Figure 1. Regional versus systemic delivery of CAR T cells.
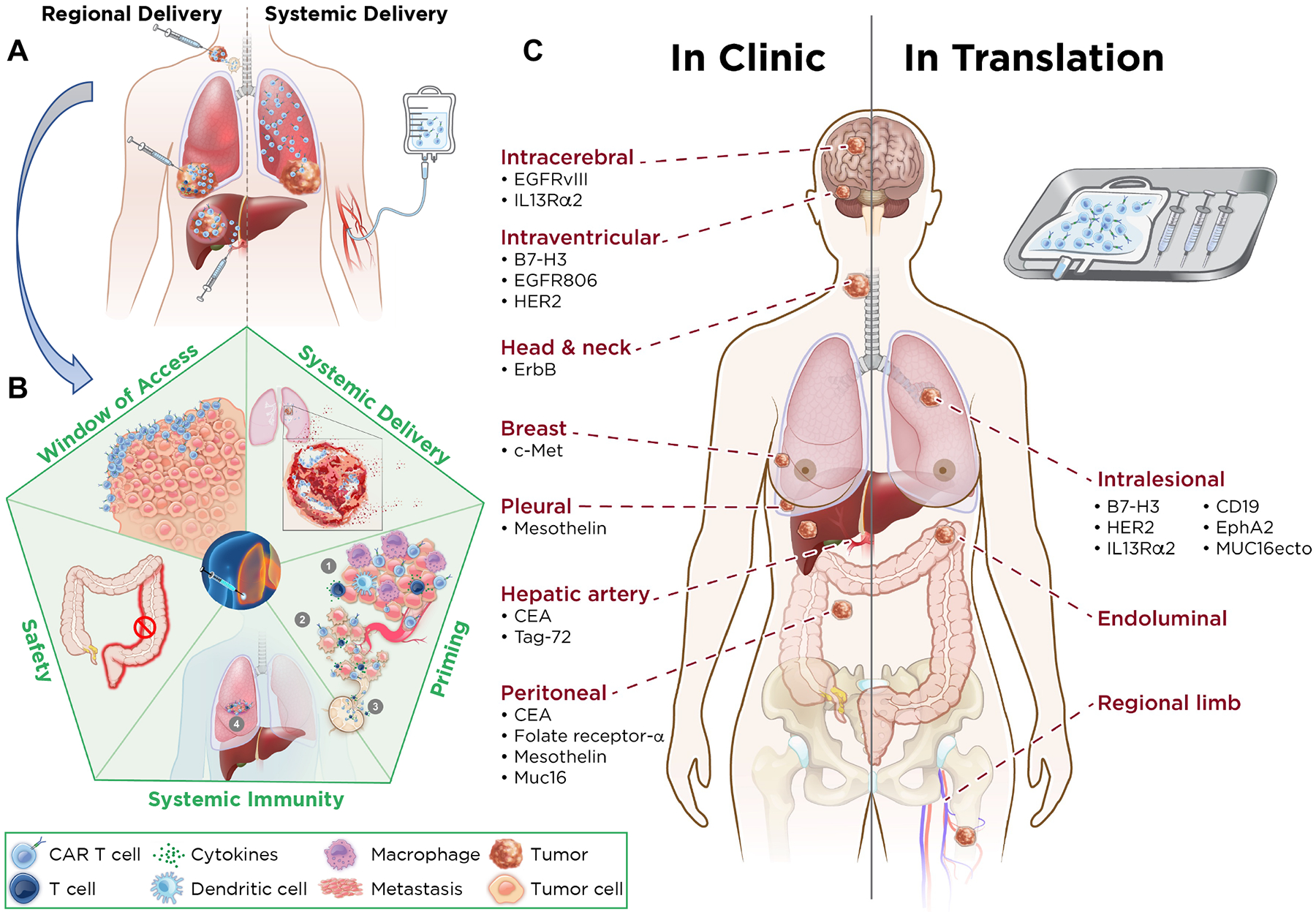
A. Characteristics of CAR T cells delivered regionally versus systemically. Regional delivery allows for increased intratumoral proliferation of CAR T cells, increased depth of penetration of CAR T cells, augmentation of CD4 help, immune balance, greater trafficking to site(s) of metastasis, and drainage to lymph nodes. Systemic delivery results in sequestration of CAR T cells in the lung, with shallow penetration into the tumor, no CD4 help, and little effect on metastatic site(s). B. Advantages of regional administration of CAR T cells. Regional delivery acts as a window of access for CAR T cells to generate systemic immunity and enter metastatic site(s) better, results in tumor lysis, and primes the environment for systemic immunity via the induction of tumor immune microenvironment changes, including decreased immune suppression via effector response in the tumor microenvironment, increased tumor cell death leading to strong immune response (via release of neoantigens that are drained to regional lymph nodes), increased susceptibility of tumor blood vessels to immune cell traffic, and increased T cell circulation and entry into metastatic sites. Regional delivery generates a local immune response that results in a long-lasting circulating T-cell immunity to eliminate systemic disease and prevent tumor recurrence and avoids systemic toxicity—that is, there is no colitis when CAR T cells are delivered intrahepatically. C. Comparing regional therapy modalities in clinic and in translation. Regional therapy is currently being administered for intracerebral, intraventricular, head and neck, breast, pleural, hepatic (via the hepatic artery), and peritoneal tumors. For each tumor type, the relative CAR target is highlighted (Left). CAR T cell targets in translation by intralesional administration are listed. Potential other routes of administration are endoluminal and regional limb infusion (Right).
