Abstract
Background
This Bayesian network meta-analysis investigated the available randomized control trials (RCTs) to point out which acupuncture protocol is the most effective for chronic aspecific low back pain (LBP). Efficacy was measured in terms of pain (Visual Analogic Scale, VAS) and disability (Roland Morris Disability Questionnaire, RMQ), Transcutaneous Electrical Nerve Stimulation (TENS).
Methods
PubMed, Google scholar, Embase, and Scopus were accessed in March 2022. All the RCTs comparing two or more acupuncture modalities for aspecific chronic LBP were accessed. Only studies which investigated the efficacy of acupuncture on patients with symptoms lasting a minimum of 1.5 months, or with at least three episodes in the previous 12 months, were considered eligible. The Review Manager Software (The Nordic Cochrane Collaboration, Copenhagen) was used for the methodological quality assessment. The STATA Software/MP, Version 14.1 (StataCorporation, College Station, Texas, USA), was used for the statistical analyses. The NMA was performed through the STATA routine for Bayesian hierarchical random-effects model analysis.
Results
Data from 44 RCTs (8338 procedures) were retrieved. 56% of patients were women. The mean age of the patients was 48 ± 10.6 years. The mean BMI was 26.3 ± 2.2 kg/m2. The individual group (95% confidence interval (CI) 2.02, 7.98) and the standard combined with TENS (95% CI 2.03, 7.97) demonstrated the highest improvement of the RMQ. The VAS score was lower in the standard combined with TENS group (95% CI 3.28, 4.56). Considering the standard acupuncture group, different studies used similar protocols and acupuncture points and the results could thus be compared. The equation for global linearity did not find any statistically significant inconsistency in any of the network comparison.
Conclusion
Verum acupuncture is more effective than sham treatment for the non-pharmacological management of LBP. Among the verum protocols, individualized acupuncture and standard acupuncture with TENS were the protocols that resulted in the highest improvement in pain and quality of life.
Level of Evidence
Level I, Bayesian network meta-analysis of RCTs.
Keywords: Acupuncture, Low back pain, Verum acupuncture, Individualized acupuncture, Sham acupuncture
Introduction
Low back pain (LBP) is common, leading to relevant economic burden [1, 2]. On average, the lifetime prevalence of LBP is as high as 80% [3, 4]. LBP is aspecific in most cases, and no pathoanatomical cause can be found [5]. In such patients, management aims to reduce symptoms and disability, allowing the return to daily life activities and participation in physiotherapy [5]. Current guidelines recommend physiotherapy as a first-line treatment for chronic LBP [6]. As some patients do not experience sufficient benefit from physiotherapy alone, further options are required. Pharmacotherapy is the second step in the management of chronic aspecific LBP [6]. NSAIDs and opiates represent the most successful treatment options [7, 8]. However, potential side-effects of pharmacotherapy, along with the risk of opioids addiction, make this option viable and safe only in the short term. As the number of patients with chronic aspecific LBP increases, so does the demand for safe and effective therapies. Among these, acupuncture has been widely investigated in recent times as possible options, proving to be a safe and effective therapy for chronic aspecific LBP [9–11]. Many different acupuncture protocols have been proposed for the management of chronic aspecific LBP. This Bayesian network meta-analysis investigated the available randomized control trials (RCTs) to try and identify which acupuncture protocol is the most effective for chronic aspecific LBP. Efficacy was measured in terms of pain (Visual Analogic Scale, VAS) and disability (Roland Morris Disability Questionnaire, RMQ) to investigate the efficacy of acupuncture on different aspects of the patients’ overall quality of life.
Material and methods
Search strategy
This Bayesian network meta-analysis was conducted according to the PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of healthcare interventions [12]. A guide protocol was preliminary drafted:
P (population): Chronic low back pain;
I (intervention): Acupuncture;
C (comparison): Standardized, sham, individual, auricular, electroacupuncture, acupuncture combined with Transcutaneous Electrical Nerve Stimulation (TENS);
O (outcomes): VAS, RMQ.
Data source and extraction
Two authors (A.M. and A.B.) independently performed the literature search in April 2022. The following databases were accessed: PubMed, Google scholar, Embase, and Scopus. The following keywords were used in combination: low, lumbar, back, lower, spine, pain, disability, management, therapy, treatments, acupuncture, auricular, tens, electroacupuncture, auricular, individualized, standardized, visual analogic scale, vas, Roland Morris questionnaire. The same authors independently performed the initial screening. If the title and abstract matched the topic, the article full-text was accessed. A cross reference of the bibliographies was also performed. Disagreement was debated and solved by a third author (N.M.).
Eligibility criteria
All the RCTs comparing two or more acupuncture modalities for aspecific chronic LBP were accessed. Only studies which investigated the efficacy of acupuncture on patients with symptoms lasting a minimum of 1.5 months, or with at least three episodes in the previous 12 months were considered eligible. Only studies involving patients aged 18 to 75 were considered. Aspecific LBP was defined as pain that was not arising from a specific pathoanatomical condition [5]. Given the authors language capabilities, articles in English, German, Italian, French and Spanish were eligible. Only level I of evidence studies, according to Oxford Centre of Evidence-Based Medicine [13], were considered. Studies reporting data over acupressure or percutaneous electrical nerve stimulation were not considered. Studies reporting the efficacy of acupuncture in patients with acute pain were not included, nor were those investigating the cervicothoracic segments. Studies investigating patients with neurological deficits were excluded, along with studies including patients with radicular pain (unless the radicular pain was only a minor complaint). Editorials, reviews, letters, opinion, technical notes, comments were not eligible, nor were biomechanical, cadaveric, or animal studies. Only articles reporting quantitative data under the outcomes of interest were considered for inclusion. Missing data under the outcomes of interest warranted exclusion from this study.
Data extraction
Two authors (A.M. and A.B.) independently performed data extraction the resulting articles for inclusion. Study generalities (author, year, journal, design, length of the follow-up) and patient demographic at baseline were extracted (number of samples and related mean BMI and age, percentage of female). For every treatment, the following data were retrieved: VAS, RMQ, adverse events. The groups considered were standard acupuncture alone, standard acupuncture with TENS, electroacupuncture, individualized acupuncture, and auricular acupuncture. The treatment group was classified as individualized acupuncture when the treating physician chose the needling points for each patient, without following a specific protocol. The treatment was defined as standard acupuncture when all patients were treated with the same protocol. Sham acupuncture was defined as the needling of points other than the known acupuncture points: as shallow needling of acupuncture points may also elicit a fibroblast reaction, this method was considered as a form of verum acupuncture [14]. The association of acupuncture with electrostimulation was considered separately.
Risk of bias assessment
The risk of bias assessment was conducted by two authors (A.M. and A.B.) independently. The Review Manager Software (The Nordic Cochrane Collaboration, Copenhagen) was used for the methodological quality assessment. The following risk of bias were evaluated: selection, detection, reporting, attrition, and other source of bias. For each comparison, the risk of bias was investigated using funnel plots. Plot asymmetries relates to greater risk of bias.
Statistical analysis
The statistical analyses were conducted by the senior author (F.M.). Baseline comparability was assessed through the IBM SPSS software. The analysis of variance (ANOVA) was used for analysis, with P values > 0.1 considered satisfactory. All other treatments rather than standardized, individual, auricular, electroacupuncture, combined with TENS, sham acupuncture were included in the “control group” and excluded from the analysis. The STATA Software/MP, Version 14.1 (StataCorporation, College Station, Texas, USA) was used for the statistical analyses. The NMA was performed through the STATA routine for Bayesian hierarchical random-effects model analysis. The inverse variance method was used for analysis, with standardized mean difference (STD) effect measure. The overall inconsistency was evaluated through the equation for global linearity via the Wald test. If the P value < 0.5, the null hypothesis cannot be rejected, and the consistency assumption could be accepted at the overall level of each treatment. Both confidence (CI) and percentile (PrI) intervals were set at 95%. For each comparison, edge plots were performed to display amount and interpolations of direct comparisons; interval plots were performed to rank the treatments according to their effect measure; and asymmetry of the funnel plots was associated with the greater risk of publication bias.
Results
Search result
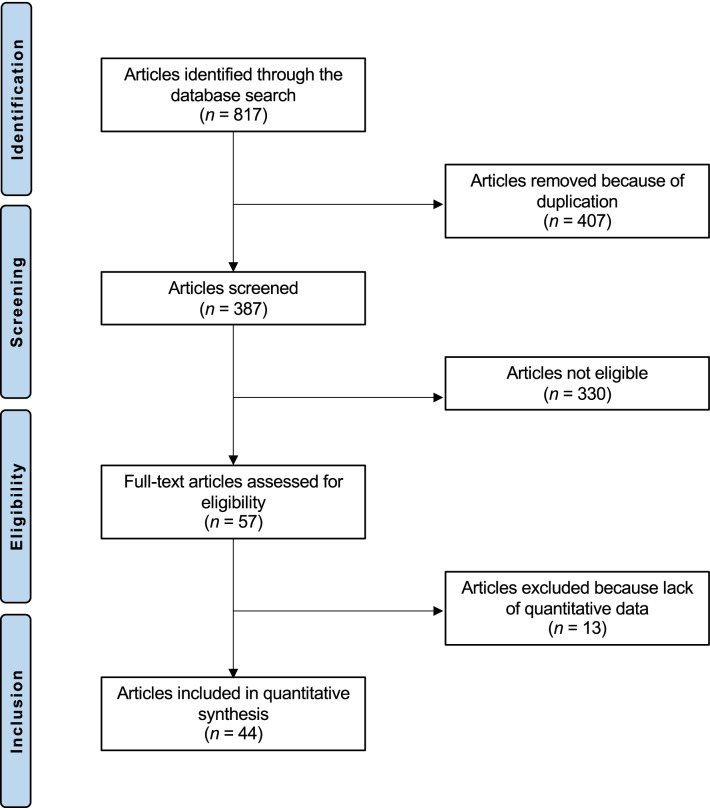
The literature search resulted in 817 RCTs. Four hundred and seven were excluded as they were duplicates. A further 330 studies were incompatible with the eligibility criteria: type of study (N = 89), not matching the topic of interest (N = 193), acupressure or percutaneous electrical nerve stimulation (N = 15), acute LBP (N = 11), concerning cervicothoracic segments (N = 5), presence of severe neurologic impairment or spine deformities (N = 3), acute setting (N = 2), old age (N = 1), language limitations (N = 2), other (N = 9). Another 13 studies were excluded as they did not report quantitative data under the outcomes of interest. This left 44 RCTs for the present study. The literature search results are shown in Fig. 1.
Fig. 1.
Flowchart of the literature search
Methodological quality assessment
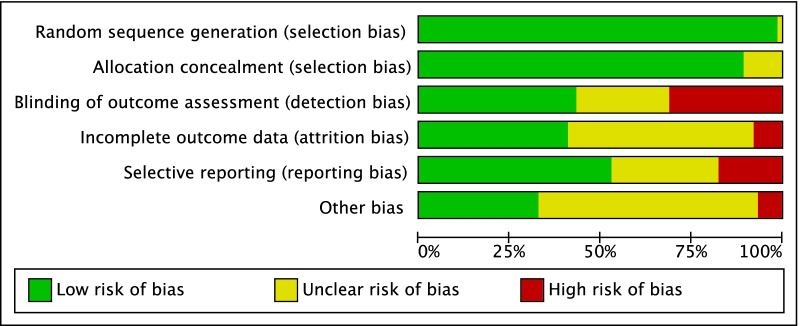
Given the randomized design of the included studies, the risk of selection bias was low. Assessor blinding was performed in 75% (33 of 44) studies; however, the blinding methods were often biased, and the overall risk of detection bias was moderate. The risk of attrition and reporting biases were low to moderate, as was the risk of other bias. Concluding, the methodological quality assessment showed low to moderate risk of bias (Fig. 2).
Fig. 2.
Methodological quality assessment
Patient demographics
Data from 8338 procedures were retrieved. 56% of patients were women. The mean age of the patients was 48 ± 10.6 years. The mean BMI was 26.3 ± 2.2 kg/m2. The ANOVA test found moderate baseline comparability in symptoms duration (P > 0.05). Patient demographics are shown in Table 1.
Table 1.
Generalities and patient baseline of the included studies
| Author, year | Journal | Treatment | Type of protocol | Patients (n) | Follow-up (months) | Mean age | Women (%) | Mean BMI |
|---|---|---|---|---|---|---|---|---|
| Brinkhaus et al. [15] | Arch Intern Med | Individualized | 12 sessions of 30 min over 8 weeks (2 sessions in each of the first 4 weeks, followed by 1 session per week in the remaining 4 weeks) | 147 | 13 | 59.1 | 64 | 26.7 |
| Sham | 75 | 58.2 | 75 | 26.2 | ||||
| Control | Patients in the waiting list group did not receive acupuncture treatment for 8 weeks after randomization | 79 | 58.9 | 68 | 26.9 | |||
| Camilotti et al. [16] | Fisioter. Mov | Physiotherapy/ Aquatic Therapy | Twice a week | 15 | 61.7 | 27.8 | ||
| Auricular/scalp/standardized | 15 | 57.3 | 27.6 | |||||
| Control | 14 | 61.2 | 28.7 | |||||
| Ceccherelli et al. [17] | The Clinical Journal of Pain | Standardized | 8 sessions for 20 min; the first four sessions were carried out in 2 weeks, whereas the remaining four sessions were carried out once per week | 21 | 3 | 41.7 | 24 | |
| Individualized | 21 | 41.6 | 33 | |||||
| Cherkin et al. [18] | Arch Intern Med | Individualized | Up to 10 massages or acupuncture treatments over 10 weeks were permitted | 94 | 12 | 45.3 | 52 | |
| Control | 78 | 45.7 | 69 | |||||
| Control | 90 | 43.8 | 56 | |||||
| Cherkin et al. [19] | Arch Intern Med | Individualized | 2 treatments weekly for 3 weeks; then once weekly for 4 weeks | 157 | 13 | 47.0 | 68 | |
| Standardized | 158 | 49.0 | 56 | |||||
| Sham | 162 | 47.0 | 60 | |||||
| Usual care | Patients received no study-related care; just the care, if any, they and their physicians chose (mostly medications, primary care, and physical therapy visits) | 161 | 46.0 | 64 | ||||
| Cho et al. [20] | Spine | Individualized |
12 acupuncture sessions (approximately 2 times a week for 6 weeks) |
65 | 6 | 42.4 | 83 | 23.9 |
| Sham | 65 | 41.8 | 86 | 24.2 | ||||
| Comachio et al. [21] | Journal of Acupuncture and Meridian Studies | Individualized | 1-h sessions, twice a week for 6 weeks | 33 | 3 | 49.0 | 70 | 26.9 |
| Electroacupuncture | 33 | 46.0 | 58 | 26.0 | ||||
| Di Cesare et al. [22] | Complementary Therapies in Medicine | Control | 1 injection per week for 4 weeks | 29 | 3 | 52.5 | 55 | |
| Standardized | 33 | 52.5 | 55 | |||||
| Giles et al. [23] | Journal of Manipulative and Physiological Therapeutics | Individualized | 15- to 20-min appointments with subsequent low-volt electrical stimulation applied to the needles, 6 treatments applied in a 3- to 4-week period, (mean 6 treatments) | 20 | 0 | 46.5 | 65 | |
| Control | Pills given for the defined 3- to 4-week treatment period, (mean 2 prescriptions) | 21 | 35.0 | 81 | ||||
| Control | 15 to 20-min appointments, 6 treatments applied in a 3- to 4-week period, (mean 6 treatments) | 36 | 42.5 | 47 | ||||
| Giles et al. [24] | Spine | Standardized | 20-min appointments, 2 treatments per week, maximum treatment duration of 9 weeks | 36 | 12 | 37.5 | 44 | 25.8 |
| Control | Maximum treatment duration of 9 weeks | 43 | 39.0 | 43 | 25.8 | |||
| Control | 20-min appointments, 2 treatments per week, maximum treatment duration of 9 weeks | 36 | 39.0 | 49 | 25.8 | |||
| Grant et al. [25] | Pain | Individualized | 2 sessions of manual acupuncture weekly for 4 weeks | 30 | 3 | 75.0 | ||
| TENS | 27 | 72.0 | ||||||
| Haake et al. [26] | Arch Intern Med | Individualized | Ten 30-min sessions, generally 2 sessions per week, and 5 additional sessions if, after the tenth session, patients experienced a 10% to 50% reduction in pain intensity | 387 | 6 | 49.6 | 57 | 26.9 |
| Sham | 387 | 49.2 | 64 | 26.5 | ||||
| Control | 388 | 51.3 | 58 | 26.3 | ||||
| Hasegawa et al. [27] | Acupunct Med | Standardized | 5 sessions during 28 days | 40 | 0 | 47.0 | 63 | |
| Sham | 40 | 43.9 | 65 | |||||
| Hunter et al. [28] | Clin J Pain | Physiotherapy | Supervised group exercise session lasting for 1 h a week for 6 weeks | 27 | 6 | 43.2 | 59 | |
| Auricular | Manual AA for the first 6 weeks of the trial before each exercise session | 24 | 42.4 | 67 | ||||
| Inoue et al. [29] | Acupunct Med | Individualized | Once | 15 | 68.0 | 27 | ||
| Sham | 16 | 70.0 | 38 | |||||
| Itoh et al. [30] | Complementary Therapies in Clinical Practice | Standardized | 1 weekly treatment over 5 weeks | 7 | 2.5 | 63 | ||
| TENS | 7 | |||||||
| Acupuncture and TENS | 7 | |||||||
| Control | No specific treatment | 7 | ||||||
| Itoh et al. [31] | Acupunct Med | Individualized |
2 phases of 3 weeks, 12 weeks in total. Each patient received a total of six 30 min treatments, one per week |
9 | 2.75 | 70.1 | 71 | |
| Individualized | 9 | 71.9 | ||||||
| Standard | 9 | 73.8 | ||||||
| Itoh et al. [30] | Complementary Therapies in Clinical Practice | Standardized | 5 treatments, once per week | 8 | 2.5 | 63 | ||
| TENS | 8 | |||||||
| Acupuncture and TENS | 8 | |||||||
| Control | 8 | |||||||
| Kalauokalani et al. [32] | Spine | Control | Up to 10 treatments within 10 weeks | 0 | ||||
| Individualized | ||||||||
| Control | ||||||||
| Control | 66 | 45.0 | 70 | |||||
| Control | 69 | 43.0 | 57 | |||||
| Kennedy et al. [33] | Complementary Therapies in Medicine | Individualized | Once or twice a week; min 3 and max 12 treatments over 4–6 weeks | 23 | 3 | 46.5 | 46 | |
| Sham | 22 | 44.6 | 58 | |||||
| Kerr et al. [34] | Clin J Pain | Standard | The treatment program consisted of 6 of these sessions over a 6-week period. This reflected the routine pattern of attendance for outpatient physiotherapy. Patients were given a leaflet regarding their low back pain that included standardized advice and exercises | 26 | 1.5 | 42.6 | 50 | |
| Placebo-TENS | 20 | 42.8 | 65 | |||||
| Leibing et al. [35] | Pain | Standardized | 20 sessions (each 30 min) of traditional and standardized acupuncture over 12 weeks, plus active physiotherapy. In the first 2 weeks of treatment, acupuncture was done five times a week, and in the next 10 weeks once a week. Plus physiotherapy 26 sessions (each 30 min) over 12 weeks | 40 | 13 | 47.9 | 55 | 26.1 |
| Sham | 20 sessions (each 30 min) of minimal acupuncture over 12 weeks, plus active physiotherapy 26 sessions (each 30 min) over 12 weeks | 45 | 49.0 | 60 | 25.9 | |||
| Control | Active physiotherapy with no other treatment 26 sessions (each 30 min) over 12 weeks | 46 | 47.5 | 59 | 26.9 | |||
| Liu et al. [36] | Clin Rehab | Standardized | Usual care + assigned acupuncture intervention according to group allocation. 30-min treatment sessions were administered twice weekly | 15 | 3 | 30.0 | 60 | 23.9 |
| Standardized | 15 | 37.1 | 60 | 27.0 | ||||
| Standardized | 15 | 30.8 | 73 | 27.4 | ||||
| Luo et al. [37] | Journal of traditional Chinese medicine | Auricular | 18 treatments were provided over 7 weeks | 54 | 6 | 39.0 | 20 | |
| Standardized | 50 | 36.0 | 24 | |||||
| Control | 48 | 37.0 | 19 | |||||
| Macdonald et al. [38] | Annals of the Royal College of Surgeons of England | Individualized | Over a short period of time once a week. The maximum number of treatments between the two assessments was arbitrarily defined as 10 | 8 | 0 | 75 | ||
| Control | 9 | 67 | ||||||
| Mendelson et al. [39] | The American Journal of Medicine | Standardized | 4 weeks of treatment, twice weekly | 36 | 1 | 54.5 | 47 | |
| Control | 41 | 53.6 | 56 | |||||
| Meng et al. [40] | Rheumatology | Standardized | In addition to standard therapy, subjects in this group received acupuncture treatments twice a week for 5 weeks, for a total of 10 sessions | 31 | 2.25 | 72.0 | 58 | |
| Control | 5 weeks | 24 | 70.0 | 63 | ||||
| Miyazaki et al. [14] | Clin J Pain | Standardized | A washout period of at least 4 weeks took place between phases 1 and 2 | 42 | 20.8 | 22.7 | ||
| Control | 39 | 21.0 | 25.1 | |||||
| Molsberger et al. [41] | Pain | Sham | In addition to the daily conservative orthopedic therapy, all patients received 12 sham treatments, (30 min, 3/ week) | 61 | 3 | 50.0 | 46 | |
| Standardized | In addition to the conventional conservative orthopedic therapy, 12 verum acupuncture treatments (30 min, 3/ week) | 65 | 49.0 | 45 | ||||
| Control | These patients received the daily conventional conservative orthopedic treatment over 4 weeks | 60 | 49.0 | 53 | ||||
| Pach et al.[42] | Evidence-Based Complementary and Alternative Medicine | Standardized | 2 treatment sessions per week had to be applied, with a maximum number of 10 to 15 sessions depending on the patient’s individual needs. The needle retention time was about 25 min | 78 | 6.5 | 59.3 | 54 | 27.2 |
| Individualized | 72 | 56.1 | 63 | 27.0 | ||||
| Rajfur et al. [43] | Medical science monitor | TENS | A series of 15 treatments, 5 times a week (Monday to Friday) for a period of 3 weeks | 20 | 0 | 50.2 | 55 | 26.7 |
| Acupuncture and TENS | 20 | 52.1 | 60 | 27.0 | ||||
| Control | 19 | 47.8 | 58 | 26.3 | ||||
| Control | 21 | 48.7 | 62 | 26.1 | ||||
| Control | 22 | 52.1 | 59 | 25.9 | ||||
| Control | Motor improvement exercises were used for 3 weeks, 5 times a week, from Monday to Friday | 21 | 49.8 | 62 | 26.1 | |||
| Sator-Katzenschlager [44] | Pain Medicine | Electroacupuncture | The acupuncture needles with the P-Stim™ devices were withdrawn 48 h after insertion in all cases and the acupuncture treatment was performed once a week for 48 h at home, for a total study period of 6 wk | 61 | 1.5 | 54.1 | 71 | 26.6 |
| Acupuncture | 53.1 | 25.3 | ||||||
| Shankar et al. [45] | Indian Journal of Physiology and Pharmacology | Electroacupuncture | 10 treatments over 3 weeks | 30 | 0 | 36.2 | 53 | 22.9 |
| Control | 10 days of Valdecoxib and 3 weeks of physiotherapy | 30 | 34.5 | 80 | 22.0 | |||
| Control | 30 | 35.9 | 57 | 23.3 | ||||
| Szczurko et al. [46] | PLoS ONE | Acupuncture | Twice per week to receive 24 treatments over a period of 12 weeks | 39 | 3 | 45.3 | 56 | 28.7 |
| Control | Participants randomized to the control group received an educational booklet (causes of back pain, prognosis, appropriate use of imaging studies and specialists, and exercises for promoting recovery and preventing recurrences) | 36 | 48.0 | 44 | 27.7 | |||
| Thomas et al. [47] | BMJ | Individualized | 10 individualized treatment sessions over 3 months | 159 | 24 | 42.0 | 62 | |
| Control | Patients in the usual care group received NHS treatment according to their general practitioner’s assessment of need | 80 | 44.0 | 58 | ||||
| Witt et al. [48] | American J Epidemiology | Individualized | Maximum of 15 acupuncture sessions over 3 months | 1451 | 6 | 53.1 | 58 | |
| Control | Conventional therapy | 1390 | 52.6 | 57 | ||||
| Yeung et al. [49] | Journal of Alternative and Complementary Medicine | Control | An hourly session each week for 4 consecutive weeks + daily 15 months of home exercise | 26 | 3 | 55.6 | 81 | 24.2 |
| Standardized | EA three times/ week, 4 weeks | 26 | 50.4 | 85 | 25.5 | |||
| Tsui et al. [50] | The journal of alternative and complementary medicine | Electroacupuncture | Treatment for 20 min on a total of 6 acupuncture points. Treatment was delivered twice per week for 4 weeks (a total of 8 sessions) | 14 | 1 | 39.7 | 76 | |
| Electroacupuncture | 14 | 39.1 | 71 | |||||
| Control | 14 | 40.9 | 62 | |||||
| Tsukayama et al. [51] | Acupuncture in medicine | Electroacupuncture | Twice a week for 2 weeks | 10 | 0 | 47.0 | 89 | 22.5 |
| TENS | 10 | 43.0 | 80 | 22.2 | ||||
| Weiß et al. [52] | The journal of alternative and complementary medicine | Standardized | 21-day inpatient rehabilitation and acupuncture twice weekly | 74 | 3 | 49.8 | 27 | 30.0 |
| Control | 21-day inpatient rehabilitation | 69 | 51.7 | 39 | 28.8 | |||
| Yoo et al. [53] | Journal of Korean Medicine Rehabilitation | Standardized | Treatment within 5 days. A total of 2 treatments | 15 | 0 | 37.9 | 22.3 | |
| Sham | 15 | 37.9 | 23.9 | |||||
| Yuan et al. [54] | Complementary Therapies in Medicine | Individualized | 10 treatments; 2 times/week | 15 | 12 | 43.5 | 40 | 27.0 |
| 10 treatments; 5 times/week | 15 | 43.9 | 40 | 27.3 | ||||
| Yun et al. [55] | The Journal of Alternative and Complementary Medicine | Control | 18 treatments were provided over 7 weeks, every other day for 3 weeks and then twice weekly for 4 weeks | 64 | 11 | 35.0 | 22 | |
| Individualized | 60 | 34.0 | 27 | |||||
| Control | 63 | 33.0 | 19 | |||||
| Zaringhalam et al. [56] | Chinese Medicine Journal | Standardized | Twice a week for 5 weeks | 20 | 2.5 | 54.2 | 0 | 32.5 |
| Control | daily | 20 | 55.1 | 29.2 | ||||
| Control | Twice a week for 5 weeks | 20 | 54.2 | 30.3 | ||||
| Control | 20 | 54.3 | 31.0 |
Outcomes of interest
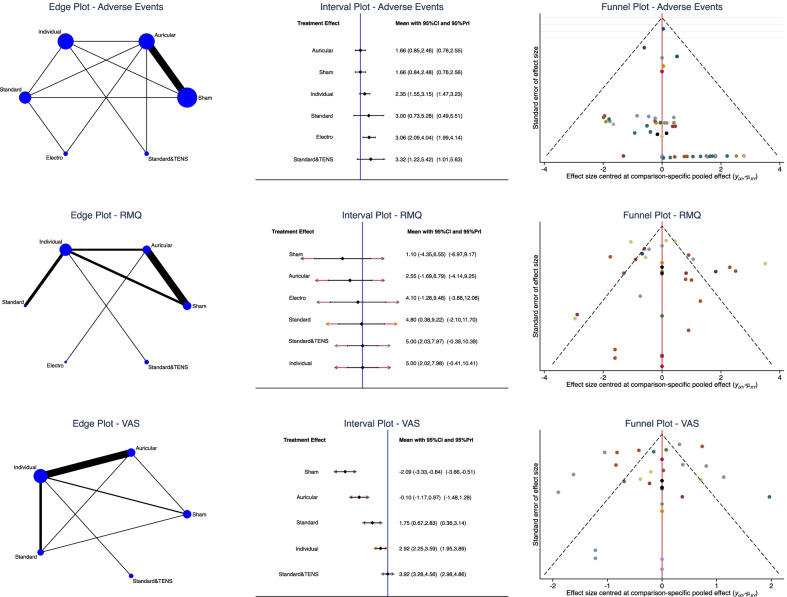
The individual group (SMD 5.00; 95% CI 2.02, 7.98) and the standard combined with TENS (SMD 5.00; 95% CI 2.03, 7.97) demonstrated the highest improvement of RMQ. The VAS score was lower in the standard combined with TENS group (SMD 3.92; 95% CI 3.28, 4.56). Considering the standard acupuncture group, different studies utilized similar protocols and acupuncture points and the results could thus be compared. The equation for global linearity did not find any statistically significant inconsistency in any of the network comparisons. Edge, interval, and funnel plots are shown in Fig. 3.
Fig. 3.
Results of the network comparisons
Discussion
According to the main findings of the present Bayesian network meta-analysis, individualized acupuncture and the standard protocol with TENS may represent the most effective acupuncture strategies for the management of chronic aspecific LBP. These two treatment protocols showed the highest improvements of VAS and RMQ. As verum acupuncture scored better than sham treatment, the present study points to the efficacy of acupuncture in the management of aspecific chronic LBP. This finding further supports current guidelines which recommend acupuncture as one of the possible first-line, non-pharmacological management modality for aspecific chronic LBP [6].
These results are consistent with previous studies [10, 11], which observed a superiority of acupuncture compared to sham treatment [57, 58]. A meta-analysis by Amaral et al. observed only moderate-quality evidence in favor of acupuncture treatment for LBP; however, this study focused only on trigger point acupuncture in the geriatric population, and the results are not directly comparable with those of the present cohort [9]. Nascimiento et al. also observed poor outcomes for acupuncture for LBP in the geriatric population [59]. While no specific characteristics could be highlighted in patients who responded to acupuncture for chronic pain [60], the role of age on the effectiveness of the therapy in the setting of LBP deserves further investigation. A meta-analysis by Mu and colleagues found that acupuncture has only limited effect on pain relief and improvement of the quality of life in the immediate to short term [61]. Li et al. highlighted that a treatment duration of at least 5 weeks is required to achieve 80% of the maximum analgesic effect [62] of acupuncture. Thus, the relatively short timeframe considered by Mu et al. (one to 12 weeks) [61], along with the high risk of bias of the included studies [61], may explain the differences in the observed results. The literature regarding the use of acupuncture in the acute setting is limited and, so far, no studies have been directed to analyze the literature regarding different types of acupuncture for the treatment of acute LBP. Thus, a direct comparison of the presented results with those of the acute setting is not possible. Overall, acupuncture seems to be modestly effective for the management of acute LBP, and the available studies agree that more high-quality work are required to gain more evidence around this topic [63, 64]. Considering the reluctance of many physicians to prescribe acupuncture in patients with chronic LBP, it is fundamental to highlight the efficacy of this treatment in comparison with sham acupuncture. However, the finding that individualized treatment is more effective than standard treatment suggests that a precise diagnosis of chronic LBP according to the criteria of traditional Chinese medicine and the choice of specific acupuncture points may be key for the efficacy of the treatment. This result confirms the clinical experience of the authors. The association of standard protocols with TENS yielded however results similar to those of individualized acupuncture.
This study has several limitations. The most important limitation is the heterogeneous protocols used. Given the randomized design of patient allocation, the risk of selection bias was low. However, some studies did not perform patients or personnel blinding, thus increasing the risk of detection and performance biases, respectively. General health measures were seldom reported, as were also information about the duration of previous symptoms, and type of pain (e.g., central sensitization). Previous conservative strategies were barely reported. Given the lack of quantitative data, the ethnicity of the patients was not analyzed separately. Given the heterogeneity of the protocols used, it was not possible to analyze the effects of the associations of acupuncture with other treatments such as pharmacological management and physio- and psychotherapy. Also, some acupuncture techniques such as moxibustion, cupping or scalp acupuncture were excluded from the study as the available data were not sufficient to grant inclusion. As a multimodal approach is often advisable to tackle the different organic and psychosocial aspects of chronic LBP [6, 65–68], further studies will be required to investigate the efficacy of different treatment associations and protocols. Furthermore, the available studies only allowed for a precise analysis of the effects of acupuncture in the population < 75 years old: targeted studies for this segment of the population will be required to investigate the efficacy of acupuncture in the elderly.
Conclusion
Verum acupuncture is more efficient than sham treatment for the non-pharmacological management of LBP. Among verum protocols, individualized acupuncture and standard acupuncture with TENS were the protocols that allowed for the highest improvement in pain and quality of life.
Acknowledgements
None
Abbreviations
- RCTs
Randomized control trials
- LBP
Low back pain
- VAS
Visual analogic scale
- RMQ
Roland Morris disability questionnaire
- PRISMA
Preferred reporting items for systematic reviews and meta-analyses
- BMI
Body mass index
- ANOVA
Analysis of variance
- NMA
Network meta-analysis
- STD
Standardized mean difference
- CI
Confidence interval
- PrI
Percentile interval
Author contribution
FM involved in conception and design of the study, literature search, data extraction, methodological quality assessment, writing, statistical analysis, interpretation of data, and final approval; AB involved in literature search, data extraction, methodological quality assessment, writing, and final approval; NM involved in revision and final approval; and FM and AK involved in supervision and final approval. All authors read and approved the final manuscript.
Funding
Open Access funding enabled and organized by Projekt DEAL. No external source of funding was used.
Availability of data and materials
The data underlying this article are available in the article and in its online supplementary material.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable
Competing interests
Professor Maffulli is Editor in Chief of the Journal of Orthopaedic Surgery and Research.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Golob AL, Wipf JE. Low back pain. Med Clin North Am. 2014;98:405–428. doi: 10.1016/j.mcna.2014.01.003. [DOI] [PubMed] [Google Scholar]
- 2.Krismer M, van Tulder M. Strategies for prevention and management of musculoskeletal conditions. Low back pain (non-specific) Best Pract Res Clin Rheumatol. 2007;21:77–91. doi: 10.1016/j.berh.2006.08.004. [DOI] [PubMed] [Google Scholar]
- 3.Ganesan S, Acharya AS, Chauhan R, et al. Prevalence and risk factors for low back pain in 1355 young adults: a cross-sectional study. Asian Spine J. 2017;11:610–617. doi: 10.4184/asj.2017.11.4.610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lee CA, Jang H-D, Moon JE, et al. The relationship between change of weight and chronic low back pain in population over 50 years of age: a nationwide cross-sectional study. Int J Environ Res Public Health. 2021 doi: 10.3390/ijerph18083969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Maher C, Underwood M, Buchbinder R. Non-specific low back pain. The Lancet. 2017;389:736–747. doi: 10.1016/S0140-6736(16)30970-9. [DOI] [PubMed] [Google Scholar]
- 6.Qaseem A, Wilt TJ, McLean RM, et al. Noninvasive treatments for acute, subacute, and chronic low back pain: a clinical practice guideline from the American college of physicians. Ann Intern Med. 2017;166:514–530. doi: 10.7326/M16-2367. [DOI] [PubMed] [Google Scholar]
- 7.Migliorini F, Maffulli N, Baroncini A, et al. Opioids for chronic low back pain management: a Bayesian network meta-analysis. Expert Rev Clin Pharmacol. 2021;14:635–641. doi: 10.1080/17512433.2021.1903316. [DOI] [PubMed] [Google Scholar]
- 8.Migliorini F, Maffulli N, Eschweiler J, et al. Non-steroidal anti-inflammatory drugs and gabapentinoids for chronic lumbar pain: a Bayesian network meta-analysis of randomized controlled trials. Br Med Bull. 2021;138:85–95. doi: 10.1093/bmb/ldab003. [DOI] [PubMed] [Google Scholar]
- 9.Amaral LKB, Souza MB, Campos MGM, et al. Efficacy of conservative therapy in older people with nonspecific low back pain: a systematic review with meta-analysis and GRADE recommendations. Arch Gerontol Geriatr. 2020;90:104177. doi: 10.1016/j.archger.2020.104177. [DOI] [PubMed] [Google Scholar]
- 10.Huang J-F, Zheng X-Q, Chen D, et al. Can acupuncture improve chronic spinal pain? A systematic review and meta-analysis. Global Spine J. 2021;11:1248–1265. doi: 10.1177/2192568220962440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Li Y-X, Yuan S-E, Jiang J-Q, et al. Systematic review and meta-analysis of effects of acupuncture on pain and function in non-specific low back pain. Acupunct Med. 2020;38:235–243. doi: 10.1136/acupmed-2017-011622. [DOI] [PubMed] [Google Scholar]
- 12.Hutton B, Salanti G, Caldwell DM, et al. The PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: checklist and explanations. Ann Intern Med. 2015;162:777–784. doi: 10.7326/M14-2385. [DOI] [PubMed] [Google Scholar]
- 13.Howick JCI, Glasziou P, Greenhalgh T, Heneghan C, Liberati A, Moschetti I, Phillips B, Thornton H, Goddard O, Hodgkinson M (2011) The 2011 Oxford CEBM Levels of Evidence. Oxford Centre for Evidence-Based Medicine Available at https://www.cebm.net/indexaspx?o=5653. www.https://www.cebm.net/
- 14.Miyazaki S, Hagihara A, Kanda R, et al. Applicability of press needles to a double-blind trial: a randomized, double-blind, placebo-controlled trial. Clin J Pain. 2009;25:438–444. doi: 10.1097/AJP.0b013e318193a6e1. [DOI] [PubMed] [Google Scholar]
- 15.Brinkhaus B, Witt CM, Jena S, et al. Acupuncture in patients with chronic low back pain: a randomized controlled trial. Arch Intern Med. 2006;166:450–457. doi: 10.1001/archinte.166.4.450. [DOI] [PubMed] [Google Scholar]
- 16.Camilotti BM, Leite N, Alberti D, et al. Effects of Ai Chi and Yamamoto new scalp acupuncture on chronic low back pain. Fisioter mov. 2015;28:723–730. doi: 10.1590/0103-5150.028.004.ao09. [DOI] [Google Scholar]
- 17.Ceccherelli F, Rigoni MT, Gagliardi G, et al. Comparison of superficial and deep acupuncture in the treatment of lumbar myofascial pain: a double-blind randomized controlled study. Clin J Pain. 2002;18:149–153. doi: 10.1097/00002508-200205000-00003. [DOI] [PubMed] [Google Scholar]
- 18.Cherkin DC, Eisenberg D, Sherman KJ, et al. Randomized trial comparing traditional Chinese medical acupuncture, therapeutic massage, and self-care education for chronic low back pain. Arch Intern Med. 2001;161:1081–1088. doi: 10.1001/archinte.161.8.1081. [DOI] [PubMed] [Google Scholar]
- 19.Cherkin DC, Sherman KJ, Avins AL, et al. A randomized trial comparing acupuncture, simulated acupuncture, and usual care for chronic low back pain. Arch Intern Med. 2009;169:858–866. doi: 10.1001/archinternmed.2009.65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cho Y-J, Song Y-K, Cha Y-Y, et al. Acupuncture for chronic low back pain: a multicenter, randomized, patient-assessor blind, sham-controlled clinical trial. Spine (Phila Pa 1976) 2013;38:549–557. doi: 10.1097/BRS.0b013e318275e601. [DOI] [PubMed] [Google Scholar]
- 21.Comachio J, Oliveira CC, Silva IFR, et al. Effectiveness of manual and electrical acupuncture for chronic non-specific low back pain: a randomized controlled trial. J Acupunct Meridian Stud. 2020;13:87–93. doi: 10.1016/j.jams.2020.03.064. [DOI] [PubMed] [Google Scholar]
- 22.Di Cesare A, Giombini A, Di Cesare M, et al. Comparison between the effects of trigger point mesotherapy versus acupuncture points mesotherapy in the treatment of chronic low back pain: a short term randomized controlled trial. Complement Ther Med. 2011;19:19–26. doi: 10.1016/j.ctim.2010.11.002. [DOI] [PubMed] [Google Scholar]
- 23.Giles LGF, Müller R. Chronic spinal pain syndromes: a clinical pilot trial comparing acupuncture, a nonsteroidal anti-inflammatory drug, and spinal manipulation. J Manipulative Physiol Ther. 1999;22:376–381. doi: 10.1016/s0161-4754(99)70082-5. [DOI] [PubMed] [Google Scholar]
- 24.Giles LGF, Muller R. Chronic spinal pain: a randomized clinical trial comparing medication, acupuncture, and spinal manipulation. Spine (Phila Pa 1976) 2003;28:1490–1502. doi: 10.1097/00007632-200307150-00003. [DOI] [PubMed] [Google Scholar]
- 25.Grant DJ, Bishop-Miller J, Winchester DM, et al. A randomized comparative trial of acupuncture versus transcutaneous electrical nerve stimulation for chronic back pain in the elderly. Pain. 1999;82:9–13. doi: 10.1016/S0304-3959(99)00027-5. [DOI] [PubMed] [Google Scholar]
- 26.Haake M, Müller H-H, Schade-Brittinger C, et al. German Acupuncture Trials (GERAC) for chronic low back pain: randomized, multicenter, blinded, parallel-group trial with 3 groups. Arch Intern Med. 2007;167:1892–1898. doi: 10.1001/archinte.167.17.1892. [DOI] [PubMed] [Google Scholar]
- 27.Hasegawa TM, Baptista AS, de Souza MC, et al. Acupuncture for acute non-specific low back pain: a randomised, controlled, double-blind, placebo trial. Acupunct Med. 2014;32:109–115. doi: 10.1136/acupmed-2013-010333. [DOI] [PubMed] [Google Scholar]
- 28.Hunter RF, McDonough SM, Bradbury I, et al. Exercise and auricular acupuncture for chronic low-back pain: a feasibility randomized-controlled trial. Clin J Pain. 2012;28:259–267. doi: 10.1097/AJP.0b013e3182274018. [DOI] [PubMed] [Google Scholar]
- 29.Inoue M, Kitakoji H, Ishizaki N, et al. Relief of low back pain immediately after acupuncture treatment–a randomised, placebo controlled trial. Acupunct Med. 2006;24:103–108. doi: 10.1136/aim.24.3.103. [DOI] [PubMed] [Google Scholar]
- 30.Itoh K, Itoh S, Katsumi Y, et al. A pilot study on using acupuncture and transcutaneous electrical nerve stimulation to treat chronic non-specific low back pain. Complement Ther Clin Pract. 2009;15:22–25. doi: 10.1016/j.ctcp.2008.09.003. [DOI] [PubMed] [Google Scholar]
- 31.Itoh K, Katsumi Y, Kitakoji H. Trigger point acupuncture treatment of chronic low back pain in elderly patients–a blinded RCT. Acupunct Med. 2004;22:170–177. doi: 10.1136/aim.22.4.170. [DOI] [PubMed] [Google Scholar]
- 32.Kalauokalani D, Cherkin DC, Sherman KJ, et al. Lessons from a trial of acupuncture and massage for low back pain: patient expectations and treatment effects. Spine (Phila Pa 1976) 2001;26(13):1418–1424. doi: 10.1097/00007632-200107010-00005. [DOI] [PubMed] [Google Scholar]
- 33.Kennedy S, Baxter GD, Kerr DP, et al. Acupuncture for acute non-specific low back pain: a pilot randomised non-penetrating sham controlled trial. Complement Ther Med. 2008;16:139–146. doi: 10.1016/j.ctim.2007.03.001. [DOI] [PubMed] [Google Scholar]
- 34.Kerr DP, Walsh DM, Baxter D. Acupuncture in the management of chronic low back pain: a blinded randomized controlled trial. Clin J Pain. 2003;19:364–370. doi: 10.1097/00002508-200311000-00004. [DOI] [PubMed] [Google Scholar]
- 35.Leibing E, Leonhardt U, Köster G, et al. Acupuncture treatment of chronic low-back pain–a randomized, blinded, placebo-controlled trial with 9-month follow-up. Pain. 2002;96:189–196. doi: 10.1016/s0304-3959(01)00444-4. [DOI] [PubMed] [Google Scholar]
- 36.Liu L, Skinner MA, McDonough SM, et al. Acupuncture for chronic low back pain: a randomized controlled feasibility trial comparing treatment session numbers. Clin Rehabil. 2017;31:1592–1603. doi: 10.1177/0269215517705690. [DOI] [PubMed] [Google Scholar]
- 37.Yong L, Min Y, Tao L, Xiaolong Z, Wen T, Mingyang G, Yonghe H. Effect of hand-ear acupuncture on chronic low-back pain: a randomized controlled trial. J Tradit Chin Med. 2019;39:587–594. [PubMed] [Google Scholar]
- 38.Macdonald AJ, Macrae KD, Master BR, et al. Superficial acupuncture in the relief of chronic low back pain. Ann R Coll Surg Engl. 1983;65:44–46. [PMC free article] [PubMed] [Google Scholar]
- 39.Mendelson G, Selwood TS, Kranz H, et al. Acupuncture treatment of chronic back pain. Am J Med. 1983;74:49–55. doi: 10.1016/0002-9343(83)91117-8. [DOI] [PubMed] [Google Scholar]
- 40.Meng CF, Wang D, Ngeow J, et al. Acupuncture for chronic low back pain in older patients: a randomized, controlled trial. Rheumatology (Oxford) 2003;42:1508–1517. doi: 10.1093/rheumatology/keg405. [DOI] [PubMed] [Google Scholar]
- 41.Molsberger AF, Mau J, Pawelec DB, et al. Does acupuncture improve the orthopedic management of chronic low back pain–a randomized, blinded, controlled trial with 3 months follow up. Pain. 2002;99:579–587. doi: 10.1016/S0304-3959(02)00269-5. [DOI] [PubMed] [Google Scholar]
- 42.Pach D, Yang-Strobel X, Lüdtke R, et al. Standardized versus individualized acupuncture for chronic low back pain: a randomized controlled trial. Evid Based Complement Alternat Med. 2013;2013:125937. doi: 10.1155/2013/125937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Rajfur J, Pasternok M, Rajfur K, et al. Efficacy of selected electrical therapies on chronic low back pain: a comparative clinical pilot study. Med Sci Monit. 2017;23:85–100. doi: 10.12659/MSM.899461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Sator-Katzenschlager SM, Scharbert G, Kozek-Langenecker SA, et al. The short- and long-term benefit in chronic low back pain through adjuvant electrical versus manual auricular acupuncture. Anesth Analg. 2004;98:1359–1364. doi: 10.1213/01.ane.0000107941.16173.f7. [DOI] [PubMed] [Google Scholar]
- 45.Shankar N, Thakur M, Tandon OP, et al. Autonomic status and pain profile in patients of chronic low back pain and following electro acupuncture therapy: a randomized control trial. Indian J Physiol Pharmacol. 2011;55:25–36. [PubMed] [Google Scholar]
- 46.Szczurko O, Cooley K, Busse JW, et al. Naturopathic care for chronic low back pain: a randomized trial. PLoS ONE. 2007;2:e919. doi: 10.1371/journal.pone.0000919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Thomas KJ, MacPherson H, Thorpe L, et al. Randomised controlled trial of a short course of traditional acupuncture compared with usual care for persistent non-specific low back pain. BMJ. 2006;333:623. doi: 10.1136/bmj.38878.907361.7C. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Witt CM, Jena S, Selim D, et al. Pragmatic randomized trial evaluating the clinical and economic effectiveness of acupuncture for chronic low back pain. Am J Epidemiol. 2006;164:487–496. doi: 10.1093/aje/kwj224. [DOI] [PubMed] [Google Scholar]
- 49.Yeung CKN, Leung MCP, Chow DHK. The use of electro-acupuncture in conjunction with exercise for the treatment of chronic low-back pain. J Altern Complement Med. 2003;9:479–490. doi: 10.1089/107555303322284767. [DOI] [PubMed] [Google Scholar]
- 50.Tsui MLK, Cheing GLY. The effectiveness of electroacupuncture versus electrical heat acupuncture in the management of chronic low-back pain. J Altern Complement Med. 2004;10:803–809. doi: 10.1089/acm.2004.10.803. [DOI] [PubMed] [Google Scholar]
- 51.Tsukayama H, Yamashita H, Amagai H, et al. Randomised controlled trial comparing the effectiveness of electroacupuncture and TENS for low back pain: a preliminary study for a pragmatic trial. Acupunct Med. 2002;20:175–180. doi: 10.1136/aim.20.4.175. [DOI] [PubMed] [Google Scholar]
- 52.Weiss J, Quante S, Xue F, et al. Effectiveness and acceptance of acupuncture in patients with chronic low back pain: results of a prospective, randomized, controlled trial. J Altern Complement Med. 2013;19:935–941. doi: 10.1089/acm.2012.0338. [DOI] [PubMed] [Google Scholar]
- 53.Yoo D-J, Jung J-Y, Chung S-H. Effects of the embedding acupuncture treatments for chronic low back pain patients. J Korean Med Rehabilit. 2015;25:105–112. doi: 10.18325/jkmr.2015.25.4.105. [DOI] [Google Scholar]
- 54.Yuan J, Purepong N, Hunter RF, et al. Different frequencies of acupuncture treatment for chronic low back pain: an assessor-blinded pilot randomised controlled trial. Complement Ther Med. 2009;17:131–140. doi: 10.1016/j.ctim.2008.10.003. [DOI] [PubMed] [Google Scholar]
- 55.Yun M, Shao Y, Zhang Y, et al. Hegu acupuncture for chronic low-back pain: a randomized controlled trial. J Altern Complement Med. 2012;18:130–136. doi: 10.1089/acm.2010.0779. [DOI] [PubMed] [Google Scholar]
- 56.Zaringhalam J, Manaheji H, Rastqar A, et al. Reduction of chronic non-specific low back pain: a randomised controlled clinical trial on acupuncture and baclofen. Chin Med. 2010;5:15. doi: 10.1186/1749-8546-5-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Asano H, Plonka D, Weeger J. Effectiveness of acupuncture for nonspecific chronic low back pain: a systematic review and meta-analysis. Med Acupunct. 2022;34:96–106. doi: 10.1089/acu.2021.0057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Xiang Y, He J-Y, Tian H-H, et al. Evidence of efficacy of acupuncture in the management of low back pain: a systematic review and meta-analysis of randomised placebo- or sham-controlled trials. Acupunct Med. 2020;38:15–24. doi: 10.1136/acupmed-2017-011445. [DOI] [PubMed] [Google Scholar]
- 59.Nascimento PRCd, Costa LOP, Araujo AC, et al. Effectiveness of interventions for non-specific low back pain in older adults. Syst Rev Meta-Anal Physiother. 2019;105:147–162. doi: 10.1016/j.physio.2018.11.004. [DOI] [PubMed] [Google Scholar]
- 60.Foster NE, Vertosick EA, Lewith G, et al. Identifying patients with chronic pain who respond to acupuncture: results from an individual patient data meta-analysis. Acupunct Med. 2021;39:83–90. doi: 10.1177/0964528420920303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Mu J, Furlan AD, Lam WY, et al. Acupuncture for chronic nonspecific low back pain. Cochrane Database Syst Rev. 2020;12:CD013814. doi: 10.1002/14651858.CD013814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Li C, Pei Q, Chen Y, et al. The response-time relationship and covariate effects of acupuncture for chronic pain: a systematic review and model-based longitudinal meta-analysis. Eur J Pain. 2020;24:1653–1665. doi: 10.1002/ejp.1617. [DOI] [PubMed] [Google Scholar]
- 63.Su X, Qian H, Chen B, et al. Acupuncture for acute low back pain: a systematic review and meta-analysis. Ann Palliat Med. 2021;10:3924–3936. doi: 10.21037/apm-20-1998. [DOI] [PubMed] [Google Scholar]
- 64.Lee J-H, Choi T-Y, Lee MS, et al. Acupuncture for acute low back pain: a systematic review. Clin J Pain. 2013;29:172–185. doi: 10.1097/AJP.0b013e31824909f9. [DOI] [PubMed] [Google Scholar]
- 65.Madhusudhan SK. Novel analgesic combination of tramadol, paracetamol, caffeine and taurine in the management of moderate to moderately severe acute low back pain. J Orthop. 2013;10(3):144–8. doi: 10.1016/j.jor.2013.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Andrea De Giorgio, Padulo J, Goran K (2018) Effectiveness of yoga combined with back school program on anxiety, kinesiophobia and pain in people with non-specific chronic low back pain: a prospective randomized trial, 8: 104–112. 10.11138/mltj/2018.8.1.104
- 67.Dimer da Luz R, De Silva Silva M, Steffen Evaldt A, et al. Neuromuscular electrical stimulation associated with core stability exercises in nonspecific postural low back pain: a randomized clinical trial. Muscle Ligaments Tendons J. 2019;09:446. doi: 10.32098/mltj.03.2019.20. [DOI] [Google Scholar]
- 68.Depaoli Lemos VJ, Selau RC, Blos C, et al. Electroacupuncture and transcutaneous electrical nerve stimulation in chronic nonspecific low back pain: a blind randomized clinical trial. Muscle Ligaments Tendons J. 2021;11:719. doi: 10.32098/mltj.04.2021.15. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data underlying this article are available in the article and in its online supplementary material.