Abstract
Purpose
The coronavirus disease 2019 (COVID-19) pandemic has caused changes in the daily lives of Korean adolescents and affected their emotional well-being. This study compared lifestyle factors and the mental health status of adolescents before and during the COVID-19 pandemic.
Methods
We conducted a secondary analysis using data from a national cross-sectional cohort (Korean Youth Risk Behavior Web-based Survey, KYRBS) collected in 2019 before the COVID-19 outbreak and in 2020 during the pandemic. This study included 57,303 students from the 2019 KYRBS and 54,948 from the 2020 KYRBS. Lifestyle factors such as dietary habits, physical activity levels, time spent studying, duration of Internet use, and mental health status, including perceived stress, experience of depressive mood, and suicidal ideation and attempts, were included in the analyses.
Results
The perceived stress levels, self-reported depressive mood, and suicidal thoughts and attempts were lower in the students surveyed in 2020 during the COVID-19 pandemic than in the students surveyed in 2019 before the COVID-19 outbreak. The time spent studying and sleep duration decreased compared to before the pandemic, and sleep satisfaction increased during the COVID-19 pandemic.
Discussion
Our results showed an improvement in mental health status in Korean adolescents during the pandemic, but caution is needed when interpreting these results. Future research is needed to determine the effects of a long-lasting pandemic on mental health and lifestyle factors in adolescents.
Keywords: COVID-19, Adolescents, Depression, Lifestyle factors, Suicide, KYRBS
Implications and Contribution.
The COVID-19 pandemic has changed in the daily lifestyle factors of adolescents and affected their mental health status. This study confirms the impact of the pandemic on Korean adolescents using national cross-sectional cohort data collected in 2019 before the COVID-19 outbreak and in 2020 during the pandemic. These results show that perceived stress and the risk of experiencing depressive mood and suicidal ideation/attempts were reduced during the pandemic.
In November 2019, a novel coronavirus (2019-nCoV) broke out in Wuhan, China, and the coronavirus disease 2019 (COVID-19) pandemic has spread rapidly across all continents [1,2]. In South Korea, the COVID-19 outbreak began in January 2020, and after February 19, the number of infected people has increased rapidly [3]. Many changes have occurred in people's daily lives, to prevent the spread of 2019-nCoV infection during the pandemic. The Korean government conducted a “social distancing” campaign to minimize contact between people and recommended minimizing people's outside activities. Due to school closures, students have experienced unprecedented disruptions in their daily lives [4] and have participated in classes at home via the Internet instead of attending school. As the COVID-19 pandemic continues, people have experienced emotional difficulties in adapting to new environments, and the number of people reporting emotional difficulties has increased [[5], [6], [7], [8], [9]]. In a previous study on Koreans, >40% of participants reported clinically significant levels of depression, anxiety, or stress because of the pandemic [5]. Similar findings on the deterioration of mental health caused by COVID-19 have been reported elsewhere [[6], [7], [8]]. An increased rate of mental health issues such as depression, insomnia, and high perceived stress has been observed because of the COVID-19 pandemic in Italy [7]. People with pre-existing mental illness reported worsening psychiatric symptoms, and a decrease in psychological well-being was observed in the general population [8].
Adolescence is the stage of transition to adulthood and an important period of identity development [10]. In this process, adolescents may also experience several changes in their lifestyle and are vulnerable to the influence of social environments [11]. They may have difficulty controlling their emotions, and the risk of developing mental disorders such as depressive and anxiety disorders are increased [12,13]. Deterioration in adolescents' mental health can cause a decline in the functioning of daily life, including academic achievement, and it can have a negative effect until adulthood [14,15]. The pandemic has made it impossible for adolescents to attend school regularly, and restrictions that can negatively affect the daily lives of adolescents have continued. School closures and restrictions are expected to negatively affect the mental health of adolescents [16]. In a recent review, Racine et al. [9] reported an increase in depressive and anxiety symptoms among children and adolescents in the United States and China during the pandemic. In countries where the pandemic is expected to prolong, the mental health of adolescents is at risk of worsening; therefore, it is important to identify high-risk adolescents who can be adversely affected.
Previous studies have reported findings on the association between COVID-19 and adolescents' mental health; however, studies using a nationally representative sample that represents adolescents in each country are limited, and this is the first such sample with Koreans. We compared the mental health and lifestyle factors of Korean adolescents through the youth survey data conducted in 2019 before the 2019-nCoV outbreak and in 2020 during the pandemic. We intended to identify the changes in mental health status and lifestyle factors of Korean adolescents during the COVID-19 pandemic. Similar to previous studies, we hypothesized that (1) Korean adolescents will experience greater perceived stress, depressive mood, suicidal ideation, and suicide attempts during the pandemic than before the pandemic; and (2) there will be changes in lifestyle factors of Korean adolescents due to the COVID-19 pandemic, and that these changes will affect the mental status of adolescents. In addition, we hypothesized that there would be a difference in the impact of the COVID-19 pandemic according to sex and age, and we examined changes in the mental health status of each group according to sex and school level.
Methods
Participants
We performed a secondary data analysis using the 2019 Korean Youth Risk Behavior Web-based Survey (KYRBS) data and 2020 KYRBS data files for the SPSS program provided by the Korea Centers for Disease Control and Prevention Agency (KDCA). The KYRBS is a cross-sectional study conducted with students aged 12–18 years at 400 middle schools and 400 high schools using a multi-stage cluster sampling design. The KYRBS is conducted annually by the KDCA to evaluate the physical and mental health status of Korean students and was introduced in a previously published paper [17]. A detailed description of the KYRBS is provided in Supplemental Information 1. Due to the COVID-19 pandemic, the 2020 KYRBS was conducted with students from 398 middle schools and 395 high schools. The 2019 KYRBS was conducted from June to July 2019, and 57,303 students participated in the study. The 2020 KYRBS was conducted from August to November 2020, and 54,948 students participated (see Supplemental Information 1). The analyses included participant demographics, perceived health status, lifestyle factors, and mental health-related data.
Assessment
Demographic information and perceived health status
Individual demographic data such as sex, school grade, academic achievement, household economic status, and type of residence were included in the analyses. Academic achievement and household economic status were subjectively evaluated by respondents and were classified into five categories: “upper”, “upper middle”, “middle”, “lower middle”, and “lower”. Participants subjectively reported information related to their health status, weight, and body perception.
Lifestyle factors
Variable lifestyle factors, such as breakfast frequency, physical activity level, sleep habits, sitting time spent studying, and duration of Internet/smartphone use were included in the analyses. Participants responded to the frequency of breakfast consumption and the number of days of physical activity in the preceding 7 days. The question on physical activity assessed the number of days on which their heart rate was higher than usual or whether they engaged in 60 minutes or more of physical activity, which left them breathless, regardless of the type of physical activity. For sleeping habits, participants answered questions on their weekday bedtime and wake-up time, which were used to calculate their total weekday sleep time. We excluded participants who reported sleep durations of <3 hours or >15 hours because the reliability of this response was considered questionable. Participants were also asked to report the average sitting time spent studying and the average Internet/smartphone usage time. The question about Internet/smartphone usage time was different in the 2019 and 2020 KYRBS. In the 2019 KYRBS, Internet usage time was used, and in the 2020 KYRBS, smartphone usage time was evaluated, and the period was revised from 30 to 7 days for the convenience of answering (see Supplemental Information 1). We also assessed other lifestyle factors, including smoking, alcohol use, sexual activity, and hospital treatment for violent events within 1 year.
Mental health status and suicidality
The degree of stress perceived by individuals and their experience of depressive mood were investigated. The individual perceived stress level was classified into five responses: “very much”, “a lot,” “a little”, “not much”, and “not at all”. Experience of depressive mood was evaluated through the question “During the last 12 months, have you ever had enough sad or desperate times to stop your daily activities for 2 weeks?” Experience of depressive mood persisting for more than 2 weeks is one of the core symptoms of major depressive disorder based on the Diagnostic and Statistical Manual of Mental Disorders, fifth Edition (DSM-V), which is also used as a screening question [18,19]. To determine whether suicidal thoughts or suicide attempts had occurred, two questions assessing suicidal ideation and suicidal attempt in the past 12 months were asked (answered yes/no) (see Supplemental Information 1).
Statistical analyses
Among the students who participated in the KYRBS in 2019 and 2020, those who answered insufficiently were excluded, and 98,126 students were included in the analyses (51,651 students in the 2019 KYRBS and 46,475 students in the 2020 KYRBS). All statistical analyses were performed using the SPSS software (version 25.0; IBM Corp., Armonk, NY, 2019), and p-values <.05 were considered statistically significant. Subjective health perception, subjective stress level, experience of depressive mood, suicidal thoughts, and suicide attempts were compared between the 2019 and 2020 KYRBS participants using a chi-square test. To assess the impact of the COVID-19 pandemic by sex and grade, participants were stratified into the following four categories: male middle school students (N = 25,942), female middle school students (N = 24,424), male high school students (N = 24,805), and female high school students (N = 22,955). Grades 7–9 are considered middle school and grades 10–12 are considered high school in the Korean education system. In this analysis, we identified differences in students' lifestyle factors before and after the COVID-19 pandemic using student's t-test. Furthermore, by comparing the degree of stress perception, experience of depressive mood, suicidal ideation, and suicide attempts of the participants by group, we identified groups that were vulnerable to the COVID-19 pandemic. We also performed two logistic regression analyses with a stepwise backward elimination model selection method to investigate whether the odds ratio for experiencing depressive mood varied with the year of study and other variables. First, we used depressive mood (reference: no depressive mood) as the dependent variable and the other study variables, except for perceived stress, as independent variables. In the other logistic regression, we used depressive mood (reference: no depressive mood) as the dependent variable and the other study variables as the independent variables.
Ethics statement
KYRBS was conducted by the Ministry of Education, Ministry of Health and Welfare, and KDCA as a nationally approved statistical data [17]. The study protocol was approved by the Institutional Review Board of the Korea University Medical Center, Ansan Hospital, Gyeonggi-do, Korea (No. 2021AS0135).
Results
Sociodemographic characteristics and perceived health status
The major findings are summarized in Table 1 and detailed information is provided in Table S1. More males participated than females in both groups, but the difference was not statistically significant. There was no significant difference in perceived economic status. The percentage of students reporting their perceived health status as “very healthy” or “healthy” increased significantly in 2020, and the percentage of adolescents who perceived their body shape as “obese” or “very obese” also increased. Similarly, the number of students reporting efforts to lose weight has increased from 33.5% in 2019 to 35.0% in 2020. The percentage of students who assessed their subjective academic performance in the upper or upper-middle class significantly decreased in 2020.
Table 1.
Sociodemographic characteristics and perceived health status
| Variables | 2019 (n: 51,651) | 2020 (n: 46,475) | t or χ2 | p value | Effect size |
|---|---|---|---|---|---|
| Age, years | 14.99 ± 1.78 | 15.12 ± 1.77 | <.001 | 0.0732 | |
| Sex, female, N (%) | 25,061 (48.5) | 22,318 (48.0) | 2.433 | .119 | 0.0050 |
| Perceived economic status, N (%) | 1.361 | .851 | 0.0037 | ||
| Upper | 5,580 (10.8) | 5,045 (10.9) | |||
| Upper middle | 14,650 (28.4) | 13,109 (28.2) | |||
| Middle | 24,846 (48.1) | 22,315 (48.0) | |||
| Lower middle | 5,475 (10.6) | 4,978 (10.7) | |||
| Lower | 1,100 (2.1) | 1,028 (2.2) | |||
| Perceived academic performance, N (%) | 22.953 | <.001 | 0.0153 | ||
| Upper | 6,876 (13.3) | 5,841 (12.6) | |||
| Upper middle | 13,049 (25.3) | 11,572 (24.9) | |||
| Middle | 15,625 (30.3) | 14,131 (30.4) | |||
| Lower middle | 11,306 (21.9) | 10,638 (22.9) | |||
| Lower | 4,795 (9.3) | 4,293 (9.2) | |||
| Perceived health status, N (%) | 17.393 | .002 | 0.0133 | ||
| Very healthy | 13,705 (26.5) | 12,837 (27.6) | |||
| Healthy | 22,668 (43.9) | 19,978 (43.0) | |||
| Mediocre | 11,571 (22.4) | 10,317 (22.2) | |||
| Unhealthy | 3,469 (6.7) | 3,153 (6.8) | |||
| Very unhealthy | 238 (0.5) | 190 (0.4) | |||
| Perception of body shape | 25.727 | <.001 | 0.0162 | ||
| Very skinny | 2,198 (4.3) | 1,896 (4.1) | |||
| Skinny | 10,893 (21.1) | 9,311 (20.0) | |||
| Average | 18,679 (36.2) | 16,832 (36.2) | |||
| Obese | 16,461 (31.9) | 15,164 (32.6) | |||
| Very obese | 3,420 (6.6) | 3,272 (7.0) | |||
| Efforts to control weight | 42.351 | <.001 | 0.0208 | ||
| No | 24,353 (47.1) | 20,954 (45.1) | |||
| Weight loss | 17,302 (33.5) | 16,247 (35.0) | |||
| Weight gain | 3,791 (7.3) | 3,529 (7.6) | |||
| Weight maintenance | 6,205 (12.0) | 5,745 (12.4) | |||
| Alcohol use, yes, N (%) | 20,009 (38.7) | 15,167 (32.6) | 396.353 | <.001 | 0.0636 |
| Violencea, yes, N (%) | 1,045 (2.0) | 509 (1.1) | 135.163 | <.001 | 0.0371 |
Each number is presented as mean ± standard deviation or sample size (ratio by group). The effect size is represented by the index w and Hedges' g.
Violence, experience of being treated by doctor due to violence.
Changes in lifestyle factors by school level and sex
The frequency of physical activity decreased significantly in men, but this result was not significant in women, which may have been because of the low physical activity of female adolescents before the COVID-19 pandemic (average time of physical activity: 1.37 ± 1.75 days in 2019 and 1.38 ± 1.81 days in 2020). The time spent studying significantly decreased in all the groups. Compared to the time spent on the Internet in 2019, the time spent on smartphones in 2020 increased significantly. The average sleep time significantly decreased in all groups, and the sleep time reduced by 2–10 minutes. Bedtime and waking time on weekdays were delayed by 2–13 minutes compared to those before the COVID-19 pandemic, showing a statistically significant difference. In all groups, students' sleep satisfaction increased (Tables 2 and S2).
Table 2.
Lifestyle factors by school level and sex
| Variables | 2019 | 2020 | p value | Effect size |
|---|---|---|---|---|
| Males (Middle school), N | 13,490 | 12,452 | ||
| Time spent studying, min | 363.27 ± 245.37 | 356.13 ± 221.67 | .015 | 0.0305 |
| Duration of internet or smartphone use, min | 141.92 ± 113.75 | 237.34 ± 172.27 | <.001 | 0.6589 |
| Sleep duration, min | 443.24 ± 76.46 | 433.04 ± 82.21 | <.001 | 0.1287 |
| Sleep satisfaction, N (%) | <.001 | 0.0880 | ||
| Very enough | 1,591 (11.8) | 1,927 (15.5) | ||
| Enough | 3,182 (23.6) | 3,396 (27.3) | ||
| Mediocre | 4,681 (34.7) | 4,186 (33.6) | ||
| Not enough | 3,017 (22.4) | 2,263 (18.2) | ||
| Not enough at all | 1,019 (7.6) | 680 (5.5) | ||
| Females (Middle school), N | 12,732 | 11,692 | ||
| Time spent studying, min | 446.82 ± 233.70 | 417.27 ± 214.50 | <.001 | 0.1315 |
| Duration of internet or smartphone use, min | 162.35 ± 119.80 | 293.87 ± 183.71 | <.001 | 0.8554 |
| Sleep duration, min | 404.21 ± 81.00 | 394.49 ± 89.84 | <.001 | 0.1138 |
| Sleep satisfaction, N (%) | <.001 | 0.1399 | ||
| Very enough | 686 (5.4) | 1,102 (9.4) | ||
| Enough | 1,757 (13.8) | 2,288 (19.6) | ||
| Mediocre | 4,315 (33.9) | 4,133 (35.3) | ||
| Not enough | 4,090 (32.1) | 3,068 (26.2) | ||
| Not enough at all | 1,884 (14.8) | 1,101 (9.4) | ||
| Males (High school), N | 13,100 | 11,705 | ||
| Time spent studying, min | 480.85 ± 267.33 | 436.04 ± 247.72 | <.001 | 0.1735 |
| Duration of internet or smartphone use, min | 138.13 ± 108.05 | 262.21 ± 183.30 | <.001 | 0.8362 |
| Sleep duration, min | 352.46 ± 74.37 | 350.16 ± 75.92 | .016 | 0.0306 |
| Sleep satisfaction, N (%) | <.001 | 0.1250 | ||
| Very enough | 700 (5.3) | 957 (8.20) | ||
| Enough | 1,816 (13.9) | 2,257 (19.3) | ||
| Mediocre | 4,525 (34.5) | 4,245 (36.3) | ||
| Not enough | 3,958 (30.2) | 3,057 (26.1) | ||
| Not enough at all | 2,101 (16.0) | 1,189 (10.2) | ||
| Females (High school), N | 12,329 | 10,626 | ||
| Time spent studying, min | 572.65 ± 240.61 | 491.94 ± 230.29 | <.001 | 0.3422 |
| Duration of internet or smartphone use, min | 148.11 ± 107.18 | 304.02 ± 189.41 | <.001 | 1.0331 |
| Sleep duration, min | 325.90 ± 76.16 | 323.69 ± 78.66 | .031 | 0.0286 |
| Sleep satisfaction, N (%) | <.001 | 0.1893 | ||
| Very enough | 391 (3.2) | 662 (6.2) | ||
| Enough | 1,078 (8.7) | 1,732 (16.3) | ||
| Mediocre | 3,343 (27.1) | 3,451 (32.5) | ||
| Not enough | 4,344 (35.2) | 3,230 (30.4) | ||
| Not enough at all | 3,173 (25.7) | 1,551 (14.6) |
Each number is presented as mean ± standard deviation or sample size (ratio by group). The effect size is represented by the index w and Hedges' g.
Changes in mental health status (by school level and sex)
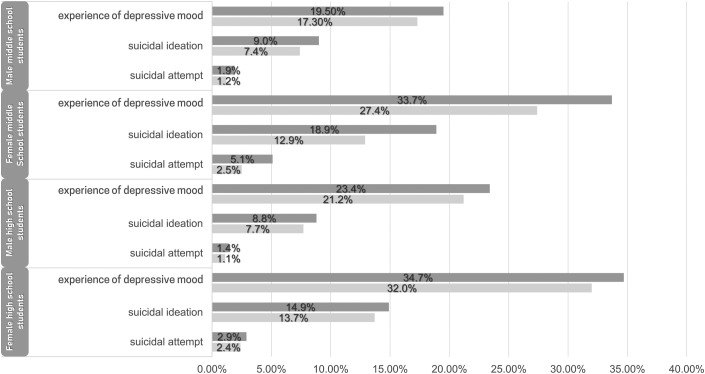
In 2020, the perceived stress level of adolescents decreased significantly compared with that of adolescents in 2019. The percentage of students who reported being stressed, with “very much” or “a lot”, decreased from 39.6% to 33.3%. Similarly, the percentage of students who experienced depressive mood decreased from 27.6% to 24.2%, which was statistically significant (males from 5,697 [21.4%] to 4,639 [19.2%] and females from 8,569 [34.2%] to 6,612 [29.6%]). Female adolescents were more likely to report experiencing depressive mood, suicidal ideation, and suicide attempts than their male counterparts in both 2019 and 2020. Experiences of depressive mood, suicidal ideation, and suicide attempts decreased in all groups during the pandemic. This change pattern was more pronounced in females than in males and in middle school students than in high school students. The mental health status of female middle school students was the most affected by the COVID-19 pandemic in groups separated by sex and age (Table 3 and Figure 1 ).
Table 3.
Comparison of the mental health status of students in 2019 and 2020
| Variables | 2019(n: 51,651) | 2020 (n: 46,475) | t or χ2 | p value | Effect size |
|---|---|---|---|---|---|
| Perceived stress, N (%) | 576.461 | <.001 | 0.0767 | ||
| Very much | 5,908 (11.4) | 3,631 (7.8) | |||
| A lot | 14,547 (28.2) | 11,848 (25.5) | |||
| A little | 21,244 (41.4) | 20,856 (44.9) | |||
| Not much | 8,044 (15.6) | 8,459 (18.2) | |||
| Not at all | 1,908 (3.7) | 1,681 (3.6) | |||
| Depressive mood, yes, N (%) | 14,266 (27.6) | 11,251 (24.2) | 147.943 | <.001 | 0.0388 |
| Suicidal ideation, yes, N (%) | 6,621 (12.8) | 4,789 (10.3) | 150.494 | <.001 | 0.0392 |
| Suicidal attempt, yes, N (%) | 1,447 (2.8) | 828 (1.8) | 112.360 | <.001 | 0.0338 |
Each number is presented as the sample size (ratio by group). The effect size is represented as an index w.
Figure 1.
Changes in mental health status by school level and sex: In all four groups divided by sex and school level, the percentage of experience of depressive mood, suicidal ideation, and suicide attempts all decreased. (dark gray bar: 2019 and light gray bar: 2020).
Logistic regression analyses of factors associated with experience of depressive mood
In a regression analysis that included all variables except subjective stress level, students who participated in the 2020 survey during the COVID-19 pandemic had a lower risk of experiencing depressive moods than those who participated in the 2019 survey. High school students had a lower risk of experiencing depressive mood than middle school students, but the risk increased for third graders in high school. High sleep satisfaction, longer sleep duration, perceived upper academic achievement, being healthy, and regular breakfast habits were rated as factors that lowered the risk of experiencing depressive mood. However, female sex, smoking, alcohol drinking, sexual behavior, violence, and frequent physical activity were found to increase the risk. The group that perceived themselves as skinny showed a higher risk of experiencing depressive mood. The group that answered that the perceived household economic status was moderate had the lowest risk, and the group that reported lower economic status was the most at risk. Similar results were found in the regression analysis when including all variables; detailed information is provided in Table S3.
Discussion
Previous studies have suggested that the COVID-19 pandemic has a negative impact on adolescent mental health [9,16,20]; however, unlike previous studies and our a priori hypothesis, the opposite result was found in Korean adolescents [20]. Our results suggest that students' mental health improved during the COVID-19 pandemic. In a previous study using KYRBS data from 2006 to 2018, experience of depressive mood and suicidal ideation/attempts showed a decreasing trend until 2015, and then showed an increasing trend from 2016 to 2018 (experience of depressive mood: 27.0%, suicidal ideation: 13.3%, and suicide attempt: 3.1% in 2018) [21]. Our results showed that this trend continued until 2019, and the subjective stress level, experience of depressive mood, suicidal ideation, and suicide attempts among Korean adolescents during the COVID-19 pandemic decreased.
We speculated that these results may be related to the following factors. First, changes in daily life due to school closures may affect mental health. In Korea, adolescents experience the burden and pressure of schoolwork, spend a lot of time at school, and are under high pressure to enter a university, which is strongly related to depression and anxiety [22,23]. The implementation of closure of schools and private educational institutions may have affected the perceived stress level during the pandemic. Adolescents were temporarily relieved of the burden of school activities and academic achievement. Furthermore, adolescents with high interpersonal anxiety have a temporary reduced risk of experiencing stressful events during school closure [24]. Interpersonal sensitivity is associated with depression and is higher in females [25]. For this reason, the decrease in the experience of depressive mood, suicidal thoughts, and suicide attempts was more noticeable in females than in males. The likely decline in school violence and bullying may have also had a positive effect on adolescents. Second, physical activity in adolescents is known to lower the risk of developing depressive disorders [26]; however, our results showed that frequent physical activity was associated with experiencing depressive mood. In a previous study, we reported similar results and suggested that appropriate Internet use during the weekend was associated with a lower risk of experiencing depressive mood, which may be related to the culture of leisure in Korean adolescents [27]. Third, the introduction of the online class system may have minimized negative changes in students' daily lives due to the pandemic. Experts are concerned about school closures disrupting students' daily lives and worsening their mental health [16,28]. In Korea, online classes began in April 2020, and school teachers contacted students and their parents to ensure that all students attended the class. These measures helped students maintain their daily lives. Fourth, at the time of the 2020 KYRBS investigation, several studies had reported that adolescents tend to have a mild course of COVID-19 with a better prognosis than adults [29,30]. These findings may have helped adolescents reduce their anxiety and worry about infection, which may have affected the results.
These results should be interpreted with caution. As participants were asked to provide responses about their mental health status and suicidal ideation and attempts in the past year, the non-pandemic period was also included and for some participants, this may have may have included a period of 5 months before the pandemic. In Korea, from April to July during the 2020 survey period, the number of confirmed cases of COVID-19 was relatively stable at <100. Therefore, our results may reflect the mental health status of adolescents during the early phase of the COVID-19 pandemic. During this period, students were temporarily free from the pressures of academic achievement and interpersonal stress, which may have effected their mental health. However, as students return to school, they may experience depression/anxiety or an increase in stress [31,32].
This study has some limitations. First, we did not determine the type of physical activity and the spontaneity of the individual and their preference for physical activity. There is a possibility that students who perform physical labor in part-time jobs or students who exercise to become professional athletes are included, and for these students, physical activity may be associated with poor mental health. Second, although students reported that they had subjectively experienced a period of sadness or desperate times, depressive symptoms or symptoms severity was not assessed, and a clinical diagnosis of depressive disorder by a clinician was not obtained. Standardized scales for suicidal ideation or attempts were not used. Therefore, our results have limited interpretability with respect to the changes in the severity and prevalence of depressive disorders. Third, instead of using objective measures of variables such as individual health status and academic achievement, participants were asked to provide subjective perceptions. A previous study reported that subjective social status, which refers to where individuals believe they rank in a social hierarchy, is related to mental disorders [33]. In this study, subjective social status was correlated with family income, an absolute socioeconomic status (SES) measure, and was suggested as the SES indicator that was most consistently related to mental health. Fourth, gender diversity was not evaluated in the KYRBS; hence, we were unable to confirm the impact of the pandemic on adolescents' gender diversity. In a previous study, Hawke et al. [34] suggested that transgender and gender-diverse adolescents were more negatively affected by their mental health during the COVID-19 pandemic. Fifth, unlike the 2019 KYRBS, the 2020 KYRBS was surveyed from August to November. Different timings may have affected the stress levels. Sixth, school type was not controlled in the logistic regression analyses. According to the characteristics of the school type, such as public high school and private high school, school climates and academic pressures on students differ, which can affect their mental health. However, there is a limit to confirming the effects of these characteristics using KYRBS data. Furthermore, we were unable to consider other aspects of family SES such as parental nationality, education level, or occupation. Future research is needed that includes not only each adolescent's individual information, but also their family information.
Nevertheless, the strengths of this study include the evaluation of lifestyle factors and mental health status of adolescents before and after the onset of the COVID-19 pandemic. To the best of our knowledge, this is the first comparison of information on perceived stress, experience of depressive mood, and suicidal ideation and attempts among adolescents sampled across South Korea, both before and during the COVID-19 pandemic. We evaluated the changes in daily life and the emotional status of adolescents due to the COVID-19 pandemic. During the pandemic, factors such as a decrease in outside activities/study time, changes in sleeping habits, subjective body perception, and academic achievement have affected the mental health of adolescents. Our results showed that perceived stress and the risk of experiencing depressive mood and suicidal ideation/attempts were reduced temporarily during the pandemic, and this was more pronounced in women than in men. As the COVID-19 pandemic continues in Korea, and schools are alternately conducting face-to-face and online classes, adolescents may experience increased mental health problems as they return to school. Thus, school policymakers and parents should focus their attention to the mental health needs of students during the readjustment period.
Footnotes
Conflicts of interest: The authors have no conflicts of interest to disclose.
Supplementary data related to this article can be found at https://doi.org/10.1016/j.jadohealth.2022.05.020.
Funding Sources
This study was supported by the National Research Foundation (NRF-2020R1A2C1008072) of the Republic of Korea. The funder had no role in the design or conduct of the study, including in the decision to submit the article for publication.
Supplementary Data
References
- 1.Huang C., Wang Y., Li X., et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization . 2020. COVID-19 weekly epidemiological update.https://www.who.int/publications/m/item/weekly-epidemiological Available at: [Google Scholar]
- 3.Shim E., Tariq A., Choi W., et al. Transmission potential and severity of COVID-19 in South Korea. Int J Infect Dis. 2020;93:339–344. doi: 10.1016/j.ijid.2020.03.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jiao W.Y., Wang L.N., Liu J., et al. Behavioral and emotional disorders in children during the COVID-19 epidemic. J Pediatr. 2020;221:264–266.e1. doi: 10.1016/j.jpeds.2020.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lee H.S., Dean D., Baxter T., et al. Deterioration of mental health despite successful control of the COVID-19 pandemic in South Korea. Psychiatry Res. 2021;295:113570. doi: 10.1016/j.psychres.2020.113570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Guessoum S.B., Lachal J., Radjack R., et al. Adolescent psychiatric disorders during the COVID-19 pandemic and lockdown. Psychiatry Res. 2020;291:113264. doi: 10.1016/j.psychres.2020.113264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rossi R., Socci V., Talevi D., et al. COVID-19 pandemic and lockdown measures impact on mental health among the general population in Italy. Front Psychiatry. 2020;11:790. doi: 10.3389/fpsyt.2020.00790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Vindegaard N., Benros M.E. COVID-19 pandemic and mental health consequences: Systematic review of the current evidence. Brain Behav Immun. 2020;89:531–542. doi: 10.1016/j.bbi.2020.05.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Racine N., Cooke J.E., Eirich R., et al. Child and adolescent mental illness during COVID-19: A rapid review. Psychiatry Res. 2020;292:113307. doi: 10.1016/j.psychres.2020.113307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Crocetti E. Identity formation in adolescence: The dynamic of forming and consolidating identity commitments. Child Dev Perspect. 2017;11:145–150. [Google Scholar]
- 11.Steinberg L., Morris A.S. Adolescent development. Annu Rev Psychol. 2001;52:83–110. doi: 10.1146/annurev.psych.52.1.83. [DOI] [PubMed] [Google Scholar]
- 12.Casey B.J., Heller A.S., Gee D.G., Cohen A.O. Development of the emotional brain. Neurosci Lett. 2019;693:29–34. doi: 10.1016/j.neulet.2017.11.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lee F.S., Heimer H., Giedd J.N., et al. Adolescent mental health—opportunity and obligation. Science. 2014;346:547–549. doi: 10.1126/science.1260497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Thapar A., Collishaw S., Pine D.S., Thapar A.K. Depression in adolescence. Lancet. 2012;379:1056–1067. doi: 10.1016/S0140-6736(11)60871-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chen H., Cohen P., Kasen S., et al. Impact of adolescent mental disorders and physical illnesses on quality of life 17 years later. Arch Pediatr Adolesc Med. 2006;160:93–99. doi: 10.1001/archpedi.160.1.93. [DOI] [PubMed] [Google Scholar]
- 16.Lee J. Mental health effects of school closures during COVID-19. Lancet Child Adolesc Health. 2020;4:421. doi: 10.1016/S2352-4642(20)30109-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kim Y., Choi S., Chun C., et al. Data resource profile: The Korea youth risk behavior web-based survey (KYRBS) Int J Epidemiol. 2016;45:1076. doi: 10.1093/ije/dyw070. 1076e. [DOI] [PubMed] [Google Scholar]
- 18.Williams J.W., Jr., Mulrow C.D., Kroenke K., et al. Case-finding for depression in primary care: A randomized trial. Am J Med. 1999;106:36–43. doi: 10.1016/s0002-9343(98)00371-4. [DOI] [PubMed] [Google Scholar]
- 19.Löwe B., Kroenke K., Gräfe K. Detecting and monitoring depression with a two-item questionnaire (PHQ-2) J Psychosom Res. 2005;58:163–171. doi: 10.1016/j.jpsychores.2004.09.006. [DOI] [PubMed] [Google Scholar]
- 20.Collier Villaume S.C., Stephens J.E., Nwafor E.E., et al. High parental education protects against changes in adolescent stress and mood early in the COVID-19 pandemic. J Adolesc Health. 2021;69:549–556. doi: 10.1016/j.jadohealth.2021.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kim K.M., Kim D., Chung U.S. Investigation of the trend in adolescent mental health and its related social factors: A multi-year cross-sectional study for 13 years. Int J Environ Res Public Health. 2020;17:5405. doi: 10.3390/ijerph17155405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kim K.M. What makes adolescents psychologically distressed? Life events as risk factors for depression and suicide. Eur Child Adolesc Psychiatry. 2021;30:359–367. doi: 10.1007/s00787-020-01520-9. [DOI] [PubMed] [Google Scholar]
- 23.Won K., Lee H. Academic stress and suicidal ideation: The mediating effects of school connectedness, depression and anxiety in adolescents. Korean J Youth Stud. 2019;26:79–104. [Google Scholar]
- 24.Morrissette M. School closures and social anxiety during the COVID-19 pandemic. J Am Acad Child Adolesc Psychiatry. 2021;60:6. doi: 10.1016/j.jaac.2020.08.436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rudolph K.D. Gender differences in emotional responses to interpersonal stress during adolescence. J Adolesc Health. 2002;30(suppl):3–13. doi: 10.1016/s1054-139x(01)00383-4. [DOI] [PubMed] [Google Scholar]
- 26.McDowell C.P., MacDonncha C., Herring M.P. Brief report: Associations of physical activity with anxiety and depression symptoms and status among adolescents. J Adolesc. 2017;55:1–4. doi: 10.1016/j.adolescence.2016.12.004. [DOI] [PubMed] [Google Scholar]
- 27.Lee J., Han C., Ko Y.H., et al. Assessment of life factors affecting the experience of depressive symptoms in adolescents: A secondary analysis using the Korea youth risk behavior survey. Child Adolesc Psychiatry Ment Health. 2021;15:50. doi: 10.1186/s13034-021-00407-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bahn G.H. Coronavirus disease 2019, school closures, and children’s mental health. J Korean Acad Child Adolesc Psychiatry. 2020;31:74–79. doi: 10.5765/jkacap.200010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mantovani A., Rinaldi E., Zusi C., et al. Coronavirus disease 2019 (COVID-19) in children and/or adolescents: A meta-analysis. Pediatr Res. 2021;89:733–737. doi: 10.1038/s41390-020-1015-2. [DOI] [PubMed] [Google Scholar]
- 30.Wang D., Ju X.L., Xie F., et al. Clinical analysis of 31 cases of 2019 novel coronavirus infection in children from six provinces (autonomous region) of Northern China. Zhong hua er ke za zhi. 2020;58:269–274. doi: 10.3760/cma.j.cn112140-20200225-00138. [DOI] [PubMed] [Google Scholar]
- 31.Karaman M.A., Eşici H., Tomar İ.H., Aliyev R. COVID-19: Are school counseling services ready? Students’ psychological symptoms, school counselors’ views, and solutions. Front Psychol. 2021;12:647740. doi: 10.3389/fpsyg.2021.647740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zhang L., Zhang D., Fang J., et al. Assessment of mental health of Chinese primary school students before and after school closing and opening during the COVID-19 pandemic. JAMA Netw Open. 2020;3 doi: 10.1001/jamanetworkopen.2020.21482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.McLaughlin K.A., Costello E.J., Leblanc W., et al. Socioeconomic status and adolescent mental disorders. Am J Public Health. 2012;102:1742–1750. doi: 10.2105/AJPH.2011.300477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hawke L.D., Hayes E., Darnay K., Henderson J. Mental health among transgender and gender diverse youth: An exploration of effects during the COVID-19 pandemic. Psychol Sex Orient Gend Divers. 2021;8:180–187. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.