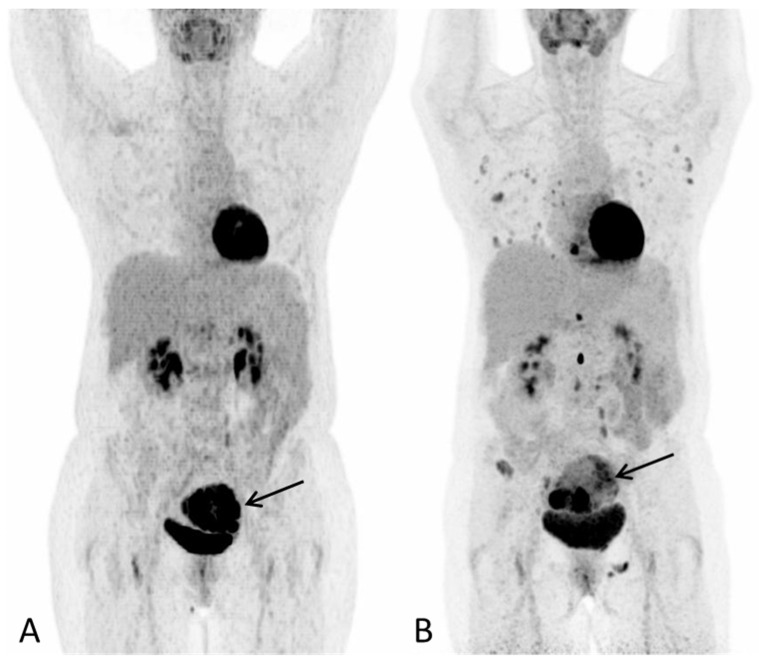
Figure 1.
A 57-year-old post-menopausal woman underwent gynecological examination due to intermittent vaginal bleeding over the course of one month with no other symptoms. On transvaginal ultrasound, a tumor thought to represent a leiomyoma was reported. A subsequent hysteroscopy showed the uterine cavity to be filled with soft necrotic tissue, suspected to derive from a leiomyoma. However, histological examination depicted hepatoid adenocarcinoma. At the time of diagnosis, the laboratory work-up for tumor markers showed S-AFP 110610 (ref: <12 kIU/L), Ca-125 13 (ref: <35 kU/L), CA 19-9 17 (ref: <37 kU/L) and CEA 4 (ref: <5µg/L). 18F-FDG PET/CT was performed for staging purposes. (A) PET Maximum intensity projection (MIP) baseline scan and (B) PET MIP evaluation scan after three series of chemotherapy (paclitaxel and carboplatin) showed progression with multiple new metabolic active lesions in the lungs, bones and lymph nodes. The primary tumour in the uterus is seen with increasing inhomogeneous metabolic activity, with areas of low metabolic activity indicating necrosis ((A,B), arrow). Notably, there were no FDG-avid lesions in the liver on either scan. S-AFP had risen to 258,900 IU/L. Due to progression, the treatment plan changed to sorafenib, which is one of the few systemic treatment options available for advanced HCC.