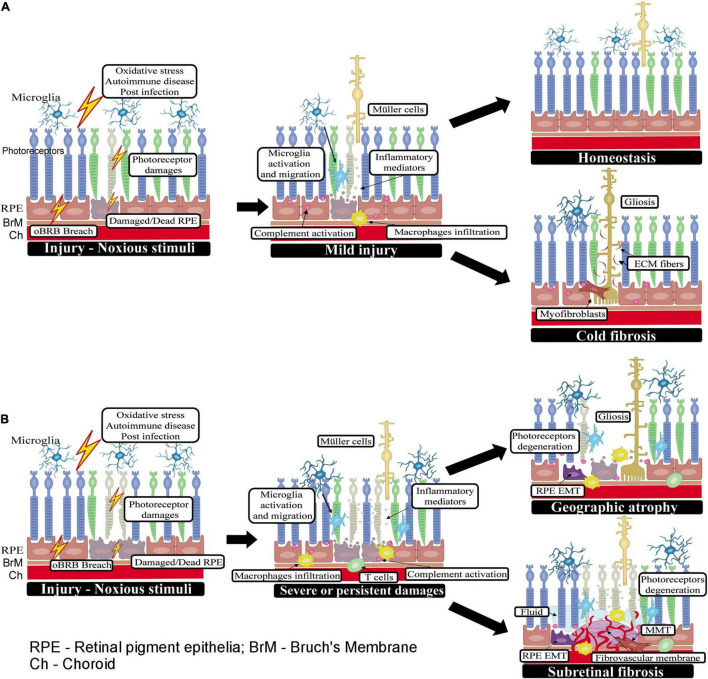
FIGURE 1.
Wound healing in the subretinal space. (A) When the initial insult is mild or one-off, the injury can be promptly rectified by retinal innate immune system (may also be assisted by infiltrating innate immune cells) and the subretinal space returns to homeostasis. If the injury causes a significant number of photoreceptor loss, Müller cells will be activated (may also be transdifferentiated into myofibroblast). Muller cells, myofibroblasts along with ECM proteins produced by them will fill the space left by dead cells forming gliosis without ongoing inflammation (or cold fibrosis). (B) When the insult to photoreceptors or RPE cells persists or is severe, retinal immune system, circulating innate and adaptive immune cells may all participate in the healing process. If the subretinal damage does not involve the ingrowth of new blood vessels, such as in GA and RRD, the damaged photoreceptor/RPE cells may be replaced by active Müller glia (i.e., gliosis) or myofibroblasts transdifferentiated from other cells such as RPE cells or macrophages. In RRD-induced PVR, the wound healing response leads to excessive ECM deposition and the development of subretinal fibrotic membrane; whereas, in GA, the wound is filled with active Muller glia and infiltrating immune cells without excessive ECM deposition and damage area becomes atrophic. In nAMD, new blood vessels are a part of the pathology, and the healing process is accompanied by continued immune cell infiltration and excessive deposition of ECM around the diseased blood vessels and eventually, the development of fibro-vascular membrane.