Abstract
Background
Ophthalmological disorders are common and frequently disabling for people with Parkinson’s disease (PD). However, details on the prevalence, severity and impact of ophthalmological disorders thus far lacking. We aimed to identify PD patients with undetected ophthalmological disorders in a large cross-sectional, observational study.
Methods
We previously delivered a screening questionnaire to detect ophthalmological symptoms (Visual impairment in PD questionnaire; VIPD-Q) to 848 patients. Here, we report on a subgroup of 102 patients who received complete ophthalmological assessment aimed at identifying clinically relevant ophthalmological diseases, which were classified as either vison-threatening or not. Impact on daily life functioning was measured using the visual functioning-25 questionnaire (VFQ-25) and fall frequency.
Results
Almost all patients (92%) had one or more clinically relevant ophthalmological disorders. Of those, 77% had a potentially vision-threatening disease, while 34% had a potentially treatable ophthalmological disease which impacted on quality of life. The most prevalent ophthalmological disorders were dry eyes (86%), ocular misalignment (50%) and convergence insufficiency (41%). We found a weak but significant association between clinically relevant ophthalmological diseases and both fall frequency (R2 = 0.15, p = 0.037) and VFQ-25 score (R2 = 0.15, p = 0.02). The VIPD-Q could not correctly identify patients with relevant ophthalmological disorders.
Conclusions
Surprisingly, in our study sample, many participants manifested previously undetected ophthalmological diseases, most of which threatened vision, impacted on daily life functioning and were amenable to treatment. Screening for these ophthalmological disorders using a questionnaire asking about symptoms seems insufficient. Instead, episodic ophthalmological assessments should be considered for PD patients, aiming to identify vision-threatening yet treatable diseases.
Trial registration
Dutch Trial Registration, NL7421.
Supplementary Information
The online version contains supplementary material available at 10.1007/s00415-022-11014-0.
Keywords: Parkinson’s disease, Ophthalmology, Ophthalmological disorders, Visual impairment, Non-motor symptoms
Introduction
Persons with Parkinson’s disease (PD) often experience ophthalmological problems, including burning eyes, visual field deficits or visual hallucinations [1, 2]. Ophthalmological symptoms are part of the non-motor symptoms of PD and are commonly observed early in the disease or even in prodromal stages [3–5]. These symptoms can result from a broad range of ophthalmological disorders, such as convergence insufficiency or decreased contrast or colour vision. Some are caused by retinal thinning and dysfunction due to retinal dopamine depletion [6–8]. Others might be age-related rather than linked to the degenerative process of PD itself, e.g. glaucoma, age-related macular degeneration or cataract [9–12]. Ophthalmological disorders, if not treated adequately, may negatively impact on physical activity, activities of daily living and quality of life [2, 13, 14]. Visual functioning seems extra important for PD patients because of their need to overcome loss of motor function with visual guidance [15]. For example, visual cueing is an established method to improve walking and reduce freezing of gait in PD, but this strategy is obviously less effective when patients cannot see the visual cues properly [16, 17].
In view of the above mentioned, ophthalmological disorders in PD have received surprisingly little interest in clinical practice and research. Earlier work compared ophthalmologic tests and ophthalmological symptoms, such as colour vision or diplopia, between PD patients and controls, but did not include a detailed search for underlying ophthalmological disorders [2, 14, 18, 19]. Therefore, little is known about the frequency, severity and impact of specific ophthalmological disorders in PD. Moreover, there is no guideline when and how to assess ophthalmological symptoms in daily practice, possibly delaying referrals to the ophthalmologist so patients are withheld effective treatments. Here, we aim to identify PD patients with undetected ophthalmological disorders, population prevalence, severity and impact of ophthalmological disorders in a convenience sample of PD patients.
Methods
Participants and setting
We performed a cross-sectional, observational study. The methodology has been detailed before [20]. Our initial study population consisted of a cohort of 848 PD patients who had completed the Visual Impairment in Parkinson’s Disease Questionnaire (VIPD-Q) [21]. Patients included in the present study were selected from this larger sample. Specifically, we selected candidates based on the order of submission of the VIPD-Q, until the number of 102 participants was reached. Selection bias may have been caused by the fact that we could only approach participants who had responded positively to a question in the questionnaire, asking whether we might contact the respondents for further research. In addition, the first responders may be the ones experiencing the greatest impact of ophthalmological disorders. However, our selected group showed a median of 13 points on the VIPD-Q and a range of 0–48 points. We included patients with a diagnosis of PD according to the UK Brain Bank criteria [22], age of PD onset older than 30 years, age at study inclusion of 60 years or older, and stable doses of dopaminergic replacement therapy for at least 4 weeks prior to the ophthalmological examination. Exclusion criteria included secondary causes of parkinsonism (e.g. vascular parkinsonism); prior brain surgery (except deep brain stimulation); history of systemic diseases (e.g. DM type I, or type II with diabetic retinopathy), other neurodegenerative diseases; medication influencing normal visual function; prior eye surgery except uncomplicated cataract surgery; blindness in one eye (i.e. blindness according to the WHO criteria, with visual acuity worse than 3/60) [23]; and presence of dementia or major depressive or psychotic disorder according to DSM IV. Between May 2017 and May 2019, a sample of 102 patients was enrolled for an extensive neurological and ophthalmological assessment at two university hospitals specialised in movement disorders (Radboudumc, Nijmegen, the Netherlands; and Medical University, Innsbruck, Austria). The study was performed in accordance with the declaration of Helsinki. Each study centre obtained local ethical approval. All the participants gave their written informed consent prior to participation.
Procedures and assessments
All assessments were performed while patients continued their regular medication. We obtained demographics and medical history, followed by a neurological and detailed ophthalmological assessment. For the complete list of examinations, see Supplementary 1.
Population prevalence and severity of ophthalmological disorders
We chose a pragmatic approach, first reviewing whether people with PD had any ophthalmological disease, based on the ophthalmological exams. We then evaluated the severity of ophthalmological diseases (based on the ophthalmological assessment). None and mild disease gradation were scored as “not clinically relevant” and moderate and severe as “clinically relevant”. This classification was based on a combination of literature and expert opinion and is depicted in detail in Supplementary file 2. The definition clinically relevant is a description of the severity of an ophthalmological disorder. This is not a grade of functional disability to a patient. Corneal diseases, blepharitis or manifest ocular misalignment were categorised as either present with or without clinically relevant manifestations, or absent. Congenital colour blindness, choroidal nevus, tilted disc, vascular changes of the retina, retinal degeneration and dermatochalasis were simply classified as either present or absent. Identified ophthalmological disorders were classified as vision threatening or not, as well as potentially treatable vs not. Potentially treatable/manageable disorders are: glaucoma, dry eyes, convergence insufficiency, ocular misalignments, cataract, vitreous haemorrhage, conjunctivitis, eyelids disorders, lens capsule opacification and cornea diseases.
Impact of ophthalmological disorders
The impact of ophthalmological disorders on daily activities was measured using the 25-item National Eye Institute Visual Function Questionnaire (VFQ-25) [24]. This questionnaire measures the influence of visual disability and visual symptoms on 11 generic health domains such as emotional well-being and social functioning, in addition to task-oriented domains related to daily visual functioning. A maximum score of 100 indicates perfect functioning in daily life. Composite scores of 10 domains of the VFQ-25 (without the domain driving) were categorised into four categories, from the highest scores to the lowest (100–81 = no impact, 80–61 = mild impact, 60–41 = moderate impact, 40–0 = severe impact) [24]. Moreover, we used fall frequency as an indicator for the impact of ophthalmological diseases on daily life activities. We asked participants how often they had experienced falls during the last 6 months preceding our study (categorised as either never, 1–2 × per month, weekly, or daily). We also explored if the VIPD-Q score could be related to quality of life.
The Visual impairment questionnaire (VIPD-Q)
The VIPD-Q was developed to detect a broad range of ophthalmological problems in PD [20]. The questionnaire consists of 17 questions on ophthalmological symptoms, categorised into four domains of ophthalmological disorders: (1) ocular surface; (2) intra-ocular; (3) oculomotor; and (4) optic nerve. Answers were given on a 4-point Likert scale ranging from “never had symptoms” to “daily symptoms”. Our published study protocol provides detailed information on the domains included in the VIPD-Q [20].
Statistical analysis
The baseline patient characteristics were expressed as means with standard deviation. Frequency distributions were calculated for all outcomes. Nonparametric variables were expressed as median, interquartile range (IQR) and minimum and maximum values. We compared characteristics of patients with and without vision-threatening diseases using the Student’s t test for parametric continuous variables and the Mann–Whitney U test for non-parametric continuous variables. The impact of ophthalmological diseases on daily life function (VFQ-25 total score, fall frequency) is assessed using linear regression with correction for age, Hoehn and Yahr stage, freezing of gait and disease duration. To evaluate the screening questionnaire, in terms of correctly identifying patients with ophthalmological disorders, we had originally planned to compare the results of the VIPD-Q with the outcomes of the ophthalmological assessments, using linear regression and receiver-operating characteristic (ROC) for the total score and the score per domain. We abstained from these analyses, because of the unexpectedly high prevalence of ophthalmological disorders in the PD population, making it impossible to compare patients with or without ophthalmological problems. All analyses were performed with SPSS 22.0 (SPSS Inc, IBM, Chicago, IL, USA).
Data availability statement
Requests for data from the VIP Study will be considered by B.R.B. in line with data protection laws. The general policy is that as long as the proposed use of the data is scientifically valid and if ethics approval permits, suitably anonymised data can be shared with other researchers.
Results
Participants
Patient characteristics are described in Table 1. There were no differences between patients with and without vision-threatening ophthalmological diseases concerning age, sex, disease duration, Levodopa-equivalent daily dose (LEDD), Hoehn and Yahr stages, cognitive function and motor examination.
Table 1.
Patients characteristics
| Demographicsa | PD patients (n = 102) |
|---|---|
| Age, median (IQR) [range], years | 68 (8) [60–68] |
| Men, n (%) | 69 (68) |
| Disease duration, median (IQR) [range], years | 6 (7) [0–19] |
| Hoehn and Yahr stage (SD) | 2 (0) [2–4] |
| Laterality (more affected body side), right: n (%) | 41 (41) |
| Schwab & England ADL scale (SD) | 84% (12) |
| Levodopa doses equivalent, median (IQR) [range], mg | 580 (605) [0–1950] |
| Polypharmacy, mean (SD), number of medications | 5 (3) |
| Education, College degree, n (%) | 28% (28) |
| Country of birth (European), n (%) | 101 (99) |
| Falls in the last month, n (%) | 25 (25) |
| Uses visual aid, n (%) | 99 (99) |
| Comorbidity | |
| Diabetes Mellitus type II, n (%) | 10 (10) |
| Hypertension, n (%) | 31 (30) |
| Cardiac arrest, n (%) | 9 (9) |
| Stroke, n (%) | 3 (3) |
| Rating scales | |
| MDS-UPDRS part III | 32 (13.7) |
| MDS-UPDRS total score | 54 (22) |
| Cognitive function assessment | |
| MoCA | 27.3 (2.7) |
| CLOX 1 | 14.2 (2.6) |
| GDS | 3.6 (2.8) |
| Questionnaires | |
| Visual function questionnaire-25 total score | 82% (12.9) |
| VIPD-Q total score, (range) | 13 (0–48) |
| NMSS (German version) (n = 72) | 40 (28) |
| NMSS (Dutch version) (n = 29) | 20 (5.3) |
| PDQ-39 | 23 (13.8) |
For MDS-UPDRS, GDS, VIPD-Q, NMSS, and PDQ-39, higher scores indicate worse functioning
For activities of daily living scale, VFQ-25, MoCA, and CLOX, lower scores indicate worse functioning
n number of participants, IQR interquartile range, PD Parkinson’s disease; Levodopa Equivalent dose (LED); activities of daily living scale according to the modified Schwab and England scale (score 0–100%), UPDRS MDS unified Parkinson’s disease rating scale (total score 0–236), UPDRS part III (score 0–132), MoCA Montreal Cognitive Assessment (score 0–30); CLOX clock drawing test (score 0–16); GDS geriatric depression scale (score 0–30); VFQ-25 visual function questionnaire-25 (score 0–100%); VIPD-Q Visual impairment in Parkinson’s disease questionnaire (score 0–51); NMSS non-motor symptoms scale (score 0–360), Dutch version (score 0–30); PDQ-39 the Parkinson’s disease questionnaire-39 (score 0–100)
aData shown as mean (SD) unless otherwise indicated
Prevalence and severity of ophthalmological disorders
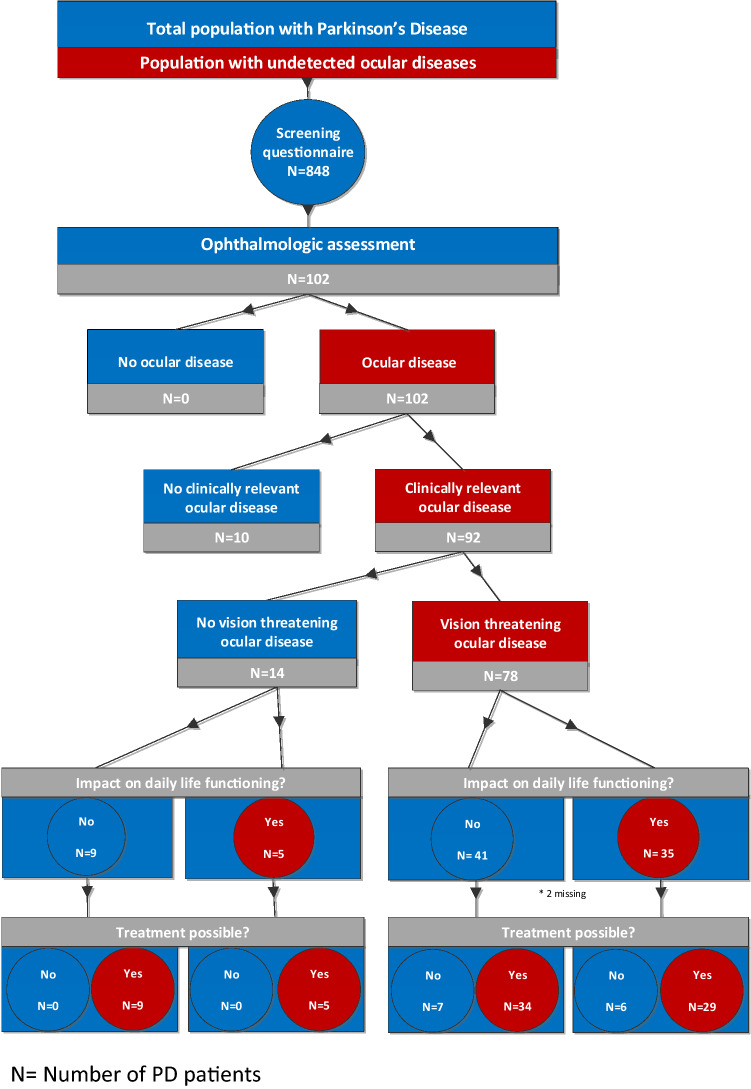
The results of the ophthalmological assessments are detailed in Table 2. The flowchart (Fig. 1) illustrates the frequency, severity, impact and treatability of the observed ophthalmological diseases. All participants had at least 1 ophthalmological disease, and 90 (92%) had an ophthalmological disease with clinical relevance; of these, 78 (77%) patients had a potentially vision-threatening ophthalmological disease. Thirty-four subjects (34%) of this subgroup had an ophthalmological disease which impacted on daily life functioning, and that could potentially be treated. Table 3 describes the prevalence of ophthalmological diseases per domain of the VIPD questionnaire. In 66% of participants, we found more than one clinically relevant ophthalmological disease, with a maximum of five different conditions. The most prevalent ophthalmological disorders were dry eyes (86%), ophthalmological misalignment (50%), optic nerve disorder (50%), convergence insufficiency (41%) and cataract (40%).
Table 2.
Ophthalmological assessment: outcomes
| Outcome | Ophthalmological Assessment a | PD patients (n = 102) | |
|---|---|---|---|
| Subjective ophthalmological assessment | OD mean (SD) | OS mean (SD) | |
| Best corrected visual acuity | LogMAR value | 0.06 (0.21) | 0.03 (0.16) |
| Snellen 20/25–20/10 (normal), % | 81% | 82% | |
| Snellen 20/32–20/63% | 12% | 11% | |
| Snellen 20/80–20/160, % | 1% | 2% | |
| Snellen worse than 20/200, % | 1% | 0% | |
| Visual acuity too low to drive (> 0.3 LogMAR) | 5% | 5% | |
| Reading | Reading speed, wpm, M:5 | 165 (49) | |
| Reading speed, wpm, M:0.25 (n = 12) | 73 (32) | ||
| Near visual acuity (LogMAR value) | 0.14 (.-0.20-0.50) | ||
| Snellen 20/25–20/10 (normal), % | 60% | ||
| Snellen 20/32–20/63,% | 39% | ||
| Snellen 20/80–20/160, % | 1% | ||
| Visual field | Humphrey field analyzer, MD (n = 30) | − 4.35 (4.6) | − 4.7 (5.5) |
| Octopus, MD (n = 71) | 5.3 (4.6) | 6.1 (4.8) | |
| Metamorphopsia | 13% | 18% | |
| Amsler grid (cannot see all corners/sides) | 7% | 8% | |
| Visual field deficit (moderate/severe) | 43% | 50% | |
| Contrast vision | Low-contrast letter charts (Pelli-Robson), CSS | 1.53 (0.20) | 1.52 (0.20) |
| Moderate/severe decreased (CSS < 1.50) | 40% | 50% | |
| Colour vision | Ishihara plates (range) | 18 (1–21) | 18 (1–21) |
| Farnsworth Munsell hue test (desaturated 15D) | |||
| Mild green blind | 2% | 6% | |
| Moderate/severe green blind | 3% | 3% | |
| Mild blue blind | 48% | 47% | |
| Moderate/severe blue blind | 24% | 26% | |
| Mild red blind | 2% | 4% | |
| Moderate/severe red blind | 5% | 6% | |
| Convergence | Near point of convergence, cm | 10.97 (0.28) | |
| Objective ophthalmological assessment | OD mean (SD) | OS mean (SD) | |
|---|---|---|---|
|
Cataract grading Lens opacity (LOCS III) |
Pseudophakia | 20% | 19% |
| NO (score 4 >) | 4% | 4% | |
| NC (score 4 >) | 4% | 4% | |
| Cortical (score 3 >) | 13% | 14% | |
| Subcapsular (score 3 >) | 2% | 0% | |
| Corneal thickness | Pachymetry, µm | 538.14 (48.84) | 533.75 (56.09) |
| Cornea appearance | Keratitis punctate/dry cornea | 10% (10) | 11% (11) |
| Cornea erosion/scarring | 3% (3) | 2% (2) | |
| Intra-ocular pressure | (Goldman) tonometry, mmHg | 14 (3.04) | 14 (2.76) |
| Tear production | Schirmer’s II test, mm | 9.86 (7.4) | 9.17 (4.31) |
| TFBUT, s | 9.0 (4.31) | 9.06 (4.37) | |
| Eye blink rate, blinks/minute | 15 (12.75) | ||
| Eyelids | Loss of lashes | 1% | 1% |
| Eye lid retraction | 1% | 1% | |
| Conjunctiva | Hyperaemia | 4% | 5% |
OD oculus dextra, OS oculus sinistra
BCVA best corrected visual acuity, in LogMAR. Normal value ≤ 0.10 LogMAR, or ≥ 20/25 Snellen visual acuity. Reading is assessed with the Radner reading chart. Wpm words per minute. Visual field is tested with the Humphrey and Octopus Automated Field Analyser in a standardised design. The mean deviation (MD) is notated. Lower MD score indicates for the Humphrey worse visual field deficit, normal value MD > 0. Higher MD score indicates for the Octopus worse visual field deficit, normal value MD ≤ -0.8
Pelli–Robson assessment consists of letters arranged in groups with varying contrast, from high to low, calculated in the CSS: contrast sensitivity score, (score 0–2.25)
To evaluate colour vision pseudo-isochromatic plates with coloured dots forming numbers (Ishihara plates) are used. Farnsworth desaturated 15D hue test is performed to evaluate subtler colour vision deficiencies. This task consists of ordering 15 coloured caps over trays in an incremental manner according to their hue
NPC near point of convergence in centimetre (cm)
To detect cataract the lens opacity is rated with the LOCSIII, Lens opacities classification system; NO nuclear opalescence (score 1–6), NC nuclear colour (score 1–6), Cortical (score 1–5), Posterior (score 1–5). Scores noted in table represent clinically relevant cataract
Cornea, eyelids and cornea are inspected. µm micrometre; IOP intra-ophthalmological pressure measured with applanation tonometry. Tear film quality is approached by the Tear-Film-Break-Up-Time (TFBUT), while the quantity of tears is measured by the Schirmer test. Schirmer II test, paper strips are inserted into the lower fornix with local anaesthesia, wet distance is measured in millimetres (mm), EBR eye blink rate is measured in blinks/minute
For NPC, LOCsIII and IOP higher scores indicate worse outcome
For visual acuity, CSS, Schirmer II, TFBUT and number of Ishihara plates lower scores indicate worse outcome
aData shown as mean (SD) unless otherwise indicated
Fig. 1.
Flowchart of the number of patients with PD and ophthalmological diseases. N = number of PD patients
Table 3.
Prevalence of ophthalmological disorders
| PD patients, age 60–86, n = 102 | OD (%) | OS (%) |
|---|---|---|
| Ocular surface | ||
| Cornea disease a | 6 | 6 |
| Blepharitis | 2 | 2 |
| Dermatochalasis | 13 | 14 |
| Conjunctivitis sicca (mild-severe) | 86 | 86 |
| Conjunctivitis sicca (moderate/severe) | 27 | 27 |
| Conjunctivitis | 4 | 5 |
| Oculomotor | ||
| Experiencing diplopia* | 30 | |
| Convergence insufficiency | 41 | 41 |
| Ocular misalignment | 54 | 50 |
| Manifest | 5 | 6 |
| Intra-ocular | ||
| Cataractb | 17 | 18 |
| Lens capsule opacification | 3 | 2 |
| Pseudophakia | 20 | 19 |
| Vitreous haemorrhage | 0 | 3 |
| Retina/optic nerve | ||
| Maculopathy c | 27 | 22 |
| AMD dry | 24 | 20 |
| AMD wet | 0 | 0 |
| Diabetic macular oedema | 0 | 0 |
| Optic nerve disorder d (n = 85/85) | 50 | 52 |
| Glaucoma suspect e | 20 | 15 |
| Elevated IOP | 1 | 1 |
| Retinopathy f | 2 | 1 |
| Retinal vascular changes | 23 | 28 |
| Peripheral drusen | 10 | 9 |
| Additional | ||
| Nevus choroid | 7 | 3 |
| Tilted disc | 7 | 4 |
| Congenital colour blindness g | 5 | |
| Visual Hallucinations | 18 | |
| Amblyopia | 3 |
OD oculus dextra, OS oculus sinistra
*Based on the VIPD-Q questionnaire. Not specifically during reading
aGroup of cornea diseases, consists of: cornea scar, verticillate, dystrophy (punctate/erosions are part of the diagnosis of dry eyes),
bCataract clinically significant, total percentage OD with cataract (present of historic):40%, OS: 39%
cGroup of macular diseases, consists of: AMD (age-related macular degeneration), scar, epiretinal gliosis, telangiectasia, macular oedema,
dGroup of optic nerve disorders consists of: optic nerve head drusen, optic nerve head atrophy, optic nerve head pallor
eGlaucoma suspects, CDR (cup-to-disc-ratio) > 0.5 and a typical visual field deficit, IOP intra-ophthalmological-pressure
fGroup of retinopathies consists of: branch retinal vein occlusion, blot bleeding,
gIn the study, population congenital colour blindness occurred in 7% of the men and 0% woman
Impact of ophthalmological diseases on daily life functioning and falling
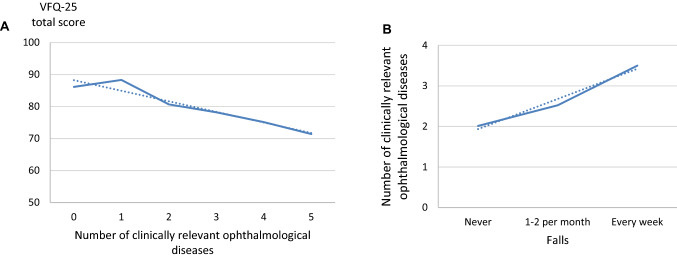
Ophthalmological diseases in PD patients impacted daily life functioning, as shown by the VFQ-25. Specifically, the mean total score of the VFQ-25 was 82% ± 12.9. Almost half of the PD patients (43%) reported functioning under the 80% threshold, indicating a negative effect on daily life functioning. The scores per domain are shown in Table 4. We found a weak but significant association between the VFQ-25 score and the number of clinically relevant ophthalmological diseases (R2 = 0.15, F3,93 = 5.165, p = 0.002, corrected for age and disease duration, Fig. 2A). In addition, a higher fall frequency was associated with a larger number of clinically relevant ophthalmological diseases (R2 = 0.15 F5,91 = 3.12, p = 0.037, corrected for age, Hoehn and Yahr stage, freezing of gait and disease duration, Fig. 2B).
Table 4.
Visual function questionnaire-25 scores
| VFQ Sub-Scale | PD patients n = 102 |
|---|---|
| (Mean ± SD) | |
| Composite score ** | 82 ± 13 |
| Role difficulties | 68 ± 28 |
| General vision | 77 ± 21 |
| Ocular pain | 78 ± 17 |
| Driving* | 78 ± 18 |
| Vision specific mental health | 81 ± 20 |
| Near activities | 82 ± 17 |
| Distance activities | 82 ± 17 |
| Peripheral vision | 88 ± 17 |
| Vision specific social functioning | 90 ± 14 |
| Vision specific dependency | 91 ± 20 |
| Colour vision | 94 ± 11 |
| General health | 68 ± 16 |
Subscale ordered highest to lowest impact
NEI VFQ-25 25-item National Eye Institute Visual Function Questionnaire 10 (maximum score, 100), SD = standard deviation
*39 subjects do not drive and were excluded from the driving subscale
**Composite score without driving
Fig. 2.
Impact of ophthalmological diseases. A Impact of clinically relevant ophthalmological diseases (grade moderate to severe) on the visual functioning-25 questionnaire (VFQ-25). A total score of 100 on the VFQ-25 indicates perfect functioning in daily life, lower scores relate to impaired function due to ophthalmological symptoms. Shown here is a decrease in the VFQ-25 total score with an increase in ophthalmological diseases. B The impact of ophthalmological diseases on the frequency of falls in the last half year. Patients tend to fall more often with an increased number of clinically relevant ophthalmological diseases
Discussion
In our study, ophthalmological disorders were common and debilitating among our sample of PD patients aged 60 years and older. Almost all people with PD had at least one clinically relevant ophthalmological disease (92%), and almost half of them (44%) reported impaired daily functioning because of these ophthalmological disorders. Importantly, many of these ophthalmological disorders were potentially treatable.
Population prevalence and severity of ophthalmological disorders
The high population prevalence of multiple ophthalmological diseases in our sample is noteworthy, particularly because little attention is typically paid to this issue in daily practice [25]. In the general population, approximately 80% of all causes of visual impairment are considered to be avoidable. Once a correct diagnosis has been established, many effective treatments are available [26]. Our present findings indicate that effective treatments are also available for many ophthalmological diseases in PD, especially dry eyes and cataract. Therefore, ophthalmological screening of PD patients is highly advisable.
From this analysis, keratoconjunctivitis sicca (dry eyes) was the most prevalent ophthalmological disease found in our PD population. Dry eyes was found in 86% of participants, which is much higher than reported previously (60%) [2, 14, 27]. This may be the result of our relatively old study population. Various factors may contribute to dry eyes in PD, including reduced eye blink rate, dysfunction of the sebaceous Meibomian glands, autonomic dysfunction and blepharitis [28–30]. Timely diagnosis and optimal treatment of dry eyes, e.g. with artificial tears, may increase the optical quality of the cornea and therefore improve the visual quality. Because of the high prevalence, standard treatment of patients with PD of 60 years and older with artificial tears could be considered.
Half of our study population had oculomotor deficits, which is a well-described feature in PD [31, 32]. Latent ocular misalignment or heterophoria, which is a subtle manifestation that can attribute to diplopia, was most frequent. While this has been described as an age-related symptom, we found a much higher prevalence in PD patients (50%) as compared to a healthy elderly population in the literature (15%) [33]. Earlier work shows that convergence insufficiency often contributes to diplopia [34]. We found convergence insufficiency in 41% of our population. Convergence ability deteriorates with age. However, it was more prevalent among PD patients than controls, both in on and off medication state [34, 35]. This suggests that ophthalmological fusional mechanisms are particularly vulnerable in PD. However, these problems can be effectively treated, for example with a prism or occupational therapy [36].
Retinal and optic nerve pathology was present in 30–50% of our study population. We found atrophy of the optic nerve head accompanied by optic nerve head pallor in half of the patients, mostly in the temporal quadrants. Optic nerve changes in PD are likely caused by primary neurodegeneration [37]. The retina and optic nerve head have drawn a lot of interest since the introduction of optical coherence tomography (OCT). The pattern of thinning of the retina and visual field deficit in PD seems to mimic that of glaucoma, with a relative sparing of the fibres entering the optic nerve head nasally [38–41]. Our data showed a much higher rate of possible glaucoma cases (17.5%) than may be expected for the general population (3.5%) [42]. Therefore we hypothesise that PD-related optic neurodegeneration may clinically mimic (normal pressure) glaucoma. In our cohort, there was only one patient with an increased intra-ophthalmological pressure. Previous studies reported a higher incidence of open-angle glaucoma in PD patients, suggesting a shared neurodegenerative process [11, 14, 43]. However, there is currently no reason to assume a significantly higher glaucoma risk for PD patients compared to healthy controls. We tried to evaluate if participants with optic nerve atrophy scored lower on the Visual Functioning questionnaire, indicating a disability in daily life functioning, however, this was not possible since almost all patient have next to an optic nerve atrophy a different ophthalmological disorder. Further research here is warranted which, to prevent possible overinterpretation and maybe unnecessary treatment of pseudo-glaucoma in PD.
Maculopathy was present in a quarter of our patients, with the most common cause being age-related macular degeneration (AMD). Only one other study reported the prevalence of AMD in PD, which was lower compared to our data [14], possibly because of a younger patient cohort. Intriguingly, two studies reported an increased risk of a new diagnosis of PD when AMD was previously diagnosed [9, 10]. We speculate that the underlying pathology of both diseases may contain some similarities, although the only known overlapping factor is an increase of prevalence with ageing [10].
Impact of ophthalmological disorders on daily life functioning
Non-motor symptoms such as ophthalmological disorders can be as debilitating as motor symptoms in PD and contribute significantly to a poor quality of life [31, 44]. In our study, 44% of patients with relevant ophthalmological diseases reported that their visual disability influenced their daily functioning negatively (mean VFQ composite score 82). This is also reflected by the correlation between a lower VFQ total score and a higher number of clinically relevant ophthalmological disorders. Even though this correlation was weak, the combined results indicate that vision-related quality of life may be worse in PD subjects with more clinically relevant ophthalmological diseases. The most impaired subscales of the VFQ-25 were ocular pain, general vision, near visual activities, and peripheral vision. These findings are consistent with our results of the most common ophthalmological disorders. For example, dry eyes may cause ocular pain and general vision problems. Only one small earlier study, studied vision-related quality of life in PD with the VFQ-25. A worse composite score was found in PD patients compared to controls (VFQ composite score of 96 n = 16 vs 87, n = 27) [35]. Unfortunately, this study did not consider dry eyes as a contributor for impaired quality of life. Other studies on vision-related quality of life focussed on the impact of single ophthalmological symptoms, such as contrast sensitivity or visuospatial disruption. They found that these contributed to difficulties performing daily life activities, such as driving, walking and reading [1, 45, 46].
Ophthalmological diseases might contribute to frequent falling and necessitate reductions in physical activity. Established risk factors for falling in PD mainly include motor features, such as freezing of gait or balance impairment [47]. The possible contribution of non-motor symptoms, such as ophthalmological problems, has been studied in much less detail. Among our patients, 25% reported at least one fall in the last 6 months. A higher fall frequency was associated with a greater number of clinically relevant ophthalmological diseases, even when corrected for age, disease duration, freezing of gait and Hoehn and Yahr stage. This suggests that patients with an accumulation of clinically relevant ophthalmological diseases tend to fall more often. Since recurrent falls are considered to be a clinical milestone in PD that increase the risk of e.g. nursing home admission and mortality, this is an important finding [15], particularly because several ophthalmological disorders can be treated, thus helping to prevent at least some of the future falls. Nevertheless, our findings should be interpreted with caution, since the group of fallers in this study was small (n = 25) and also because the effect size is relatively small, which may lead to an overestimation of the outcome. Moreover, we did not specify the reason of falling and there is a potential recall bias. The key point is that ophthalmological issues should be considered among the many different factors that jointly contribute to the risk of falls. Pending further evidence, we do recommend that frequent fallers should be thoroughly screened for presence of ophthalmological disorders, using a detailed ophthalmologic examination focussing in particular on the common ophthalmological disorders identified here. Future intervention study should demonstrate whether adequate treatment of any identified ophthalmological disorders will help to reduce the risk of falls and enhance the independency of PD patients.
Value of a screening questionnaire
Since all ophthalmological diseases that we detected were potentially relevant and since all could have justified a referral to an ophthalmologist, the VIPD-Q in its current form does not seem to be of additional value to initiate an effective referral for ophthalmologic screening. Every patient had at least one ophthalmological disease, even those patients who scored zero points on the VIPD-Q (indicating no ophthalmological symptoms). Therefore, it was not possible to find a cutoff point to identify those patients with more than one ophthalmological disorder. This finding may be explained by several factors. First, patients may be unaware of ophthalmological symptoms. Some ophthalmological diseases have an asymptomatic progression until a very late stage (e.g. glaucoma) [48]. In older adults, visual impairment is often unrecognised, because visual changes can be relatively subtle, progress slowly over time, or occur in persons with concurrent cognitive dysfunction [48]. Therefore, actual ophthalmological disease may be difficult to screen using a questionnaire on problems. Moreover, patients may focus in particular on their motor symptoms without paying attention to their sight, so many ophthalmological problems are not volunteered during routine clinical consultations [49].
Limitations
Our study had certain limitations. First, because we did not have a control group, it is unclear if the observed prevalence rates of specific ophthalmological disorders for PD patients are truly different from the general population. The prevalence numbers observed here are specific to our present study population, and we do not know if these are generalizable to the complete population of people with PD. As such, our current findings can only be interpreted as a first indication that relevant ophthalmological problems may be commonly overlooked in daily clinical practice. Determining the true prevalence of this issue requires further study.
In the ophthalmologic literature, prevalence data are mostly categorised for specific age groups; therefore, it was difficult to compare the population prevalence of the ophthalmological disorders in our cohort to those reported in the literature. We acknowledge that selection bias may have been caused by the fact the first responders may be the ones experiencing the greatest impact of ophthalmological disorders, although the scores on the VIPD-Q showed a large range of 0–48 with a median of 13 points and the median score was 10 (range 0–48) in the total group of 848 responders. Second, we planned to compare patients with and without ophthalmological disorders, but the group without an ophthalmological disease was very small. Therefore, a comparison was not possible. A third limitation is the challenge to replicate a normal clinical ophthalmological practice within a research setting. We tried to minimise this using a strict protocol and expert assessment.
Future perspective
Further efforts are needed to develop improved screening tools to timely detect (and subsequently treat) ophthalmological disorders in PD patients, before they deteriorate further and begin to impact on daily functioning. One possibility is to improve the present VIPD-Q, for example by adding questions about the severity of ophthalmological problems. Until more reliable screening tools are available, we recommend that clinicians consider an episodic routine screening of people with PD by an ophthalmologist. However, we did not study the possible effects of routine screening by an ophthalmologist. Future research should study these effects, in addition to focussing on identifying the optimal moment, interval rate (ophthalmological disorders may become more prevalent as PD progresses and as patients grow older), and method of screening.
Of other great interest is the optic nerve atrophy and possible retinal thinning pattern. Recently, several studies have focussed on this issue [38–41]. Parkinson patients show an optic nerve atrophy and retinal thinning pattern, which resembles the retinal patterns in glaucoma patients and different neurodegenerative diseases, like Alzheimer’s disease. The question remains if this pattern could play a role as a possible biomarker. To solve that question, in depth longitudinal analyses are needed, with detailed clinical descriptions of the separate syndromes, which should dictate future research on this topic.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
The Center of Expertise for Parkinson & Movement Disorders was supported by a center of excellence grant by the Parkinson Foundation. We thank the patients and their families, without whose generous donation and support none of this research would have been possible. No compensation from a funding source was received.
Author contributions
CDJMB had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. CDJMB: design and conceptualised study; major role in the acquisition of data; analysed the data; drafted the manuscript for intellectual content. MW: design and conceptualised study; major role in the acquisition of data. DdG: major role in the acquisition of data. FV: major role in the acquisition of data. MP: major role in the acquisition of data; revised the manuscript for intellectual content. AH: major role in the acquisition of data. KlS: conceptualised study; interpreted the data; revised the manuscript for intellectual content. KaS: major role in the acquisition of data; revised the manuscript for intellectual content. DP: interpreted the data; revised the manuscript for intellectual content. WP: conceptualised study; interpreted the data; revised the manuscript for intellectual content. CH: interpreted the data; revised the manuscript for intellectual content. BB: conceptualised study; interpreted the data; revised the manuscript for intellectual content. TT: interpreted the data; revised the manuscript for intellectual content. NdV: conceptualised study; interpreted the data; revised the manuscript for intellectual content.
Funding
This study is funded by a research Grant from the Stichting Parkinson Fonds (Grant Number 38000). The funding source had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Declarations
Conflicts of interest
Drs. Borm: reports no disclosures. Drs. Werkmann: reports no disclosures. Drs. De Graaf: reports no disclosures. Drs. Visser: reports no disclosures. A. Hofer: reports no disclosures. Drs. Peball: is an employee of the Medical University Innsbruck and reports travel grants from the International Parkinson’s disease and Movement Disorder Society and the Austrian Parkinson’s Disease Society. Dr. Smilowska: reports research fellowship from European Academy of Neurology. Dr. Putz: reports no disclosures. Prof. Seppi: reports personal fees from Teva, UCB, Lundbeck, AOP Orphan Pharmaceuticals AG, Roche, Grünenthal and Abbvie, honoraria from the International Parkinson and Movement Disorders Society, research grants from FWF Austrian Science Fund, Michael J. Fox Foundation, and International Parkinson and Movement Disorder Society, outside the submitted work. Prof. Poewe: reports no disclosures. Prof. Hoyng: reports no disclosures. Prof. Bloem: Dr Bloem reports grants from the Michael J. Fox Foundation, ZonMw, Stichting Parkinson Nederland, Parkinson Vereniging, Hersenstichting Nederland, Parkinson’s Foundation, Verily Life Sciences, Horizon 2020, and Topsector Life Sciences and Health; grants and personal fees from UCB; and personal fees from Abbvie, Bial, and Zambon, outside the submitted work. Dr. Theelen: reports no disclosures. Dr. De Vries: reports grants from ZonMw and The Michael J Fox Foundation. No other disclosures were reported.
Ethics approval
The Medical Ethics Committee Arnhem-Nijmegen (NL58535.091.16) and Innsbruck (AN2016–0181) approved the study.
References
- 1.Davidsdottir S, Cronin-Golomb A, Lee A. Visual and spatial symptoms in Parkinson's disease. Vision Res. 2005;45:1285–1296. doi: 10.1016/j.visres.2004.11.006. [DOI] [PubMed] [Google Scholar]
- 2.Biousse V, Skibell BC, Watts RL, Loupe DN, Drews-Botsch C, Newman NJ. Ophthalmologic features of Parkinson's disease. Neurology. 2004;62:177–180. doi: 10.1212/01.WNL.0000103444.45882.D8. [DOI] [PubMed] [Google Scholar]
- 3.Weil RS, Schrag AE, Warren JD, Crutch SJ, Lees AJ, Morris HR. Visual dysfunction in Parkinson's disease. Brain. 2016 doi: 10.1093/brain/aww175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Turcano P, Chen JJ, Bureau BL, Savica R. Early ophthalmologic features of Parkinson's disease: a review of preceding clinical and diagnostic markers. J Neurol. 2018 doi: 10.1007/s00415-018-9051-0. [DOI] [PubMed] [Google Scholar]
- 5.Hamedani AG, Willis AW. Self-reported visual dysfunction in Parkinson disease: the survey of health, ageing and retirement in Europe. Eur J Neurol. 2020;27:484–489. doi: 10.1111/ene.14092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Archibald NK, Clarke MP, Mosimann UP, Burn DJ. The retina in Parkinson's disease. Brain. 2009;132:1128–1145. doi: 10.1093/brain/awp068. [DOI] [PubMed] [Google Scholar]
- 7.Nguyen-Legros J. Functional neuroarchitecture of the retina: hypothesis on the dysfunction of retinal dopaminergic circuitry in Parkinson's disease. Surg Radiol Anat. 1988;10:137–144. doi: 10.1007/BF02307822. [DOI] [PubMed] [Google Scholar]
- 8.Ahn J, Lee JY, Kim TW, Yoon EJ, Oh S, Kim YK, Kim JM, Woo SJ, Kim KW, Jeon B. Retinal thinning associates with nigral dopaminergic loss in de novo Parkinson disease. Neurology. 2018 doi: 10.1212/WNL.0000000000006157. [DOI] [PubMed] [Google Scholar]
- 9.Chung SD, Ho JD, Hu CC, Lin HC, Sheu JJ. Increased risk of Parkinson disease following a diagnosis of neovascular age-related macular degeneration: a retrospective cohort study. Am J Ophthalmol. 2014;157:464–469. doi: 10.1016/j.ajo.2013.09.026. [DOI] [PubMed] [Google Scholar]
- 10.Etminan M, Samii A, He B. Risk of Parkinson's disease in patients with neovascular age-related macular degeneration. J Curr Ophthalmol. 2018;30:365–367. doi: 10.1016/j.joco.2018.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bayer AU, Keller ON, Ferrari F, Maag KP. Association of glaucoma with neurodegenerative diseases with apoptotic cell death: Alzheimer's disease and Parkinson's disease. Am J Ophthalmol. 2002;133:135–137. doi: 10.1016/S0002-9394(01)01196-5. [DOI] [PubMed] [Google Scholar]
- 12.Klettner A, Richert E, Kuhlenbaumer G, Nolle B, Bhatia KP, Deuschl G, Roider J, Schneider SA. Alpha synuclein and crystallin expression in human lens in Parkinson's disease. Mov Disord. 2016;31:600–601. doi: 10.1002/mds.26557. [DOI] [PubMed] [Google Scholar]
- 13.Archibald NK, Clarke MP, Mosimann UP, Burn DJ. Visual symptoms in Parkinson's disease and Parkinson's disease dementia. Mov Disord. 2011;26:2387–2395. doi: 10.1002/mds.23891. [DOI] [PubMed] [Google Scholar]
- 14.Nowacka B, Lubinski W, Honczarenko K, Potemkowski A, Safranow K. Ophthalmological features of Parkinson disease. Med Sci Monit. 2014;20:2243–2249. doi: 10.12659/MSM.890861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wood BH, Bilclough JA, Bowron A, Walker RW. Incidence and prediction of falls in Parkinson's disease: a prospective multidisciplinary study. J Neurol Neurosurg Psychiatry. 2002;72:721–725. doi: 10.1136/jnnp.72.6.721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nonnekes E, Jr, Nieuwboer A, Hallett M, Fasano A, Bloem B. Compensation strategies for gait impairments in Parkinson disease. JAMA Neurol. 2019 doi: 10.1001/jamaneurol.2019.0033. [DOI] [PubMed] [Google Scholar]
- 17.Ginis P, Nackaerts E, Nieuwboer A, Heremans E. Cueing for people with Parkinson's disease with freezing of gait: a narrative review of the state-of-the-art and novel perspectives. Ann Phys Rehabil Med. 2018;61:407–413. doi: 10.1016/j.rehab.2017.08.002. [DOI] [PubMed] [Google Scholar]
- 18.Uc EY, Rizzo M, Anderson SW, Qian S, Rodnitzky RL, Dawson JD. Visual dysfunction in Parkinson disease without dementia. Neurology. 2005;65:1907–1913. doi: 10.1212/01.wnl.0000191565.11065.11. [DOI] [PubMed] [Google Scholar]
- 19.Chaudhuri KR, Martinez-Martin P, Schapira AH, Stocchi F, Sethi K, Odin P, Brown RG, Koller W, Barone P, MacPhee G, Kelly L, Rabey M, MacMahon D, Thomas S, Ondo W, Rye D, Forbes A, Tluk S, Dhawan V, Bowron A, Williams AJ, Olanow CW. International multicenter pilot study of the first comprehensive self-completed nonmotor symptoms questionnaire for Parkinson's disease: the NMSQuest study. Mov Disord. 2006;21:916–923. doi: 10.1002/mds.20844. [DOI] [PubMed] [Google Scholar]
- 20.Borm C, Werkmann M, Visser F, Peball M, Putz D, Seppi K, Poewe W, Notting IC, Vlaar A, Theelen T, Hoyng C, Bloem BR, de Vries NM. Towards seeing the visual impairments in Parkinson's disease: protocol for a multicentre observational, cross-sectional study. BMC Neurol. 2019;19:141. doi: 10.1186/s12883-019-1365-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Borm C, Visser F, Werkmann M, de Graaf D, Putz D, Seppi K, Poewe W, Vlaar AMM, Hoyng C, Bloem BR, Theelen T, de Vries NM. Seeing ophthalmologic problems in Parkinson disease: results of a visual impairment questionnaire. Neurology. 2020 doi: 10.1212/WNL.0000000000009214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gelb DJ, Oliver E, Gilman S. Diagnostic criteria for Parkinson disease. Arch Neurol. 1999;56:33–39. doi: 10.1001/archneur.56.1.33. [DOI] [PubMed] [Google Scholar]
- 23.WHOLoOI-UI-U (2006) http://www.who.int/classifications/icd/2006updates.pdf RO, 2015).
- 24.Mangione CM, Lee PP, Gutierrez PR, Spritzer K, Berry S, Hays RD, National Eye Institute Visual Function Questionnaire Field Test I Development of the 25-item national eye institute visual function questionnaire. Arch Ophthalmol. 2001;119:1050–1058. doi: 10.1001/archopht.119.7.1050. [DOI] [PubMed] [Google Scholar]
- 25.Ekker MS, Janssen S, Seppi K, Poewe W, de Vries NM, Theelen T, Nonnekes J, Bloem BR. Ocular and visual disorders in Parkinson's disease: common but frequently overlooked. Parkinsonism Relat Disord. 2017;40:1–10. doi: 10.1016/j.parkreldis.2017.02.014. [DOI] [PubMed] [Google Scholar]
- 26.Pascolini D, Mariotti SP. Global estimates of visual impairment: 2010. Br J Ophthalmol. 2012;96:614–618. doi: 10.1136/bjophthalmol-2011-300539. [DOI] [PubMed] [Google Scholar]
- 27.Lemp MA. The definition and classification of dry eye disease: report of the definition and classification subcommittee of the international dry eye workshop (2007) Ocul Surf. 2007;5:75–92. doi: 10.1016/S1542-0124(12)70081-2. [DOI] [PubMed] [Google Scholar]
- 28.Milner MS, Beckman KA, Luchs JI, Allen QB, Awdeh RM, Berdahl J, Boland TS, Buznego C, Gira JP, Goldberg DF, Goldman D, Goyal RK, Jackson MA, Katz J, Kim T, Majmudar PA, Malhotra RP, McDonald MB, Rajpal RK, Raviv T, Rowen S, Shamie N, Solomon JD, Stonecipher K, Tauber S, Trattler W, Walter KA. Dysfunctional tear syndrome: dry eye disease and associated tear film disorders—new strategies for diagnosis and treatment. Curr Opin Ophthalmol. 2017;27(Suppl 1):3–47. doi: 10.1097/01.icu.0000512373.81749.b7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kwon OY, Kim SH, Kim JH, Kim MH, Ko MK. Schrimer test in Parkinson's disease. J Korean Med Sci. 1994;9:239–242. doi: 10.3346/jkms.1994.9.3.239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Borm C, Smilowska K, de Vries NM, Bloem BR, Theelen T. How I do it: the neuro-ophthalmological assessment in Parkinson's disease. J Parkinsons Dis. 2019;9:427–435. doi: 10.3233/JPD-181523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chaudhuri KR, Odin P, Antonini A, Martinez-Martin P. Parkinson's disease: the non-motor issues. Parkinsonism Relat Disord. 2011;17:717–723. doi: 10.1016/j.parkreldis.2011.02.018. [DOI] [PubMed] [Google Scholar]
- 32.Visser F, Vlaar AMM, Borm C, Apostolov V, Lee YX, Notting IC, Weinstein HC, Berendse HW. Diplopia in Parkinson's disease: visual illusion or oculomotor impairment? J Neurol. 2019 doi: 10.1007/s00415-019-09430-w. [DOI] [PubMed] [Google Scholar]
- 33.Leat SJ, Chan LL, Maharaj PD, Hrynchak PK, Mittelstaedt A, Machan CM, Irving EL. Binocular vision and eye movement disorders in older adults. Invest Ophthalmol Vis Sci. 2013;54:3798–3805. doi: 10.1167/iovs.12-11582. [DOI] [PubMed] [Google Scholar]
- 34.Lepore FE. Parkinson's disease and diplopia. Neuro-Ophthalmology. 2006;30:37–40. doi: 10.1080/01658100600742838. [DOI] [Google Scholar]
- 35.Almer Z, Klein KS, Marsh L, Gerstenhaber M, Repka MX. Ocular motor and sensory function in Parkinson's disease. Ophthalmology. 2012;119:178–182. doi: 10.1016/j.ophtha.2011.06.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Savitt J, Mathews M. Treatment of visual disorders in Parkinson disease. Curr Treat Options Neurol. 2018;20:30. doi: 10.1007/s11940-018-0519-0. [DOI] [PubMed] [Google Scholar]
- 37.Pilat A, McLean RJ, Proudlock FA, Maconachie GD, Sheth V, Rajabally YA, Gottlob I. In vivo morphology of the optic nerve and retina in patients with Parkinson's disease. Invest Ophthalmol Vis Sci. 2016;57:4420–4427. doi: 10.1167/iovs.16-20020. [DOI] [PubMed] [Google Scholar]
- 38.Chrysou A, Jansonius NM, van Laar T. Retinal layers in Parkinson's disease: a meta-analysis of spectral-domain optical coherence tomography studies. Parkinsonism Relat Disord. 2019 doi: 10.1016/j.parkreldis.2019.04.023. [DOI] [PubMed] [Google Scholar]
- 39.Yenice O, Onal S, Midi I, Ozcan E, Temel A, D IG, Visual field analysis in patients with Parkinson's disease. Parkinsonism Relat Disord. 2008;14:193–198. doi: 10.1016/j.parkreldis.2007.07.018. [DOI] [PubMed] [Google Scholar]
- 40.Yu JG, Feng YF, Xiang Y, Huang JH, Savini G, Parisi V, Yang WJ, Fu XA. Retinal nerve fiber layer thickness changes in Parkinson disease: a meta-analysis. PLoS ONE. 2014;9:e85718. doi: 10.1371/journal.pone.0085718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Matlach J, Wagner M, Malzahn U, Schmidtmann I, Steigerwald F, Musacchio T, Volkmann J, Grehn F, Gobel W, Klebe S. Retinal changes in Parkinson's disease and glaucoma. Parkinsonism Relat Disord. 2018 doi: 10.1016/j.parkreldis.2018.06.016. [DOI] [PubMed] [Google Scholar]
- 42.Tham YC, Li X, Wong TY, Quigley HA, Aung T, Cheng CY. Global prevalence of glaucoma and projections of glaucoma burden through 2040: a systematic review and meta-analysis. Ophthalmology. 2014;121:2081–2090. doi: 10.1016/j.ophtha.2014.05.013. [DOI] [PubMed] [Google Scholar]
- 43.Ramirez AI, de Hoz R, Salobrar-Garcia E, Salazar JJ, Rojas B, Ajoy D, Lopez-Cuenca I, Rojas P, Trivino A, Ramirez JM. The role of microglia in retinal neurodegeneration: Alzheimer's disease, Parkinson, and glaucoma. Front Aging Neurosci. 2017;9:214. doi: 10.3389/fnagi.2017.00214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Witjas T, Kaphan E, Azulay JP, Blin O, Ceccaldi M, Pouget J, Poncet M, Cherif AA. Nonmotor fluctuations in Parkinson's disease: frequent and disabling. Neurology. 2002;59:408–413. doi: 10.1212/WNL.59.3.408. [DOI] [PubMed] [Google Scholar]
- 45.Amick MM, Grace J, Ott BR. Visual and cognitive predictors of driving safety in Parkinson's disease patients. Arch Clin Neuropsychol. 2007;22:957–967. doi: 10.1016/j.acn.2007.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Worringham CJ, Wood JM, Kerr GK, Silburn PA. Predictors of driving assessment outcome in Parkinson's disease. Mov Disord. 2006;21:230–235. doi: 10.1002/mds.20709. [DOI] [PubMed] [Google Scholar]
- 47.van der Marck MA, Klok MP, Okun MS, Giladi N, Munneke M, Bloem BR, Force NPFFT. Consensus-based clinical practice recommendations for the examination and management of falls in patients with Parkinson's disease. Parkinsonism Relat Disord. 2014;20:360–369. doi: 10.1016/j.parkreldis.2013.10.030. [DOI] [PubMed] [Google Scholar]
- 48.Chou R, Dana T, Bougatsos C, Grusing S, Blazina I. Screening for impaired visual acuity in older adults: updated evidence report and systematic review for the US preventive services task force. JAMA. 2016;315:915–933. doi: 10.1001/jama.2016.0783. [DOI] [PubMed] [Google Scholar]
- 49.Chaudhuri KR, Prieto-Jurcynska C, Naidu Y, Mitra T, Frades-Payo B, Tluk S, Ruessmann A, Odin P, Macphee G, Stocchi F, Ondo W, Sethi K, Schapira AH, Martinez Castrillo JC, Martinez-Martin P. The nondeclaration of nonmotor symptoms of Parkinson's disease to health care professionals: an international study using the nonmotor symptoms questionnaire. Mov Disord. 2010;25:704–709. doi: 10.1002/mds.22868. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Requests for data from the VIP Study will be considered by B.R.B. in line with data protection laws. The general policy is that as long as the proposed use of the data is scientifically valid and if ethics approval permits, suitably anonymised data can be shared with other researchers.