of Social Security for their valuable help. We acknowledge students in Nutrition Luis Roberto Mejia Godoy and Ivette Xitlalli Eleuterio Salvador, as well as Pharmaceutical Chemists Fabiola B. Moreno Escalera, Kevin J, Frías Delgadillo and Sara A. Campos Huerta for their support in obtaining data of all patients in this study.
To the Interinstitutional Program for the Strengthening of Research and Graduate Studies of the Pacific (Dolphin Program) for promoting the collegiate work that led to the creation of the Dolphin Research Networks within the mobility subprogram of professors and researchers.
Funding Statement
The laboratory infrastructure was supported by The National Council for Science and Technology (CONACyT), México (grant number: INFR-2016-01-268517) and material by The Secretary of Public Education (SEP), México (grant number: P/PFCE-2018-18MSU0019M-04). Part of this project was carried out with resources from the special tax destined to the Autonomous University of Nayarit (Article Publishing Charge) Both sources did not participate in the collection, analysis and interpretation of data; neither in the writing and/or in the decision to submit this article.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.An H, He L. Current understanding of metformin effect on the control of hyperglycemia in diabetes. J Endocrinol. 2016;228(3):R97–R106. doi: 10.1530/JOE-15-0447 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jing Y, Wu F, Li D, Yang L, Li Q, Li R. Metformin improves obesity-associated inflammation by altering macrophages polarization. Mol Cell Endocrinol. 2018;461:256–264. doi: 10.1016/j.mce.2017.09.025 [DOI] [PubMed] [Google Scholar]
- 3.Yerevanian A, Soukas AA. Metformin: mechanisms in human obesity and weight loss. Curr Obes Rep. 2019;8(2):156–164. doi: 10.1007/s13679-019-00335-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Le S, Lee GC. Emerging trends in metformin prescribing in the United States from 2000 to 2015. Clin Drug Investig. 2019;39(8):757–763. doi: 10.1007/s40261-019-00799-0 [DOI] [PubMed] [Google Scholar]
- 5.Madiraju AK, Erion DM, Rahimi Y, et al. Metformin suppresses gluconeogenesis by inhibiting mitochondrial glycerophosphate dehydrogenase. Nature. 2014;510(7506):542–546. doi: 10.1038/nature13270 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.American Diabetes Association. 8. obesity management for the treatment of type 2 diabetes: standards of medical care in diabetes-2021. Diabetes Care. 2021;44(Suppl1):S100–S110. doi: 10.2337/dc21-S008. [DOI] [PubMed] [Google Scholar]
- 7.Lu X, Dong Y, Jian Z, et al. Systematic investigation of the effects of long-term administration of a high-fat diet on drug transporters in the mouse liver, kidney and intestine. Curr Drug Metab. 2019;20(9):742–755. doi: 10.2174/1389200220666190902125435 [DOI] [PubMed] [Google Scholar]
- 8.Mofo Mato EP, Guewo-Fokeng M, Essop MF, Owira PMO. Genetic polymorphisms of organic cation transporter 1 (OCT1) and responses to metformin therapy in individuals with type 2 diabetes: a systematic review. Medicine. 2018;97(27):e11349. doi: 10.1097/MD.0000000000011349 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nasykhova YA, Tonyan ZN, Mikhailova AA, Danilova MM, Glotov AS. Pharmacogenetics of Type 2 diabetes-progress and prospects. Int J Mol Sci. 2020;21(18):E6842. doi: 10.3390/ijms21186842 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Torres-Valadez R, Ramos-Lopez O, Frías Delgadillo KJ, et al. Impact of APOE alleles-by-diet interactions on glycemic and lipid features- a cross-sectional study of a cohort of type 2 diabetes patients from Western Mexico: implications for personalized medicine. Pharmgenomics Pers Med. 2020;13:655–663. doi: 10.2147/PGPM.S277952 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.World Medical Association. World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA. 2013;310(20):2191–2194. doi: 10.1001/jama.2013.281053. [DOI] [PubMed] [Google Scholar]
- 12.American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care. 2010;33(Suppl 1):S62–69. doi: 10.2337/dc10-S062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Torres-Castillo N, Campos-Perez W, Gonzalez-Becerra K, et al. Waist circumference is an anthropometric parameter that identifies women with metabolically unhealthy phenotypes. Nutrients. 2018;10(4):E447. doi: 10.3390/nu10040447 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.WHO consultation on obesity(1999: Geneva S, World Health Organization). Obesity: preventing and managing the global epidemic: report of a WHO consultation. World Health Organization; 2000. Accessed November 14, 2021. https://apps.who.int/iris/handle/10665/42330. [PubMed] [Google Scholar]
- 15.SMAE-4a-ed-Ana-Bertha-P®rez-Lizaur.pdf. Available from: https://www.cdefis.com/wp-content/uploads/2020/01/SMAE-4a-ed-Ana-Bertha-P%C2%AErez-Lizaur.pdf. Accessed November 14, 2021.
- 16.Official Mexican Standard NOM-015-SSA2-2010, for prevention, treatment and control of diabetes mellitus. Available from: http://www.dof.gob.mx/normasOficiales/4215/salud/salud.htm. Accessed November 9, 2021.
- 17.Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem. 1972;18(6):499–502. doi: 10.1093/clinchem/18.6.499 [DOI] [PubMed] [Google Scholar]
- 18.Navarro-González D, Sánchez-íñigo L, Pastrana-Delgado J, Fernández-Montero A, Martinez JA. Triglyceride-glucose index (TyG index) in comparison with fasting plasma glucose improved diabetes prediction in patients with normal fasting glucose: the vascular-metabolic CUN cohort. Prev Med. 2016;86:99–105. doi: 10.1016/j.ypmed.2016.01.022 [DOI] [PubMed] [Google Scholar]
- 19.National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). Third Report of the National Cholesterol Education Program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel III) final report. Circulation. 2002;106(25):3143–3421. doi: 10.1161/circ.106.25.3143 [DOI] [PubMed] [Google Scholar]
- 20.Miller SA, Dykes DD, Polesky HF. A simple salting out procedure for extracting DNA from human nucleated cells. Nucleic Acids Res. 1988;16(3):1215. doi: 10.1093/nar/16.3.1215 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rena G, Hardie DG, Pearson ER. The mechanisms of action of metformin. Diabetologia. 2017;60(9):1577–1585. doi: 10.1007/s00125-017-4342-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.You Y, Doubova SV, Pinto-Masis D, Pérez-Cuevas R, Borja-Aburto VH, Hubbard A. Application of machine learning methodology to assess the performance of DIABETIMSS program for patients with type 2 diabetes in family medicine clinics in Mexico. BMC Med Inform Decis Mak. 2019;19(1):221. doi: 10.1186/s12911-019-0950-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.American Diabetes Association. Standards of medical care in diabetes–2014. Diabetes Care. 2014;37(Suppl 1):S14–80. doi: 10.2337/dc14-S014. [DOI] [PubMed] [Google Scholar]
- 24.NICE. Overview | type 2 diabetes in adults: management | guidance | NICE. Available from: https://www.nice.org.uk/guidance/ng28. Accessed November 14, 2021.
- 25.U.K. Prospective Diabetes Study Group. U.K. prospective diabetes study 16. Overview of 6 years’ therapy of type II diabetes: a progressive disease. Diabetes. 1995;44(11):1249–1258. doi: 10.2337/diab.44.11.1249 [DOI] [PubMed] [Google Scholar]
- 26.Weir GC, Bonner-Weir S. Five stages of evolving beta-cell dysfunction during progression to diabetes. Diabetes. 2004;53(Suppl 3):S16–21. doi: 10.2337/diabetes.53.suppl_3.s16 [DOI] [PubMed] [Google Scholar]
- 27.Ramos-Lopez O, Panduro A, Rivera-Iñiguez I, Roman S. Dopamine D2 receptor polymorphism (C957T) is associated with sugar consumption and triglyceride levels in West Mexicans. Physiol Behav. 2018;194:532–537. doi: 10.1016/j.physbeh.2018.07.004 [DOI] [PubMed] [Google Scholar]
- 28.Santiago-Torres M, Kratz M, Lampe JW, et al. Metabolic responses to a traditional Mexican diet compared with a commonly consumed US diet in women of Mexican descent: a randomized crossover feeding trial. Am J Clin Nutr. 2016;103(2):366–374. doi: 10.3945/ajcn.115.119016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Reséndiz-Abarca CA, Flores-Alfaro E, Suárez-Sánchez F, et al. Altered glycemic control associated with polymorphisms in the SLC22A1 (OCT1) gene in a Mexican Population with type 2 diabetes mellitus treated with metformin: a cohort study. J Clin Pharmacol. 2019;59(10):1384–1390. doi: 10.1002/jcph.1425 [DOI] [PubMed] [Google Scholar]
- 30.Rotroff DM, Yee SW, Zhou K, et al. Genetic variants in CPA6 and PRPF31 are associated with variation in response to metformin in individuals with type 2 diabetes. Diabetes. 2018;67(7):1428–1440. doi: 10.2337/db17-1164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Khan MAB, Hashim MJ, King JK, Govender RD, Mustafa H, Al Kaabi J. Epidemiology of type 2 diabetes – global burden of disease and forecasted trends. J Epidemiol Glob Health. 2020;10(1):107–111. doi: 10.2991/jegh.k.191028.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Global report on diabetes. Available from: https://www.who.int/publications-detail-redirect/9789241565257. Accessed November 14, 2021.
- 33.Ramos-Lopez O, Mejia-Godoy R, Frías-Delgadillo KJ, et al. Interactions between DRD2/ANKK1 TaqIA polymorphism and dietary factors influence plasma triglyceride concentrations in diabetic patients from Western Mexico: a cross-sectional study. Nutrients. 2019;11(12):E2863. doi: 10.3390/nu11122863 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kanis JA, Harvey NC, McCloskey E, et al. Algorithm for the management of patients at low, high and very high risk of osteoporotic fractures. Osteoporos Int. 2020;31(1):1–12. doi: 10.1007/s00198-019-05176-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Al-Saleh Y, Al-Daghri NM, Sabico S, et al. Diagnosis and management of osteoporosis in postmenopausal women in Gulf Cooperation Council (GCC) countries: consensus statement of the GCC countries’ osteoporosis societies under the auspices of the European Society for Clinical and Economic Aspects of Osteoporosis and Osteoarthritis (ESCEO). Arch Osteoporos. 2020;15(1):109. doi: 10.1007/s11657-020-00778-5 [DOI] [PubMed] [Google Scholar]
- 36.Towler MC, Hardie DG. AMP-activated protein kinase in metabolic control and insulin signaling. Circ Res. 2007;100(3):328–341. doi: 10.1161/01.RES.0000256090.42690.05 [DOI] [PubMed] [Google Scholar]
- 37.Foretz M, Guigas B, Viollet B. Understanding the glucoregulatory mechanisms of metformin in type 2 diabetes mellitus. Nat Rev Endocrinol. 2019;15(10):569–589. doi: 10.1038/s41574-019-0242-2 [DOI] [PubMed] [Google Scholar]
- 38.Banerjee J, Bruckbauer A, Zemel MB. Activation of the AMPK/Sirt1 pathway by a leucine-metformin combination increases insulin sensitivity in skeletal muscle, and stimulates glucose and lipid metabolism and increases life span in Caenorhabditis elegans. Metabolism. 2016;65(11):1679–1691. doi: 10.1016/j.metabol.2016.06.011 [DOI] [PubMed] [Google Scholar]
- 39.Ido Y. Diabetic complications within the context of aging: nicotinamide adenine dinucleotide redox, insulin C-peptide, sirtuin 1-liver kinase B1-adenosine monophosphate-activated protein kinase positive feedback and forkhead box O3. J Diabetes Investig. 2016;7(4):448–458. doi: 10.1111/jdi.12485 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Zang Y, Fan L, Chen J, Huang R, Qin H. Improvement of lipid and glucose metabolism by capsiate in palmitic acid-treated HepG2 cells via activation of the AMPK/SIRT1 signaling pathway. J Agric Food Chem. 2018;66(26):6772–6781. doi: 10.1021/acs.jafc.8b01831 [DOI] [PubMed] [Google Scholar]
- 41.Fu L, Bruckbauer A, Li F, et al. Leucine amplifies the effects of metformin on insulin sensitivity and glycemic control in diet-induced obese mice. Metabolism. 2015;64(7):845–856. doi: 10.1016/j.metabol.2015.03.007 [DOI] [PubMed] [Google Scholar]
- 42.Richter EA, Hargreaves M. Exercise, GLUT4, and skeletal muscle glucose uptake. Physiol Rev. 2013;93(3):993–1017. doi: 10.1152/physrev.00038.2012 [DOI] [PubMed] [Google Scholar]
- 43.Fogarty S, Hawley SA, Green KA, Saner N, Mustard KJ, Hardie DG. Calmodulin-dependent protein kinase kinase-β activates AMPK without forming a stable complex: synergistic effects of Ca2+ and AMP. Biochem J. 2010;426(Pt1):109–118. doi: 10.1042/BJ20091372 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Swulius MT, Waxham MN. Ca2+/Calmodulin-dependent protein kinases. Cell Mol Life Sci. 2008;65(17):2637–2657. doi: 10.1007/s00018-008-8086-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Shibata M, Toyoshima J, Kaneko Y, Oda K, Nishimura T. A drug-drug interaction study to evaluate the impact of peficitinib on OCT1- and MATE1-mediated transport of metformin in healthy volunteers. Eur J Clin Pharmacol. 2020;76(8):1135–1141. doi: 10.1007/s00228-020-02876-2 [DOI] [PMC free article] [PubMed] [Google Scholar]