Table 4.
Treatment for cholera case management.
| Acute Watery Diarrhea (AWD) with: | ||||
|---|---|---|---|---|
| No dehydration |
Moderate dehydration (if two or more signs, including at least one major sign) |
Severe dehydration (if two or more signs, including at least one major sign) |
||
| Signs | Mouth/tongue | Moist | Dry | Very dry |
| Thirst1 | Drinks normally | Thirsty, drinks eagerly3 | Drinks poorly or not able to drink3 | |
| Skin pinch2 | Goes back quickly | Goes back slowly3 | Goes back very slowly (>2 sec) 3 | |
| Treatment4 | Maintain hydration (Treatment plan A) |
ORS (Treatment plan B) |
IV, ORS, antibiotic (Treatment plan C) |
|
| • ORS after each loose stool to maintain hydration until diarrhea stops • If patient lives far from treatment center or correct home treatment can't be guaranteed: keep under observation • Sent home with a 2-day supply of ORS with instruction on preparing ORS solution with clean water and schedule: 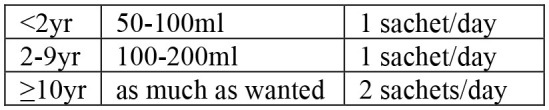 • Instruct patient to return to treatment center if condition deteriorates (if repeated vomiting, number of stools increased, patient drinks or eats poorly) • If patient starts vomiting or develops abdominal distension: Ringer's Lactate 50 ml/kg over 3 h, followed by ORS after assessment of hydration status (monitor every 4 h) |
• Admit to treatment center • ORS and monitor until diarrhea/vomiting stops (if patient vomits, wait 10 min, and continue slowly) • Amount of ORS required in 4 h subject to patient's weight (75 ml/kg in 4 h). If patient's weight is unknown, use age 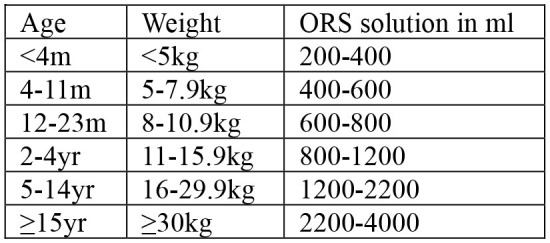 • During first 2 h of treatment: monitor rehydration frequently (at least every hour) • After first 4 hours of treatment: if no more signs of dehydration, follow Treatment Plan A • After first 4 h of treatment: if still signs of moderate dehydration, repeat Treatment plan B for another 4 h and reassess • At any time during treatment: if patient's symptoms deteriorate (if signs of severe dehydration, confused or disorientated, frequent/severe vomiting), immediately shift to Treatment plan C • If patient can't drink and if IV therapy not feasible at treatment center: rehydrate patient using nasogastric tube |
• Admit to treatment center • IV treatment immediately to restore normal hydration within 3–6 h: 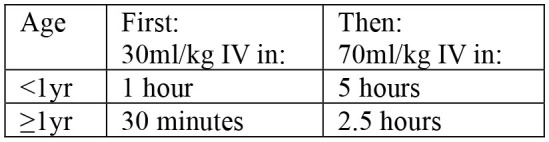 - Ringer's lactate as first choice of IV fluids - If Ringer's lactate not available, normal saline or 5% glucose in normal saline - Plain 5% glucose solution not recommended • If patient can drink, ORS 5 ml/kg/h can be also given simultaneouly with IV drip • If fluid can't be given through IV route, give ORS (20 ml/kg over 6 h) through a nasogastric tube • Assess patient's condition every 30 min during the first 2 h; then every h for next 6–12 h • Monitor pulse and respiratory rates, frequency of urine, stool, and vomiting- Regular urine output (every 3–4 h): good sign of enough fluid- Sign of increasing edema: evidence of over hydration- Sign of continued fast breathing and rapid pulse rate during rehydration: may be early signs of heart failure- Stop rehydration immediately if patient shows any of these signs • Antibiotics5 only to patients with severe dehydration to shorten duration of illness and carriage of pathogen |
||
Reconstructed based on the Guideline on Cholera Outbreak Management Ethiopia, Ethiopia Health and Nutrition Research Institute (EHNRI (now EPHI)), 2011.
ORS (Oral Rehydration Solution), IV (Intravenous) rehydration therapy, yr (year), m (month), h (hour).
Thirst: Give fluid to patient to observe this sign.
Skin pinch: Pinch abdominal skin and release to observe this sign. Notably, skin pinch may go back quickly in a severely malnourished patient such as a child with kwashiorkor even at dehydration condition. In such situation, monitoring the patient's weight is recommended to confirm dehydration.
Major signs.
For treatment of severely malnourished patients: ORS for moderate dehydration with no signs of shock (20ml/kg in first 2 hours at rate of 5ml/kg every 30 minutes, followed by 50ml/kg at rate of 5ml/kg/hour for up to 10 hours); and IV for severe dehydration with signs of shock (Ringer Lactate 15ml/kg/hour over 2 hours, followed by ORS 10ml/kg/hour until dehydration is corrected). Breast-feeding and therapeutic milk possible during oral rehydration.
Antibiotics (per EHNRI/EPHI guideline): For only severely dehydrated cholera patients; after IV rehydration. Mass chemoprophylaxis not recommended for cholera outbreak control. Selective chemoprophylaxis (1 dose of Doxycycline) may be useful for household members sharing food and shelter with cholera patient. Doxycycline (1 dose): for adults (except pregnant women); contra-indicated in pregnant or breast-feeding women and children under 8 years of age but can be used to treat cholera as 1 dose should not have any adverse effects. Amoxicillin syrup: for children; can be used also for adults if other antibiotics not available or V. cholerae resistant to those. Erythromycin: for pregnant women; may be used if other antibiotics not available or V. cholerae resistant to those.
