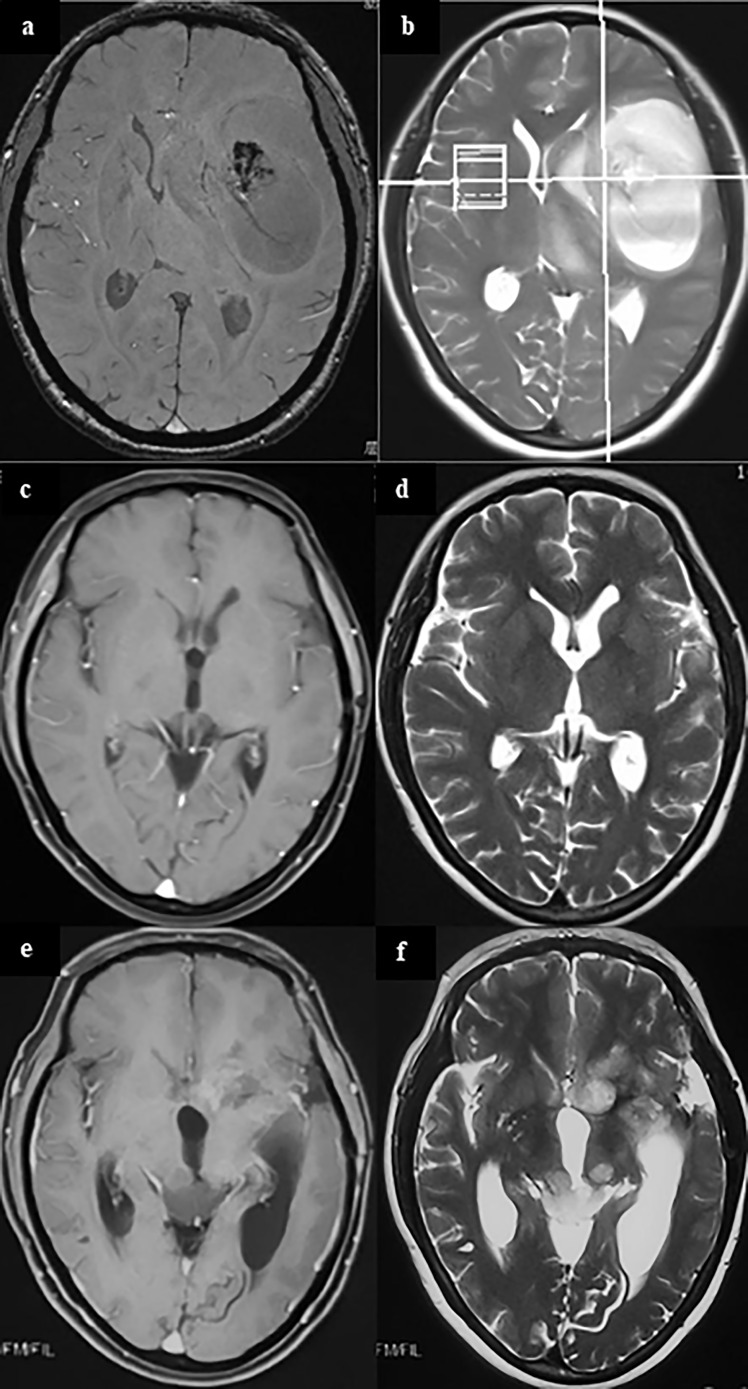
Figure 1.
A case of metachronous multicentric glioma. The patient underwent MRI for headache and found a tumor in the left temporal insula (A, B). She was given partial resection of the tumor. Pathology showed GBM. Local radiation and temozolomide based chemotherapy were given after surgery. The tumor completely regressed in MRI 1 year after surgery (C, D). However, in follow-up 1.5 years after surgery, it was found that the patient had a recurrent lesion in the left caudate head and insula, and an ectopic lesion in the midbrain tectum (E, F). On sequential T2 and FLAIR MR images, there was no connection between the lesion in the midbrain tectum and in the right basal ganglia. In addition, cytologic test of CSF and MR of the brain and spinal cord did not find there was any evidence of CSF dissemination. Therefore, the lesion in the midbrain tectum is considered as a metachronous multicentric glioma in contrast with the initial tumor. The patient underwent ventricular-abdominal shunt surgery to relieve hydrocephalus and was given temozolomide chemotherapy again. She is still under follow-up (21 months after tumor resection). (a,c,e, MRI of T1 enhanced signal; b, d, f, MRI of T2 signal).