Abstract
Across the United States, physician burnout is progressively escalating, with accompanying negative sequelae for myriad stakeholders in healthcare, including communities, patients, physicians, and Healthcare Organizations (HCOs) with essential manpower implications. This ubiquitous trend is due to complex and multifactorial elements, including individual physician-related influences, generational perspectives, sociocultural communal effects, HCOs, and more recently the mounting challenges accompanying the COVID-19 pandemic. To achieve the overarching goals of US healthcare provision (ie, safe, effective, patient-centered, timely, efficient, and equitable patient care), proposed solutions should focus on longitudinal actionable data acquisition to meet workforce needs preemptively, resource allocation for wellness programs geared towards enhancing recruitment and retention, and shared responsibility at the level of individual physician and HCO. This descriptive literature-based treatise expounds on the underlying causality for physician burnout, its consequences for the healthcare workforce in the US, and provides individual- and institution-based solutions for its mitigation.
Keywords: burnout, pandemic, workforce, healthcare, COVID-19
Introduction and Scope of the Problem
The American Psychologist Herbert Freudenberger1 identified the phenomenon of “burnout” in 1974, describing it as a state corollary to protracted pressure and apprehension manifesting in those engaged in the “healing professions” who are particularly predisposed to employment-associated emotional and physical debilitation. Maslach et al2 further advanced the concept by characterizing burnout as a “work-related syndrome” of emotional enervation and pessimism that often expresses in individuals engaged in social services that typically encompasses emotional lassitude and a contracted sense of personal achievement and contribution to a shared mission. This literature-based perspective explicates on the underlying causes and consequences of physician burnout, influences posed by the COVID-19 pandemic, and proposes solutions for alleviating its escalating rate in the US.
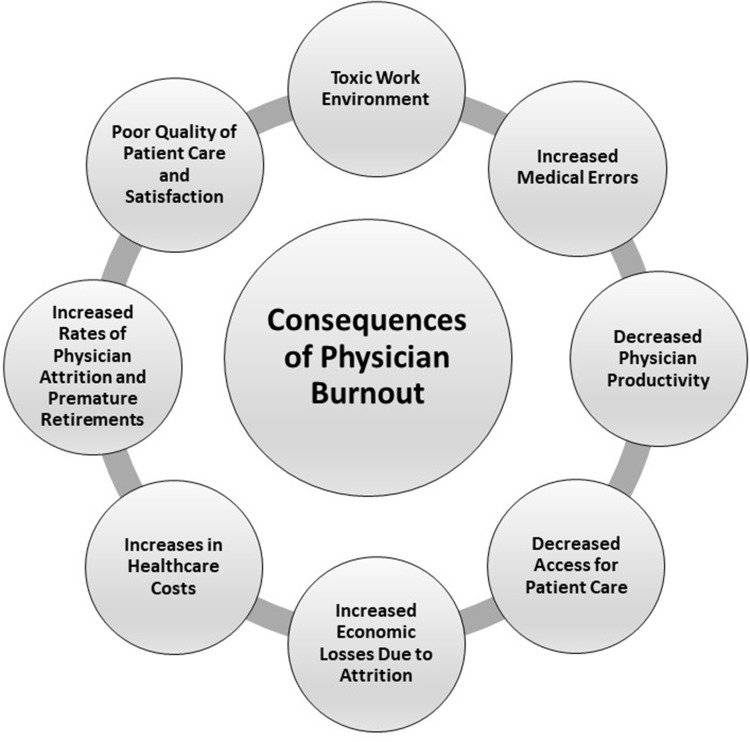
From the workforce point of view, the phenomenon of burnout has resulted in widespread detrimental sequelae including a culture of doubt, interpersonal skirmishes and other toxic or unprofessional interactions in the workplace, discontent in personal life, despair, and destructive behaviors such as substance abuse.1 Physician burnout is worsening the frequency of premature retirement and attrition rates, thereby exacerbating the anticipated shortfall in the physician workforce (estimated to be between 21,000–45,000 in primary care and 34,000–87,000 in specialty care physicians by 2025) as an aggregate effect of other influences including an epidemiological shift toward an aging US population with accompanying chronic medical conditions and multiple co-morbidities, a reduced number of students pursuing the medical profession resulting in fewer physician graduates from medical schools and residency training programs.3 Consequently, a multitude of stakeholders – patients, physicians, trainees, Healthcare Organizations (HCOs)) – are adversely affected by physician burnout. Downstream effects include compromised patient care quality and satisfaction, an increase in medical oversight and errors, diminished physician productivity, decreased access to patient care, substantial economic losses for replacement of vacancies from resignations (~2–3-times base salary), all culminating in accentuated healthcare costs4,5 (Figure 1). To provide perspective, the total annual cost from burnout among healthcare managers alone is estimated to be $300 billion.6
Figure 1.
Consequences of physician burnout.
Utilizing validated instruments such as Maslach, Oldenburg, and Copenhagen Burnout Inventories, Stanford Fulfillment Index, and the Well-Being Index, the prevalence of physician burnout over the past two decades, including trainees as well as those in practice, is estimated to exceed 50%. Clearly, this represents a public health and healthcare crisis.7 Moreover, the trends in physician burnout are disconcerting. In a study that included 6,880 US physicians, the overall mean rate of burnout increased significantly from 45% to 54% (~10% increase from 2011–2014), while concurrent satisfaction with work and life balance dropped from 48% to 40%.7 Concomitantly in the same timeframe, the prevalence of burnout in the general employed workforce remained stable at ~28%.8 Data from the Well-Being Index in 2021 (n=165,129 assessments) demonstrates the incidence of physician burnout to be ~55%, with 52% of respondents narrating emotional lability, and one-third of physicians reporting not having adequate time for personal or family life.9 Burnout is not limited to any particular type of medical practice, in that it affects physicians across the gamut (academic and government-owned HCOs, private practice). Medical subspecialties play a substantial role, with some being more susceptible than others, eg, physicians in Emergency Medicine, General Internal Medicine, Neurology, and Family Medicine, are affected with the highest frequency, Anesthesiology with intermediate, and Preventive and Occupational Medicine with the lowest rates.7,10 The surge in physician burnout and its downstream detrimental sequelae have amplified the need for researchers and administrative leaders to investigate its underlying causation as a prelude to articulating and implementing pragmatic solutions.
Causality and Predispositions
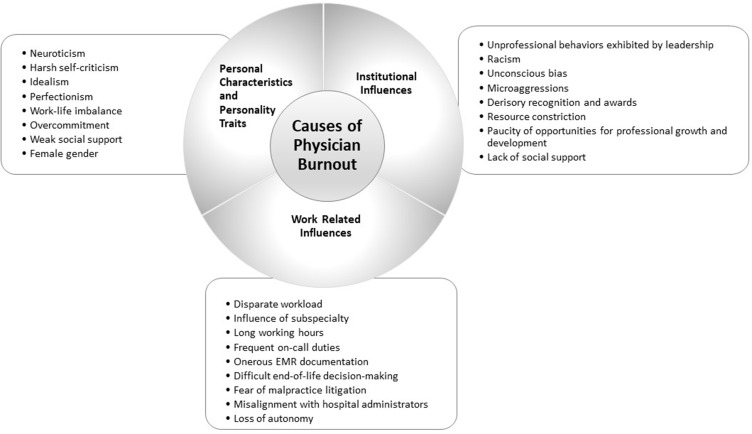
Burnout syndrome can be seen as an aggregate effect of the complex interaction of personal attributes coupled with work- and organizational-related dynamics (Figure 2). Personal characteristics, phenotypes, and character traits that presage burnout include neuroticism, severe self-criticism, over-commitment, idealism, a perfectionist outlook, and work–personal life disparity, with a suboptimal communal sustenance structure – eg, daycare services for children, care for elderly relatives, public transportation, etc. In contrast, extraversion and a collaborative outlook portend less physician burnout. Surprisingly given the not-unreasonable assumption that the phenomenon is a late-career syndrome in older physicians, younger physicians are twice as much at risk for developing the syndrome with its onset during their residency and fellowship training.11 There is a gender influence to burnout (20–60% increased probability in females) manifested as experiencing a combination of emotional exhaustion and reification, presumably resulting from having to undertake multiple roles at home in addition to career stressors. Consequently – and ominously, the physicians most vulnerable to burnout syndrome tend to be fervent, meticulous, committed physicians who have excelled during their training (medical school, residency, and fellowship) and have a track record of accomplishments along with a promising career path.11 It has been posited that generational differences may also play a significant role with issues surrounding lifestyle and work–life balance taking increasing importance in younger generations (eg, Millennials, Gen Z).
Figure 2.
Causes of physician burnout.
Work-related factors in physician burnout include incongruent workload correlated to certain subspecialties, long working hours, frequent on-call obligations, work carried home for incessant documentation, completion of tedious electronic patient health records (“pajama time”), computerized physician order entry, trepidations pertaining to malpractice lawsuits, participating in challenging end-of-life decision-making with patients’ families, loss of autonomy with moderated control of their time and work environment, ever-constricting resources, being “policed” by administrators, and a lack of trust between HCOs’ administrative leadership and physicians.12,13 Factors attributable to HCOs include acceptance of unprofessional behaviors demonstrated by organizational leadership, xenophobia, unconscious bias, micro-aggressions, inadequate recognition and awards, a dearth of opportunities for professional growth and development, and a lack of social support for physicians.8
Recalibrating in the Era of the COVID-19 Pandemic
The COVID-19 pandemic has radically affected the physician workforce in the US for a multitude of reasons, including compromised physical and emotional wellbeing (eg, due to scarcity of Personal Protective Equipment, increased workload, managing gravely ill patients, and having difficult end-of-life discussions with their families), an increased need to augment healthcare personnel capabilities, and through diminished manpower when employees are quarantined due to seropositivity or are staying away from work to provide care to a sick relative or render parental care to children due to school closures. Most HCOs in the US have had to modulate archaic internal procedures and workflows, task-assignment protocols, or union contracts to circumvent staffing shortages to render safe and efficient patient care without compromising quality. Affording surge capacity by re-hiring healthcare professionals who have retired or transiently left the workforce is an additional tactic being utilized by many HCOs.14 Other methodologies to surmount staffing shortages include expanding scopes of practice, issuing cross-state licensures, and utilizing telehealth services more widely, especially for ambulatory care. In a recent survey, ~74% of physicians reported a change in work settings (partially remote and onsite), ~4% relocated from their primary department, and ~12% from onsite to remote locations during the COVID-19 pandemic.15 It is highly likely that additional stresses and anxieties associated with the pandemic from direct patient care, and witnessing and sharing in families’ grieving process, will further exacerbate physician burnout and augment rates of attrition. These postulates are supported by a recent study (over 2,000 US physicians) in which nearly 75% reported being overworked, with ~50% considering an employment change during the pandemic, with the preponderance of women physicians (25%) contemplating early retirement.16 This scenario is reminiscent of the aftermaths of the events of September 11, 2001, Hurricane Katrina in 2004, and Hurricane Ike in 2008, when many healthcare workers experienced Post-Traumatic Stress Disorder (PTSD) and other affective disorders. The specific deleterious effects of the COVID “Long-Haulers” (post-COVID syndrome)17 with failure to thrive with accompanying neurological, affective, and cognitive dysfunction remains indeterminate at present and poses a diagnostic challenge in differentiating organic disease from burnout syndrome or PTSD.
Proposed Solutions for Mitigation
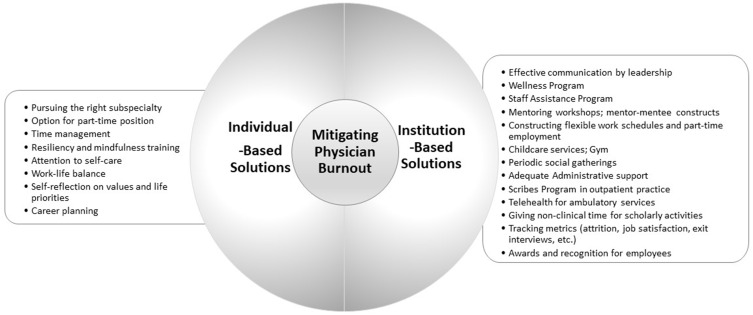
There is mounting evidence that multimodal approaches focused on the individual physician as well as on institutional leadership, governance structure, operations, and processes in HCOs are essential for addressing physician burnout.18 However, published reports on proposed solutions to date have significant limitations for various reasons. First, there is a paucity of evidence-based research. Second, reports have focused on solitary interventions as opposed to multimodal methodologies. Third, studies have negligible randomized control design function, particularly as it pertains to elucidations from organizational or structural modifications. And, fourth, studies have relied on extrapolation of results between different medical subspecialties as well as extension across different institutions.19 Notwithstanding these shortcomings, taken together, such interventions have demonstrated amelioration in burnout symptoms of 14% for emotional lassitude, 4% for objectification, and 10% for global burnout symptoms.18
Specific individual-based and organizational-level solutions (Figure 3) have been proposed for each of the above limitations, with HCO leadership working in close collaboration with various departments and Human Resources that include: 1) addressing disparate workloads through consideration of part-time positions, well-appraised practice, and pursuing specialty choices at the individual level, delineating judicious productivity goals, redefining duty hour thresholds, and proper allotment of organization level functional positions and duties; 2) addressing perceived loss of control and autonomy through stress management, resiliency, and mindfulness coaching, as well as constructive coping approaches at the individual level; 3) nurturing collaborative physician engagement and leadership in establishing work requirements, structure, and shared decision-making at the organizational level; 4) tackling work-related ineptitude and lack of support by the HCO through optimizing electronic medical records and offloading the burden of documentation by support staff; 5) physicians focusing on issues at the individual level regarding life–work balance by paying attention to self-care and introspection on their values and life priorities; 6) in addition to Staff Assistance Programs, cultivating and implementing an institutional Wellness Program at the organizational level – many premier academic HCOs, including Stanford, Johns Hopkins University, and the Mayo Clinic have implemented thoughtful, methodical approaches such as instituting an iterative Wellness Program that includes an institutional committee with a designated Chief Wellness Officer as a principal organizational tactic to help healthcare providers20 engender cognizance for obligations outside of work and in constructing adjustable work schedules that include part-time employment; 7) investing in on- and off-site periodic social gatherings for sharing challenges and experiences in small group luncheons or dinners sponsored by the organization; 8) developing longitudinal valid burnout assessments as part of a “dashboard” for appraising and tracking metrics stratified by specialties, departments, and work units (eg, employee attrition rates, job satisfaction, quality outcomes, and leadership performance longitudinally)21 to offer valuable insights on actionable data in a confidential manner.
Figure 3.
Mitigating physician burnout.
Others have proposed utilizing the approach of “Appreciative Inquiry” to mitigate burnout syndrome.22 Especially valuable would be for government and regulatory bodies to address the onerous documentation that diverts physicians away from direct patient care by instituting a scribes’ program in ambulatory practices. It is suggested that “Triple Aim” methodology be at the forefront to incorporate improving the work lives of healthcare personnel, environment, and processes to enhance patient experience, attenuate costs, and ameliorate the health of populations.23 Lastly, it would be beneficial to safeguard “non-clinical time” for non-revenue generating educational and scholarly activities, and administrative duties for physicians in academic HCOs.13,21 It must be underscored that the delivery of healthcare is a team effort, and physicians must have a heightened sense of awareness and compassion that other members of the healthcare team (nursing staff, ancillary healthcare staff, etc.) are also prone to burnout syndrome.
With the ongoing COVID-19 pandemic over the past 2 years, it is evident that HCOs will require human resources and capital; vibrant organizational leadership; as well as judicious interventions to ensure employee health and welfare to maintain a balance between job demands, resources, and institutional performance. Concrete solutions and resources – eg, working remotely, employee assistance and Wellness programs, counseling and therapy, and psychological support —will all be critical in meeting these goals. Ongoing longitudinal research should shed light on and provide valuable insights into job re-design and crafting in the era of this pandemic.24
Conclusions and Future Directions
Physician burnout is becoming increasingly prevalent with adverse sequelae impacting numerous stakeholders in healthcare, including patients, physicians, the public, and HCOs,15 with profound effects on the US healthcare workforce. The underlying causes of this pervasive phenomenon are multifactorial and primarily attributable to sociocultural societal influences, HCOs, and healthcare systems, in addition to individual physician-related pressures. Effective solutions should target continued research and collective accountability at both individual physician and HCO levels with an amalgam of authentic, servant, and transformational leadership25,26 to fulfill healthcare’s mission(s) as articulated by the Institute of Medicine27 in providing “safe, effective, patient-centered, timely, efficient, and equitable” patient care while meeting the needs of all other stakeholders.
Disclosure
The author reports no conflicts of interest in this work.
References
- 1.Freudenberger HJ. Staff burn-out. J Social Issues. 1974;30:159–165. doi: 10.1111/j.1540-4560.1974.tb00706.x [DOI] [Google Scholar]
- 2.Maslach C, Jackson SE, Leiter MP. Maslach Burnout Inventory Manual. 3rd ed. Palo Alto, CA: Consulting Psychologist Press; 1996. [Google Scholar]
- 3.Association of American Medical Colleges. The complexities of physician supply and demand projections from 2018 to 2033. Available from: https://www.aamc.org/system/files/2020-06/stratcomm-aamc-physician-workforce-projections-june-2020.pdf. Accessed February 20, 2022.
- 4.Shanafelt TD, Noseworthy JH. Executive leadership and physician well-being: nine organizational strategies to promote engagement and reduce burnout. Mayo Clin Proc. 2016;92:129–146. doi: 10.1016/j.mayocp.2016.10.004 [DOI] [PubMed] [Google Scholar]
- 5.West CP, Dyrbye LN, Shanafelt TD. Physician burnout: contributors, consequences, and solutions. J Intern Med. 2018;283:516–529. doi: 10.1111/joim.12752 [DOI] [PubMed] [Google Scholar]
- 6.Andrews B, Bonvicini K. Caring for caregivers: addressing physician burnout; 2016. Available from: http://healthcarecomm.org/wp-content/uploads/2016/11/PhysicianBurnout_AUG_2016_MGMA-CONNECTIONS.pdf. Accessed February 21, 2022.
- 7.Shanafelt TD, Hasan O, Dyrbye LN, et al. Changes in burnout and satisfaction with work-life balance in physicians and the general US working population between 2011 and 2014. Mayo Clin Proc. 2015;90:1600–1613. [DOI] [PubMed] [Google Scholar]
- 8.Rothenberger DA. Physician burnout and well-being: a systematic review and framework for action. Dis Colon Rectum. 2017;60(6):567–576. doi: 10.1097/DCR.0000000000000844 [DOI] [PubMed] [Google Scholar]
- 9.Well-Being Index. State of well-being 2021–2022. Available from: Mywellbeingindex.org. Accessed May 24, 2022.
- 10.Lee RT, Seo B, Hladkyj S, et al. Correlates of physician burnout across regions and specialties: a meta-analysis. Hum Resour Health. 2013;11(1):1–16. doi: 10.1186/1478-4491-11-48 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Patel RS, Bachu R, Adikev A, et al. Factors related to physician burnout and its consequences. A review. Behav Sci. 2018;8(11):98. doi: 10.3390/bs8110098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bhardwaj A. Alignment between physicians and hospital administrators: historical perspective and future directions. Hosp Pract. 2017;45:81–87. doi: 10.1080/21548331.2017.1327302 [DOI] [PubMed] [Google Scholar]
- 13.Bhardwaj A. What’s new in academic International medicine? The evolving terrain of American Academic medicine. Int J Acad Med. 2019;5:85–92. doi: 10.4103/IJAM.IJAM_25_19 [DOI] [Google Scholar]
- 14.Fraher EP, Pittman P, Frogner BK, et al. Ensuring and sustaining a pandemic workforce. N Engl J Med. 2020;382(23):2181–2183. doi: 10.1056/NEJMp2006376 [DOI] [PubMed] [Google Scholar]
- 15.Well-Being Index Insights. COVID-19 impact report. Phase 1; 2020. Available from: Mywellbeingindex.org. Accessed May 24, 2022.
- 16.Doximity. 2021 physician compensation report. Fifth Annual Study. Available from: https://c8y.doxcdn.com/image/upload/v1/Press%20Blog/Research%20Reports/Doximity-Compensation-Report-2021.pdf. Accessed May 4, 2022.
- 17.Collins F. Study finds 1 in 10 healthcare workers with mild COVID have lasting symptoms. Available from: https://directorsblog.nih.gov/2021/04/20/study-finds-1-in-10-healthcare-workers-with-mild-covid-have-lasting-symptoms/. Accessed February 22, 2022.
- 18.West CP, Dyrbye LN, Erwin PJ, Shanafelt TD. Interventions to prevent and reduce physician burnout: a systematic review and meta-analysis. Lancet. 2018;388:2272–2281. doi: 10.1016/S0140-6736(16)31279-X [DOI] [PubMed] [Google Scholar]
- 19.Williams ES, Rathert C, Buttigieg SC. The personal and professional consequences of physician burnout: a systematic review of the literature. Med Care Res Rev. 2020;77(5):371–386. doi: 10.1177/1077558719856787 [DOI] [PubMed] [Google Scholar]
- 20.Shanafelt T, Trockel M, Ripp J, et al. Building a program on well-being: key design considerations to meet the unique needs of each organization. Acad Med. 2019;94:156–161. doi: 10.1097/ACM.0000000000002415 [DOI] [PubMed] [Google Scholar]
- 21.Shanafelt TD, Mungo M, Schmitgen J, et al. Longitudinal study evaluating the association between physician burnout and professional work effort. Mayo Clin Proc. 2016;91(4):422–431. doi: 10.1016/j.mayocp.2016.02.001 [DOI] [PubMed] [Google Scholar]
- 22.Gunderman RB. An appreciative approach to burnout; 2019. Available from: https://scholarworks.iupui.edu/bitstream/handle/1805/22057/Gunderman_2019_Appreciative.pdf?sequence=1. Accessed February 20, 2022. [DOI] [PubMed]
- 23.Berwick DM, Nolan TW, Whittington J. The triple AIM: care, health, and cost. Health Aff. 2008;27:759–769. doi: 10.1377/hlthaff.27.3.759 [DOI] [PubMed] [Google Scholar]
- 24.Kniffin KM, Narayanan I, Anseel F, et al. COVID-19 and the workplace: implications, issues, and insights for future research and action. Am Psychol. 2021;76(1):63–77. doi: 10.1037/amp0000716 [DOI] [PubMed] [Google Scholar]
- 25.Kumar RDC, Khiljee N. Leadership in healthcare. Anaesth Intensive Care. 2016;17:63–65. doi: 10.1016/j.mpaic.2015.10.012 [DOI] [Google Scholar]
- 26.Zenger JH, Folkman J. The Extraordinary Leader, Turning Good Managers into Great Leaders. 2nd ed. McGraw Hill; 2009. [Google Scholar]
- 27.Institute of Medicine (IOM). Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, D.C: National Academy Press; 2001. [PubMed] [Google Scholar]