Figure 1. Patients with BP exhibit an increased rate of Staphylococcus aureus colonization, and most of these isolates produce TSST-1.
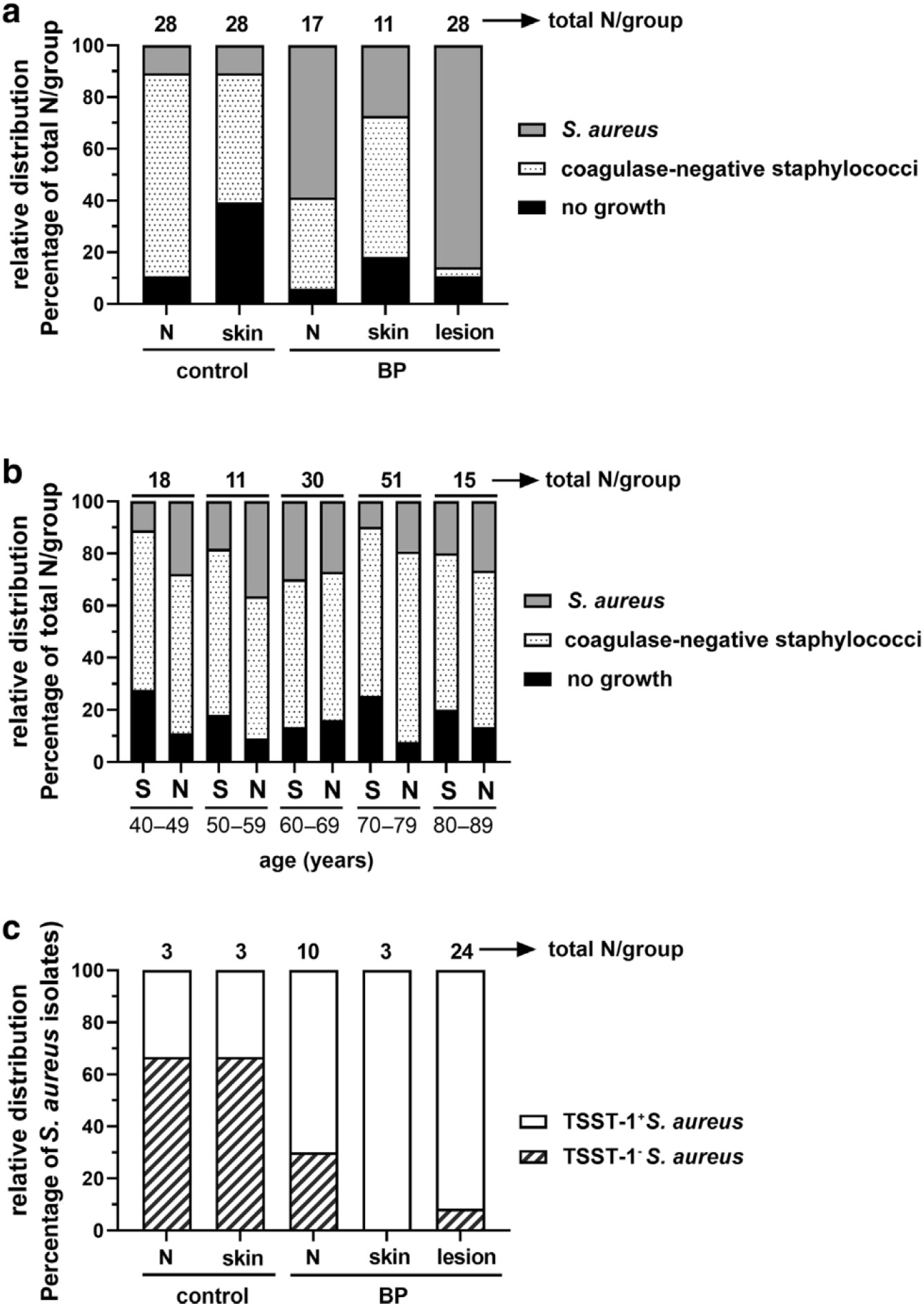
(a) Staphylococcal colonization was categorized as S. aureus (coagulase positive) or coagulase-negative staphylococci or no growth, and their relative distribution is shown as a percentage of the total number (above bars). BP lesions were six-fold more likely to be colonized by S. aureus than control Ns or S (Fisher’s exact test, 95% CI = 2.790–15.78, P < 0.0001). (b) Staphylococcal colonization of the S or Ns of 128 healthy individuals aged 40–99 years shows that bacterial distribution is not influenced by age (logistic regression models, AUC ~0.5). (c) Most S. aureus isolates from patients with BP produce TSST-1, whereas most of the control isolates do not. Using Fisher’s exact test, BP lesions were >4-fold more likely to be colonized by TSST-1+ S. aureus than control Ns (95% CI = 2.422–9.468, P < 0.0001) or S (95% CI = 2.215–9.144, P < 0.0001). AUC, area under the curve; BP, bullous pemphigoid; CI, confidence interval; N, nare; S, skin; TSST-1, toxic shock syndrome toxin-1.
