Abstract
Purpose:
To describe maximal and submaximal cardiorespiratory fitness from early adulthood to midlife and examine differences in maximal fitness at age 20 and changes in fitness over-time by sub-categories of socio-demographic, behavioral, and health-related factors.
Methods:
Data include 5,018 Coronary Artery Risk Development in Young Adults participants [mean (SD) age 24.8 (3.7) years, 53.3% female and 51.4% Black participants] who completed at least one maximal graded exercise test at baseline and/or the Year 7 and 20 exams. Maximal and submaximal fitness were estimated by exercise duration and heart rate at the end of stage 2. Multivariable adjusted linear mixed models were used to estimate fitness trajectories using age as the mechanism for time after adjustment for covariates. Fitness trajectories from ages 20 to 50 in 5-year increments were estimated overall and by sub-groups determined by each factor after adjustment for duration within the less favorable category.
Results:
Mean (95% confidence interval) maximal fitness at age 20 and 50 years was 613 (607, 616) and 357 (350, 362) seconds; submaximal heart rate during this period also reflected age-related fitness declines [126 (125, 127) and 138 (137, 138) beats per minute]. Compared to men, women had lower maximal fitness at age 20 (p<0.001), which persisted over follow-up (p<0.001); differences were also found by race within sex-strata (all p<0.001). Differences in maximal fitness at age 20 were noted by socio-economic, behavioral, and health-related status in young adulthood (all p<0.05), which persisted over follow-up (all p<0.001) and were generally consistent in sex-stratified analyses.
Conclusions:
Targeting individuals experiencing accelerated fitness declines with tailored intervention strategies may provide an opportunity to preserve fitness throughout midlife to reduce lifetime cardiovascular disease risk.
Keywords: EXERCISE TEST, FOLLOW-UP STUDIES, YOUNG ADULT, MIDDLE LIFE
INTRODUCTION
Substantial evidence accumulated over the past several decades has informed the inverse association of cardiorespiratory fitness (henceforth: fitness) with risk of premature mortality and non-fatal and fatal cardiovascular disease (CVD) (1–9). Age-related declines in fitness have also been documented (10–17) and have been attributed to changes in heart structure and function that are mediated by reductions in cardiac output and/or arteriovenous oxygen difference (18). The association of age with fitness is further influenced by hereditary factors and underlying disease, as well as potentially modifiable risk factors including physical activity and body composition (12, 18).
However, much of the evidence cited for age-related declines in fitness comes from cross-sectional studies, which suggests a 5–10% lower fitness level per decade increase in age across adulthood (10–16). Evidence from longitudinal studies is significantly more limited and includes small, homogenous samples including endurance-trained athletes (19–25). A study by Fleg et al. (17) using the Baltimore Longitudinal Study of Aging (BLSA) cohort expanded this evidence by documenting age-related declines in a population-based sample and found that the rate of decline in peak oxygen uptake (VO2) ranged from 3–6% per decade in the second and third decade of life to 20% per decade in the seventh decade and beyond. Study findings also suggested that the rate of decline per decade was higher in men than women after the fourth decade (17). Similar to prior work, the BLSA sample was largely homogeneous; primarily comprised of White and affluent participants. Additional limitations of prior longitudinal studies documenting age-related declines in fitness include relatively short follow-up periods and limited assessments (<10 years; n≈2 assessments), which is not ideal given adulthood lasts several decades (17, 24).
Given the importance of fitness across the life course to optimize cardiovascular health, additional research is also needed to examine early adult factors that are associated with lower concurrent fitness and accelerated age-related fitness declines. Early adulthood may be a particularly important period of the life-course given it is when a greater appreciation of, and value is placed on, healthy lifestyle behaviors (26), but it is also when there is a perception of invincibility to future risk of disease (27). Early adulthood is also a period when a number of important life events occur that can potentially impact intentions to engage in healthy lifestyle behaviors (28). Given potential differences in fitness by sex (29), it is also important to examine the role of socio-economic, behavioral, and health-related factors on age-related declines in fitness in women and men, separately.
To address these research gaps, we leverage Coronary Artery Risk Development in Young Adults (CARDIA), a diverse and well-characterized prospective cohort study that conducted a symptom-limited graded exercise treadmill test (GXT) protocol at baseline and year 7 and 20 follow-up exams. The objectives of this study are to: 1) describe maximal and submaximal fitness from early adulthood to midlife and 2) examine differences in estimated maximal fitness at age 20 and changes in fitness through midlife by sub-categories of socio-demographic, behavioral, and health-related factors in the entire cohort and by sex.
METHODS
Design Overview and Study Participants
The CARDIA cohort includes 5,115 adults aged 18 to 30 years enrolled at baseline (1985–86) at four clinics across the United States (U.S.), including Birmingham, Alabama; Chicago, Illinois; Minneapolis, Minnesota, and Oakland, California, to provide approximately equal representation within each clinic by race (Black or White), sex (male or female), age (18–24 or 25–30 years), and education (high school or less or more than high school). Community-based sampling was performed at three clinics (Birmingham, Chicago, and Minneapolis), while Oakland participants were sampled from the membership of a large integrated health care program (Kaiser Permanente Northern California). Approximately 50% of those invited were successfully enrolled. Participants have been re-examined approximately every 2 to 5 years. At the year 20 follow-up exam (2005–06), 72% of the surviving cohort was examined (30). All CARDIA participants provided informed consent at each examination and the institutional review boards at each participating center approve the study annually.
Data Collection
Standardized questionnaires and protocols were used to assess age and early adult factors associated with concurrent fitness levels and fitness change, which included socioeconomic (sex assigned at birth, self-defined race, education and financial strain), behavioral (physical activity, alcohol and tobacco use), and health-related [body mass index (BMI); based on measured height (m) and weight (kg) and self-rated health] factors. All data collection measures and protocols are publicly available through the CARDIA website (see Exam Materials under Scientific Resources) (30).
Factors associated with early adult fitness levels and fitness change from early adulthood through midlife were organized as time-invariant or time-varying measures and selected a priori based on literature review and/or biological plausibility for confounding the main associations of interest. Time-invariant measures included: sex assigned at birth (male or female), self-identified race (Black or White), and enrolling CARDIA clinic to account for U.S. regional differences. Time varying measures included: education [high school (or equivalent) degree or less or Associate’s degree or more), financial strain (difficulty paying for basics like food, medical care and heating: somewhat hard, hard, very hard or not very hard), physical activity (not meeting or meeting physical activity guidelines based on a threshold of <300 or ≥300 exercise units (i.e., unit of expression for summary estimates), respectively (31), as reported on the CARDIA Physical Activity Questionnaire), alcohol use (yes or no in the past year), tobacco use (former/current or never tobacco user), BMI [overweight/obese (≥25 kg/m2)] or underweight/normal (<25 kg/m2)] and self-rated health from the Short Form 12 Health Survey® (SF-12) (32) (poor/fair or good/excellent). Baseline measures were used to infer early adult factors associated with concurrent fitness and fitness change from early adulthood to midlife. To account for the effect of measures that could change during the 20 years of follow-up, the cumulative number of years classified within the less favorable category was estimated using data collected at the Year 0, 2, 5, 7, 10, 15, and 20 exams. Specifically, beginning with the baseline exam, each of the early adult factors were defined by the number of years a participant reported (or was): 1) having less than or equal to a high school degree or equivalent; 2) having it be at least somewhat hard to pay for basics; 3) not meeting physical activity guidelines; 4) using alcohol or tobacco products; 5) having overweight or obese; and/or 6) having fair or poor health.
Maximal Graded Exercise Test
The CARDIA GXT was designed to estimate maximal, symptom-limited performance and utilized a modified Balke protocol (33), consisting of up to nine 2-minute stages of increasing difficulty (increase in treadmill speed and/or grade), beginning at an estimated workload of 4.1 metabolic equivalent of task (MET)s and ending at 19.0 METs (34). The testing procedure at Years 0, 7, and 20 was identical and included the following components: screening for medical eligibility using American College of Sports Medicine criteria (35); participant preparation for electrocardiogram (ECG); resting (supine) 12-lead ECG; pre-exercise (standing) 3-lead ECG and blood pressure; exercise on the treadmill; recovery following exercise; and participant discharge. Participant disposition at each of the exams when the GXT was offered has been previously reported (36).
Resting heart rate [beats per minute (bpm)] was obtained as part of the core exam after sitting quietly at rest for five minutes. Pulse, blood pressure, and a 12-lead ECG were obtained on each participant at rest, and heart rate, blood pressure, and a three-lead ECG obtained during the last 30 seconds of each 2-minute stage, at peak effort (immediately prior to stopping), and every minute for 3 minutes post-exercise. A rating of perceived exertion (RPE; 6–20 scale) was obtained near the end of each stage and at maximal exercise (37).
Peak VO2, defined as the highest value of VO2 attained during a staged GXT (38), was used to estimate maximal fitness based on exercise duration on the treadmill (in seconds) among those achieving ≥85% of age-predicted maximal heart rate using the CARDIA formula, which considers the quadratic association of age with maximal heart rate (39). Submaximal fitness was estimated based on heart rate at the end of stage 2, with higher values indicative of lower submaximal fitness. The workload for stage 2 was: 3.4 mph treadmill speed, 6% grade or 6.4 METs. A protocol deviation occurred at one clinic during the Year 7 follow-up exam by allowing use of the treadmill handrails (39) during exercise, which resulted in inflated (longer) exercise duration estimates (i.e., maximal fitness indicator). The exercise duration values were corrected using a calibration equation that utilized information collected at the baseline and year 20 exams (see Supplemental Text, SDC 5). For these tests, a rating of perceived exertion threshold of ≥15 or “hard” (37), rather than 85% of age-predicated maximal heart rate, was used to infer maximal effort (85% age-predicted maximal heart rate for mean cohort age of 31 years at Year 7 = 150.8 bpm). A sensitivity analysis, excluding these tests (n=926) was conducted.
Statistical Analysis
Analyses were conducting using R version 4.0.1, and the code used to complete these analyses is publicly available at: https://github.com/bcjaeger/CARDIA---GXT-duration. Initial statistical analyses involved data cleaning, variable derivation, and a descriptive content analysis that included univariate summaries of primary analysis variables at the Year 0, 7, and 20 exams, overall and by groups defined by race and sex.
Linear mixed models were fit to estimate maximal and submaximal fitness over-time using age as the mechanism for time. The association of age with fitness indicators was modeled using restricted cubic splines with five knots at the 10th, 25th, 50th, 75th, and 90th age percentiles. All models included participant-specific random intercepts to account for correlation in repeated assessments and were adjusted for sex (in models including the entire cohort), race (in models not examining differences by race), education, and CARDIA clinic. Models were further adjusted for sociodemographic, behavioral, and health-related factors that may influence maximal fitness at baseline and during the follow-up. Factors influencing maximal fitness during the follow-up period included the cumulative number of years within the less favorable category. To assess whether there was a difference in maximal fitness over follow-up, we tested for interaction between age and each factor listed above. All models were fitted to the entire cohort and to male and female participants, separately.
The percent change in fitness for each successive 5-year increment was also calculated using estimated maximal and submaximal fitness by race within sex strata [(mean fitness at given 5-year age increment – mean fitness at immediately prior age increment) / mean fitness at immediately prior age increment * 100]. Five-year, rather than 10-year (17), increments were used to provide more granular estimates of fitness change during this important life-course transition. We also estimated the difference in fitness between sub-groups determined by baseline status of sociodemographic, behavioral, and health-related factors. These differences were estimated from age 20 to 50 in 5-year increments. Bootstrap resampling was applied to generate 95% confidence intervals (CI) for the differences in estimated fitness described above.
The count and proportion of missing values was examined overall, by exam, and by race and sex groups. Based on these data, we assumed the primary analysis variables were missing at random and conducted multiple imputation to obtain valid standard errors for statistical inference. Multiple imputation with chained equations was applied, accounting for the longitudinal design of the study. Five imputed datasets were formed by fitting a random forest to each variable with missing data, separately, and then performing predictive mean matching.
As the current analysis jointly performed multiple imputation and bootstrapping, recommendations of Schomaker et al. (40) were followed to obtain bootstrapped CIs that incorporate uncertainty from missing values. That is, we imputed five datasets using each bootstrapped replicate of the current study’s data and formed bootstrapped distributions of model estimates using the pooled estimates from the multiple imputed data.
RESULTS
The analytic sample included 5,018 CARDIA participants who completed the GXT protocol at least once (n=11,108 tests), did not use beta blocker medications at the time of the GXT, and achieved ≥85% of their age-predicted maximal heart rate (Figure 1) (39). Table 1 shows the baseline characteristics of the entire analytic sample and after stratification by race and sex. Mean [standard deviation (SD)] age and BMI were 24.8 (3.7) years and 24.5 (5.0) kg/m2, respectively, and most were women (53.3%) and identified as Black (51.4%). Black men and White women had the highest and lowest proportion of less than or equal to a high school degree or equivalent (82% and 52%, respectively). Black and White men also had the highest and lowest proportion of financial strain (41% and 27%, respectively) and current tobacco use (37% and 27%, respectively). Black women and White men had the lowest and highest proportion of meeting physical activity guidelines (37% and 73%, respectively) and alcohol use (78% and 92%, respectively). Black and White women also had the highest and lowest proportion of fair or poor health status (16% and 6%, respectively).
Figure 1.

The number of participants, and graded exercise tests at each timepoint, available for analysis with each exclusion applied.
Table 1.
| Characteristic | Overall | Black Women | Black Men | White Women | White Men |
|---|---|---|---|---|---|
| No. of participants | 4,924 | 1,415 | 1,117 | 1,258 | 1,134 |
| Testing center, % | |||||
| Birmingham | 23 | 25 | 26 | 20 | 23 |
| Chicago | 22 | 22 | 21 | 22 | 24 |
| Minnesota | 27 | 21 | 26 | 31 | 32 |
| Oakland | 28 | 33 | 28 | 27 | 21 |
| Age, years‡ | 24.8 (3.7) | 24.4 (3.9) | 24.2 (3.7) | 25.4 (3.4) | 25.4 (3.4) |
| Maximum Education by Year 20, % | |||||
| Associate’s Degree or more | 32 | 20 | 18 | 48 | 46 |
| High school or less | 68 | 80 | 82 | 52 | 54 |
| Difficulty paying for basics, % | |||||
| Not very hard | 65 | 61 | 59 | 68 | 73 |
| ≥Somewhat hard | 35 | 39 | 41 | 32 | 27 |
| Marital status, % | |||||
| Married or cohabitating | 22 | 20 | 18 | 28 | 23 |
| Other | 78 | 80 | 82 | 72 | 77 |
| Meeting Physical Activity Guidelines, % | |||||
| Yes | 59 | 37 | 72 | 58 | 73 |
| No | 41 | 63 | 28 | 42 | 27 |
| Alcohol use, % | |||||
| Yes | 86 | 78 | 85 | 91 | 92 |
| No | 14 | 22 | 15 | 9.2 | 7.7 |
| Smoking status, % | |||||
| Never smoked | 57 | 60 | 54 | 53 | 58 |
| former | 13 | 8.4 | 9.1 | 20 | 16 |
| current | 30 | 31 | 37 | 27 | 26 |
| Body mass index, kg/m2‡ | 24.5 (5.0) | 25.8 (6.4) | 24.5 (4.2) | 23.0 (4.3) | 24.3 (3.5) |
| Self-rated health, % | |||||
| ≥Good | 90 | 84 | 89 | 94 | 94 |
| ≤Fair | 10.0 | 16 | 11 | 6.0 | 6.4 |
Data are from the baseline exam unless otherwise noted.
Baseline data are not represented for 94 participants (1.9% of analytic sample) who did not complete the graded exercise test at the baseline exam but did complete the protocol at the Year 7 and/or Year 20 follow-up exams.
Mean (standard deviation)
Mean (95% CI) estimated maximal fitness at age 20 years was 613 (607, 616) seconds, which decreased to 357 (350, 362) seconds at age 50. These age-related declines in fitness were consistent when considering mean (95% CI) estimated heart rate at the end of stage 2 which ranged from 126 (125, 127) to 138 bpm (137, 138) bpm. Both maximal and submaximal fitness indicators supported significantly higher estimated fitness at age 20 in men compared with women [736 (732, 743) and 510 (501, 516) seconds, respectively, and 113 (112, 114) and 137 (135, 138) bpm, respectively; both p<0.001]. While men had higher fitness levels than women through age 50 years (both p<0.001), the estimated differences attenuated over-time [435 (426, 441) and 292 (283, 297) seconds at age 50, respectively, and 127 (126, 128) and 147 (145, 148) bpm at age 50, respectively].
When comparing differences by race within sex-strata (Figure 2; Supplemental Table 1, SDC 1), Black woman had lower estimated maximal fitness levels at age 20 and the rate of 5-year fitness decline ranged from −6.4% (ages 20 to 25) to −10% per 5-year age increment through age 50 years compared with a more attenuated range of maximal fitness decline from −0.8% to −10% in White women. Black men had lower estimated maximal fitness levels at age 20 than White men and these differences increased over-time [Black men: −6.9% (ages 20–25) to −11% per 5-year age increment through age 50 years; White men: −4.2% to −8.2%]. Among women, estimated submaximal fitness at age 20 did not significantly differ by race (p=0.48); however, the rate of increase in heart rate at the end of stage 2 was higher in Black compared with White women (p<0.001). In men, estimated submaximal fitness at age 20 was higher in Black men compared with White men (p=0.008). However, differences in estimated submaximal fitness by race were not statistically supported at age 25. At each 5-year increment from age 30 and beyond, estimated submaximal fitness was lower in Black men compared with White men (p for differences in estimated submaximal fitness over follow-up <0.001).
Figure 2.
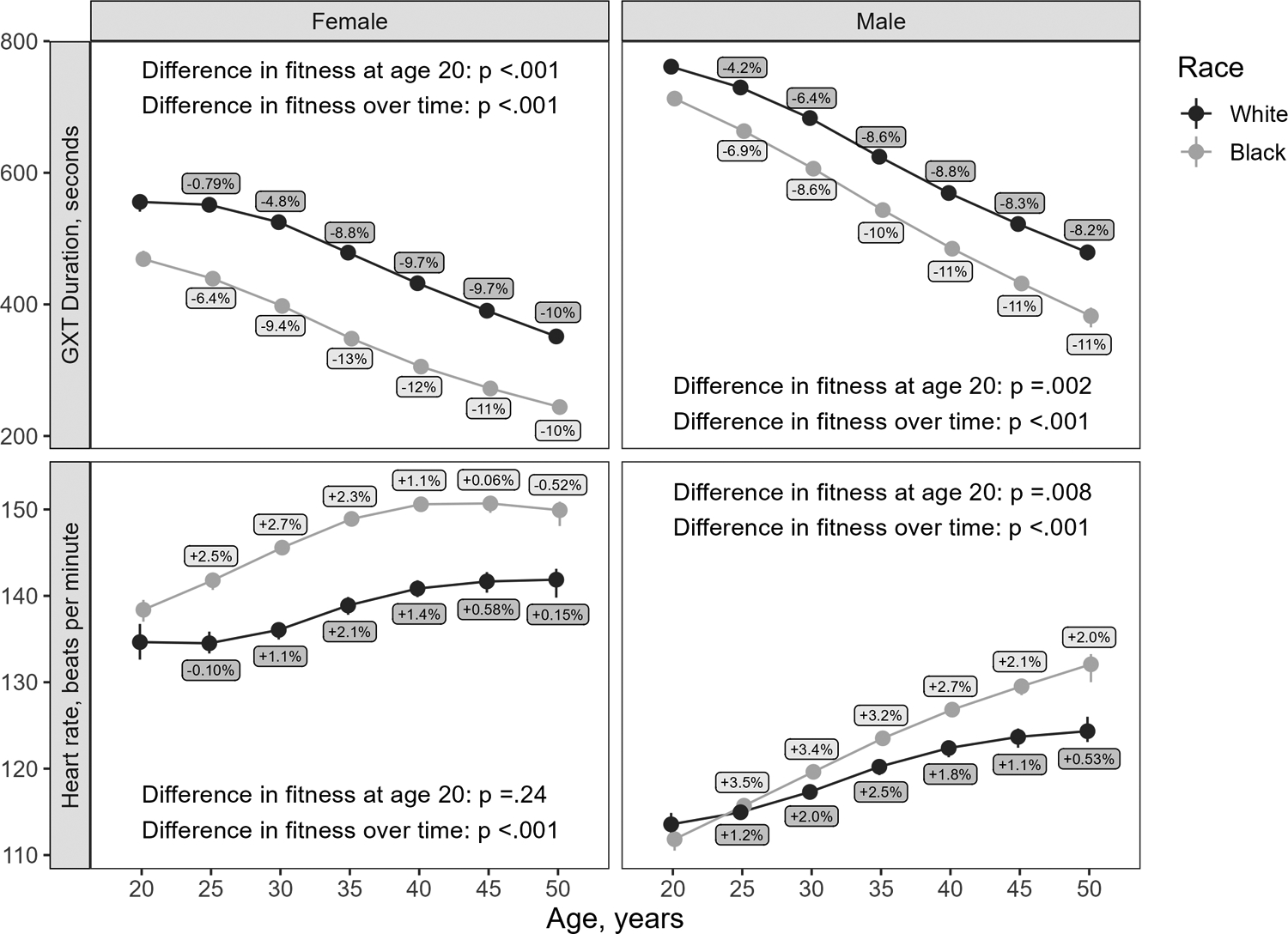
Estimated graded exercise test duration (top row) and heart rate at the end of stage 2 (bottom row) for female (left column) and male (right column) participants with respect to age in years. Point estimates are adjusted for education and field center. Interval estimates indicate 95% confidence intervals. Differences in fitness were estimated from age 20 to 50 in 5-year increments by race within sex strata.
Supplemental Table 2, SDC 2, shows the differences in estimated maximal fitness at age 20 and changes in fitness over-time by sub-categories of socio-demographic, behavioral, and health-related factors in the overall cohort. After multi-variable adjustment, maximal fitness levels at age 20 were lower in those with less education, with more difficulty paying for basics, not physically active, no alcohol use, former or current smokers, having overweight or obese, and in fair or poor self-rated health (all p<0.05). Similarly, differences in age-related declines in fitness were noted over the follow-up period by sub-categories of education, financial strain, physical activity, alcohol use, smoking status, weight status, and self-rated health (all p<0.001). Of note, differences in age-related declines in fitness by sub-categories of alcohol use attenuated and reversed direction after age 45 with those not consuming alcohol having higher estimated maximal fitness levels than those reporting alcohol use when considering the cumulative number of years reporting alcohol use.
Results were largely consistent in sex-stratified analysis, with a few differences noted. Specifically, among women (Supplemental Table 3, SDC 3), there was no evidence for a difference in estimated maximal fitness at age 20 by baseline category of financial strain or smoking status [−7.7 (−19.0, 3.1) and 19 (8.9, 34) seconds, respectively]. Also, there was a lack of evidence for a difference in fitness over-time by alcohol status. While there was a lack of evidence that estimated fitness at age 20 differed by education or alcohol consumption in men [−25 (−47, −9.9) and 8.5 (−6.1, 26.0) seconds, respectively; Supplemental Table 4, SDC 4), changes in fitness over-time differed by these factors (both p<0.001).
Sensitivity Analysis
After excluding tests (n=926) subject to the protocol deviation at Year 7, the estimates and interpretations did not vary substantially; therefore, the corrected maximal fitness estimates obtained from this clinic were included in primary analysis (results available upon request).
DISCUSSION
Optimizing cardiorespiratory fitness across the life-course, despite age-related anatomical and physiological changes to the cardiorespiratory system, is a critically important factor to reduce the ongoing cardiovascular disease burden. While prior exercise training and epidemiologic studies have described age-related declines in fitness, the current study contributes several novel findings to this evidence base. First, age-related declines in maximal fitness appeared to occur within the first few years of early adulthood and accelerated through midlife; declines that were mirrored when considering submaximal fitness. Second, important differences in maximal and submaximal fitness levels during early adulthood, and changes in fitness from early adulthood to midlife, were noted by race in men and women. Over the follow-up period, submaximal and maximal fitness declines were more attenuated in White men compared to Black men. Third, there were several factors present in early adulthood that were associated with both lower concurrent fitness levels and accelerated fitness declines through midlife; particularly when accounting for the cumulative number of years within the less favorable category since baseline.
While there remains limited evidence from longitudinal studies documenting age-related declines during earlier periods of adulthood, cross-sectional and longitudinal findings from the BLSA suggested a 5% per decade decline in peak VO2 starting at age 30 years (17). A rate of decline that was similar among Finnish Geriatric Intervention Study to Prevent Cognitive Impairment and Disability (FINGER) participants aged 60–77 years over 2-years [mean (SD): 23.4 (6.2) to 22.4 (6.0) ml/kg/min] (24). In contrast, findings from CARDIA suggest more accelerated declines in estimated maximal fitness per 5-year increment, ranging from 4.6% from ages 20–25 years to ≈10% per 5-year increment after age 30 years. This is equivalent to a reduction in estimated maximal workload from approximately 12 METs at baseline (duration just over 10 minutes) to 8 METs over the follow-up period (duration just under 6 minutes). While differences in findings between studies could be partially explained by use of estimated, rather than measured, maximal fitness in the current study, other reasons likely exist. Specifically, the limited racial diversity, smaller sample sizes of BLSA (particularly those aged <30 years; n=105) and FINGER, fewer assessment time-points, and shorter follow-up periods (7.9 and 2 years) may also contribute to the more attenuated fitness declines from early adulthood to midlife observed in prior longitudinal studies compared to CARDIA.
In CARDIA, differences in estimated submaximal fitness levels at each 5-year age increment and age-related declines by race within sex-strata mirrored those shown with maximal fitness with one exception. Specifically, estimated submaximal fitness at age 20 was higher in Black men while estimated maximal fitness at this age was higher in White men. After age 30, estimated submaximal and maximal fitness levels were consistently higher in White men compared with Black men. Regardless, the consistency in observed differences in submaximal and maximal fitness by a variety of subgroups has important research and clinical implications. For example, investigators of studies with limited financial resources to purchase necessary equipment (e.g., stress test systems, treadmills) and/or access to certified exercise testing personnel and/or medical (physician) supervisions could consider assessing fitness using submaximal test protocols. Given submaximal test protocols often pose less risk to participants and/or patients, eligibility would likely expand to include those with prevalent conditions, functional limitations, or experience symptoms of pain and/or fatigue, which would potentially result in a less biased sample (36).
Sex-related differences in estimated fitness at age 20 years and age-related declines were expected given known biological differences in the capacity to achieve a given level of fitness. In women, greater fat mass, lower hemoglobin concentrations, and lower maximal cardiac output due to smaller heart size and lower plasma volume all contribute to lower fitness levels in women compared to men (29). Conversely, while racial differences in fitness have been previously described in the literature (34, 41–43), the underlying mechanisms remain poorly understood and are likely not due to differences in genetics or ancestry. For example, when accounting for age, sex, body size, and physical activity levels, the HERITAGE Family Study (43), found no statistically significant difference in VO2max by race. Rather, observations of race-specific differences may instead be attributable to differences in socioeconomic, structural, or cultural inequities that are directly or indirectly associated with poorer fitness (44). Studies, including those published using prior CARDIA data (45, 46), have demonstrated the importance of habitual physical activity and maintenance of a healthy body weight to optimize fitness. As shown in the current study, Black women had a higher prevalence of inadequate physical activity and obesity in early adulthood (i.e., baseline) than other race/sex groups. Given observational data, it is not possible to isolate the factors causing or contributing to the observed racial differences in fitness from early adulthood through midlife among CARDIA participants. However, these observed differences may arise in part to health disparities associated with race including differences in access to safe places to be physically active and/or health care access and quality, including obesity prevention and management.
Perhaps the most important findings relate to the observed differences in age-related fitness declines through midlife by socioeconomic, behavioral, and health-related factors present in early adulthood. Early adulthood is a period of rapid change (47, 48), characterized by major life events including changes in relationships (e.g., marriage), family structure (e.g., birth of a child), residence, and employment, which can temporarily or permanently alter lifestyle behaviors and have subsequent implications on overall health. In the current study, participants who reported sufficient physical activity to meet guidelines, consumed alcohol, and never smoked had higher estimated fitness at age 20; a pattern that persisted for all behaviors except alcohol use after age 45. Also, individuals with overweight/obesity and fair/poor reported health had lower fitness in early adulthood and during the early adult to midlife transition. Together these findings suggest that early adulthood may serve as a critical life-course stage to intervene on unhealthy behaviors to optimize cardiovascular health to reduce risk or delay onset of subsequent disease.
Study strengths include use of the well-characterized CARDIA cohort to describe age-related changes in fitness during an earlier period of adulthood than previously described. Further, the fitness assessments in CARDIA span 20 years and this longer follow-up period was identified as a critical need for future studies (17). CARDIA is also a non-clinical sample and may provide a more accurate representation of fitness and aging in the general population, including antecedents of fitness changes using a life-course framework. While a prior CARDIA study documented the potential biases associated when evaluating health risks only among those willing and able to perform a GXT (36), our statistical approach allowed us to include 98% of the baseline sample. Also, maximal fitness estimates originating from a single field center were corrected due to a protocol deviation with a threshold of ≥15 RPE used to infer peak effort. While prior studies have a priori excluded these tests, findings from the sensitivity analysis support the utility of this approach.
There are also important limitations that should be considered when interpreting the findings. First, the CARDIA GXT protocol did not include collection of expired gases needed to obtain measured peak VO2, which is considered a gold standard measure of maximal cardiorespiratory fitness. The criterion validity of treadmill duration as an estimate of measured peak VO2 is unknown in CARDIA; however, this strategy is used in other studies without gas collection (49). However, whether measured or estimated fitness assessments are obtained, maximal GXT protocols rely on the participant’s intrinsic motivation to achieve a workload consistent with their maximal effort; particularly among population-based samples. Similarly, estimated peak VO2 values correspond to actual maximal heart rate that ranged within 85–100% of age-predicted maximal heart rate, depending on motivation, fatigue, pain or other symptomology. In the current analyses, we used the CARDIA formula to predict maximal heart rate based on age; however, other formulas exist. Also, heart rate at the end of Stage 2 was used to estimate submaximal fitness given the associated workload; however, it is possible that this may have represented a maximal effort in deconditioned individuals. Second, early adulthood factors associated with differences in concurrent fitness levels and fitness changes from early adulthood through midlife were participant-reported and may be subject to recall and prevarication biases. However, these data were collected every 2–5 years for 20 years, which may be more sensitive to change. Further, body composition measures (lean and fat mass) across exam years were not available and, due to limited numbers (4.56% at baseline), the underweight and normal weight BMI categories were combined. However, studies have shown that the potential health risks of having underweight increase with age (50). Also, given participant information prior to baseline are not available, estimates of cumulative number of years within the less favorable category were assigned a zero at baseline and accumulated thereafter. Finally, while models included several key covariates, the potential for residual confounding cannot be disregarded.
CONCLUSIONS
In summary, among the well-characterized CARDIA cohort, age-related declines in fitness from early adulthood to midlife were observed. In addition, several factors present as young adults were associated with lower concurrent fitness levels and/or accelerated fitness declines over-time, including education, financial strain, physical activity, alcohol and tobacco use, BMI, and self-rated health. Since fitness provides a reflection of total body health given required integration of several anatomical systems, these novel findings support the importance of the early adult period when developing and testing strategies focused on increasing healthy life expectancy.
Supplementary Material
SDC 1: Supplemental Table 1.docx - Estimated maximal and submaximal fitness
SDC 2: Supplemental Table 2.docx - Estimated graded exercise test duration in female participants
SDC 3: Supplemental Table 3.docx – Estimated graded exercise test duration for the overall cohort
SDC 4: Supplemental Table 4.docx - Estimated graded exercise test duration in male participants
SDC 5: Supplemental Text 5,docx – Formula to correct the graded exercise test duration estimates influenced by a protocol deviation
ACKNOWLEDGMENTS
The authors would like to acknowledge the CARDIA participants.
Conflict of Interest and Funding Source:
The authors have no conflicts of interest to disclose. The results of the study do not constitute endorsement by the American College of Sports Medicine. Study results are presented clearly, honestly, and without fabrication, falsification, or inappropriate data manipulation. The Coronary Artery Risk Development in Young Adults Study (CARDIA) is conducted and supported by the National Heart, Lung, and Blood Institute (NHLBI) in collaboration with the University of Alabama at Birmingham (HHSN268201800005I & HHSN268201800007I), Northwestern University (HHSN268201800003I), University of Minnesota (HHSN268201800006I), and Kaiser Foundation Research Institute (HHSN268201800004I). Additional support for this work was provided by the CARDIA Fitness Study (R01 HL078972 to BS & SS) and CARDIA Activity and Heart Failure Study (R01 HL149796 to KPG). The views expressed in this manuscript are those of the authors and do not necessarily represent the views of the National Heart, Lung, and Blood Institute; the National Institutes of Health; or the U.S. Department of Health and Human Services.
The Coronary Artery Risk Development in Young Adults Study (CARDIA) is conducted and supported by the National Heart, Lung, and Blood Institute (NHLBI) in collaboration with the University of Alabama at Birmingham (HHSN268201800005I & HHSN268201800007I), Northwestern University (HHSN268201800003I), University of Minnesota (HHSN268201800006I), and Kaiser Foundation Research Institute (HHSN268201800004I). This manuscript has been reviewed by CARDIA for scientific content. Additional support for this work was provided by the CARDIA Fitness Study (R01 HL078972 to BS & SS) and CARDIA Activity and Heart Failure Study (R01 HL149796 to KPG). The views expressed in this manuscript are those of the authors and do not necessarily represent the views of the National Heart, Lung, and Blood Institute; the National Institutes of Health; or the U.S. Department of Health and Human Services.
Footnotes
CONFLICT OF INTEREST: The authors have no conflicts of interest to disclose. The results of the study do not constitute endorsement by the American College of Sports Medicine (ACSM). Study results are presented clearly, honestly, and without fabrication, falsification, or inappropriate data manipulation.
REFERENCES
- 1.Ekelund LG, Haskell WL, Johnson JL, Whaley FS, Criqui MH, Sheps DS. Physical fitness as a predictor of cardiovascular mortality in asymptomatic North American men. The Lipid Research Clinics Mortality Follow-up Study. N Engl J Med. 1988;319(21):1379–84. [DOI] [PubMed] [Google Scholar]
- 2.Erikssen J Physical fitness and coronary heart disease morbidity and mortality. A prospective study in apparently healthy, middle aged men. Acta Med Scand Suppl. 1986;711:189–92. [PubMed] [Google Scholar]
- 3.Sandvik L, Erikssen J, Thaulow E, Erikssen G, Mundal R, Rodahl K. Physical fitness as a predictor of mortality among healthy, middle-aged Norwegian men. N Engl J Med. 1993;328(8):533–7. [DOI] [PubMed] [Google Scholar]
- 4.Hein HO, Suadicani P, Gyntelberg F. Physical fitness or physical activity as a predictor of ischaemic heart disease? A 17-year follow-up in the Copenhagen Male Study. J Intern Med. 1992;232(6):471–9. [DOI] [PubMed] [Google Scholar]
- 5.Peters RK, Cady LD Jr., Bischoff DP, Bernstein L, Pike MC. Physical fitness and subsequent myocardial infarction in healthy workers. JAMA. 1983;249(22):3052–6. [PubMed] [Google Scholar]
- 6.Slattery ML, Jacobs DR Jr., Nichaman MZ. An assessment of caloric intake as an indicator of physical activity. Prev Med. 1989;18(4):444–51. [DOI] [PubMed] [Google Scholar]
- 7.Slattery ML, Jacobs DR Jr., Nichaman MZ. Leisure time physical activity and coronary heart disease death. The US Railroad Study. Circulation. 1989;79(2):304–11. [DOI] [PubMed] [Google Scholar]
- 8.Sobolski J, Kornitzer M, De Backer G, et al. Protection against ischemic heart disease in the Belgian Physical Fitness Study: physical fitness rather than physical activity? Am J Epidemiol. 1987;125(4):601–10. [DOI] [PubMed] [Google Scholar]
- 9.Kokkinos P, Myers J, Kokkinos JP, et al. Exercise capacity and mortality in black and white men. Circulation. 2008;117(5):614–22. [DOI] [PubMed] [Google Scholar]
- 10.Astrand I Aerobic work capacity in men and women with special reference to age. Acta Physiol Scand Suppl. 1960;49(169):1–92. [PubMed] [Google Scholar]
- 11.Buskirk ER, Hodgson JL. Age and aerobic power: the rate of change in men and women. Fed Proc. 1987;46(5):1824–9. [PubMed] [Google Scholar]
- 12.Heath GW, Hagberg JM, Ehsani AA, Holloszy JO. A physiological comparison of young and older endurance athletes. J Appl Physiol Respir Environ Exerc Physiol. 1981;51(3):634–40. [DOI] [PubMed] [Google Scholar]
- 13.Jackson AS, Beard EF, Wier LT, Ross RM, Stuteville JE, Blair SN. Changes in aerobic power of men, ages 25–70 yr. Med Sci Sports Exerc. 1995;27(1):113–20. [PubMed] [Google Scholar]
- 14.Jackson AS, Wier LT, Ayers GW, Beard EF, Stuteville JE, Blair SN. Changes in aerobic power of women, ages 20–64 yr. Med Sci Sports Exerc. 1996;28(7):884–91. [DOI] [PubMed] [Google Scholar]
- 15.Fitzgerald MD, Tanaka H, Tran ZV, Seals DR. Age-related declines in maximal aerobic capacity in regularly exercising vs. sedentary women: a meta-analysis. J Appl Physiol (1985). 1997;83(1):160–5. [DOI] [PubMed] [Google Scholar]
- 16.Wilson TM, Tanaka H. Meta-analysis of the age-associated decline in maximal aerobic capacity in men: relation to training status. Am J Physiol Heart Circ Physiol. 2000;278(3):H829–34. [DOI] [PubMed] [Google Scholar]
- 17.Fleg JL, Morrell CH, Bos AG, et al. Accelerated longitudinal decline of aerobic capacity in healthy older adults. Circulation. 2005;112(5):674–82. [DOI] [PubMed] [Google Scholar]
- 18.Spina RJ. Cardiovascular adaptations to endurance exercise training in older men and women. Exerc Sports Sci Rev. 1999;27:317–32. [PubMed] [Google Scholar]
- 19.Katzel LI, Sorkin JD, Fleg JL. A comparison of longitudinal changes in aerobic fitness in older endurance athletes and sedentary men. J Am Geriatr Soc. 2001;49(12):1657–64. [DOI] [PubMed] [Google Scholar]
- 20.Pollock ML, Mengelkoch LJ, Graves JE, et al. Twenty-year follow-up of aerobic power and body composition of older track athletes. J Appl Physiol (1985). 1997;82(5):1508–16. [DOI] [PubMed] [Google Scholar]
- 21.Astrand I, Astrand PO, Hallback I, Kilbom A. Reduction in maximal oxygen uptake with age. J Appl Physiol. 1973;35(5):649–54. [DOI] [PubMed] [Google Scholar]
- 22.Rogers MA, Hagberg JM, Martin WH 3rd, Ehsani AA, Holloszy JO. Decline in VO2max with aging in master athletes and sedentary men. J Appl Physiol (1985). 1990;68(5):2195–9. [DOI] [PubMed] [Google Scholar]
- 23.Marti B, Howald H. Long-term effects of physical training on aerobic capacity: controlled study of former elite athletes. J Appl Physiol (1985). 1990;69(4):1451–9. [DOI] [PubMed] [Google Scholar]
- 24.Pentikainen H, Savonen K, Ngandu T, et al. Cardiorespiratory Fitness and Cognition: Longitudinal Associations in the FINGER Study. J Alzheimers Dis. 2019;68(3):961–8. [DOI] [PubMed] [Google Scholar]
- 25.Dougherty R, Lose SR, Gaitan JM, et al. Five-year changes in objectively measured cardiorespiratory fitness, physical activity, and sedentary time in mid-to-late adulthood. Appl Physiol Nutr Metab. 2021; Nov 25:1–4. Epub 2021/11/26. doi: 10.1139/apnm-2021-0500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Board on Children, Youth, and Families; Institute of Medicine; National Research Council. Improving the Health Safety and Well-Being of Young Adults: Workshop Summary. Washington (DC): National Academies Press (US); 2013. Sep 27. [PubMed] [Google Scholar]
- 27.Bibbins-Domingo K, Burroughs Pena M. Caring for the “young invincibles”. J Gen Intern Med. 2010;25(7):642–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Allender S, Hutchinson L, Foster C. Life-change events and participation in physical activity: a systematic review. Health Promot Int. 2008;23(2):160–72. [DOI] [PubMed] [Google Scholar]
- 29.Kenney WL, Wilmore JH, Costill DL. Physiology of sport and exercise. Sixth edition. ed. Champaign, IL: Human Kinetics; 2015. xix, 627 pages p. [Google Scholar]
- 30.Coronary Artery Risk Development in Young Adults (CARDIA) Study 2021. [cited 2021 October 11]. Available from: https://www.cardia.dopm.uab.edu/.
- 31.Gabriel KP, Sidney S, Jacobs DR Jr., et al. Convergent validity of a brief self-reported physical activity questionnaire. Med Sci Sports Exerc. 2014;46(8):1570–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ware JE, Kosinski M, Keller SD. A 12-item short-form health survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34(3):220–3. [DOI] [PubMed] [Google Scholar]
- 33.Balke B, Ware RW. An experimental study of physical fitness of Air Force personnel. U S Armed Forces Med J. 1959;10(6):675–88. [PubMed] [Google Scholar]
- 34.Sidney S, Haskell WL, Crow R, et al. Symptom-limited graded treadmill exercise testing in young adults in the CARDIA study. Med Sci Sports Exerc. 1992;24(2):177–83. [PubMed] [Google Scholar]
- 35.American College of Sports Medicine. ACSM’s Guidelines for Exercise Testing and Prescription - 10th edition. Medicine ACoS, editor: Lippincott Williams & Wilkins; 2017. [DOI] [PubMed] [Google Scholar]
- 36.Pettee Gabriel K, Whitaker KM, Duprez D, et al. Clinical importance of non-participation in a maximal graded exercise test on risk of non-fatal and fatal cardiovascular events and all-cause mortality: CARDIA study. Prev Med. 2018;106:137–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Borg GA. Psychophysical bases of perceived exertion. Med Sci Sports Exerc. 1982;14(5):377–81. [PubMed] [Google Scholar]
- 38.Whipp BJ, Ward SA. Physiological determinants of pulmonary gas exchange kinetics during exercise. Med Sci Sports Exerc. 1990;22(1):62–71. [PubMed] [Google Scholar]
- 39.Zhu N, Suarez-Lopez JR, Sidney S, et al. Longitudinal examination of age-predicted symptom-limited exercise maximum HR. Med Sci Sports Exerc. 2010;42(8):1519–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Schomaker M, Heumann C. Bootstrap inference when using multiple imputation. Stat Med. 2018;37(14):2252–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ribisl PM, Lang W, Jaramillo SA, et al. Exercise capacity and cardiovascular/metabolic characteristics of overweight and obese individuals with type 2 diabetes: the Look AHEAD clinical trial. Diabetes Care. 2007;30(10):2679–84. [DOI] [PubMed] [Google Scholar]
- 42.Swift DL, Johannsen NM, Lavie CJ, et al. Racial differences in the response of cardiorespiratory fitness to aerobic exercise training in Caucasian and African American postmenopausal women. J Appl Physiol (1985). 2013;114(10):1375–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Skinner JS, Jaskolski A, Jaskolska A, et al. Age, sex, race, initial fitness, and response to training: the HERITAGE Family Study. J Appl Physiol (1985). 2001;90(5):1770–6. [DOI] [PubMed] [Google Scholar]
- 44.Flanagin A, Christiansen S, Frey T. Reporting of Race and Ethnicity in Medical and Scientific Journals-Reply. JAMA. 2021;326(7):674–5. [DOI] [PubMed] [Google Scholar]
- 45.Sidney S, Sternfeld B, Haskell WL, Quesenberry CP Jr., Crow RS, Thomas RJ. Seven-year change in graded exercise treadmill test performance in young adults in the CARDIA study. Cardiovascular Risk Factors in Young Adults. Med Sci Sports Exerc. 1998;30(3):427–33. [DOI] [PubMed] [Google Scholar]
- 46.Lewis CE, Smith DE, Wallace DD, Williams OD, Bild DE, Jacobs DR Jr., Seven-year trends in body weight and associations with lifestyle and behavioral characteristics in black and white young adults: the CARDIA study. Am J Public Health. 1997;87(4):635–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Arnett JJ. Emerging adulthood. A theory of development from the late teens through the twenties. Am Psychol. 2000;55(5):469–80. Epub 2000/06/08. [PubMed] [Google Scholar]
- 48.Winpenny EM, Smith M, Penney T, et al. Changes in physical activity, diet, and body weight across the education and employment transitions of early adulthood: A systematic review and meta-analysis. Obes Rev. 2020;21(4):e12962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Blair SN, Kohl HW 3rd, Paffenbarger RS Jr., Clark DG, Cooper KH, Gibbons LW. Physical fitness and all-cause mortality. A prospective study of healthy men and women. JAMA. 1989;262(17):2395–401. [DOI] [PubMed] [Google Scholar]
- 50.Lorem GF, Schirmer H, Emaus N. What is the impact of underweight on self-reported health trajectories and mortality rates: a cohort study. Health Qual Life Outcomes. 2017;15(1):191. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
SDC 1: Supplemental Table 1.docx - Estimated maximal and submaximal fitness
SDC 2: Supplemental Table 2.docx - Estimated graded exercise test duration in female participants
SDC 3: Supplemental Table 3.docx – Estimated graded exercise test duration for the overall cohort
SDC 4: Supplemental Table 4.docx - Estimated graded exercise test duration in male participants
SDC 5: Supplemental Text 5,docx – Formula to correct the graded exercise test duration estimates influenced by a protocol deviation


