FIG 3.
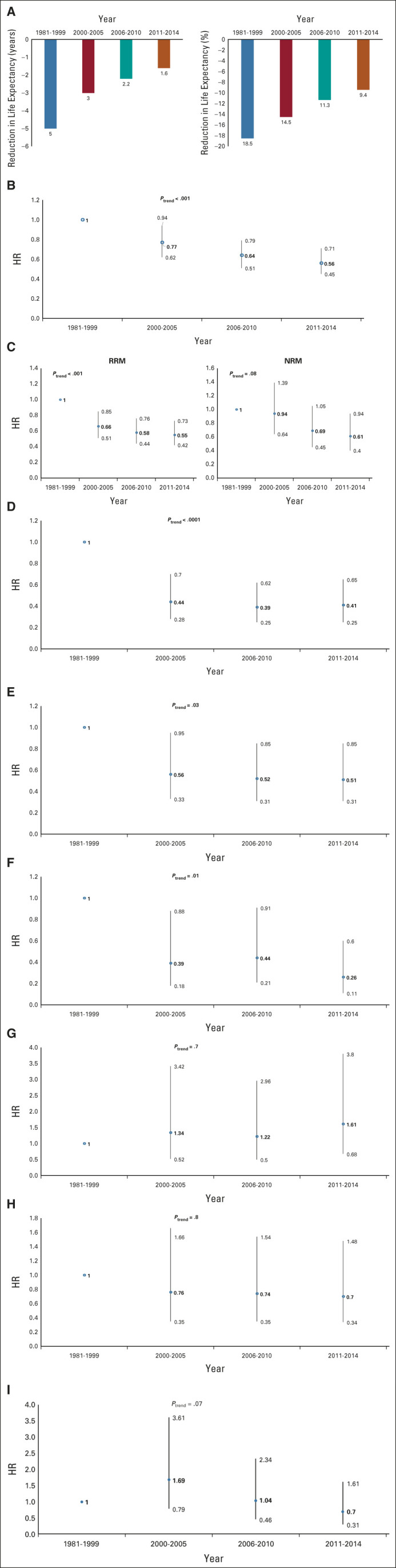
(A) Trends in reduction in life expectancy by transplant era in a cohort of autologous BMT recipients surviving 2 or more years after transplantation. The follow-up was truncated at 5 years post-BMT to allow comparison across the four eras. The models were adjusted for age at transplantation, sex, race/ethnicity, primary diagnosis, disease status at BMT, stem-cell source, and use of TBI. (B) Trends in hazard of all-cause late mortality by transplant era in a cohort of autologous BMT recipients surviving 2 or more years after transplantation. The follow-up was truncated at 5 years post-BMT to allow comparison across the four eras. The models were adjusted for age at transplantation, sex, race/ethnicity, primary diagnosis, disease status at BMT, stem-cell source, and use of TBI. (C) Trends in hazard of cause-specific late mortality by transplant era in a cohort of autologous BMT recipients surviving 2 or more years after transplantation. The follow-up was truncated at 5 years post-BMT to allow comparison across the four eras. The models were adjusted for age at transplantation, sex, race/ethnicity, primary diagnosis, disease status at BMT, stem-cell source, and use of TBI. (D) Trends in hazards of infection-related late mortality by transplant era in a cohort of autologous BMT recipients surviving 2 or more years after transplantation. The follow-up was truncated at 5 years post-BMT to allow comparison across the four eras. The models were adjusted for age at transplantation, sex, race/ethnicity, primary diagnosis, disease status at BMT, stem-cell source, and use of TBI. (E) Trends in hazards of SMN-related late mortality by transplant era in a cohort of autologous BMT recipients surviving 2 or more years after transplantation. The follow-up was truncated at 5 years post-BMT to allow comparison across the four eras. The models were adjusted for age at transplantation, sex, race/ethnicity, primary diagnosis, disease status at BMT, stem-cell source, and use of TBI. (F) Trends in hazards of t-MN–related late mortality by transplant era in a cohort of autologous BMT recipients surviving 2 or more years after transplantation (t-MN). The follow-up was truncated at 5 years post-BMT to allow comparison across the four eras. The models were adjusted for age at transplantation, sex, race/ethnicity, primary diagnosis, disease status at BMT, stem-cell source, and use of TBI. (G) Trends in hazards of solid SMN-related late mortality by transplant era in a cohort of autologous BMT recipients surviving 2 or more years after transplantation. The follow-up was truncated at 5 years post-BMT to allow comparison across the four eras. The models were adjusted for age at transplantation, sex, race/ethnicity, primary diagnosis, disease status at BMT, stem-cell source, and use of TBI. (H) Trends in hazards of cardiac-related late mortality by transplant era in a cohort of autologous BMT recipients surviving 2 or more years after transplantation. The follow-up was truncated at 5 years post-BMT to allow comparison across the four eras. The models were adjusted for age at transplantation, sex, race/ethnicity, primary diagnosis, disease status at BMT, stem-cell source, and use of TBI. (I) Trends in hazards of renal-related late mortality by transplant era in a cohort of autologous BMT recipients surviving 2 or more years after transplantation. The follow-up was truncated at 5 years post-BMT to allow comparison across the four eras. The models were adjusted for age at transplantation, sex, race/ethnicity, primary diagnosis, disease status at BMT, stem-cell source, and use of TBI. BMT, blood or marrow transplantation; HR, hazard ratio; NRM, non–recurrence-related mortality; RRM, recurrence-related mortality; SMN, subsequent malignant neoplasm; TBI, total body irradiation; t-MN, therapy-related myeloid neoplasm.
