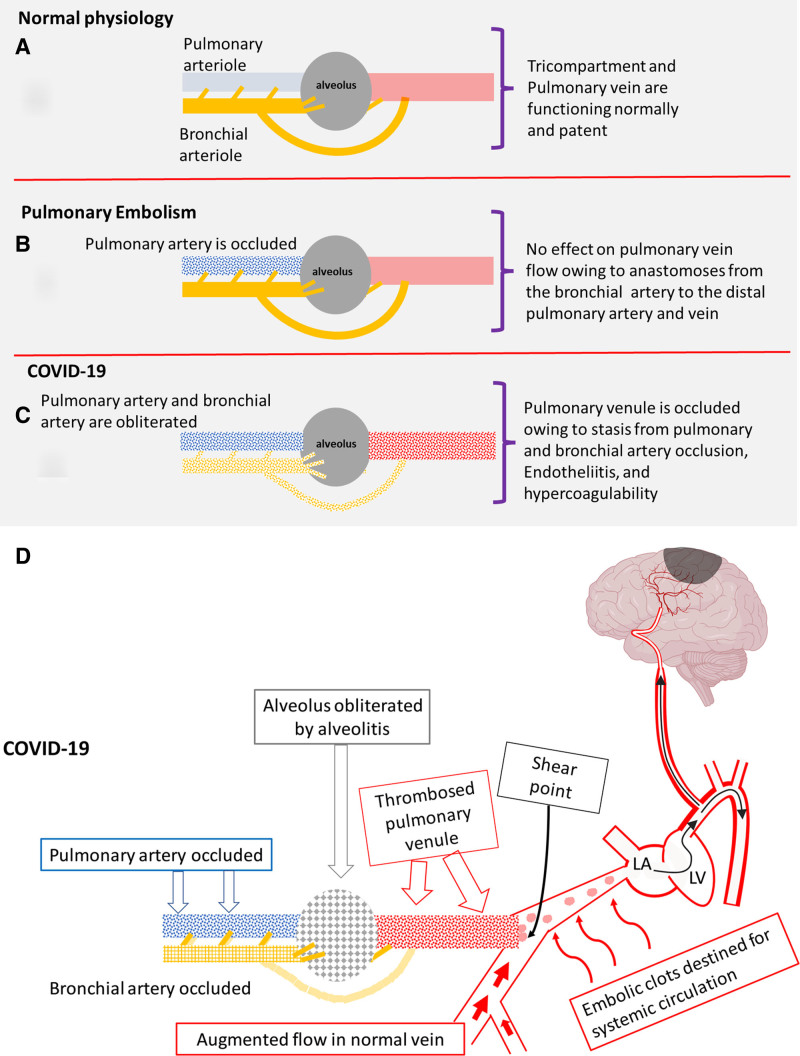
Figure 1.
Oxygenation in normal physiology, pulmonary embolism, and COVID-19. A, Normal: Pulmonary artery, bronchial artery, and alveolus are normal. Pulmonary vein flow is uninterrupted. B, Pulmonary embolism: Pulmonary artery is occluded, but the bronchial artery remains patent. Alveolus is normal (no interference with ventilation). Pulmonary vein remains patent despite loss of the major blood supply (the pulmonary artery) owing to flush-through from profuse anastomoses from bronchial artery to the pulmonary venules. C, COVID-19: The pulmonary and bronchial arteries are occluded by immunothrombosis, and the alveolus is occluded by alveolitis. The pulmonary vein is also occluded because of endotheliitis, hypercoagulability, and loss of the flush-through from the profuse bronchial artery-pulmonary vein anastomoses. D, Dislodgement of small clots at confluence points with patent pulmonary vein segments, leads to clots accessing the systemic circulation which cause strokes. Immunothrombosis in COVID-19 areas leads to augmented flow in adjacent normal areas with 2 important effects. First, central clot propagation is limited apart from the most severe cases; second, increased shear forces on thrombus protruding into patent segments at confluence points (curved arrow) leads to systemic emboli (in a manner similar to the stump emboli theory of stroke in extracranial carotid occlusion).53 LA indicates left atrium; and LV, left ventricle.